Abstract
Context:
The adrenal gland is a common site for neoplastic diseases and primary adrenal lymphoma (PAL) is a rare tumor with around 120 cases reported so far.
Case Report:
We present a rare case of 76-year-old male who presented with headache, confusion, inappropriate body movements and abdominal pain. Adrenal biopsy revealed PAL and he has had an excellent neurologic outcome to date with chemotherapy and involved field radiation.
Conclusion:
The majority of cases of PAL are B cell lymphomas with diffuse large cell in 70% of cases. Clinical symptoms are variable and patients may present with abdominal pain, fever, anorexia, weight loss, fatigue or symptoms of adrenal insufficiency. Therapeutic modalities for PAL include surgery, chemotherapy and radiotherapy and corticosteroid replacement. With this case report, we hope to raise awareness about this rare disease and to include lymphoma in the differential of adrenal masses.
Keywords: Diffuse large B cell lymphoma, Encephalopathy, Paraneoplastic syndrome, Primary adrenal lymphoma
Introduction
Primary adrenal lymphoma (PAL) is a rare neoplastic disease. This entity must be included in the differential diagnosis of adrenal masses as timely diagnosis will ultimately affect intervention. We present a rare case of PAL in an elderly male who presented with paraneoplastic neurological symptoms, which resolved with chemotherapy and radiation.
Case Presentation
This was a case report of 76-year-old male patient who was transferred to our facility with a 3 weeks history of headache, confusion, agitation, difficulty with speech, inappropriate body movements, anorexia and abdominal pain. On presentation, he had a temperature of 38.4°C, cognitive impairment and generalized weakness. His complete blood count, comprehensive metabolic panel, thyroid stimulating hormone, sedimentation rate, ammonia, vitamin B12 levels and anti-nuclear antibody test were negative. Patient was started on vancomycin and piperacillin/tazobactam for his fevers. Magnetic resonance imaging (MRI) of the brain showed tiny hyper-intensities in the right cerebellum on diffusion weighted sequence. Cerebrospinal fluid (CSF) analysis showed a normal cell count and glucose with elevated protein of 102 mg/dl (normal 15-45 mg/dl) and negative cultures. Electroencephalogram showed moderate to severe diffuse encephalopathic process in both hemispheres. His cultures remained negative. As no obvious source of his fever was found, a computed tomography (CT) of chest, abdomen and pelvis was done to rule out occult infection. CT of abdomen revealed 8.6 cm × 6.8 cm × 13 cm left adrenal mass displacing the left kidney laterally [Figure 1]. Adrenal hormone levels were normal and adrenal insufficiency was not demonstrated. Enzyme-linked immunosorbent assay immunoassay was positive for tau protein (1617 pg/ml) in CSF while the Creutzfeldt Jakob 14-3-3 test was ambiguous. Paraneoplastic antibody work-up showed N-type calcium channel antibody, though his CSF antineuronal nuclear antibodies, purkinje cell cytoplasmic antibodies, antiglial nuclear antibody and amphiphysin antibodies were negative.
Figure 1.
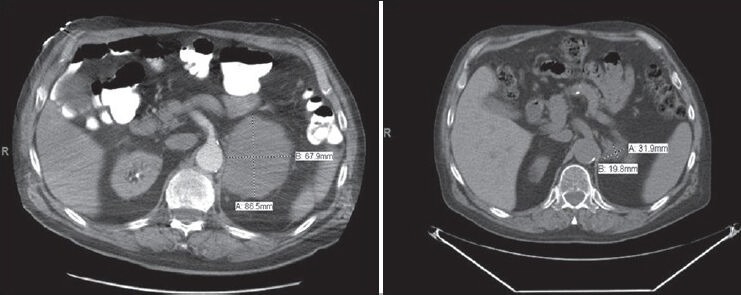
Computed tomographic scan of abdomen showing decrease in the size of left adrenal mass with treatment
Biopsy of the adrenal gland revealed diffuse large B cell lymphoma positive for CD20 and Ki-67 stain showing a proliferative index >90%. Immunostains for cyclin D-1, CD10, S-100, chromogranin A, pankeratin and calretinin were negative [Figure 2]. Chemotherapy with cyclophosphamide, doxorubicin, vincristine, prednisone and rituximab (CHOP-R) was administered followed by involved field radiation therapy. He had resolution of his neurological symptoms and repeat positron emission tomography (PET)-CT scan revealed a residual mass measuring 3.2 cm × 2 cm in the left suprarenal area without hypermetabolic activity [Figure 1].
Figure 2.
