Abstract
Objectives
To examine the efficacy of three theoretically distinct interventions among substance-abusing runaway adolescents and to explore individual differences in trajectories of change.
Methods
Adolescents (N=179) between the ages of 12–17 were recruited from a runaway shelter in a Midwestern city. The sample included 94 females (52.5%) and 85 males (47.5%), the majority of the adolescents were African American (n= 118, 65.9%). Adolescents were randomly assigned to the Community Reinforcement Approach (CRA, n = 57), Motivational Interviewing (MI, n = 61), or Ecologically-Based Family Therapy (EBFT, n = 61). Substance use was assessed at baseline, 3, 6, 9, 12, 18, and 24 months via Form 90 and urine screens.
Results
Hierarchical linear modeling revealed statistically significant improvement in frequency of substance use among runaways in all three treatment groups with a slight increase at post-treatment. Latent trajectory profile analysis explored individual differences in change trajectories and yielded a 3 class model. The majority of adolescents (n = 136, 76%) showed reductions in substance use over time with a slight increase at follow-up (Class 1: Decreasing). Twenty-four (13.4%) adolescents had shown high levels of substance use over time with patterns of increase and decrease (Class 2: Fluctuating high users), and 19 (10.6%) decreased but returned to baseline levels by two years post-baseline (Class 3: U shaped). Few differences among treatment conditions were noted; within the “decreasing” group, adolescents in MI treatment showed a quicker decline in their substance use but a faster relapse compared to those receiving EBFT.
Conclusions
These findings suggest that CRA, EBFT and MI are viable treatments for runaway substance-abusing adolescents.
Keywords: runaway adolescents, substance abuse treatment, randomized controlled trial
Intervention with Substance Abusing Runaway Adolescents and their Families: Results of a Randomized Clinical Trial
Although substance use prevalence among teenagers has been declining since the 1990’s and use trends have been holding steady in recent years, alcohol and drug use remain widespread among teenagers (Johnston, O’Malley, Bachman, & Schulenberg, 2008). Based on the Substance Abuse and Mental Health Service Administration’s (SAMHSA) National Survey on Drug Use and Health (2006), 1.5 million adolescents (6.1% of the total adolescent population) were classified as needing alcohol treatment and only 111,000 of those needing alcohol treatment (7.2%) received it in the past year. Similarly, about 1.4 million adolescents were classified as needing illicit drug use treatment in the past year and 124,000 (9.1%) received such treatment. In sum, over 90% of adolescents aged 12 to 17 who are in need of substance use treatment do not receive treatment. Further, the report noted that the majority of these adolescents were not likely to perceive a need for substance use treatment (SAMHSA, 2006).
Most adolescents (80%) that seek substance abuse treatment seek outpatient therapy (SAMHSA, 2004). Outpatient options can include family therapy, 12-step/self-help, behavioral/cognitive behavioral individual and group therapy or motivational interventions (Vaughn & Howard, 2004). In their review, Vaughn and Howard (2004) identified 15 controlled treatment evaluation studies between 1989 to 2003 and concluded that multidimensional family therapy (Liddle et al., 2001) followed by cognitive-behavioral group treatment (Kaminer & Burleson, 1999) received the highest level of empirical support. In their review, Waldron and Turner (2008) concluded that no clear pattern emerged for the superiority of one treatment model over another even though some models were identified as well-established and others as probably efficacious. By contrast, Becker and Curry (2008) assessed the quality of evidence among 31 clinical trials and identified ecological family therapies, brief motivational interventions and cognitive behavioral therapies to evidence immediate treatment superiority to other approaches in two or more methodologically strong studies. Reviews converge on the conclusion that outpatient therapy’s efficacy with subpopulations of substance abusing adolescents is not well-known, and much more research in this area is needed (Waldron & Turner, 2008).
One subpopulation, runaway adolescents, is a vulnerable and understudied group. The U.S. Department of Health and Human Services defines runaway teens as those minors who have left home for 24 hours without their parent’s or guardian’s permission. In 2002, the McKinney-Vento Act defined homeless individuals as those who lack a fixed, regular, and adequate nighttime residence; and an individual who has a primary nighttime residence that is: a) a supervised publicly or privately operated shelter designed to provide temporary living accommodations; b) an institution that provides a temporary residence for individuals intended to be institutionalized; or c) a public or private place not designed for, or ordinarily used as regular sleeping accommodations for human beings. By this definition, adolescents residing in a public (runaway) shelter meet criteria for homelessness. Even so, most adolescents residing in runaway shelters have never spent a night on the streets and are at less risk for a range of problems compared to street recruited youths (Robertson & Toro, 1999). Furthermore, the majority of shelter residing runaways return home, which is not the case for street living youth (Ensign & Bell, 2004). This study focused on adolescents who briefly accessed a runaway crisis shelter, had contact with their family, and were able to return home to a family situation, referred to as ‘runaways.’
A recent literature review (Slesnick, Dashora, Letcher, Erdem, & Serovich, 2009) shows that only four randomized intervention studies, two focused on substance use (Slesnick & Prestopnik, 2005; 2009), and two focused on HIV prevention (Rotheram-Borus, Koopman, Haignere, & Davies, 1991; Rotheram-Borus et al., 2003) have been conducted with shelter-recruited runaways. This is of concern because runaways are not rare; between 500,000 to 2.8 million runaway and homeless youth exist in the U.S. (Cooper, 2006). Family conflict and physical and sexual abuse are often cited reasons for adolescents leaving home or being asked to leave home (Lindsey, Kurtz, Jarvis, William, & Nackerud, 2000). But there are other and sometimes overlapping reasons including family crises, drug and alcohol abuse in the home and/or parental unwillingness or inability to care for them. Runaway teenagers consume alcohol and use drugs at significantly higher levels than non-runaway teenagers (Lifson & Halcon, 2001), begin using alcohol and drugs at a younger age and report significantly more associated problems (Slesnick et al, 2009).
Current Study
The current trial was designed to evaluate three theoretically distinct interventions which hold promise for addressing substance abuse and related problem behaviors among shelter-recruited runaway adolescents – an ecological family therapy intervention (Ecologically-Based Family Therapy, EBFT) (Slesnick, 1997), an individual, primarily operant-based approach (Community Reinforcement Approach, CRA) (Meyers & Smith, 1995), and a brief, client-focused motivational intervention (Motivational Interviewing, MI) (Miller & Rollnick, 2001). These three treatments were chosen as each has been tested with homeless youth, and each has a distinct theoretical basis for guiding procedures (e.g., family systems, behavioral and cognitive-behavioral and motivational). Studies comparing outcomes of treatments that use a similar theoretical basis (such as family systems therapy) rarely show differences in outcome, presumably because of the shared theoretical foundation (e.g., Liddle, 2004). If all treatments are associated with reductions in problems behaviors, this information could potentially offer shelters a range of options fitting their agency’s philosophy.
EBFT is a home-based family systems therapy that is theoretically based upon Bronfenbrenner’s theory of social ecology (Bronfenbrenner, 1979). The family systems framework assumes that as positive changes in family interaction patterns, including improved communication and family cohesion, become established through the intervention, substance use and related problems will dissipate over time as the new patterns of interaction become established. This new interaction style, along with reduced problem behaviors, is expected to be maintained over time through homeostatic or negative feedback loops. Adolescents staying in runaway shelters reported that their greatest needs concerned their living arrangements, family relationships and communication with their primary caregivers (Teare et al., 1992). Because research suggests that family factors are highly correlated with the act of running away, engaging primary caregivers in counseling is almost always considered advisable (Chamberlain & Mackenzie, 2004; Rohr & James, 1994). An intervention that addresses multiple risk and protective factors including family relationships, communication, and other individual and ecological factors should theoretically produce greater reductions in substance use over time than alternative interventions that do not address the family (as well as other) risk and protective factors.
Two studies evaluated EBFT for substance abusing adolescents recruited from emergency runaway shelters (Slesnick & Prestopnik, 2005; 2009) as compared to treatment as usual through the shelter. In both studies, adolescents who received EBFT showed dramatic declines in alcohol and drug use up to 15 months post-baseline compared to treatment as usual or shelter services. Significant declines in associated problem behaviors (depressive symptoms, delinquency, perceived family conflict and cohesion) were also observed. One of these studies indicated that family therapy offered in the home of runaway families is associated with better engagement and treatment retention than office-based therapy (Slesnick & Prestopnik, 2009). This supports other research suggesting that home-based therapies are particularly effective at engaging chaotic families with substance abusing adolescents (e.g., Henggeler & Borduin, 1995). Therefore, in this study, all treatment interventions were conducted in the home.
CRA is an individual therapy model; it reinforces successive approximations, utilizes contingency management techniques to promote non-substance using and adaptive coping strategies to address difficult situations (Meyers & Smith, 1995). CRA has shown efficacy in treating adolescent marijuana abusers (Dennis et al., 2004) and street living, homeless youth with a range of substance use and related problems (Slesnick, Prestopnik, Myers, & Glassman, 2007).
As a brief intervention, Motivational Interviewing (MI; Miller & Rollnick, 2001) has shown utility even when compared to high intensity interventions (Dennis et al., 2004) and for individuals with high levels of substance use (Burke, Arkowitz, & Menchola, 2003). Miller et al. (1995) concluded that brief interventions have the greatest evidence for efficacy and also have been the focus of the largest number of studies, conclusions which have been reiterated more recently (Becker & Curry, 2008). The World Health Organization (1996) reported the findings of a multinational trial of brief intervention in primary care settings that showed a significant decrease in daily alcohol consumption following a 5 to 15 minute intervention with a health care provider. Several studies indicate that MI is likely to have a significant short-term (Bonsack et al., 2011) but larger (Kay-Lambkin, Baker, Lewin, & Carr, 2009) effect on targeted outcomes compared to longer-term interventions. But the lack of observed difference in long-term effects when compared to other treatment modalities (Baker, Turner, Kay-Lambkin & Lewin, 2009; Bonsack et al., 2011) suggests that the short-term reductions may be compensated by a greater relapse/increase in the targeted problem behaviors during long-term follow-ups.
Additionally, as CRA is theoretically distinct from EBFT, MI is theoretically distinct from both CRA and EBFT, as it focuses on the motivation component of change rather than the family or skills training components.
