Abstract
The purpose of this study was to examine relationships between neurocognition, theory of mind, and community functioning in a sample of 43 outpatients with serious mental illness (SMI). Relationships between baseline values and changes over time were analyzed using multilevel modeling. Results showed that: 1. Neurocognition and theory of mind were each associated with community functioning at baseline. 2. Community functioning improved over approximately 12 months of treatment. 3. Greater improvement in neurocognition over time predicted higher rates of improvement in community functioning. 4. Theory of mind did not predict change in community functioning after controlling for neurocognition. 5. The effect of change in neurocognition on community functioning did not depend on the effect of baseline neurocognition. This study provides empirical support that individuals with SMI may experience improvement in community functioning, especially when they also experience improvement in neurocognition. Limitations and recommendations for future research are discussed.
Keywords: multilevel modeling, cognitive remediation, psychiatric rehabilitation
Introduction
Cognitive impairments are highly prevalent in people with serious mental illness (SMI; Combs and Mueser, 2007).1 For heuristic purposes, these impairments are described as falling within the domains of neurocognition and social cognition. Neurocognition includes basic information processing functions as assessed by neuropsychological methods (e.g. attention, memory, concept formation and executive processes; Spaulding et al., 2003). Social cognition pertains to the “processes and functions that allow a person to understand, act on, and benefit from the interpersonal world” (Corrigan and Penn, 2001, p. 3). Domains of social cognition that have been a focus of research include emotion perception, social perception and knowledge, attributional bias (Addington et al., 2010), and theory of mind (Couture et al., 2006).
An extensive body of research has linked neurocognition and social cognition to functional outcomes in those with SMI (Couture et al., 2006; Green et al., 2000; Wykes et al., 2011). In this context, “functional outcomes” refer to behavior and social role performance necessary for normal everyday functioning. Neurocognition has been estimated to explain up to 60% of the variance in outcomes such as social problem solving, community functioning, and skill acquisition during psychiatric rehabilitation (Green et al., 2000). Domains of social cognition have also been found to be related to community, social, and work functioning (Couture et al., 2006; Mancuso et al., 2011). Many studies have demonstrated that social cognition accounts for additional variance in sociobehavioral outcomes after controlling for neurocognition (Brekke et al., 2007; Meyer and Kurtz, 2009; Pinkham and Penn, 2006; Roncone et al., 2002). Still, it remains unclear to what extent various findings reflect unique contributions from truly separate cognitive domains, or whether they all reflect a common global cognitive impairment, measured by instruments of variable reliability and construct validity.
A decade-long proliferation of neuropsychological and social cognitive assessment tools has improved our ability to analyze relationships between separate cognitive domains and functional outcomes. In addition, new quantitative methods for analyzing longitudinal change are playing an increasingly important role (see Green et al., 2004 for a review). As was anticipated early in the contemporary era of schizophrenia research (Cromwell and Spaulding, 1978; Nuechterlein and Dawson, 1984), some cognitive impairments are quite static, while others change over time, at least under certain conditions. Understanding relationships between change trajectories may be as important as understanding cross-sectional relationships between domains of functioning (Brekke et al., 2007; Peer et al., 2007).
There are several limitations to the extant longitudinal research in SMI. Green and colleagues (2004) identified only two of eighteen longitudinal studies that evaluated the relationship between changes in cognitive functioning and functional outcomes, both focusing on cognitive decline rather than improvement. Additionally, despite promising findings on links between cognitive and functional outcomes (Wykes et al., 2007a; Wykes et al., 2007b), less than a third of the published studies include functional outcome measures (Twamley et al., 2003). Of the studies that have examined changes in cognitive functioning and functional outcomes (e.g., Reeder et al., 2004; 2006), the applied analytical strategies may not be equipped to address the nuances of longitudinal change. Furthermore, most studies of change have been conducted in a prognostic time frame, over a year or more. There is accumulating evidence, from studies of treatments that directly target cognitive impairments, that functional changes can occur in a much shorter time frame (Roder et al., 2006; Twamley et al., 2003). A more complete understanding of these changes and their functional outcomes will inform design of psychosocial treatment and rehabilitation, and enhance individualization of clinical decision making.
Another inhibiting factor in longitudinal research is the instability, unreliability and problematic interpretability of change between two time points (Singer and Willett, 2003). Currently, research on cognitive change and functional outcomes in SMI is mostly limited to two time points (e.g., Brekke et al., 2005; Fujii and Wylie, 2002; Kee et al., 2003; Kurtz et al., 2008). Addition of a third assessment point is a strong solution, but this has greater requirements for laboratory resources, stability in the treatment setting and continuous access to the subject population. Application of new analytic methods requires special investment in continuous data collection capabilities (e.g., protocols that create multivariate databases in the course of routine treatment and rehabilitation). In this study, resources for obtaining 3 assessments are prioritized over maximizing the sample size with only 2 assessments, reflecting prioritized interest in providing a more reliable account of longitudinal change.
The present study was an analysis of cross-sectional and longitudinal relationships between neurocognitive and theory of mind impairments, and functional outcomes in people with SMI, over the course of 12 months of individualized treatment, rehabilitation and support services. The 12-month time period included three assessment points. Drawing upon the findings of a previous longitudinal study of an outpatient SMI sample undergoing psychiatric rehabilitation (Brekke et al., 2007), it was hypothesized that:
Better baseline neurocognition and theory of mind would be associated with higher levels of initial community functioning.
Community functioning would improve on average over time.
Higher rates of change in community functioning would be predicted by both higher baseline neurocognition on average and greater improvement in neurocognitive functioning.
Better baseline theory of mind on average and greater improvement in theory of mind over time would predict additional variance in community functioning after controlling for neurocognition.
The effect of change in neurocognition and theory of mind would depend upon baseline neurocognition and theory of mind.
Methods
Participants
The purposive sampling frame was outpatients with SMI receiving services between 2007 and 2009 at two treatment centers in the Midwest. Forty percent of the sample came from treatment center 1 only, 2% from treatment center 2 only, and 58% from both centers. Individual services included case management, medication management, day activities, and rehabilitation classes. All services shared the goal of maximizing functioning necessary for successful community living.
