Abstract
Background and Aim
Existing tests for supraesophageal gastric reflux (SEGR) that focus on pH drops <4 in the proximal esophagus have had limited sensitivity and specificity. The aim of the present study was to evaluate the effect of newly proposed pH criteria on SEGR detection.
Patients and Methods
Twenty-four-hour dual-sensor pH tracings of 32 patients were reviewed. Proximal esophageal pH data were evaluated according to the conventional definition of pH drop <4 and 2 proposed definitions: pH drop <5.5 while upright and <5.0 while supine and pH drop of >10% from a running baseline. For each potential SEGR event, the preceding 1-minute window was examined for corresponding distal acid reflux.
Results
Of the 542 distal acid reflux events detected, 200 were associated with a proximal pH drop <4; this number increased to 295 using the definition of proximal pH drop <5.5 (upright)/<5.0 (supine) and 301 using the definition of proximal pH drop >10%. A proportion of proximal events, however, was not associated with distal acid reflux: 21 of 200 (10.5%) proximal pH <4 events, 119 of 414 (29%) proximal pH <5.5 (upright)/<5.0 (supine) events, and 272 of 573 (47%) proximal pH drop >10% events lacked a preceding or simultaneous drop in distal pH <4.
Conclusions
Although the use of more liberal pH criteria increased the diagnostic yield for SEGR events with dual-sensor monitoring, a significant proportion of proximal pH events did not correlate with distal acid reflux. These events could represent either false-positive measurements or association with weakly acid reflux.
Keywords: gastroesophageal reflux, pH criteria, pH probe, supraesophageal gastric reflux
Although the association of gastroesophageal reflux (GER) and respiratory disease has been well described in adults and children, a direct causal relation has yet to be established (1,2). Atypical symptoms of GER such as cough, wheezing, or stridor are hypothesized to be caused when acidic gastric contents are refluxed into areas above the upper esophageal sphincter (UES), which is known as supraesophageal gastric reflux (SEGR) (3–6). In addition to symptoms such as chronic cough or asthma, SEGR has also been implicated as an exacerbating factor for pulmonary disorders including cystic fibrosis and postlung transplant bronchiolitis obliterans syndrome (7–11).
Making the diagnosis of SEGR has been difficult using esophagoscopy, laryngoscopy, empiric trials of proton pump inhibitors, or validated patient symptom scores. Even the use of 24-hour dual-sensor pH monitoring, generally accepted as the “gold standard” diagnostic test for SEGR, has been limited by poor correlation of proximal pH data with distal pH data, extraesophageal symptoms, and/or histological findings of esophagitis or laryngitis (12–16). The ability to predict SEGR symptom response to reflux therapies based on proximal pH monitoring has also been less reliable compared with traditional GER disease (17,18).
By convention, a proximal reflux event has been defined as a drop in pH <4, at or above the UES, in association with a preceding or simultaneous distal reflux event with pH <4. The poor correlation of proximal and distal acid events detected by dual-probe monitoring may be partly explained by the observation that a significant proportion of distal acid reflux does not reach the upper esophagus. Even when it does, the refluxate can become weakly acidic by the time it reaches the proximal esophagus (5,19). Furthermore, recent data have suggested that nonacid or weakly acid reflux with pH between 4 and 7, which would be invisible to traditional pH monitoring but is detectable by impedance, may also be a significant contributor to respiratory disease and symptoms such as chronic cough (20–22). Thus, the traditional cutoff of pH <4 for SEGR could actually underestimate the presence of clinically significant reflux. This underestimation may explain the lack of sensitivity and specificity of traditional diagnostic methods to diagnose SEGR.
In conjunction with the recent introduction of a minimally invasive oropharyngeal probe that measures liquid and aerosolized pH changes in the pharynx (5,6,23), newer definitions for clinically significant SEGR based on oropharyngeal pH have been proposed. To improve the detection of SEGR and its correlation with extraesophageal symptoms, Wiener et al (5) have suggested using a relative drop in pH >10% from a running baseline. Alternatively, Ayazi et al (6) recently proposed raising the pH threshold to <5.5 while upright and <5.0 while supine.
These newer definitions of SEGR have yet to be validated in children, and we are concerned about their use in pH studies, which only monitor the proximal esophagus or airway. The primary goal of the present study therefore was to evaluate the effect of applying alternative pH criteria for the detection of proximal reflux events compared with the conventional threshold of pH <4. We also aimed to estimate how these new definitions affect the association between proximal events with corresponding distal acid reflux events and ultimately determine whether the results of proximal pH monitoring can be accurately evaluated without concurrent distal esophageal pH monitoring.