Research objectives and hypotheses
Research objective 1: Treatment outcomes
The primary goal of the study was to test the effectiveness of three theoretically distinctive interventions on substance use up to 24 months post-baseline. It was hypothesized that frequency of drug and alcohol use among runaways would be reduced over time in all treatment conditions (main effect of time). Treatment differences were also expected; those assigned to EBFT would show greater reductions over time than those assigned to CRA and MI (main effect of treatment).
Research objective 2: Exploring change classes across treatment conditions
Some researchers have noted that even if a treatment has been shown to be effective on average, no treatment has been shown to work for everyone (Lutz, Martinovich, & Howard, 1999). Therefore, the secondary aim was to explore the variability in individual patterns of change among substance abusing adolescents. Change classes were expected to occur with the majority of the adolescents showing decreasing substance use over time (i.e, linear trend) whereas some adolescents were expected to change in different patterns (i.e., cubic, quadratic or cyclical trends). In addition, it was hypothesized that rates of change in substance use and potential relapse could be related to treatment condition. Specifically, the majority of the adolescents who showed a consistent change pattern (i.e., linear) with slight relapse were expected to be in the EBFT and CRA groups, rather than in MI. Given its brevity, MI condition was expected to have more adolescents with a nonlinear change pattern with quicker decline in substance use and sooner relapse than CRA and EBFT. This focus on differences in change trajectories aligns with changes in the field seeking to understand which treatment intervention is effective for which individuals, and how individuals respond to different treatments (Murphy, Lynch, Oslin, & TenHave, 2007).
Method
Participants
All participants were recruited from a runaway shelter which provided short-term (usually 3 days) crisis shelter and services for minor adolescents. The data were collected in a Midwestern city from February 2005 to December 2007. Eligible participants (N=179) were between the ages of 12 to 17 years, had the legal option of returning home, had at least one parent/primary caregiver willing to participate to the study, and met DSM-IV (American Psychiatric Association (APA), 2000) criteria for alcohol or drug abuse or dependence. Of the 467 adolescents who were approached at the shelter, 62.7% (N=293) were eligible and 61.4% (N=179) of eligible families were successfully engaged into the study.
Characteristics of the sample at baseline are presented in Table 1. The adolescents were on average 15.4 years of age (SD= 1.2) while their primary caregivers were on average 41.2 years old (SD =8.4 years). There were 94 females (52.5%) and 85 males (47.5%) in the adolescent sample. The majority of the adolescents were African American (n= 118, 65.9%), with another 26% being White, non-Hispanic (n = 46). Eighty-seven percent of the primary caregivers were female (n = 156), and 76.4% were mothers to the adolescents in the project. More than half of the caregivers reported working full-time (n = 101, 58.7%), 20 (11.6%) caregivers worked less than 40 hours a week, and 42 (24.4%) were unemployed. The majority of the adolescents (81.6%) were enrolled in school. At baseline, adolescents reported 3.22 (SD = 5.32) runs on average and 31.58% days of substance use in the last 3 months.
Table 1.
Characteristics of the Sample
| Runaway youth | Primary caregivers | ||||
|---|---|---|---|---|---|
| n (%) | Mean (SD) | n (%) | Mean (SD) | ||
| Gender | |||||
| Female | 94 (52.5%) | 156 (87.2%) | |||
| Male | 85 (47.5%) | 23 (12.8%) | |||
| Ethnicity | |||||
| African American | 118 (65.9%) | 117 (65.4%) | |||
| White, non-Hispanic | 46 (25.7%) | 51 (28.5%) | |||
| Hispanic | 3 (1.7%) | 1 (.6%) | |||
| Native American | 2 (1.1%) | 3 (1.7%) | |||
| Asian/Asian American | 1 (.6) | 0 | |||
| Other | 9 (5%) | 7 (3.9%) | |||
| Age | 15.4 (1.2) | 41.2 (8.4) | |||
| Currently enrolled in school | 146 (81.6%) | 0 | |||
| Employment status | |||||
| Full time: 40 hours a week | 101 (58.7%) | ||||
| Part time: less than 40hours | 20 (11.6%) | ||||
| Homemaker | 6 (3.5%) | ||||
| Retired | 3 (1.7%) | ||||
| Unemployed | 42 (24.4%) | ||||
| Marital status | |||||
| Single, never been married | 78 (45.3%) | ||||
| Legally married | 39 (22.7%) | ||||
| Divorced | 26 (15.1%) | ||||
| Separated but still married | 18 (10.5%) | ||||
| Widowed | 5 (2.9%) | ||||
| Total family annual income | |||||
| $0–$5000 | 19 (13.2%) | ||||
| $5001–$15000 | 37 (25.7%) | ||||
| $15001–$30000 | 44 (30.6%) | ||||
| $30001–$45000 | 25 (17.4%) | ||||
| More than $45001 | 19 (5.6%) | ||||
| # of runs | 3.22 (5.32) | ||||
| % days of substance use | 31.58 (29.16) | ||||
Procedure
A research assistant (RA) engaged runaway adolescents at the shelter within 24 hours of their stay and screened them to determine eligibility and interest. Once the adolescent’s permission was obtained, RAs contacted the adolescent’s parent or legal guardian. If the parent agreed to participate and provided written consent, initial assessments for both parent and adolescent were scheduled within 24 hours when possible. During the initial assessment, written assent was obtained from the adolescent and the research assistant administered the Computerized Diagnostic Interview Schedule for Children (CDISC; Shaffer, 1992). Adolescents not meeting eligibility criteria continued with treatment as usual through the runaway shelter. Upon completion of the baseline assessment, adolescents received a $40 gift card and primary caregivers received $25 cash. The participants were assigned to a treatment condition at the end of the assessment and were informed about their group. RAs contacted the therapist to facilitate communication with the client and to schedule the first session. This strategy was preferred so as to engage the client into treatment as soon as possible. Urn randomization, with conditions balancing age, gender and ethnicity, was used to assign adolescents to one of three treatments: (1) 4 sessions, Motivational Interviewing (MI) (n = 61), (2) 14 sessions, the Community Reinforcement Approach (CRA) (n = 61), or (3) 14 sessions, Ecologically-Based Family Therapy (EBFT) (n = 57). All therapy sessions were conducted in the home. Therapists assisted adolescents when they needed transportation to the sessions and were flexible with meeting times. A six-month treatment window was set so that all therapy had to be completed by six months post-baseline.
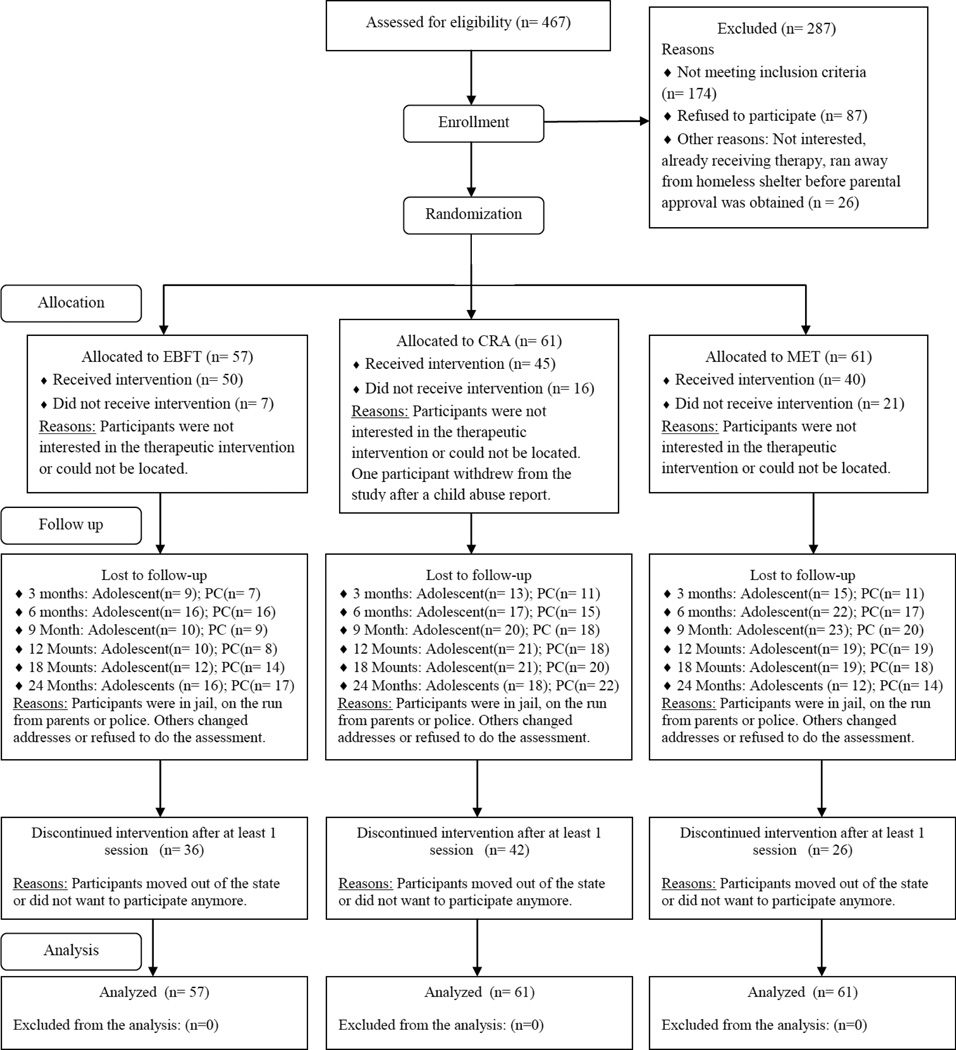
Adolescents and their primary caregivers were evaluated at 3, 6, 9, 12, 18 and 24-months after the baseline assessment. All assessments were conducted at the participant’s home. Similar to the initial assessment, adolescents received a $40 gift card and primary caregivers received $25 for completing each follow-up assessment. Study design and flow of participants are presented in Figure 1. All procedures were approved by the Institutional Review Board of The Ohio State University.
Figure 1.