Archival data from 43 outpatients were included in this study. The majority of participants had DSM-IV diagnoses of Schizophrenia or Schizoaffective Disorder (n = 20 and 12, respectively); other diagnoses included Bipolar Disorder (n = 5), Major Depressive Disorder (n = 1), Depressive Disorder NOS (n = 2), Generalized Anxiety Disorder (n = 1), and Intermittent Explosive Disorder (n = 1). One participant had missing diagnostic data; however, in order to be treated at the centers involved in this study, the participant would have had to have met criteria for SMI. Demographic and clinical characteristics of the study participants are summarized in Table 1.
Table 1. Demographic and Clinical Characteristics of the Study Sample (N = 43).
| Variable | n | M | SD |
|---|---|---|---|
| Sex (%) | |||
| Men | 29 (67.4) | - | - |
| Women | 14 (32.6) | - | - |
| Ethnicity (%) | |||
| White | 41 (95.3) | - | - |
| African American | 1 (2.3) | - | - |
| Other | 0 (0.0) | - | - |
| Missing | 1 (2.3) | - | - |
| Age | 43 | 42.16 | 13.08 |
| Education | 42 | 12.88 | 2.19 |
| HT1a | 43 | 15.74 | 3.56 |
| HT2 | 24 | 15.21 | 4.05 |
| HT3 | 18 | 16.72 | 3.33 |
| S-NAB1b | 43 | 441.12 | 68.14 |
| S-NAB2 | 24 | 438.58 | 56.77 |
| S-NAB3 | 18 | 470.28 | 46.91 |
| MCAS1c | 43 | 14.77 | 2.59 |
| MCAS2 | 24 | 15.76d | 2.24 |
| MCAS3 | 18 | 16.62e | 1.62 |
HT = Hinting Task Time 1, 2, and 3.
S-NAB = Neuropsychological Assessment BatteryTotal Time 1, 2, and 3.
MCAS = Multnomah Community Ability Scale Mean Time 1, 2, and 3.
Dash marks (-) indicate data that were not obtained.
Materials and Procedure
Cognition was assessed using the Neuropsychological Assessment Battery Screening Module (S-NAB; Stern and White, 2003) and the Hinting Task (Corcoran et al., 1995). The neurocognitive and theory of mind measures were administered by trained testers who were blind to the research hypotheses. The Multnomah Community Ability Scale (MCAS; Barker et al., 1994), an assessment of community functioning, was completed by treatment center staff who had frequent contact with participants and were also blind to the research hypotheses. MCAS raters were trained by an advanced clinical psychology doctoral student. Scores from the S-NAB and the Hinting Task served as predictors and scores from the MCAS served as outcomes.
Neuropsychological assessment battery – screener (S-NAB)
The S-NAB assesses neurocognitive functioning in individuals between the ages of 18 and 97. It produces five index scores (i.e., attention, language, memory, spatial ability, and executive functioning) and consists of aural and visual stimuli. The S-NAB consists of 2 alternate forms, both of which were used in this study in order to minimize practice effects. In this study, a total score was computed by summing the five index scores (S-NAB). The total scores, as well as the five index scores, were used in the analyses in this study. Higher scores reflect better neuropsychological functioning. The S-NAB possesses good psychometric properties (Wilfred et al., 2005). Cronbach's alpha for total S-NAB scores in this study ranged from .48 (time 3) to .66 (time 2).
The hinting task
The Hinting Task was designed to assess the social cognitive concept, theory of mind, or the ability to infer the intentions of others (Corcoran, 2001). It was used as the sole measure of social cognition in this study because theory of mind has received considerable attention in the literature, as it is known to be deficient in individuals with SMI (Couture et al., 2006). Examinees listen to 10 short stories involving an exchange between two characters, during which one character makes a hint statement. Examinees must explain what was meant by the statement. They receive a score of 2 by answering correctly on the first attempt, 1 by answering correctly on the second attempt, and 0 if they are unable to answer correctly after two attempts. A total score is computed by summing scores on each item. Due to the unavailability of individual item scores, internal reliability estimates could not be calculated from the data used in this study. However, the Hinting Task is a primary assessment of theory of mind in SMI samples and demonstrates acceptable psychometric properties (Corcoran, 2001; Corcoran et al., 1995; Marjoram et al., 2005; Pinkham & Penn, 2006).
Multnomah community ability scale (MCAS)
The MCAS is a clinician-rated instrument that was designed for use in SMI populations to assess community functioning. It consists of 17 items rated on a 5-point scale (1 = extremely impaired to 5 = normal) based on behavioral observations within 4 domains: interference with functioning (e.g., “How impaired are the client's thought processes as evidenced by such symptoms as hallucinations, delusions,…etc.?”), adjustment to living (e.g., “How well does the client perform independently in day-to-day living?”), social competence (e.g., “How frequently does the client initiate social contact or respond to others' initiation of social contact?”), and behavioral problems (e.g., “How frequently does the client abuse drugs and/or alcohol?”). In an attempt to minimize the tendency for staff to base ratings at time points 2 and 3 on ratings made previously, the majority of staff did not have access to their prior ratings. A mean MCAS score was computed by summing the means of each of the subscales. Mean MCAS scores, as well as mean subscale scores, were used in the analyses in this study. The MCAS demonstrates good concurrent validity, and reliability coefficients have been shown to fall within an acceptable range (Hendryx et al., 2001). Cronbach's alpha reliability coefficients in this sample ranged from .83 (time 3) to .92 (time 2).
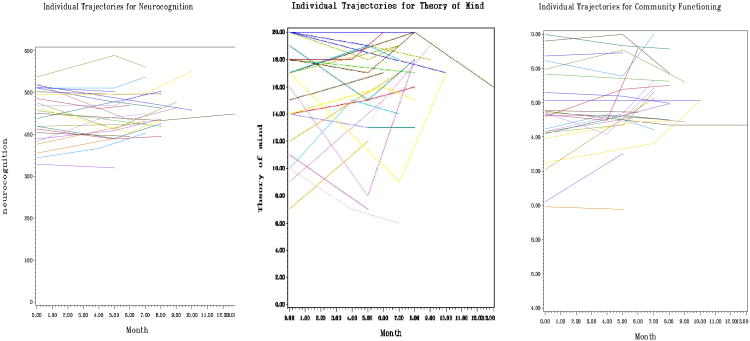
Participants and their associated staff members completed assessments at approximately 3-6 month intervals (see Figure 1 for individual trajectories). Outpatients at treatment center 1 voluntarily participated in routine psychological testing. Results were shared with participants and treatment team members, and informed recommendations to the treatment team regarding how to improve neurocognitive and social cognitive functioning. Participants received no monetary compensation for completing the assessments.