Patients and Methods
Patients
Dual-sensor pH probe studies performed at Children's Hospital Boston with a specially designed catheter that allowed for the simultaneous measurement of pH at 2 heights as well as esophageal pressures were reviewed. Patients between the ages of 3 and 18 years undergoing dual-pH probe studies for the evaluation of gastrointestinal symptoms such as regurgitation, pain, or dysphagia were included if they had completed 20- to 24-hour studies performed “off” all acid suppression medications for at least 1 week (eg, H2 receptor blocker or proton pump inhibitor), no history of congenital anomalies, and no history of gastric or esophageal surgery. Permission to conduct the study was approved by the investigational review board of Children's Hospital Boston.
Recording Technique
Each study was performed using a solid-state probe with 3 strain-gauge pressure transducers arrayed at 5-cm intervals from the distal tip. A pH electrode with an external diameter of 5 mm was located 1 cm proximal to the distal pressure transducer, and another electrode was located 1 cm proximal to the upper pressure transducer (Konigsberg Instruments Inc, Pasadena, CA). The assembly was calibrated for pH and pressure before placement and was introduced nasally. Catheter location was confirmed by chest radiograph and esophageal manometry. The catheters were adjusted following European Society of Pediatric Gastroenterology, Hepatology, and Nutrition guidelines so that the distal pH sensor was located 3 to 5 cm above the lower esophageal sphincter by manometry (24). The proximal pH sensor was located 1 to 2 cm above the UES, as confirmed by manometry.
When subjects experienced symptoms, changed body position (ie, supine vs upright), or ate meals, they recorded their events on a symptom log and pushed the corresponding buttons on the recording device. Subjects ate a regular diet with a minimum of 3 hours between each meal while in the hospital. To minimize artifacts, subjects were instructed to avoid acidic food or drink such as apple juice or carbonated beverages. Data were collected by a Synectics Microdigitrapper (Synectics Inc, Chicago, IL) and analyzed using a personal computer as previously described (25). All of the information from the written logs was manually entered into the pH tracing. Meals were excluded from the analysis.
Analysis of Data
The tracings were manually analyzed by 1 investigator (E.C.) using pH data analysis software (PolyGram Function Testing Software, Medtronic Synectics, Shoreview, MN). Each distal and proximal esophageal event was manually identified and analyzed. A distal acid reflux episode was defined as a discrete drop in pH to <4 for ≥5 seconds. The distal acid reflux index was determined by calculating the amount of time with pH <4 as a percentage of the total recording time. According to North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition criteria for GER, a pH probe was considered abnormal if the distal reflux index was >6% for children older than 1 year of age (26). The proximal acid reflux index was determined by calculating the amount of time with proximal pH <4 as a percentage of the total recording time. Distal weakly acidic episodes were defined by a >10% drop in pH from baseline, while remaining between a pH of 4 and 7 (27).
Proximal pH data were evaluated according to the conventional definition of SEGR (pH drop <4) as well as 2 recently proposed definitions: pH drop of at least 10% from a running baseline (5) and pH drop <5.5 while upright and <5.0 while supine (6). The number of potential reflux events was determined using each definition separately. For each proximal reflux event that was detected, the preceding 1-minute window of the concurrent distal pH tracing was examined for a distal acid reflux event, with pH <4 to be considered an episode of SEGR. If no distal acid event was identified, then the distal pH tracing was analyzed for the presence of weakly acidic reflux as defined above. Proximal events were categorized according to the association with a distal acid reflux event with pH <4, with a distal pH drop > 10% to pH 4 to 7, or with minimal or no distal pH change at all. Correlation of distal and proximal reflux events were also analyzed according to the subject's position (ie, supine versus upright).
Statistical Analysis
Means of continuous variables were compared using t tests. For comparisons of proportions, χ2 or the Fisher exact test was used where appropriate. We used the Statistical Package for the Social Sciences PC version 16.0 (SPSS Inc, Chicago, IL) for all of the statistical calculations. A P value of <0.05 was considered to be statistically significant.
Results
Thirty-two patients (21 boys, 11 girls) with median age of 13 years (range 3–17 years) who underwent dual-sensor pH monitoring were included. A total of 542 distal acid reflux events were detected. Six patients met North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition criteria for abnormal distal acid reflux with pH <4 for >6% of the study (GER group). The remaining 26 patients had normal distal esophageal pH results (non-GER group). As would be expected, subjects in the GER group had a significantly higher mean number of SEGR events identified by proximal pH <4 compared with subjects in the non-GER group (17.3 ± 12.4 vs 4.9 ± 4.8 events, respectively; P = 0.03).