The CONSORT E-Flowchart
Therapists, clinical training and supervision
Therapists were nested within treatment conditions (MI = 3 therapists, CRA = 2 therapists, EBFT = 3 therapists). Therapists (one male, seven female) included Master’s level independent counselors or social workers (n = 4) and graduate students in couple and family therapy (n = 4). Initially, clinical training included review of treatment manuals and standard protocols (MI, Miller & Rollnick (2002); CRA, Meyers & Smith, 1995; EBFT, Slesnick, 2000), and a two day didactic training and extensive role plays. In addition, therapists received weekly supervision, and case consultation with audiotape reviews. Supervisors (two male, one female) were highly-skilled expert clinicians, including Master’s level, certified MI clinical supervisor (Gary Lamb-Hart), and the original developers of CRA (Robert J. Meyers) and EBFT (Natasha Slesnick). The number of years of clinical experience among the supervisors ranged from 15 to 30 years.
Treatment fidelity
In an attempt to ensure treatment adherence and competence, codes were developed for each intervention condition utilizing standard treatment manuals and protocols (Meyers & Smith, 1995; Miller & Rollnick, 2002; Slesnick, 2000). Codes included two parts for various treatment procedures, 1) the occurrence (yes/no) of the procedure during the session and 2) how well it was done by the therapist (rated on a 7 point Likert scale). Response categories were 1=very poorly, 2=poorly, 3=somewhat, 4=average, 5=well, 6=very well and 7=exceptional. Specifically, MI codes included 10 procedures and sample items were “Did the therapist express confidence in the client’s ability to make changes? If yes, how effectively?” and “Did the therapist allow the client to “win” during power struggles or when resistance was encountered? If yes, how effectively?”
CRA codes rated the fidelity over 9 procedures which included items such as “Did the therapist link positive rewards to non-drinking/non-problematic behavior? If yes, how effectively?” “Did the therapist examine triggers or reasons the client is using drugs/participating in problematic behavior, including the emotions behind the response? If yes, how effectively?” and “Did the therapist spend time teaching skills? (i.e., communication, anger management, drug refusal etc.) If yes, how effectively?”
EBFT adherence was rated over 10 procedures. Examples include, “Did the therapist use relational comments? If yes, how effectively?” “Did the therapist side with each family member? If yes, how effectively?” and “Did the therapist reframe/relabel family members’ comments? If yes, how effectively?” If the procedure was not observed in the session, it received a zero. If it was observed, it was rated in its effectiveness on a 7 point Likert scale. The procedure items were summed and means were calculated for each session (therapist’s fidelity to treatment for that session). For competence, the possible range was 0 – 7 for all treatment conditions.
Using these coding schemes, audio recordings of sessions were independently coded by supervisors and six graduate student coders (two in each treatment condition). Coders were not project therapists and were also nested within treatment condition. Each was trained in the respective intervention by the clinical supervisor. In addition, coders achieved a .80 inter-rater reliability with the clinical supervisor prior to beginning coding. For CRA and EBFT, the first two sessions of each case were coded and a randomized selection of 20% of the remaining sessions. For MI, each session was coded. For all conditions, 10% of the coded session recordings were double-coded by the second rater to ensure inter-rater reliability of 80%. When reliability was found to dip below 80%, coders met together with the supervisor to resolve discrepancies, with the goal to maintain at least an 80% inter-rater reliability of codes throughout the study.
Treatment conditions
Motivational Interviewing
MI assumes that the client is responsible for and capable of change; the therapist’s role is to enhance the client’s intrinsic motivation (Miller & Rollnick, 2002). MI is based on the principles of expressing empathy, developing discrepancies between actual behavior and desired behavior, rolling with resistance, and supporting the client’s self–efficacy (Miller & Rollnick, 2002). Sessions focus on eliciting and reinforcing client’s “change talk” and increasing client’s motivation to change substance use. Forty-four recordings were coded for adherence and competence. Good therapist adherence was observed - the average number of procedures used during a session was 9.84 out of 10 possible procedures (SD=.64, range 6.67 – 10.0). Good therapist competence was observed with an average rating of 5.14 on a scale from 0 to 7 (SD = .64, range 3.17 – 6.33). Inter-rater reliability for 39 double-coded recordings for procedure occurrence (adherence) was Kappa=0.98, while the rater reliability of the procedure rating (competence) was ICC=0.81. The average number of therapy sessions attended among all those assigned to MI was 1.6 (SD = 1.6).
Community Reinforcement Approach
CRA is based on operant behavioral principles (Meyers & Smith, 1995). The therapist helps the client identify triggers as well as the short-term positive and long-term negative consequences of substance use using a functional analysis. Alternative behaviors which compete with substance use are identified. CRA teaches new communication and problem-solving skills and increases coping skills through role play and discussion. Fifty-two recordings were coded for adherence and competence. Good therapist adherence was observed - the average number of procedures used during a session was 7.55 out of 9 potential procedures (SD=1.50, range 4.00 – 9.00). Average therapist competence had an overall rating of 4.44 on a scale from 0 to7 (SD = 1.16, range 1.60 – 6.40). Inter-rater reliability for 20 double-coded recordings for procedure occurrence (adherence) was Kappa=0.71, while the rater reliability of the procedure rating (competence) was ICC=0.86. The average number of therapy sessions attended among all those assigned to CRA was 5.3 (SD = 4.6).
Ecologically-Based Family Therapy
EBFT is a family systems intervention which also includes concepts from Bronfenbrenner’s theory of social ecology (1979). The EBFT therapist works with the adolescent, family, and others significant to the family to target specific dysfunctional interactions which correspond to the development and continuation of problem behaviors. Thus, the intervention is focused on the social interactions among all participants that create the type of skill sets and emotional baseline for use in social interactions within and across systems. One hundred fifteen recordings were coded for adherence and competence. Good therapist adherence was observed - the average number of procedures used during a session was 8.61 out of 10 potential procedures (SD=1.69, range 2.50 – 10.00). Good therapist competence was also found, with an average rating of 4.10 out of 7 (SD = 1.24, range .50 – 6.50). Inter-rater reliability for 21 double-coded recordings for procedure occurrence (adherence) was Kappa=0.75, while the rater reliability of the procedure rating (competence) was ICC=0.84. The average number of therapy sessions attended among all those assigned to EBFT was 6.8 (SD = 5.5).
In sum, each intervention had a distinctive approach to treatment; CRA operated through reinforcers, EBFT included interventions to change family interaction patterns and MI worked through change talk in a nondirective manner. In addition, each intervention group was offered two HIV prevention sessions based upon Becoming a Responsible Teen (BART; St. Lawrence et al., 1995). Considering the differences between treatment approaches, BART was not incorporated or integrated into the treatment protocols. Instead, it was provided as a separate, standardized add-on treatment and was offered to the participants after completion of at least one session of the main intervention. BART employs a psychoeducational approach and includes an emphasis on skills acquisition and safe sex practice using role play and discussion (Cornelius & St. Lawrence, 2009; St. Lawrence et al., 1995). The first session was devoted to AIDS education, assessment of risk, risk reduction and skills practice and the second session included focus on sexual assertiveness and practicing negotiation.
Materials
All data for the current analysis were collected using interview and self-administered questionnaires. An RA administered the Computerized Diagnostic Interview Schedule for Children (CDISC; Shaffer, 1992) to adolescents. This diagnostic interview is based on DSM IV-TR (APA, 2000) and diagnoses alcohol, tobacco, and other substance abuse and dependence. CDISC was used to determine formal eligibility. Adolescents and PCs completed demographic questionnaires, assessing age, gender, ethnicity, education, income and marital status.
The Form 90 Substance Use Interview (Miller, 1996) was administered to adolescents to assess frequency of drug and alcohol use. The Form 90 is a semi-structured questionnaire that yields total number of days of all drug use including alcohol in the past 90 days. This tool has shown excellent test-retest reliability in a sample of runaway substance-abusing adolescents with kappas ranging from .74 to .95 (Slesnick & Tonigan, 2004). In this study, the total percent days of alcohol and drug use (except tobacco) in the prior 90 days was used as the primary dependent variable.
Similar to previous substance abuse treatment outcome studies (e.g., Simpson, Joe, & Broome, 2002), research assistants also collected urine samples from the adolescents at baseline and follow-up assessments. BMC ToxCup® Test Kit was utilized and tested for Cannabinoids, Amphetamines, Methamphetamines, Phencyclidine (PCP), Cocaine/Crack, and Opiates (Branan Medical Corp., Irvine, CA). ToxCup reports that THC is detected in the urine for 3–5 days after use for occasional users and up to 14 days for chronic users. Opiates are detectable for up to 3 days, cocaine for 24–60 hours, and amphetamines for 3–5 days after last use. This drug screening procedure has shown high specificity and sensitivity to the drugs tested converging with the findings from self-reported drug use (Lennox et al., 2006).
Overview of Statistical Analysis
Preliminary analysis
Characteristics of participants (gender, age, ethnicity) and substance use at pretreatment were compared using Chi square and One-way ANOVA. There were 6 follow up assessments in total and each youth received a score for the percent of follow ups completed across the study (labeled as “follow up rates”). Given that treatment conditions offered unequal number of sessions (MI = 4 sessions vs. EBFT and CRA = 14 sessions.), percentages were also calculated for the number of sessions youth attended (labeled as “treatment attendance”). One-way ANOVAs were conducted to compare follow up rates and treatment attendance rates across treatment groups. Following Hansen et al.’s (1985) suggestions, missing data analyses were also performed, using independent samples t-tests and bivariate correlations. Means of substance use were compared to test whether those who completed vs. missed the next follow up assessment had reported different levels of substance use at the prior assessment. For instance, substance use reported at the 3 month follow up was compared among those who completed vs. skipped the 6 month follow up. Similarly, substance use reported at 6 months was compared to those who completed vs. skipped the 9 month follow up and so on. If the means of substance use were not different between assessment completers and drop outs, it would be assumed that data are missing at random (Hansen et al., 1985).