Figure 1. Individual Trajectories for Neurocognition, Theory of Mind, and Community Functioning.
Participants and their associated staff members at treatment center 2 completed the assessments as part of a separate study for which they provided informed consent. Participants were paid $5 for completing assessments at each time point.
Design and Statistical Analysis
This study utilized a naturalistic, single-group, longitudinal design.
In order to assess cross-sectional relationships between neurocognition and community functioning, and between theory of mind and community functioning, Pearson's product-moment correlations were examined between S-NAB total, Hinting Task total, and mean MCAS scores.
Longitudinal relationships between neurocognition, theory of mind, and community functioning were assessed using multilevel modeling (MLM; i.e., hierarchical linear modeling). MLM is a statistical procedure well suited to answer questions about individual change (i.e., level-1 or within-person effect) and group change (i.e., level-2 or between-person effect; Singer and Willett, 2003). MLM was especially appropriate for our study because we were interested in predicting community functioning based on how individuals' cognitive functioning changed since baseline (i.e., a level-1 effect) and based on baseline neurocognition and theory of mind on average (i.e., a level-2 effect). Moreover, MLM offers a number of advantages over traditional methods (e.g., ANOVA), such as the ability to include data from people assessed at varying time points (Singer and Willett, 2003). Because the participants in our study were assessed at different time points as part of routine care, MLM was appropriate for our data.
Unconditional and conditional polynomial models of within-person change were utilized, and included fixed effects (based on the grand mean or slope of the sample) and random effects (based on individual/person means or slopes). Unconditional models of change, that is, models examining the pattern of the means, variances, and covariances of the outcome variable over time, were estimated prior to conditional models that included predictors to determine whether there was within-person or between-person change in community functioning (Singer and Willett, 2003). Unconditional models were initially performed using mean MCAS scores (i.e., overall community functioning) as the dependent variable, and secondary unconditional analyses were performed using mean MCAS subscale scores as the dependent variables.
Conditional models first utilized total S-NAB scores and Hinting Task scores to predict changes in mean MCAS scores (i.e., overall community functioning). Subsequent conditional models were performed using S-NAB index scores and Hinting Task scores to predict mean MCAS scores and MCAS subscale scores. Conditional models were hierarchically organized, with the effects of theory of mind being added to a model with the effects of neurocognition. Given that numerous studies that have shown that social cognition accounts for unique variance in functional outcomes, we considered the “burden of proof” to be more on theory of mind to demonstrate unique contributions to variance in outcome.
According to custom (Singer and Willett, 2003), models that differed in fixed effects were compared using maximum likelihood (ML) while models differing in random effects were compared using restricted maximum likelihood (REML). Wald's tests with Satterthwaite denominator degrees of freedom were used to assess the significance of fixed effects (Hoffman, 2007). Unless otherwise specified, month in the study was used as the metric of time and was centered at the first occasion (month 0), such that the intercept represented baseline status in all models. Because an absence of standardized fixed effects in MLM precludes the reporting of typical effect sizes, Pseudo-R2 (Singer and Willett, 2003) was used to explain the proportion of variance in community functioning that was accounted for by neurocognition and theory of mind. Pseudo-R2 was calculated by subtracting each variance component estimate (i.e., residual, intercept, slope) from the same variance component in a previously tested model, and dividing by the variance component from the previous model. Overall R2 for the final predictor models was calculated as the square of the correlation between model-predicted values and observed community functioning.
All analyses were performed using SPSS version 17 and SAS PROC MIXED.
Results
Correlational Analyses
Pearson's product moment correlations at baseline were significant between total neurocognition and community functioning, and between total theory of mind and community functioning. These findings indicate that as baseline neurocognition and theory of mind became higher, baseline community functioning became higher. However, all correlations became non-significant by time 3 (see Table 2).
Table 2. Intercorrelations between Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. HT1 | - | - | - | .57** | - | - | .35* | - | - |
| 2. HT2 | - | - | - | .34 | - | - | .46* | - | |
| 3. HT3 | - | - | - | .36 | - | - | .07 | ||
| 4. S-NAB1 | - | - | - | .37* | - | - | |||
| 5. S-NAB2 | - | - | - | .34 | - | ||||
| 6. S-NAB3 | - | - | - | .40 | |||||
| 7. MCAS1 | - | - | - | ||||||
| 8. MCAS2 | - | - | |||||||
| 9. MCAS3 | - |
Note. HT = Hinting Task Total; S-NAB = Neuropsychological Assessment Battery Screener Total; MCAS = Multnomah Community Ability Scale Mean. Dash marks (-) indicate data that were not obtained.
p < .05.
p< .01.
Longitudinal Analyses
Change in overall community functioning (unconditional models)
Linear mixed models were estimated in order to examine the overall pattern of and individual differences in overall community functioning over time. A saturated means, unstructured variance model served as a baseline model and was estimated in order to determine whether there were significant mean differences in community functioning across time. To facilitate comparison of the means at each time point, time was rounded to perfect 6-month intervals in this model only (i.e., month 0, month 6, or month 12). As a test of hypothesis 2, the Type-3 Test of Fixed Effects was examined in order to determine whether there were significant mean differences across months in community functioning. This effect was significant, (F (2,22.5) = 9.67, p < .01). Thus, community functioning improved on average across time.
Fixed and random slopes of overall community functioning over time were examined next. Initially, polynomial models were specified with only a random intercept (i.e., individual baseline community functioning). Given that there were significant differences in mean community functioning over time, a fixed linear effect of month was then specified, which examined the effect of community functioning over time on average. This fixed linear effect was significant (p < .01), such that community functioning increased on average at each additional month. To test whether there were individual differences in the linear rate of change across months, a random linear model was specified next. The addition of a random linear effect (and intercept-slope covariance) resulted in a significant improvement to the model, REML deviance difference (2) = 6.4, p <.05, suggesting differences in the linear rate of change among individuals across months. Thus, the random linear model for overall community functioning was retained and served as a baseline model for subsequent conditional models using this dependent variable.