Impact of Definition on SEGR Event Detection
Of the 542 distal reflux episodes detected, 200 (36.9%) were associated with a proximal pH drop <4 for >5 seconds. When the definition of proximal pH drop <5.5 while upright and <5.0 while supine was applied, 295 SEGR events were detected, which is an increase of 47.5% compared with the traditional definition. Using the proposed definition of proximal >10% drop from baseline, this number increased to 301, which represents an increase of 51% compared with the traditional definition. On a per-patient basis, this equated to an increase from a mean of 6.3 ± 8.0 proximal events per study using a pH cutoff of <4 to 9.2 ±9.7 proximal events using the definition of proximal pH drop <5.5 while upright and <5.0 while supine, and 9.4 ± 10.2 using the definition of proximal >10% drop from baseline (P < 0.001).
Correlation Between Proximal and Distal Events
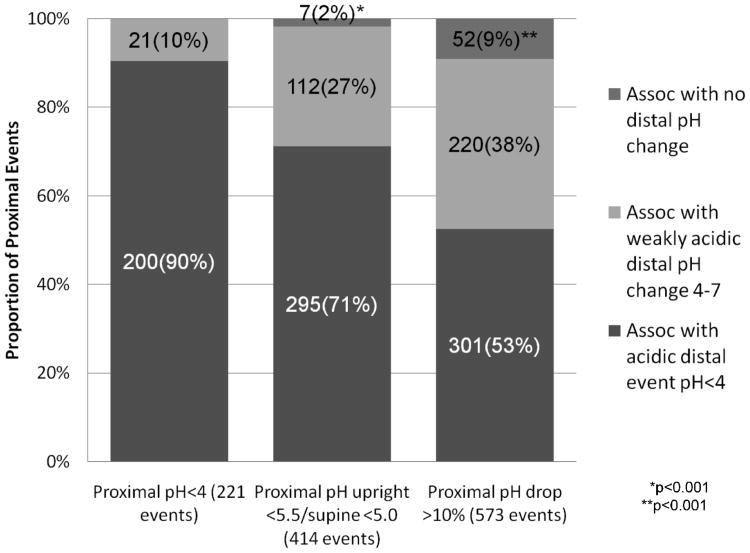
The proportion of proximal reflux events with and without associated acidic distal pH changes, according to each definition of SEGR, is shown in Figure 1. Although the number of SEGR episodes increased as more liberal definitions were used, the overall proportion that was associated with a pH drop <4 at the distal sensor decreased substantially. Using the strictest definition of a pH drop <4 at both the proximal and distal sensors, there was a 90% rate of concordance. On the contrary, 71% of proximal events identified by pH <5.5 while upright and <5.0 while supine, and only 53% of proximal events defined by a drop in pH > 10% from baseline were associated with a concurrent distal acid reflux event (P < 0.001). Likewise, the proportion of proximal events without any correlation at the distal pH sensor increased with more liberal definitions of SEGR.
Figure 1.
Association of proximal pH events with changes in distal esophageal pH, according to each of the definitions for abnormal proximal pH used. As can be seen, the proportion of proximal events without any correlation at the distal pH sensor increased with more liberal definitions of supraesophageal gastric reflux (* and ** indicate P values for pairwise comparisons of the proportions of events with and without distal correlation, as detected by each alternative definition of supraesophageal gastric reflux versus conventional criteria [pH <4.0]).
Effect of Body Position
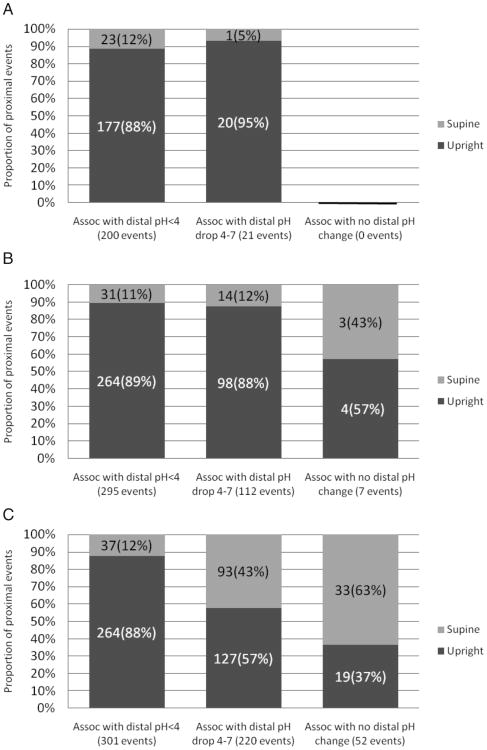
Overall, the majority of distal and proximal reflux events occurred while subjects were in an upright position. Eighty-three percent of distal reflux events occurred while subjects were upright. Similarly, 177 of 200 (88.5%) proximal events with pH <4, 264 of 295 (89.5%) proximal events with pH drop <5.5 while upright and <5.0 while supine, and 264 of 301 (88%) proximal pH drops >10% occurred in the upright position. With more liberal definitions of SEGR, however, a disproportionate number of proximal events with no associated changes in distal pH occurred while patients were supine (Fig. 2). All proximal events with pH <4 were associated with a preceding or simultaneous change in distal pH.