Research objective 1: HLM Analysis testing treatment outcomes
Given the longitudinal design of the study with participants nested in treatment conditions over time, multilevel modeling was conducted using HLM 6 software (Raudenbush, Bryk, & Congdon, 2004). HLM included two levels; at the within subjects level (Level 1), substance use varied within participants over time as a function of a person-specific growth curve. This level tested for time effects, estimating the change in substance use across the 3-,6-, 9-, 12-, 18 and 24 months. At level 1, the linear factor (TIME) described the linear growth in outcome, and the quadratic factor (TIME2) described acceleration in the rates of change such as relapse in substance use. At the between subjects level (Level 2), person specific change parameters varied randomly across participants as a function of three treatment conditions (EBFT, CRA, MI). That is, at level 2 dummy coded treatment conditions (1= EBFT, 0 = MI and 1= CRA, 0 = MI) were entered to explain the linear or quadratic change in outcomes. In addition, treatment attendance (percent of sessions attended), ethnicity (dummy coded 1=minority, −1=White), gender (dummy coded 1=male, −1=female), and age were entered as covariates at Level 2 in the model. The growth models were estimated for the frequency of substance use (FORM 90 score) with Full Maximum Likelihood estimation using an intent to treat design.
Research objective 2: Latent Profile Trajectory Analysis (LPTA) exploring change classes
In order to examine trajectories of change from baseline across the 6 follow-up assessments, LPTA was performed using MPLUS 6 statistical software (Muthen & Muthen, 2010). This exploratory analysis identifies clusters of individuals who change in different ways, by creating groups with similar variances, but different mean intercepts and mean slopes. MPLUS utilizes an expectation maximization algorithm and the maximum likelihood estimator under the assumptions of data missing at random (Muthen & Muthen, 2010). The analyst tests several models to determine the best fit using the Bayesian Information Criterion (BIC) and the entropy estimate. Entropy is the ability of the model to estimate the correct group for an individual based on the model and observed variables. Analysis revealed several latent profile trajectory models and the model with the best empirical and conceptual fit was selected as the solution.
Comparative analyses to characterize change classes
One-Way ANOVA with a post-hoc Tukey procedure was run to determine if there were differences between each change trajectory group by treatment condition. Specifically, differences in the mean intercept, mean slope and mean quadratic terms were compared among three treatment conditions for each change class. The SPSS version 17 (SPSS, 2008) was used for the initial data screening, descriptive analyses, multinomial logistic regression and One-Way ANOVAs.
Results
Preliminary analysis
Data screening for randomization
At baseline, treatment conditions did not differ in age [F (2,176) = 1.35, p > .05], ethnicity [χ2 (8) = 7.08, p > .05], or gender [χ2 (2) = 4.10, p > .05]. Similarly, no statistical differences at baseline were found between EBFT, CRA or MI groups in substance use [F (2,176) = 1.70. p > .05] or number of runaway episodes [F (2,170) = 1.07, p > .05].
Concurrent validity of substance use data
Urine screens were compared to the calendar data information obtained in Form 90. To that aim, the agreement between self-reported substance use (used at least one day vs. no use) and urine screen (urine positive vs. negative for a particular substance) was analyzed using Kappas. Overall, percent days of drug use in the past 90 days (as reported in Form 90) showed high agreement with the urine screening, with Kappas ranging from .92 to .98 across follow ups.
Allocation
As presented in Figure 1, forty-six (25.7%) adolescents did not attend any therapy sessions. In particular, 50 of 57 (87.7%) participants received intervention in the EBFT condition, 45 of 61 (73.8%) adolescents received CRA, and 40 of 61 (65.6%) adolescents received MI. It was found that adolescents in EBFT condition were more likely to receive intervention than those in CRA and MI condition [χ2 (2) = 7.50, p < .05].
Treatment attendance
(Percent of sessions attended). Adolescents attended 43% (SD = 38.3%) of the sessions on average with 29 (16.2%) adolescents attending all sessions. Specifically, adolescents participated in 51.1% of the sessions (SD = 40.5%) in EBFT, 39.8% of the sessions (SD = 34.5%) in CRA, and 38.1% of the sessions (SD = 39.4%) in MI. There were no statistically significant differences in therapy attendance across treatment conditions [F (2,176) = 2.003. p > .05].
Differential attrition from assessments and missing data analysis
Follow up rates (percent of assessments completed) for adolescents ranged from 69% to 79% across 6 time points (3, 6, 9, 12, 18 and 24 months) and did not differ among treatment conditions [F(2,176)=3.09, p <.05]. In addition, t tests were run for each follow up point. The analysis revealed no differences between assessment drop outs and assessment completers in their substance use at 3 months [t (177) = −.37, p > .05], 6 months [t (136) = −.64, p > .05], 9 months [t (118) = −1.32, p > .05], 12 months [t (124) = .18, p > .05], 18 months [t (123) = −.59, p > .05], or 24 months [t (126) = .34, p > .05]. These findings suggested that attrition from a particular follow up assessment did not appear to be a function of prior status on substance use (i.e. missing 9 month follow up was not associated with substance use at 6 months). Therefore, missing data due to assessment non-completion were assumed to be missing at random (Graham & Donaldson, 1993).
Research objective 1: HLM Analysis testing treatment outcomes
Following a stepwise model construction procedure, the unconditional model was tested first (Table 2). The results yielded significant variability in the baseline substance use scores between participants [χ2 (178) = 887.26, p < .001]. ICC was .43, indicating nonindependence and the need for multilevel modeling (Raudenbush, Bryk, & Congdon, 2004). Next, the random coefficients models were run to determine the general form of change that best fit the data across seven time points. Using deviance test, the quadratic model revealed significantly better fit than the linear model [χ2 (3) = 47.22, p < .001]. Specifically, the quadratic model indicated a significant negative intercept for the linear slope [b = −7.55, SD = 1.39, t(178) = − 5.45, p < .001] and positive intercept for the quadratic slope [b = 1.18, SD = .23, t(178) = 5.04, p < .001]. These results indicated significant reductions in substance use over time with a slight increase at follow ups (Table 2).
Table 2.
Results of multilevel modeling testing change in substance use over time across treatment conditions
| Unconditional model |
Random coefficients Linear model |
Random coefficients Linear and Quadratic model |
Combined model |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient(SE) | t-value | Coefficient(SE) | t-value | Coefficient (SE) | t-value | Coefficient(SE) | t-value | ||||
| Fixed effects | |||||||||||
| Intercept | |||||||||||
| Intercept | 24.18 (1.77) | 13.65*** | 26.01 (2.01) | 12.96*** | 30.66 (2.1) | 14.57*** | 31.69 (3.62) | 8.76*** | |||
| EBFT | |||||||||||
| CRA | |||||||||||
| Linear slope | |||||||||||
| Intercept | −.75 (.52) | −1.45 | −7.55 (1.39) | −5.45*** | −9.73 (2.41) | 4.03*** | |||||
| EBFT | 4.93 (3.39) | 1.46 | |||||||||
| CRA | 1.34 (3.41) | .39 | |||||||||
| Quadratic slope | |||||||||||
| Intercept | 1.18 (.23) | 5.04*** | 1.45 (.40) | 3.58*** | |||||||
| EBFT | −.63 (.57) | 1.11 | |||||||||
| CRA | −.15 (.57) | .26 | |||||||||
| Random effects | Variance component(SD) |
χ2 | Variance component(SD) |
χ2 | Variance component(SD) |
χ2 | Variance component(SD) |
χ2 | |||
| Intercept | 432.52 (20.79) | 887.26*** | 459.19 (21.43) | 441.48*** | 468.05 (21.63) | 356.98*** | 470.96 (21.70) | 357.27*** | |||
| Linear slope | - | - | 23.83 (4.88) | 350.65*** | 90.41 (9.51) | 222.01*** | 87.54 (9.36) | 218.77*** | |||
| Quadratic slope |
- | - | - | - | 2.62 (1.62) | 231.21*** | 2.62 (1.62) | 229.21*** | |||
| Level 1 error | 571.87 (23.91) | 460.09 (21.45) | 395.84 (19.89) | 395.69 (19.89) | |||||||
p < .001
Treatment effect was tested by adding intervention type at level 2 to explain the variability in change in substance use. This mixed effects model retained significant linear [b = −9.73, SD = 2.41, t(176) = − 4.03, p < .001] and quadratic [b = 1.45, SD = .40, t(176) = 3.58, p < .001] time effects, but yielded no differences across treatment conditions (p > .05) (Table 2). That is, youth showed improvements in their substance use with an increase at follow ups in all treatment conditions and none of the interventions was superior to the other.
Next, age, gender, ethnicity and treatment attendance were added to the mixed model to test if they explained the variability in intercepts (baseline substance use) and slopes (change in substance use). It was found that ethnicity predicted change in substance use; minority youth showed significantly more reductions in substance use [b = −5.76, SD = 2.7, t(172) = − 2.14, p < .05], but relapsed sooner [b = 1.04, SD = .44, t(172) = 2.37, p < .05], than the White youth (Table not shown).
Clinical significance
Following Jacobson and Truax’s (1991) empirical approach, reliable change index (RC) was calculated for each participant, using the formula [(XPost-treatment at 6 months – XPre-treatment) / Sdiff]. RC > 1.96 was operationalized as the threshold for improvement in clinical outcomes whereas −1.96 ≤ RC ≤ 1.96 referred to some change that was not clinically significant (Jacobson & Truax, 1991). Finally, RC < −1.96 was defined as deterioration. It was found that 66 (55%) youth in the current sample showed clinically significant change at 6 months in their substance use. In addition, thirty-five (29.2%) youth had some reductions in substance use, but they did not achieve clinical change (‒1.96 ≤ RC ≤ 1.96) and nineteen youth (15.8%) showed deterioration at post-treatment (RC < −1.96). These findings revealed that the majority of the participants reported less substance use at post-treatment compared to baseline.
Multinomial logistic regression suggested no differences across treatment conditions to predict clinical change group (p > .05). Similarly, youth who showed meaningful improvement in their substance use or youth who showed some improvement were not different in gender, age, ethnicity, or their participation to treatment than those who deteriorated. These clinical significance findings partially confirm the HLM analysis, suggesting overall improvement in substance use in the sample with no treatment differences.