Change in specific domains of community functioning (unconditional models)
Secondary unconditional analyses demonstrated that a fixed linear, random intercept model fit the data best for the interference with functioning and social competence MCAS subscales, and that a fixed quadratic, random intercept model fit the data best for the behavioral problems subscale. A random intercept model fit the data best for the adjustment to living subscale, indicating that there was no systematic change on average on this subscale. Thus, conditional analyses involving prediction of change in this subscale was not conducted. Model parameters for each unconditional model are given in Table 3.
Table 3. Parameter Estimates and Model Fit Statistics for Community Functioning Over Time (Unconditional Models).
| Parameter | MCAS | IF | AL | SC | BP |
|---|---|---|---|---|---|
| Fixed Effects: | |||||
| Intercept | 14.79** (0.40) | 3.84** (0.10) | 3.50** (0.12) | 3.27** (0.13) | 4.18** (0.11) |
| Linear Month | 0.13** (0.04) | 0.03** (0.01) | 0.05** (0.01) | 0.08** (0.03) | |
| Quadratic Month | -0.01* (0.003) | ||||
| Variance Components: | |||||
| Residual Variance | 0.97** (0.25) | 0.13** (0.03) | 0.22** (0.05) | 0.19** (0.04) | 0.06** (0.01) |
| Intercept Variance | 6.07** (1.54) | 0.33** (0.09) | 0.50** (0.14) | 0.52** (0.14) | 0.43** (0.11) |
| Linear Month Variance | 0.02 (0.01) | ||||
| Intercept-Linear Covariance | -0.28* (0.13) | ||||
| Model Fit: | |||||
| REML Deviance | 342.9 | 150.3 | 183.7 | 182.1 | 133.7 |
| AIC | 350.9 | 154.3 | 187.7 | 186.1 | 137.7 |
| BIC | 357.9 | 157.8 | 191.2 | 189.6 | 141.2 |
Note. Standard errors are in parentheses. MCAS = multnomah community ability scale mean (overall community functioning); IF = interference with functioning; AL = adjustment to living; SC = social competence; BP = behavioral problems.
p < .05.
p< .01.
Predictors of change in overall community functioning by total neurocognition and theory of mind (conditional models)
Time-varying predictors of neurocognition and theory of mind were parameterized using a variant of person-mean centering (see Singer and Willett (2003) for a description of person-mean centering). This approach was used in order to facilitate interpretation of the effects of: (1) baseline neurocognition and theory of mind on average, and (2) change in neurocognition and theory of mind, on change in community functioning. The effect of change in neurocognition and theory of mind (i.e., the level-1 or within-person effect) was created by subtracting baseline values from values at each time point. The effect of baseline neurocognition and theory of mind on average (i.e., the level-2 or between-person effect) was created by centering baseline neurocognition and theory of mind at their approximate grand mean values in our sample.
Linear mixed models were estimated to examine the overall pattern of and individual differences in community functioning over months in the study. In order to assess the impact of neurocognition on community functioning, fixed effects for the following were added to the baseline model (i.e., random linear model): the main effect of baseline neurocognition, the effect of baseline neurocognition by linear slope interaction, the main effect of change in neurocognition, the effect of change in neurocognition by linear slope interaction, and the interaction between the effect of baseline neurocognition and the effect of change in neurocognition. The addition of these fixed effects resulted in a significant improvement to the model, ML deviance difference (5) = 14.5, p = .01, suggesting that these effects of neurocognition should be used to predict community functioning.
As a test of hypothesis 3 (that better baseline neurocognition on average would be associated with higher rates of change in community functioning), the effect of baseline neurocognition by linear slope interaction was investigated. This interaction was non-significant (p = .69), signifying that baseline neurocognition on average was not significantly related to change in community functioning over time.
As another test of hypothesis 3 (that greater improvement in neurocognition compared to baseline would be associated with higher rates of change in community functioning), the effect of change in neurocognition by linear slope interaction was examined. This interaction was significant (p = .01), indicating that for every additional 1 point improvement in neurocognition compared to baseline, the linear slope for month became more positive. Thus, change in neurocognition was related to change in community functioning.
As a test of hypothesis 5 (that the effect of change in neurocognition would depend upon baseline neurocognition), the interaction between the effect of baseline neurocognition and the effect of change in neurocognition was examined. This interaction was non-significant (p = .57), suggesting that the effect of change in neurocognition did not depend upon baseline neurocognition.
In order to improve parsimony, non-significant fixed effects of neurocognition were removed from the model one at a time. Parameters and fit statistics for the final neurocognition model are given in Table 4. Pseudo-R2, which was calculated through comparison of this model to the baseline model (i.e., random linear model), revealed that approximately 19% of the residual variance, 16% of the random intercept variance, and 10% of the random slope variance was explained by the fixed effects of neurocognition. Overall R2 indicated that the final neurocognition model accounted for approximately 22% of the total variation in community functioning.
Table 4. Parameter Estimates and Model Fit Statistics for Community Functioning (Predictor/Conditional Models).