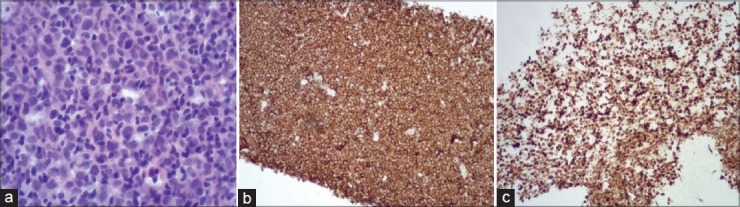
(a) Adrenal biopsy showing neoplastic cells with nuclear pleomorphism and prominent nucleoli with a relatively dark cytoplasm. (b) The cells show diffuse strong staining for B-cell marker CD20 and a very high proliferation rate on the Ki-67 stain (c)
Discussion
The adrenal gland is a common site for neoplastic diseases and can be from metastatic disease, primary adreno-cortical tumors, pheochromocytoma or PAL. Secondary involvement of the adrenal gland with non-Hodgkin's lymphoma occurs in about 25% of patients, PAL represents only 3% of extranodal lymphomas.[1,2] Males are affected more commonly than females; usually in the 6th and 7th decades.[3,4] PAL usually presents with bilateral involvement and may present with adrenal insufficiency with extensive gland involvement. The majority of cases are B cell lymphomas with diffuse large cell in 70% of cases.[1,4]
Autoimmune adrenalitis and origin from hematopoietic tissue within a single gland and gravitation to the contralateral gland has been proposed as an etiology of bilateral PAL.[2] Immune dysfunction such as concurrent or past history of cancer, human immunodeficiency virus, Epstein Barr virus infection or autoimmune disorder may be a predisposing factor in some patients.[3] Clinical symptoms are variable and patients may present with abdominal or lumbar pain, fever, anorexia, weight loss, fatigue or symptoms of adrenal insufficiency.[1,4,5] Laboratory may reveal hyponatremia, hyperkalemia and hypercalcemia. Diagnostic imaging includes ultrasonography, CT, MRI or fluorodeoxyglucose-PET imaging. Ultrasound or CT guided biopsy is the preferred diagnostic procedure;[6] however, carries the risk of metastatic spread of cancer cells and should be performed after exclusion of pheochromocytoma by catecholamine levels.[7]
Central nervous system involvement with PAL is very rare with only few cases reported[8] and review of the literature did not show any other case with paraneoplastic neurological symptoms. Our patient had encephalopathy with anti-N type calcium channel antibodies and tau protein in CSF. Calcium channel antibodies were found in patients with paraneoplastic encephalomyeloneuropathic complication of lung, ovarian, or breast carcinoma.[9] Creutzfeldt Jakob 14-3-3 protein can be found in CSF of patients with limbic encephalitis and paraneoplastic cerebellar degeneration.[10]
Therapeutic modalities for PAL include surgery, combination chemotherapy and radiotherapy and corticosteroid replacement. As it is a rare entity, appropriate treatment guidelines have not been determined. Patients are generally treated with typical regimens used for other lymphomas. Chemotherapeutic regimens that have been used include CHOP ± R, cyclophosphamide, vincristine, prednisone and methotrexate, adriamycin, cyclophosphamide, vincristine, prednisolone.[1,2]
Our case was unique because the patient had unilateral involvement and presented with predominant paraneoplastic neurological symptoms. He has had an excellent neurologic outcome to date and remains in remission at 12 months.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kumar R, Xiu Y, Mavi A, El-Haddad G, Zhuang H, Alavi A. FDG-PET imaging in primary bilateral adrenal lymphoma: A case report and review of the literature. Clin Nucl Med. 2005;30:222–30. doi: 10.1097/01.rlu.0000155983.46815.1c. [DOI] [PubMed] [Google Scholar]
- 2.Ozimek A, Diebold J, Linke R, Heyn J, Hallfeldt K, Mussack T. Bilateral primary adrenal non-Hodgkin's lymphoma and primary adrenocortical carcinoma–Review of the literature preoperative differentiation of adrenal tumors. Endocr J. 2008;55:625–38. doi: 10.1507/endocrj.k08e-035. [DOI] [PubMed] [Google Scholar]
- 3.Ozimek A, Diebold J, Linke R, Heyn J, Hallfeldt KK, Mussack T. Bilateral primary adrenal non-Hodgkin's lymphoma-A case report and review of the literature. Eur J Med Res. 2008;13:221–8. [PubMed] [Google Scholar]
- 4.Mantzios G, Tsirigotis P, Veliou F, Boutsikakis I, Petraki L, Kolovos J, et al. Primary adrenal lymphoma presenting as Addison's disease: Case report and review of the literature. Ann Hematol. 2004;83:460–3. doi: 10.1007/s00277-003-0838-3. [DOI] [PubMed] [Google Scholar]
- 5.Bouchikhi AA, Tazi MF, Amiroune D, Mellas S, El Ammari J, Khallouk A, et al. Primary bilateral non-Hodgkin's lymphoma of the adrenal gland: A case report. Case Rep Urol 2012. 2012 doi: 10.1155/2012/325675. 325675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh D, Kumar L, Sharma A, Vijayaraghavan M, Thulkar S, Tandon N. Adrenal involvement in non-Hodgkin's lymphoma: Four cases and review of literature. Leuk Lymphoma. 2004;45:789–94. doi: 10.1080/10428190310001615756. [DOI] [PubMed] [Google Scholar]
- 7.Spyroglou A, Schneider HJ, Mussack T, Reincke M, von Werder K, Beuschlein F. Primary adrenal lymphoma: 3 case reports with different outcomes. Exp Clin Endocrinol Diabetes. 2011;119:208–13. doi: 10.1055/s-0031-1271629. [DOI] [PubMed] [Google Scholar]
- 8.Hahn JS, Choi HS, Suh CO, Lee WJ. A case of primary bilateral adrenal lymphoma (PAL) with central nervous system (CNS) involvement. Yonsei Med J. 2002;43:385–90. doi: 10.3349/ymj.2002.43.3.385. [DOI] [PubMed] [Google Scholar]
- 9.Lennon VA, Kryzer TJ, Griesmann GE, O’Suilleabhain PE, Windebank AJ, Woppmann A, et al. Calcium-channel antibodies in the Lambert-Eaton syndrome and other paraneoplastic syndromes. N Engl J Med. 1995;332:1467–74. doi: 10.1056/NEJM199506013322203. [DOI] [PubMed] [Google Scholar]
- 10.Saiz A, Graus F, Dalmau J, Pifarré A, Marin C, Tolosa E. Detection of 14-3-3 brain protein in the cerebrospinal fluid of patients with paraneoplastic neurological disorders. Ann Neurol. 1999;46:774–7. [PubMed] [Google Scholar]