Research objective 2: Latent trajectory profile analysis exploring change classes
Both HLM and clinical significance findings suggested heterogeneity of participants in their trajectories of change in substance use. A Latent Trajectory Profile analysis (LTPA) was performed to further explore this variability in the sample. Models with 5, 4, 3, 2 and 1 classes were tested using self-reported substance use at 7 assessment points as indicators of class membership. Examining BIC and entropy values of the models, the 3 class model yielded the optimal fit (LL = −4490.59; BIC=9230.17, Entropy= .947) to the data.
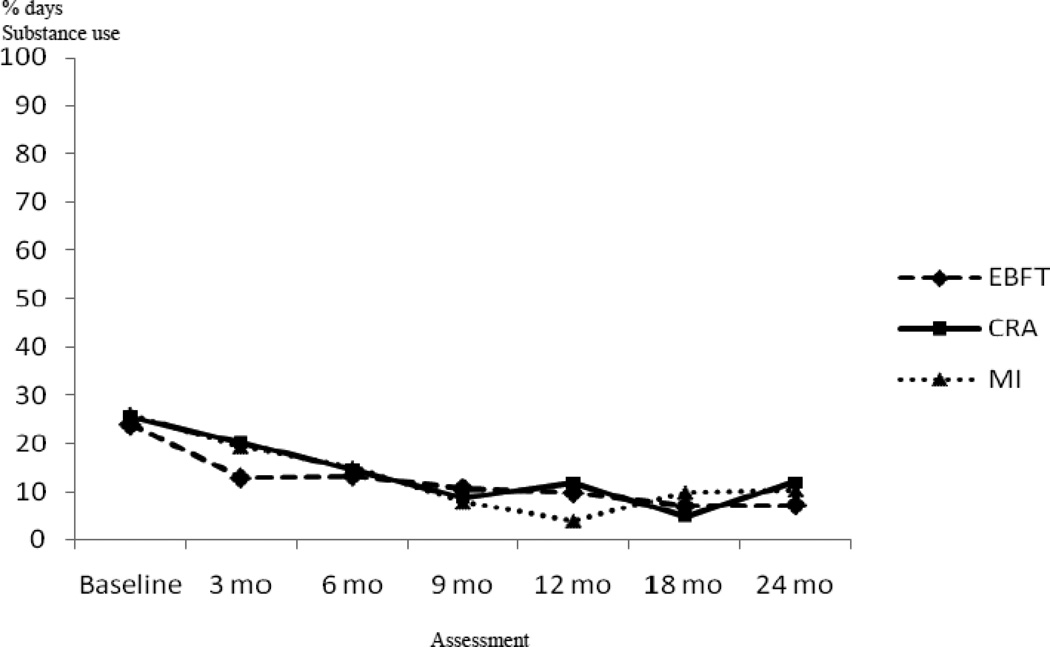
According to the LTPA, the majority of the participants (n=136, 76%) showed a decrease and then a slight increase in substance use over time. This change group was labeled as “Decreasing” (Figure 2). Specifically, 36 of 57 (63.2%) adolescents in EBFT, 50 of 61 (82%) adolescents in CRA and 50 of 61 (82%) adolescents in MI treatment condition revealed a decreasing pattern. As presented in Table 3, substance use continued to decrease at 18 months in EBFT condition (Mean=6.94, SD=13.28) and increased at 24 months (Mean=7.18, SD=10.21). Similarly, adolescents in the CRA group reported the lowest frequency of substance use at 18 months (Mean=4.95, SD=8.68) with an increase at 24 months (Mean=11.99, SD=16.16). Substance use was reduced over time in the MI condition at 12 months (Mean=3.95, SD=6.79), but increased at 18 months (Mean=9.89, SD=19.08) and 24 months (Mean=10.33, SD=18.87).
Figure 2.
Decreasing change class by treatment condition
Table 3.
Percent days of drug and alcohol use (except tobacco) in the past 90 days as reported in Form 90
| Total | EBFT | CRA | MI | |||||
|---|---|---|---|---|---|---|---|---|
| N | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Class 1: Decreasing |
||||||||
| Baseline | 136 | 25.27 (23.11) | 36 | 23.94 (22.77) | 50 | 25.50 (21.08) | 50 | 26.01 (25.59) |
| 3 months | 107 | 17.72 (27.56) | 31 | 12.84 (20.01) | 37 | 20.23 (32.43) | 39 | 19.22 (27.89) |
| 6 months | 94 | 14.32 (21.27) | 28 | 13.23 (21.23) | 35 | 14.54 (17.91) | 31 | 15.06 (25.14) |
| 9 months | 92 | 9.05 (13.42) | 29 | 10.66 (13.82) | 32 | 8.79 (13.66) | 31 | 7.81 (13.07) |
| 12 months | 96 | 8.59 (12.94) | 33 | 9.74 (14.35) | 32 | 11.89 (14.89) | 31 | 3.95 (6.79) |
| 18 months | 99 | 7.29 (14.39) | 32 | 6.94 (13.28) | 33 | 4.95 (8.68) | 34 | 9.89 (19.08) |
| 24 months | 93 | 10.09 (16.03) | 24 | 7.18 (10.21) | 32 | 11.99 (16.16) | 37 | 10.33 (18.87) |
| Class 2: Fluctuating high user | ||||||||
| Baseline | 24 | 64.69 (34.66) | 15 | 64.81 (34.75) | 4 | 39.67 (40.94) | 5 | 84.34 (17.74) |
| 3 months | 17 | 52.0 (39.76) | 11 | 42.21 (41.28) | 3 | 73.25 (26.33) | 3 | 66.65 (43.67) |
| 6 months | 11 | 61.45 (35.98) | 7 | 63.13 (37.90) | 2 | 84.12 (22.46) | 2 | 32.92 (33.84) |
| 9 months | 17 | 79.23 (29.87) | 11 | 84.51 (23.46) | 3 | 46.98 (48.68) | 3 | 92.16 (7.14) |
| 12 months | 17 | 85.33 (23.45) | 10 | 77.61 (27.47) | 3 | 100.00 (.00) | 4 | 93.61 (12.78) |
| 18 months | 14 | 84.76 (28.31) | 8 | 74.86 (34.92) | 3 | 95.89 (3.71) | 3 | 100.00 (.00) |
| 24 months | 16 | 67.88 (40.21) | 9 | 66.13 (42.34) | 3 | 51.28 (50.05) | 4 | 84.26 (31.48) |
| Class 3: U Shaped |
||||||||
| Baseline | 19 | 33.54 (33.05) | 6 | 38.28 (37.91) | 7 | 25.23 (33.61) | 6 | 38.49 (31.41) |
| 3 months | 14 | 19.18 (34.44) | 6 | 21.95 (38.42) | 5 | 21.42 (43.16) | 3 | 9.94 (11.47) |
| 6 months | 15 | 13.61 (25.82) | 6 | 11.21 (13.21) | 5 | 3.44 (3.15) | 4 | 29.93 (47.63) |
| 9 months | 17 | 10.62 (16.95) | 6 | 18.36 (19.23) | 6 | 2.64 (3.19) | 5 | 10.90 (22.10) |
| 12 months | 12 | 17.21 (19.01) | 3 | 11.79 (13.95) | 5 | 9.59 (12.42) | 4 | 30.77 (24.87) |
| 18 months | 15 | 56.01 (35.95) | 5 | 77.23 (31.29) | 5 | 36.14 (31.10) | 5 | 54.66 (38.98) |
| 24 months | 17 | 92.35 (17.36) | 6 | 90.69 (22.52) | 6 | 88.89 (19.83) | 5 | 98.49 (3.38) |
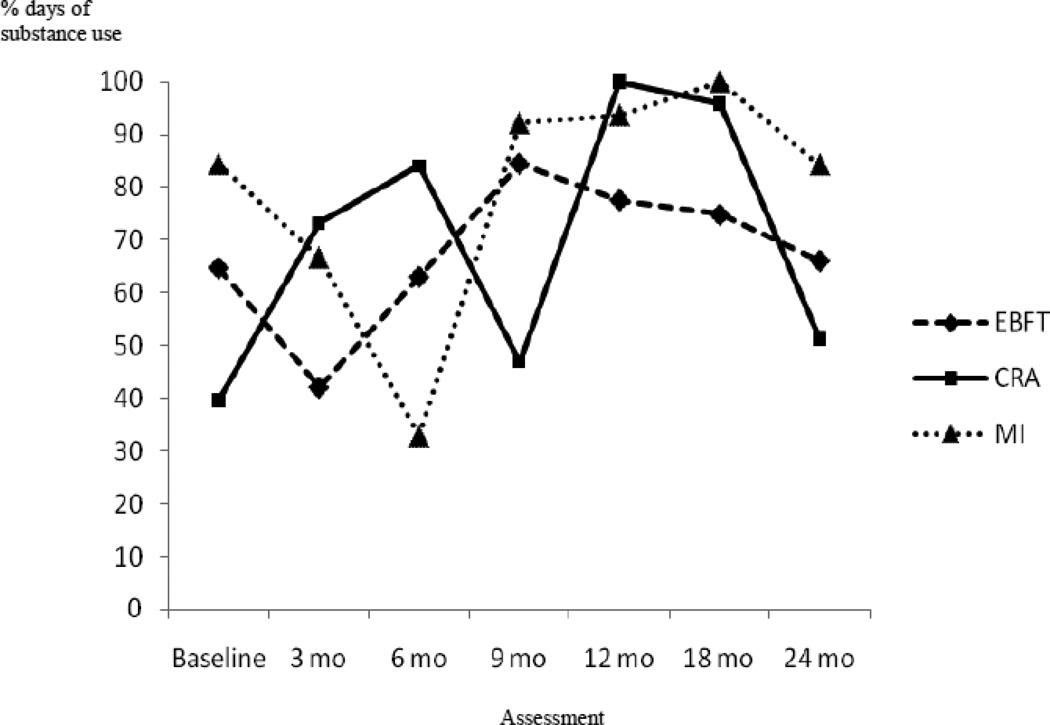
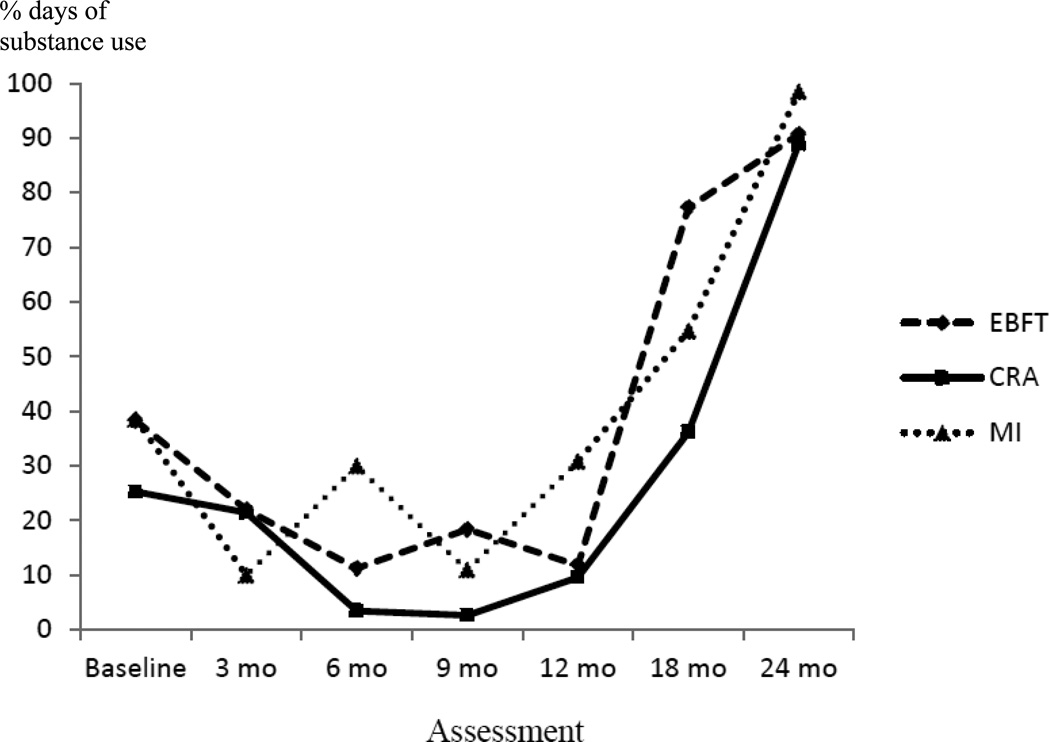
The second group was smaller in size (n= 24, 13.4%). Despite, some patterns of increase and decrease over time, youth in that group showed high levels of substance use. Therefore, this group was labeled as “Fluctuating high users” (Figure 3). Finally, a third group with an even smaller size (n=19, 10.6%) was identified. Adolescents in this change group showed a steep decrease and then a sharp increase in their substance use at follow ups (Table 3) and this group was called “U shaped” (Figure 4).