| Parameter | Tot. Neuro.-MCAS | Tot. Neuro.TOM-MCAS | Dom. Neuro.-MCAS | Dom. Neuro.-IF | Dom. Neuro.-SC | Dom. Neuro.-BP |
|---|---|---|---|---|---|---|
| Fixed Effects: | ||||||
| Intercept | 14.86** (0.37) | 14.89** (0.36) | 14.95** (0.37) | 3.85** (0.09) | 3.28** (0.11) | 4.22** (0.10) |
| Linear month | 0.12** (0.04) | 0.14** (0.04) | 0.12** (0.03) | 0.04** (0.01) | 0.05** (0.01) | 0.08** (0.02) |
| Quadratic month | -0.01** (0.02) | |||||
| Baseline neuro. | 0.01* (0.01) | 0.01 (0.01) | ||||
| Change in neuro. | -0.04* (0.02) | -0.03 (0.02) | ||||
| Change in neuro./linear slope | 0.01* (0.002) | 0.01 (0.003) | ||||
| Baseline TOM | 0.14 (0.12) | |||||
| Change in TOM | 0.07 (0.20) | |||||
| Baseline TOM/linear slope | -0.01 (0.01) | |||||
| Change in TOM/linear slope | -0.002 (0.03) | |||||
| Baseline TOM/Change in TOM | 0.02 (0.02) | |||||
| Baseline attention | ||||||
| Change in attention | -0.12** (0.04) | |||||
| Change in attention/linear slope | 0.02** (0.01) | |||||
| Baseline language | 0.03** (0.01) | 0.01** (0.003) | ||||
| Baseline memory | -0.003 (0.003) | |||||
| Change in memory | 0.01* (0.003) | 0.001 (0.002) | ||||
| Baseline memory/linear slope | -0.002 (0.001) | |||||
| Baseline memory/quadratic slope | 0.0004** (0.0001) | |||||
| Baseline memory/change in | memory | 0.0001* (0.0001) | ||||
| Change in spatial ability | 0.03** (0.01) | 0.01* (0.01) | ||||
| Baseline exec. func. | 0.02** (0.01) | 0.02** (0.01) | ||||
| Change in exec. func. | -0.04** (0.01) | -0.03** (0.01) | ||||
| Baseline exec. func./linear sl ope | -0.002** (0.001) | |||||
| Change in exec. func./linear slope | 0.01** (0.002) | 0.004** (0.001) | ||||
| Variance Components: | ||||||
| Residual Variance | 0.78** (0.21) | 0.77** (0.20) | 0.76** (0.20) | 0.11** (0.02) | 0.11** (0.02) | 0.03** (0.01) |
| Intercept Variance | 5.09** (1.27) | 4.91** (1.23) | 5.24** (1.30) | 0.22** (0.07) | 0.44** (0.11) | 0.41** (0.09) |
| Linear Month Variance | 0.01 (0.01) | 0.02 (0.01) | 0.01 (0.01) | |||
| Intercept-Linear Covariance | -0.24* (0.11) | -0.26* (0.11) | -0.30** (0.11) | |||
| Model Fit: | ||||||
| ML Deviance | 323.6 | 320.4 | 313.7 | 120.1 | 144.0 | 83.8 |
| AIC | 341.6 | 348.4 | 333.7 | 134.1 | 160.0 | 109.8 |
| BIC | 357.4 | 354.4 | 351.3 | 146.5 | 174.1 | 132.7 |
Note. Standard errors are in parentheses. Tot. Neuro.-MCAS = Total neurocognition model predicting multnomah community ability scale mean (overall community functioning); Tot. Neuro. TOM-MCAS = Total neurocognition-theory of mind model predicting multnomah community ability scale mean (overall community functioning); Dom. Neuro.-MCAS = Neurocognitive domains model predicting multnomah community ability scale mean (overall community functioning); Dom. Neuro.-IF = Neurocognitive domains model predicting interference with functioning;); Dom. Neuro.-SC = Neurocognitive domains model predicting social competence; Dom. Neuro.-BP = Neurocognitive domains model predicting behavioral problems; neuro. = Total neurocognition; TOM = Theory of mind; exec. func. = executive functioning.
p < .05.
p< .01.
To assess the impact of theory of mind on community functioning (hypotheses 4 and 5), fixed effects for the following were added to the final neurocognition model: the main effect of baseline theory of mind, the effect of baseline theory of mind by linear slope interaction, the main effect of change in theory of mind, the effect of change in theory of mind by linear slope interaction, and the interaction between the effect of baseline theory of mind and the effect of change in theory of mind. The addition of these fixed effects resulted in a non-significant improvement to the model, ML deviance difference (5) = 3.4, p = .64, suggesting that these effects in combination should not be used to predict community functioning. All previously significant effects of neurocognition became non-significant after theory of mind effects were added to the model and none of the theory of mind effects were significant. Thus, better baseline theory of mind on average and greater improvement in theory of mind compared to baseline did not predict additional variance in community functioning after controlling for neurocognition. Parameters and fit statistics from this model are given in Table 4. Pseudo-R2, which was calculated through comparison of this model to the final neurocognition model, revealed that the fixed effects of theory of mind accounted for an additional 2% of the residual variance, 3% of the random intercept variance, and 0% of the random slope variance. Overall R2 revealed that the final neurocognition-theory of mind model accounted for approximately 26% of the total variation in community functioning.
In a follow-up analysis, in which only fixed effects of theory of mind were added to the baseline model (i.e., random linear model), the addition of these fixed effects resulted in a non-significant improvement to the model, ML deviance difference (5) = 9.8, p = .08, suggesting that these effects in combination should not be used in order to predict community functioning.
Predictors of change in community functioning by neurocognitive domains and theory of mind (conditional models)
In order to assess the impact of individual neurocognitive domains (i.e., attention, language, memory, spatial ability, and executive functioning) on overall community functioning, separate models were first estimated in which fixed effects of each neurocognitive domain alone predicted overall community functioning. The most parsimonious models for each neurocognitive domain were then combined, such that a combination of neurocognitive domains predicted overall community functioning. Non-significant effects in the combined model were then removed to produce a final model. This hierarchical approach to modeling was performed to maximize the ability to detect significant effects.
The final combined neurocognitive domain model consisted of a main effect of change in attention, an interaction between change in attention and the linear slope, a main effect of baseline language, and a main effect of change in spatial ability. The addition of these fixed effects to the baseline unconditional model for overall community functioning resulted in a significant improvement to the model, ML deviance difference (4) = 24, p < .01, suggesting that these effects of neurocognition should be used to predict community functioning. Parameters and fit statistics for the final neurocognition model are given in Table 4. Pseudo-R2, which was calculated through comparison of this model to the baseline model (i.e., random linear model), revealed that approximately 22% of the residual variance, 14% of the random intercept variance, and 4% of the random slope variance was explained by the fixed effects of neurocognition. Overall R2 indicated that the final neurocognition model accounted for approximately 26% of the total variation in community functioning.