Figure 3.
Fluctuating high user change class by treatment condition
Figure 4.
U Shaped change class by treatment condition
These findings suggest that not all participants changed their use of substances in the same way over the course of the study. Although the sample was fairly small, it appears that there were three different change trajectories. The relationship between change class membership and treatment condition was explored further with a follow up analysis.
Comparative analyses: One-Way ANOVA
Intercepts, slopes and quadratic terms of each treatment condition was compared within each change class. In this analysis, intercepts referred to the baseline substance use, slopes indicated the rate of change in substance use across time and quadratic terms revealed potential relapse of substance use at the follow-ups (i.e., increase in frequency of use). It was found that in the “Decreasing” change class, the one-way ANOVA was significant for the slope [F(2,133)=4.14, p <.05] (Table 4). Post hoc analysis using Tukey’s indicated that the slope (all negative) for MI was significantly different than the slope for EBFT. That is, those in the MI showed a quicker decline in their substance use than those in EBFT. In addition, the quadratic term was significant in the ANOVA [F(2,133)=4.28, p <.05], indicating that relapse rates differed among treatment conditions. Tukey’s suggested that adolescents in MI condition relapsed sooner than the adolescents in the EBFT condition.
Table 4.
Comparison of mean intercept, mean slope, and mean quadratic terms for the three change classes among the treatment groups.
| Treatment Group | ||||
|---|---|---|---|---|
| EBFT | CRA | MI | ||
| Mean (SD) | Mean (SD) | Mean (SD) | Test statistic | |
| Change class | ||||
| Class 1: Decreasing | ||||
| Intercept | 23.26 (11.55) | 25.85 (12.43) | 27.25 (13.54) | F (2,133) = 1.5 |
| Slope | −6.23 (4.70) | −8.11 (6.54) | −9.92 (5.97)† | F (2,133) = 4.14* |
| Quadratic | .65 (.78) | 1.04 (1.09) | 1.26 (.94)† | F (2,133) = 4.28* |
| Class 2: Fluctuating high user | ||||
| Intercept | 57.99 (15.97) | 37.98 (24.88) | 75.17 (10.46)‡ | F (2,21) = 5.49* |
| Slope | 9.77 (10.11) | 18.53 (11.32) | 1.95 (7.88) | F (2,21) = 3.11 |
| Quadratic | −1.34 (1.65) | −1.96 (1.83) | .12 (1.52) | F (2,21) = 2.06 |
| Class 3: U shaped | ||||
| Intercept | 38.33 (17.91) | 29.83 (13.71) | 38.55 (15.62) | F (2,16) = .53 |
| Slope | −24.46 (4.02) | −21.28 (9.99) | −22.88 (5.95) | F (2,16) = .74 |
| Quadratic | 5.69 (.82) | 4.55 (1.81) | 5.24 (1.37) | F (2,16) = .34 |
Note: Intercept: Substance use at baseline; Slope: Rate of change in substance use over time; Quadratic: Potential relapse in substance use at post-treatment.
p < .05
MI and EBFT are different at p < .05.
MI and CRA are different at p < .05.
The one-way ANOVAs for the “Fluctuating high users” group were not significant for slopes [F (2,21) = 3.11, p >.05], or quadratic terms [F (2,21) = 2.06, p >.05]. Thus, treatment groups did not differ in their rate of change and relapse in the “Fluctuating high users” group (Table 4). However, it was found that intercepts of CRA and MI were different in this change class [F (2,21) = 5.59, p <.05]. Adolescents in the CRA condition were using substances significantly less than those in the MI condition at baseline..Finally, the one-way ANOVA for the “U shaped” change class was non-significant for the intercepts, slopes and quadratic terms.
Discussion
This trial compared the response of shelter-recruited adolescent runaways randomly assigned to one of three empirically-supported, but theoretically distinct interventions: family systems-based EBFT, operant-based CRA, and non-directive, motivation focused MI. Overall, the three treatments performed similarly with the majority of adolescents showing a significant decrease in substance use in all three treatment groups with a slight increase at post-treatment. However, not all participants in the treatments changed in the same way, and change was not linear. In addition to the group that revealed a decreasing pattern with a slight increase at follow up, two small groups (Fluctuating high users and U shaped) were identified. These findings are consonant with research suggesting that even if a treatment has been shown to be effective on average, one treatment is not effective for everyone as there is heterogeneity of treatment response and a variable course of substance use (Murphy, Lynch, Oslin, & TenHave, 2007).
Research objective 1: Treatment outcomes
It was hypothesized that frequency of drug and alcohol use among runaways would be reduced over time in all treatment conditions (main effect of time). Those assigned to EBFT were expected to show greater reductions over time than those assigned to CRA and MI (main effect of treatment). In summary, study hypotheses were partially met. As expected, adolescents showed improvement in their substance use over time. However, the family therapy condition (EBFT) did not outperform MI or CRA, and all treatment conditions showed reductions in substance use.
Other studies have similarly shown little difference between conditions when comparing family systems therapy (Multidimensional Family Therapy, Liddle, 2002), adolescent CRA (Godley et al., 2001), and MET/CBT12 (Sampl & Kadden, 2001) (Dennis et al., 2004). Dennis and colleagues (2004) suggested that the similarity in findings could be explained by factors common to all treatments such as therapeutic alliance or other shared factors such as juvenile justice monitoring. In the current study, it cannot be ruled out that the decrease in substance use might be related to factors common to all treatments (e.g., therapeutic alliance), shelter involvement, regression toward the mean, or to specific skills learned in the HIV prevention sessions which included assertiveness training and role play practice.
Of interest is that minority adolescents showed significantly more reductions in substance use than White adolescents across treatments, but also a quicker relapse, or increase in substance use. Cooper et al. (2010) notes that more information is available on treatment retention than outcomes among African Americans, with data suggesting that African Americans are less likely to be retained in substance abuse treatment than Whites (McCaul, Svikis, & Moore, 2001), possibly because of distrust of social services and unfavorable views of treatment (Aponte & Barnes, 1995). Among adolescents, one study showed no differences in substance use outcomes between African American and other racial groups (Rounds-Bryant & Staab, 2001). However, among adults, Moos, Moos, and Finney (2001) reported that African American men were 1.58 times more likely to deteriorate post-treatment compared to other racial groups. Research suggests that compared to White adolescents, African American adolescents experience greater contextual risk factors for substance use (economic deprivation, neighborhood disorganization, availability of drugs) (Wallace & Muroff, 2002) exposure to which could explain the higher relapse or deterioration rates post-treatment.
Research objective 2: Exploring change classes across treatment conditions
Variability in individual patterns of change among substance abusing adolescents was explored. It was hypothesized that the majority of the adolescents who showed a consistent change pattern (i.e., linear) would be in the EBFT and CRA groups, rather than in MI. Interestingly, there were differences in the trajectories of change among treatment conditions. The majority of adolescents decreased their substance use (76%) up to two years, and variability in outcomes was observed. A small number of adolescents (10.6%) increased their use by two years post-baseline and another small number of adolescents (13.4%) showed a high amount of substance use with some patterns of increase and decrease by two years. Among those in the decreasing group, those assigned to EBFT showed more consistent change maintaining reductions at 18 months, while those assigned to MI, overall, showed a faster rate of decrease in substance use but a quicker relapse. These findings indicate differences between the MI condition and other treatment approaches in the study. One consideration is MI is a brief intervention that focuses primarily on motivation to change substance use whereas EBFT (and CRA) offer longer treatment and address other ecological issues associated with risk and protection of substance use (e.g., family communication and interaction patterns, alternative reinforcing activities). Future research will need to confirm whether more intensive treatment, to a certain minimum dose, which also addresses multiple ecological risk and protective factors is associated with a longer duration of its effects.
Substance abuse researchers have recently proposed adaptive treatment designs to more effectively manage the heterogeneity of treatment response and potentially reduce treatment failure (Murphy, Lynch, Oslin, & TenHave, 2007). Adaptive treatment strategies operationalize the clinical practice of adapting and re-evaluating treatment options based on patient progress, however, formal trials evaluating this approach are lacking (Murphy et al., 2007). This may be a promising direction in future research that seeks to reduce treatment failure.
Limitations
A treatment as usual control condition was not utilized in this study. Two prior stage 1b randomized trials (Slesnick & Prestopnik, 2005; 2009) showed that EBFT was more effective than treatment as usual (services provided by the shelter) at reducing substance use among adolescents. Therefore, consistent with Rounsaville, Carroll and Onken’s (2005) recommendations for stage 2 clinical trials, viable, empirically-supported comparison conditions were utilized. Also, the sample size was relatively small, reducing the power to detect potential differences among treatment conditions and change classes. As this was a sample of convenience through the only runaway shelter in a large Midwestern city, the findings might not generalize to other cities whose population of runaways may vary in substance use severity, race, socioeconomic status and other sociocultural factors.
An additional consideration is that, on average, participants completed less than 50% of the available sessions. However, given that this sample did not include adolescents or families seeking or requesting substance abuse treatment, were not court-ordered to treatment and their treatment was not tracked by the juvenile justice system or child protective services, the retention rates were considered to be reasonable in comparison to other trials that seek to engage non-treatment seeking, residentially unstable, substance abusing populations. For example, Meyers, Miller, Hill and Tonigan (1999) reported that 64% of their initially unmotivated drug users completed 5 or more sessions, which compares to the 60% found in this sample. However, it is unknown whether receiving 43% of the intended dose across treatments is adequate for maximal change.
The necessary “dose” of treatment to facilitate change is unknown. Several studies indicate that the majority of psychotherapy clients complete approximately six sessions, and that clinically significant change usually occurs early in treatment. Baldwin et al. (2009) examined the relationship between significant change and total dose among 4676 psychotherapy patients who received individual psychotherapy. The average treatment attendance was 6.46 sessions (range = 3–29) and there was no relationship between treatment dose and clinically significant improvement after session 8. Snell et al. (2001) also assessed the relationship between treatment dosage and clinically significant change. Clients (n = 106) at a university counseling clinic completed a mean of 6.4 sessions, and those clients that attended only one session achieved and maintained clinically significant change through the 10-month follow-up at a higher rate than those that completed between 2–7 sessions. Finally, Barkham (2006) examined dose and outcomes among 1868 clients offered up to 12 psychotherapy sessions. The majority of clients attended between 2 to 6 sessions, and those that attended fewer sessions showed more clinically significant change than those that attended more sessions. The authors suggested that the easier to treat clients respond more quickly to treatment and the more difficult to treat clients remain in therapy. Some have argued that the quality of treatment participation, rather than the number of sessions attended, may be a more useful factor for understanding therapeutic change (Hien et al., 2012). Much more work is needed to examine the necessary dosage of each of the interventions examined in this study for initiating change with this population. Improving treatment engagement and retention of this traditionally ‘difficult to engage’ (Ensign & Bell, 2004) population is an important focus, and might include contingency management procedures or other reinforcement-based processes. It is unknown whether the observed findings from this study might improve, remain the same, or deteriorate if more participants in all treatments completed the total available sessions.
In addition, EBFT and CRA fidelity ratings were in the “average” range whereas MI was in the “well” range. However, the small sample size limited the ability to perform analyses of potential therapist effects and the relationship between treatment adherence, therapist competence and treatment outcomes. Future research with a fully powered sample should investigate possible therapist effects and differences in each treatment condition.
Clinical Implications
The majority of randomized clinical trials of substance abuse treatment include treatment seeking samples. Among adolescents, usually the parent initiates treatment for the adolescent (Nock & Kazdin, 2005), with several studies identifying adolescents as having low levels of motivation to change (Battjes et al., 2003; Pelkonen, Marttunen, Laippala, & Loennqvist, 2000), including among runaway adolescents (Slesnick et al., 2009). Anecdotally, in this study, adolescents were easier to engage than their primary caregivers, who were often frustrated with their child and the system of care. While only 12% of the EBFT sample versus 26% of the CRA and 34% of the MI samples attended no therapy sessions, there were no overall differences in the total proportion of sessions attended. Family therapy studies often report that family therapy is associated with a greater engagement in treatment compared to individual therapies (Liddle, 2004) possibly because engagement of primary caregivers in the treatment also serves to reinforce adolescent involvement. However, when compared to other manualized and well-designed alternative treatments, few differences in overall treatment retention are found (Hogue & Liddle, 2009), similar to that found this study. Therefore, while family therapy is more effective at engaging clients in treatment, retention was similar across treatment conditions.
This sample of non-treatment seeking, substance abusing adolescents responded positively to treatment, lending support to EBFT, CRA and MI as potentially viable treatment options for these difficult to engage adolescents. MI showed a quicker decline in substance use but also a quicker relapse, so the intervention and its impact on substance use was significantly more brief than the other interventions. Future cost-effectiveness and cost-benefit studies are needed to determine which intervention is more favorable. That is, CRA and EBFT require more training, more sessions, and therefore more resources, but in this study, appeared to result in longer-term substance use reductions whereas MI requires less training, fewer sessions, shows a quicker decline in substance use but also a quicker relapse. Additionally, noninferiority and equivalence designs are needed to answer the question whether the three treatments perform equally well (Greene, Morland, Durkalski, & Frueh, 2008).
And finally, these findings have some implications for youth serving agencies such as runaway shelters. Generally, these programs seek to use those interventions that have the most positive impact on the youth they serve (Walsh & Donaldson, 2010). Identifying ‘best practices’ and providing intervention options for agencies allows them the flexibility to choose treatments that may be better matched (theoretically, training needs) to the agency and its staff, easing adoption and implementation into community practice.
Conclusions and Future Directions
Without using a latent trajectory analysis to analyze the change patterns in the sample, the treatment conditions would have looked the same. By recognizing that not everyone changes in the same way, individual differences in change were able to be explored. For example, in this study, those assigned to EBFT appeared to evidence more consistent change, at least for the largest change class. On the other hand, those in MI showed reductions in their substance use quicker than those in EBFT, but revealed a quicker relapse in substance use. For 10.6% of the adolescents, frequency of substance use increased past baseline levels at two years. As early substance use predicts continued substance use, and substance use generally increases during adolescence (SAMHSA, 2006), it is possible that these interventions served to prevent worsening substance use among some adolescents. Future strategies to prevent treatment failure might include a stepped care approach which advocates for beginning with a minimally intensive, but effective therapy, such as MI, and transitioning to more intensive therapy or other types of therapy only if indicated (Sobell & Sobell, 2000). Other strategies include addressing acute problems, such as an increase in substance use, as they arise and then returning to maintenance therapy once acute problems are resolved (McKay et al., 2004). The treatments in this study were brief, from 4–14 sessions, with no booster sessions. For some adolescents, this may have been sufficient, but others may have benefited from additional treatment. Overall, however, the findings offer preliminary support for these three treatment options for use by service providers who seek to intervene in the lives of substance abusing runaway adolescents.
Acknowledgments
This work has been supported by NIDA grant # R01 DA016603.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Arlington, VA: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Aponte JF, Barnes JM. Impact of acculturation and moderator variables on the intervention and treatment of ethnic groups. In: Aponte JF, River RY, Wohl J, editors. Psychological Interventions and Cultural Diversity. Boston: Allyn & Bacon; 1995. pp. 19–39. [Google Scholar]
- Baker A, Turner A, Kay-Lambkin FJ, Lewin TJ. The long and the short of treatments of alcohol or cannabis misuse among people with severe mental disorders. Addictive Behaviors. 2009;34:852–858. doi: 10.1016/j.addbeh.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Bonsack C, Manetti SG, Favord J, Montagrin Y, Besson J, Bovet P, Conus P. Motivational intervention to reduce cannibus use in young people with psychosis: A randomized controlled trial. Psychotherapy and Psychosomatics. 2011;80:287–297. doi: 10.1159/000323466. [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Berkeljon A, Atkins DC, Olson JA, Nielsen SL. Rates of change in naturalistic psychotherapy: Contrasting dose-effect and good-enough level models of change. Journal of Consulting and Clinical Psychology. 2009;77:203–211. doi: 10.1037/a0015235. [DOI] [PubMed] [Google Scholar]
- Battjes RJ, Gordon MS, O’Grady KE, Kinlock TW, Carswell MA. Factors that predict adolescent motivation for substance abuse treatment. Journal of Substance Abuse Treatment. 2003;24:221–232. doi: 10.1016/s0740-5472(03)00022-9. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: A quality of evidence review. Journal of Consulting and Clinical Psychology. 2008;76:531–544. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge: Harvard University Press; 1979. [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Chamberlain C, MacKenzie D. Youth Homelessness: Four Policy Proposals. Australian Housing and Urban Research Institute. 2004 Final Report. [Google Scholar]
- Chung TA, Maisto SA. Relapse to alcohol and other drug use in treated adolescents: Review and reconsideration of relapse as a change point in clinical course. Clinical Psychology Review. 2006;26:149–161. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Cooper EF. The runaway and homeless youth program: Administration, funding, and legislative actions. 2006 Mar 23; CRS Report for Congress. Retrieved August 15, 2011, from http://opencrs.cdt.org/rpts/RL31933_20060323.pdf.