Conditional models were then estimated for each domain of community functioning (i.e., interference with functioning, social competence, and behavioral problems) that demonstrated systematic change over time. The combined neurocognitive domain model predicting interference with functioning consisted of a main effect of baseline attention, a main effect of change in executive functioning, and an interaction between change in executive functioning and the linear slope. The addition of these fixed effects to the baseline unconditional model for interference with functioning resulted in a significant improvement to the model, ML deviance difference (3) = 18.2, p < .01, suggesting that these effects of neurocognition should be used to predict interference with functioning. Parameters and fit statistics for the final neurocognition model are given in Table 4. Pseudo-R2, which was calculated through comparison of this model to the baseline model (i.e., fixed linear, random intercept model), revealed that approximately 13% of the residual variance and 27% of the random intercept variance was explained by the fixed effects of neurocognition. Overall R2 indicated that the final neurocognition model accounted for approximately 30% of the total variation in interference with functioning.
The combined neurocognitive domain model predicting social competence consisted of a main effect of change in memory, a main effect of change in spatial ability, a main effect of baseline executive functioning, and an interaction between baseline executive functioning and the linear slope. The addition of these fixed effects to the baseline unconditional model for social competence resulted in a significant improvement to the model, ML deviance difference (4) = 29.1, p < .01, suggesting that these effects of neurocognition should be used to predict interference with functioning. Parameters and fit statistics for the final neurocognition model are given in Table 4. Pseudo-R2, which was calculated through comparison of this model to the baseline model (i.e., fixed linear, random intercept), revealed that approximately 39% of the residual variance and 12% of the random intercept variance was explained by the fixed effects of neurocognition. Overall R2 indicated that the final neurocognition model accounted for approximately 27% of the total variation in social competence.
The combined neurocognitive domain model predicting behavioral problems consisted of a main effect of baseline language, a main effect of baseline memory, interactions between baseline memory and the linear and quadratic slopes, a main effect of change in memory, an interaction between baseline memory and change in memory, a main effect of change in executive functioning, and an interaction between change in executive functioning and the linear slope. The addition of these fixed effects to the baseline unconditional model for behavioral problems resulted in a significant improvement to the model, ML deviance difference (8) = 29.8, p < .01, suggesting that these effects of neurocognition should be used to predict behavioral problems. Parameters and fit statistics for the final neurocognition model are given in Table 4. Pseudo-R2, which was calculated through comparison of this model to the baseline model (i.e., fixed quadratic, random intercept model), revealed that approximately 47% of the residual variance and 4% of the random intercept variance was explained by the fixed effects of neurocognition. Overall R2 indicated that the final neurocognition model accounted for approximately 15% of the total variation in behavioral problems.
Fixed effects of theory of mind were then used to predict each domain of community functioning. While some fixed effects of theory of mind significantly predicted interference with functioning and behavioral problems, these effects were no longer significant when added to the final neurocognition models and thus were not retained.
Discussion
Hypothesis 1, that better baseline neurocognition and theory of mind would be significantly associated with higher levels of initial community functioning, was supported. This finding is convergent with the findings of Brekke and colleagues (2007) and lends support to other research demonstrating that neurocognitive and social cognitive abilities are linked to global functional outcomes (Couture et al., 2006; Green et al., 2000).
In support of hypothesis 2, community functioning improved on average over time. Presumably, this effect is attributable to the fact that all participants were receiving integrated psychiatric rehabilitation services. Previous studies support the expectation of improvement through non-specific effects, provided there is psychiatric rehabilitation of sufficient intensity (Spaulding et al., 1999; Brekke et al., 2007). Significant functional improvement creates the opportunity to analyze concomitants of that improvement. However, this study was designed to assess the correlates, not causes, of the improvement; this is an area for further research.
Hypothesis 3 was partially supported. Contrary to Brekke et al. (2007), better baseline neurocognition on average was not a significant predictor of higher rates of change in overall community functioning. However, greater improvement in neurocognition (namely attention) compared to baseline was associated with higher rates of change in overall community functioning. Consistent with the scant research in this area (Wykes et al., 2007a; Wykes et al., 2007b), this finding provides evidence that improvement in neurocognition is associated with positive change in functional outcomes, and in a time frame that makes longitudinal cognitive assessment relevant to ongoing clinical decision making.
Secondary analyses which examined prediction of changes in specific domains of community functioning demonstrated that as executive functioning improved over time, participants demonstrated less interference with functioning (i.e., fewer psychiatric symptoms). This finding is consistent with Wykes et al. (2007b). In addition, individuals with better baseline memory demonstrated fewer behavioral problems over time. However, as baseline executive functioning improved, social competence became slightly worse over time. This was an unexpected finding, and may reflect bias in terms of staff perceptions of participants' social competence. More specifically, staff may have expected participants who were considered to be “higher functioning” in terms of cognitive abilities to be more socially adept, thus rating these individuals more severely after observing isolated neutral or negative social interactions. Alternatively, this finding may have been attributable to low reliability of the S-NAB executive functioning subscale.
Hypothesis 4 was not supported. We did not show a significant relationship between theory of mind and change in community functioning. Because research has shown that theory of mind may be more closely associated with neurocognition than other domains of social cognition (van Hooren et al., 2008), we hypothesized that the non-significant effects of theory of mind may have been due to multicollinearity in the combined neurocognition-theory of mind model. Thus, we tested only effects of theory of mind in a follow up analysis, but still failed to detect any associations between theory of mind and change in community functioning. It is unclear whether this finding is attributable to theory of mind as a predictor or the Hinting Task itself. According to Couture, Penn, and Roberts (2006), it may be more advantageous to investigate associations between social cognition and individual skills needed for real-world functioning than more global outcomes. For example, theory of mind may be more closely associated with skills such as conflict management than broad measures of community functioning. Alternatively, as suggested by Couture, Penn, and Roberts (2006), the Hinting Task may possess poor measurement properties for a longitudinal analysis, impeding the ability to detect significant findings. A lack of significant baseline theory of mind effects may have been due to ceiling effects, as on average, participants' scores at baseline fell within the “average range” of functioning (ceiling effects on the S-NAB did not appear to be a problem, as participants' scores fell within the “impaired” range on average). Thus, ceiling effects may have limited variance of scores, impeding the ability to detect a relationship between theory of mind and community functioning. Other measures of theory of mind (e.g., Marjoram et al., 2005), which have been demonstrated to be more difficult in both clinical and non-clinical control populations, may be better suited for longitudinal analyses examining the relationship between theory of mind and functional outcomes.