- Cooper RL, MacMaster S, Rasch R. Racial differences in retention in residential substance abuse treatment: The impact on African American men. Research on Social Work Practice. 2010;20:183–190. [Google Scholar]
- Cornelius JB, St. Lawrence JS. Receptivity of African American adolescents to an HIV-prevention curriculum enhanced by text messaging. Journal of Specialists in Pediatric Nursing. 2009;14:123–131. doi: 10.1111/j.1744-6155.2009.00185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FF, Babor T, Donaldson J, Funk R. The cannabis youth treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Ensign J, Bell M. Illness experiences of homeless youth. Qualitative Health Research. 2004;14:1239–1254. doi: 10.1177/1049732304268795. [DOI] [PubMed] [Google Scholar]
- Godley SH, Meyers RJ, Smith JE, Godley MD, Titus JM, Karvinen T, Dent G, Passetti L, Kelberg P. The Adolescent Community Reinforcement Approach for adolescent cannabis users. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and mental Health Services Administration; 2001. [Google Scholar]
- Graham JW, Donaldson SI. Evaluating interventions with differential attrition: The importance of nonresponse mechanisms and use of follow up data. Journal of Applied Psychology. 1993;78:119–128. doi: 10.1037/0021-9010.78.1.119. [DOI] [PubMed] [Google Scholar]
- Greene CJ, Morland LA, Durkalski VL, Frueh BC. Noninferiority and equivalence designs: Issues and implications for mental health research. Journal of Traumatic Stress. 2008;21(5):433–439. doi: 10.1002/jts.20367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen WB, Collins LM, Mallette CK, Johnson CA, Fielding JE. Attrition in prevention research. Journal of Behavioral Medicine. 1985;8:261–275. doi: 10.1007/BF00870313. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Borduin CM. Multisystemic treatment of serious juvenile offenders and their families. In: Scwartz IM, AuClaire P, editors. Home-based services for troubled children. Lincoln: University of Nebraska Press; 1995. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to define meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national results on adolescent drug use. Overview of key findings. U.S: Department of Health and Human Services; 2008. 2008. [Google Scholar]
- Kaminer Y, Burleson JA. Psychotherapies for adolescent substance abusers: 15-month follow-up of a pilot study. American Journal on Addictions. 1999;8:114–119. doi: 10.1080/105504999305910. [DOI] [PubMed] [Google Scholar]
- Kay-Lambkin FJ, Baker AL, Lewin TJ, Carr VJ. Computer-based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: A randomized controlled trial of clinical efficacy. Addiction. 2009;104:378–388. doi: 10.1111/j.1360-0443.2008.02444.x. [DOI] [PubMed] [Google Scholar]
- Lennox R, Dennis ML, Scott CK, Funk RR. Combining psychometric and biometric measures of substance use. Drug and Alcohol Dependence. 2006;83(2):95–103. doi: 10.1016/j.drugalcdep.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle HA. Multidimensional Family Therapy (MDFT) for adolescent cannabis users. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and mental Health Services Administration; 2002. [Google Scholar]
- Liddle HA. Family-based therapies for adolescent alcohol and drug use: research contributions and future research needs. Addiction. 2004;99:76–92. doi: 10.1111/j.1360-0443.2004.00856.x. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug and Alcohol Abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- Lifson AR, Halcon LL. Substance abuse and high risk drug and needle-related behaviors among homeless youth in Minneapolis: Implications for prevention. Journal of Urban Health. 2001;78(4):690–698. doi: 10.1093/jurban/78.4.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey EW, Kurtz D, Jarvis S, Williams NR, Nackerud L. How runaways and homeless youth navigate troubled waters: Personal strengths and resources. Child and Adolescent Social Work Journal. 2000;17:115–140. [Google Scholar]
- Lutz W, Martinovich Z, Howard KI. Patient profiling: An application of random coefficient regression models to depicting the response of a patient to outpatient psychotherapy. Journal of Consulting and Clinical Psychology. 1999;67(4):571–577. doi: 10.1037//0022-006x.67.4.571. [DOI] [PubMed] [Google Scholar]
- McCaul ME, Svikis DS, Moore RD. Predictors of outpatient treatment retention: Patient versus substance use characteristics. Drug & Alcohol Dependence. 2001;62:9–17. doi: 10.1016/s0376-8716(00)00155-1. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, Pettinati HM. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. Journal of Consulting and Clinical Psychology. 2004;72(6):967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- McKinney-Vento Homeless Assistance Act, Re-Authorized. 2002;42 U.S.C. 11431 et seq 725. [Google Scholar]
- Meyers RJ, Miller WR, Hill DE, Tonigan JS. Community Reinforcement and Family Training (CRAFT): Engaging unmotivated drug users in treatment. Journal of Substance Abuse. 1999;10(3):291–308. doi: 10.1016/s0899-3289(99)00003-6. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Smith JE. Clinical guide to alcohol treatment: The Community Reinforcement Approach. New York: Guilford Press; 1995. [Google Scholar]
- Miller WR. Project MATCH Monograph Series. Vol. 5. U.S. Dept. of Health: Bethesda, MD; 1996. Form 90 a structured assessment interview for drinking and related problem behaviors. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- Moos RH, Moos BS, Finney JW. Predictors of deterioration among patients with substance-use disorders. Journal of Clinical Psychology. 2001;57:1403–1419. doi: 10.1002/jclp.1105. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Lynch KG, McKay JR, Oslin D, TenHave T. Developing adaptive treatment strategies in substance abuse research. Drug and Alcohol Dependence. 2007;88(2):24–30. doi: 10.1016/j.drugalcdep.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide: Statistical analysis with latent variables. Sixth edition. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Nock MK, Kazdin AE. Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology. 2005;73:872–879. doi: 10.1037/0022-006X.73.5.872. [DOI] [PubMed] [Google Scholar]
- Pelkonen M, Marttunen M, Laippala P, Loennqvist J. Factors associated with early dropout from adolescent psychiatric outpatient treatment. Journal of the American Academy of Child Adolescent Psychiatry. 2000;39:329–336. doi: 10.1097/00004583-200003000-00015. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 6 for Windows. Lincolnwood, IL: Scientific Software International, Inc; 2004. Computer software. [Google Scholar]
- Robertson MJ, Toro PA. Homeless youth: Research, intervention, and policy. In: Fosburg LB, Dennis DB, editors. Practical lessons: The 1998 national symposium on homelessness research. Washington, DC: U.S. Department of Housing and Urban Development; 1999. pp. 3-1–3-32. [Google Scholar]
- Rohr ME, James R. Runaways: Some suggestions for prevention, coordinating services, and expediting the reentry process. The School Counselor. 1994;42:40–47. [Google Scholar]
- Rotheram-Borus MJ, Koopman C, Haignere C, Davies M. Reducing HIV sexual risk behaviors among runaway adolescents. Journal of the American Medical Association. 1991;266:1237–1241. [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Song J, Gwadz M, Lee M, Van Rossem R, Koopman C. Reductions in HIV risk among runaway youth. Prevention Science. 2003;4:173–187. doi: 10.1023/a:1024697706033. [DOI] [PubMed] [Google Scholar]
- Rounds-Bryant JL, Staab J. Patient characteristics and treatment outcomes for African American, Hispanic, and White adolescents in DATOS-A. Journal of Adolescent Research. 2001;16:624–641. [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8:133–142. [Google Scholar]
- Sampl S, Kadden R. Motivational Enhancement Therapy and Cognitive Behavioral Therapy (MET-CBT-5) for adolescent cannabis users. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and mental Health Services Administration; 2001. [Google Scholar]
- Shaffer D. The Diagnostic Interview Schedule for Children −2.3 Version. New York: Columbia University; 1992. [Google Scholar]
- Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Archives of General Psychiatry. 2002;59(6):538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Slesnick N. Treatment manual: Ecologically-Based Family Therapy for substance abusing runaway youth. 2000 doi: 10.1016/j.adolescence.2005.02.008. Unpublished manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Dashora P, Letcher A, Erdem G, Serovich JM. A review of interventions for runaway and homeless youth: Moving forward. Children and Youth Services Review. 2009;31:732–742. doi: 10.1016/j.childyouth.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik JL. Ecologically-based family therapy outcome with substance abusing runaway adolescents. Journal of Adolescence. 2005;28:277–298. doi: 10.1016/j.adolescence.2005.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik J. Comparison of family therapy outcome with alcohol abusing, runaway adolescents. Journal of Marital and Family Therapy. 2009;35:255–277. doi: 10.1111/j.1752-0606.2009.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik JL, Meyers RJ, Glassman M. Treatment outcome for homeless, street-living youth. Addictive Behaviors. 2007;32:1237–1251. doi: 10.1016/j.addbeh.2006.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell M, Sobell L. Stepped care as a heuristic approach to the treatment of alcohol problems. Journal of Consulting and Clinical Psychology. 2000;68(4):573–579. [PubMed] [Google Scholar]
- SPSS Inc. SPSS, Version 17. Chicago, IL, USA: 2008. [Google Scholar]
- St. Lawrence JS, Jefferson KW, O’Bannon RE, Shirley A. Cognitive-behavioral intervention to reduce African American adolescents’ risk for HIV infection. Journal of consulting and Clinical Psychology. 1995;63:221–237. doi: 10.1037//0022-006x.63.2.221. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The DASIS Report: Adolescent Treatment Admissions: 1992 and 2002. Office of Applied Studies. 2004 Retrieved September 1, 2011, from http://www.oas.samhsa.gov/2k4/youthTX/youthTX.pdf.
- Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06–4194; 2006. [Google Scholar]
- Teare JF, Furst D, Peterson RW, Authier K. Family reunification following shelter placement: Child, family and program correlates. American Journal of Orthopsychiatry. 1992;62(1):142–146. doi: 10.1037/h0079314. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Howard MO. Adolescent substance abuse treatment: A synthesis of controlled evaluations. Research on Social Work Practice. 2004;14(5):325–335. [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child & Adolescent Psychology. 2008;37:238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Wallace JM, Muroff JR. Preventing substance abuse among African American children and youth: Race differences in risk factor exposure and vulnerability. The Journal of Primary Prevention. 2002;22(3):235–261. [Google Scholar]
- Walsh SM, Donaldson RE. National safe place: Meeting the immediate needs of runaway and homeless youth. Journal of Youth and Adolescence. 2010;39(5):437–445. doi: 10.1007/s10964-010-9522-9. [DOI] [PubMed] [Google Scholar]
- WHO Brief Intervention Study Group. A cross-national trial of brief interventions with heavy drinkers. American Journal of Public Health. 1996;86(7):948–955. doi: 10.2105/ajph.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]