Lastly, hypothesis 5, that the effect of change in neurocognition and theory of mind would depend upon baseline neurocognition and theory of mind, was not supported. This is surprising, considering the usual general finding that therapeutic gains are greater in individuals with less severe problems at baseline (Brekke et al., 2007). In light of the overall improvements in cognition and behavioral functioning, this finding suggests that individuals across the range of severity at baseline have potential for improvement. There are clear implications for development of treatment modalities and for design of treatment programs.
It is possible that results from this study are not consistent with Brekke et al. (2007) given that there were a few differences in sample characteristics. For example, the present study utilized a predominantly White sample, while Brekke et al.'s (2007) was more racially diverse. In addition, the present study included a small number of people with non-schizophrenia spectrum diagnoses, while Brekke et al. (2007) included only individuals with these diagnoses. While this explanation cannot be ruled out completely, the fact that there were more similarities than differences between samples renders it dubious.
There were several limitations to this study. First, the sample and thus statistical power was relatively small. In addition to the possibilities discussed previously, non-significant effects may have been due to limited power. While obtaining unbiased fixed effect parameter estimates and variance components is possible even with relatively small sample sizes (Maas & Hox, 2005), we may have been particularly limited in the ability to detect significant cross-level interactions (e.g., baseline cognition by change in cognition interactions), as it has been proposed that at least 30 groups with 30 observations each is needed to obtain adequate power for this purpose (Scherbaum & Ferreter, 2009). Replication with a larger sample size is recommended. Second, internal reliability, as indicated by Cronbach's alpha, of the S-NAB was low, and reliability estimates for the Hinting Task were unable to be calculated. Thus, results should be interpreted with caution and replication is recommended. Lastly, given that time between testing sessions was as short as 3 months for some participants, it is possible that at least some of the improvement observed in neurocognitive test scores could be attributed to practice effects, as opposed to “true” improvement in cognitive functioning. The extent to which familiarity with the measures influenced participants' test scores on the S-NAB is likely not large, due to our use of alternate test forms and the test authors' estimate of “small” practice effects during repeated administrations. Nevertheless, to further reduce the likelihood of this potential confound, future researchers should aim for at least six months between test administrations, in accordance with the recommendations of S-NAB authors (Stern & White, 2003). In addition, because there were not alternate forms of the Hinting Task, it is possible that practice effects may have contributed to improvements over time. This is an area for further research.
Conclusions
The purpose of this study was to investigate the effects of neurocognition and theory of mind as longitudinal predictors of community functioning in an outpatient SMI sample. This study is important because it addressed the methodological limitations of previous longitudinal studies by assessing the predictive effects of both baseline cognition and change in cognition between more than 2 time points. While the priority on obtaining 3 assessment points resulted in a relatively small sample size, it significantly enhances the current literature by providing a more reliable report of relationships between functional domains over time. It is the first to assess change in theory of mind as a predictor of change in community functioning. Most significantly, by highlighting the important relationship between neurocognitive improvement and enhancement of community functioning, these results inform clinical decision-making and treatment planning.
Acknowledgments
We wish to acknowledge the members of the Serious Mental Illness Research Lab at the University of Nebraska-Lincoln for their help developing the dataset used in this study. We also wish to acknowledge Lesa Hoffman, Ph.D., who provided consultation regarding statistical analysis.
Source of Funding: This work was supported in part by the National Institute of Mental Health (5R24MH73858), Decision Science in Rehabilitation, awarded to the fifth author.
Footnotes
Conflicts of Interest: The authors declare that they have no conflicts of interest associated with this research.
The term “SMI” refers to a heterogeneous set of diagnostic categories that result in serious disabilities, such as impairment in community functioning
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addington J, Girard TA, Christensen BK, Addington D. Social cognition mediates illness-related and cognitive influences on social function in patients with schizophrenia-spectrum disorders. J Psychiatry Neurosci. 2010;35:49–54. doi: 10.1503/jpn.080039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker S, Barron N, McFarland BH, Bigelow DA. A community ability scale for chronically mentally ill consumers: part I. reliability and validity. Community Ment Health J. 1994;30:363–383. doi: 10.1007/BF02207489. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Hoe M, Long J, Green MF. How neurocognition and social cognition influence functional change during community-based psychosocial rehabilitation for individuals with schizophrenia. Schizophr Bull. 2007;33:1247–1256. doi: 10.1093/schbul/sbl072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brekke J, Kay DD, Lee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–225. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Combs DR, Mueser KT. Schizophrenia. In: Hersen M, Turner SM, Beidel DC, editors. Adult psychopathology and diagnosis. 5th. New Jersey: John Wiley & Sons, Inc; 2007. pp. 234–265. [Google Scholar]
- Corcoran R Theory of mind and schizophrenia. In: Social cognition and schizophrenia. Corrigan PW, Penn DL, editors. Washington, DC: American Psychological Association; 2001. pp. 149–174. [Google Scholar]
- Corcoran R, Mercer G, Frith CD. Schizophrenia, symptomatology and social inference: investigating “theory of mind” in people with schizophrenia. Schizophr Res. 1995;17:5–13. doi: 10.1016/0920-9964(95)00024-g. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Penn DL. Social cognition and schizophrenia. Washington, DC: American Psychological Association; 2001. [Google Scholar]
- Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;32:S44–S63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cromwell RL, Spaulding W. How schizophrenics handle information. In: Fann WE, Karacan I, Pokorny AD, Williams RL, editors. The phenomenology and treatment of schizophrenia. New York, NY: Spectrum; 1978. pp. 127–162. [Google Scholar]
- Fujii DE, Wylie AM. Neurocognition and community outcome in schizophrenia: long-term predictive validity. Schizophr Res. 2002;59:219–223. doi: 10.1016/s0920-9964(01)00328-0. [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Hendryx M, Dyck DG, McBride D, Whitbeck J. A test of the reliability and validity of the multnomah community ability scale. Community Ment Health J. 2001;37:157–168. doi: 10.1023/a:1002713816110. [DOI] [PubMed] [Google Scholar]
- Hoffman L. Multilevel models for examining individual differences in within-person variation and covariation over time. Multivariate Behav Res. 2007;42:609–629. [Google Scholar]
- Kee KS, Green MF, Mintz J, Brekke JS. Is emotion processing a predictor of functional outcome in schizophrenia? Schizophr Bull. 2003;29:487–497. doi: 10.1093/oxfordjournals.schbul.a007021. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Wexler BE, Fujimoto M, Shagan DS, Seltzer JC. Symptoms versus neurocognition as predictors of change in life skills in schizophrenia after outpatient rehabilitation. Schizophr Res. 2008;102:303–311. doi: 10.1016/j.schres.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas CJM, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology. 2005;1:6–92. [Google Scholar]
- Mancuso F, Horan WP, Kern RS, Green MF. Social cognition in psychosis: multidimensional structure, clinical correlates, and relationship with functional outcome. Schizophr Res. 2011;125:143–151. doi: 10.1016/j.schres.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marjoram D, Gardner C, Burns J, Miller P, Lawrie SM, Johnstone EC. Symptomatology and social inference: a theory of mind study of schizophrenia and psychotic affective disorders. Cogn Neuropsychiatry. 2005;10:347–359. doi: 10.1080/13546800444000092. [DOI] [PubMed] [Google Scholar]
- Meyer MB, Kurtz MM. Elementary neurocognitive function, facial affect recognition and social-skills in schizophrenia. Schizophr Res. 2009;110:173–179. doi: 10.1016/j.schres.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuechterlein KH, Dawson ME. Information processing and attentional functioning in the developmental course of schizophrenic disorders. Schizophr Bull. 1984;10:106–203. doi: 10.1093/schbul/10.2.160. [DOI] [PubMed] [Google Scholar]
- Peer JE, Kupper Z, Long JD, Brekke JS, Spaulding WD. Identifying mechanisms of treatment effects and recovery in rehabilitation of schizophrenia: longitudinal analytic methods. Clin Psychol Rev. 2007;27:696–714. doi: 10.1016/j.cpr.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Pinkham A, Penn DL. Neurocognitive and social cognitive predictors of interpersonal skill in schizophrenia. Psychiatry Res. 2006;143:167–178. doi: 10.1016/j.psychres.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Reeder C, Newton E, Frangou S, Wykes T. Which executive skills should we target to affect social functioning and symptom change? A study of a cognitive remediation therapy program. Schizophr Bull. 2004;30:87–100. doi: 10.1093/oxfordjournals.schbul.a007070. [DOI] [PubMed] [Google Scholar]
- Reeder C, Smedley N, Butt K, Bogner D, Wykes T. Cognitive predictors of social functioning improvements following cognitive remediation for schizophrenia. Schizophr Bull. 2006;32(1):S123–S131. doi: 10.1093/schbul/sbl019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roder V, Mueller DR, Mueser KT, Brenner HD. Integrated psychological therapy (IPT) for schizophrenia: is it effective? Schizophr Bull. 2006;32(1):S81–S93. doi: 10.1093/schbul/sbl021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncone R, Falloon IRH, Mazza M, De Risio A, Pollice R, Necozione S, Morosini PL, Casacchia M. Is theory of mind in schizophrenia more strongly associated with clinical and social functioning than with neurocognitive deficits? Psychopathology. 2002;35:280–288. doi: 10.1159/000067062. [DOI] [PubMed] [Google Scholar]
- Scherbaum CA, Ferreter JM. Estimated statistical power and required sample sizes for organizational research usingmultilevel models. Organizational Res Methods. 2009;12:347–367. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. New York: Oxford University; 2003. [Google Scholar]
- Spaulding WD, Reed D, Sullivan M, Richardson C, Weiler M. Effects of cognitive treatment in psychiatric rehabilitation. Schizophr Bull. 1999;25:657–676. doi: 10.1093/oxfordjournals.schbul.a033409. [DOI] [PubMed] [Google Scholar]
- Spaulding WD, Sullivan ME, Poland JS. Treatment and rehabilitation of severe mental illness. New York: Guilford Publications; 2003. [Google Scholar]
- Stern RA, White T. Neuropsychological assessment battery. Lutz, FL: Psychological Assessment Resources; 2003. [Google Scholar]
- Twamley EW, Jeste DV, Bellack AS. A review of cognitive training in schizophrenia. Schizophr Bull. 2003;29:359–382. doi: 10.1093/oxfordjournals.schbul.a007011. [DOI] [PubMed] [Google Scholar]
- van Hooren S, Versmissen D, Janssen I, Myin-Germeys I, à Campo J, Mengelers R, van Os J, Krabbendam L. Social cognition and neurocognition as independent domains in psychosis. Schizophr Res. 2008;103:257–265. doi: 10.1016/j.schres.2008.02.022. [DOI] [PubMed] [Google Scholar]
- Wilfred G, Van Gorp G, Hassenstab J. Review of the neuropsychological assessment battery. In: Spies RA, Plake BS, Murphy LL, editors. The sixteenth mental measurements. Lincoln, Nebraska: The Buros Institute of Mental Measurements; 2005. [Google Scholar]
- Wykes T, Huddy V, Cellard C, McGurk S, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168:472–485. doi: 10.1176/appi.ajp.2010.10060855. [DOI] [PubMed] [Google Scholar]
- Wykes T, Newton E, Landau S, Rice C, Thompson N, Frangou S. Cognitive remediation therapy (CRT) for young early onset patients with schizophrenia: an exploratory randomized controlled trial. Schizophr Res. 2007a;94:221–230. doi: 10.1016/j.schres.2007.03.030. [DOI] [PubMed] [Google Scholar]
- Wykes T, Reeder C, Landau S, Everitt B, Knapp M, Patel A, Romeo R. Cognitive remediation therapy in schizophrenia: randomized controlled trial. Br J Psychiatry. 2007b;190:421–427. doi: 10.1192/bjp.bp.106.026575. [DOI] [PubMed] [Google Scholar]