Figure 2.
Effect of body position on the association of proximal events with changes in distal pH, for each of the definitions of abnormal proximal pH used: (A) proximal pH drop <4; (B) proximal pH drop <5.5 while upright, <5.0 while supine; (C) proximal pH drop >10% from baseline.
Discussion
Results of the present study demonstrate that recently proposed definitions for SEGR that use a relative pH drop or a higher pH threshold significantly increased the detection of proximal reflux events in children compared with the conventional criteria of a proximal pH decrease <4. Our study also shows, however, that using these new definitions increased the identification of proximal episodes with no corresponding distal esophageal acid reflux (as defined by pH <4).
Consensus regarding optimal pH criteria for the definition of a supraesophageal regurgitation event is currently lacking. The minimum amount of supraesophageal acid exposure needed to produce clinically significant pathological changes in humans is not well understood. By convention, most investigators have applied the same criteria used to define distal GER, namely, a decrease in pH to <4, to proximal pH measurements as well. Compared with the distal esophagus however, areas proximal to the UES possess a different epithelial structure and are thought to be more sensitive to acid reflux injury (28). Recognizing these potential differences, it may not be appropriate to assume that the same pH criteria should be applied to both locations. This observation is supported by the failure of previous clinical studies to establish a correlation between SEGR symptoms upper esophageal or pharyngeal pH findings using a conventional cutoff of pH <4. The concern that the upper esophagus and pharyngeal tissues are more sensitive to changes in acidity has prompted some investigators to propose alternative definitions for SEGR, such as the ones examined in the present study, to increase the sensitivity of proximal pH monitoring.
Our data showed that these new definitions of SEGR resulted in the detection of a significant number of episodes that would not have been observed using the stricter, conventional criteria of pH <4. Increased detection of SEGR events has the potential to improve clinical correlation between symptoms and changes in proximal esophageal pH. With more liberal definitions of SEGR however, there was also an increase in the number of proximal events, which were not associated with a preceding or simultaneous distal drop in pH <4. Although it is evident that the use of these newly proposed definitions of SEGR identifies additional proximal events that are clearly associated with distal acid reflux, it is not clear whether to interpret changes in proximal pH that are not temporally correlated to distal acid reflux as artifacts of monitoring versus clinically relevant events.
These observations raise the question of how it is possible to have significant proximal esophageal reflux events without evidence of prior distal esophageal acidification. In theory, lack of correlation between proximal and distal sensors could be partly due to artifact. The possibility of these episodes being artifacts is supported by a previous study by Williams et al (29), which observed that small pharyngeal decreases by 1 to 2 pH units, roughly equivalent to a >10% drop in pH, had a 92% chance of being a definite artifact. Other explanations for how an SEGR event could occur without any apparent change in distal pH include the possibility of different physiopathology of pharyngeal acidification (eg, nongastric sources of acidity); differences in catheter contact with wet mucosa; or the presence of nonacid reflux, which would not be detected by conventional esophageal pH monitoring.
Nonacid reflux has been associated with chronic cough and other respiratory disorders (30,31). In the present investigation, 48% of proximal events with pH drop >10%, and 27% of proximal events with pH <5.5 while upright or pH <5.0 while supine were associated with weakly acidic changes in distal pH between 4 and 7. Although this association suggests that there may be a correlation between SEGR events and weakly acid distal reflux, it is impossible to confirm this with distal pH monitoring data alone. Given that both acid and nonacid reflux can now be identified with the use of impedance monitoring (27,32), future studies in which the supraesophageal detection of reflux is correlated with esophageal impedance measurements are needed.
We also investigated the relation between body position and SEGR and found that the majority of proximal events with corresponding distal acid reflux occurred when subjects were upright, which is consistent with prior studies (33–35). On the contrary, we found that proximal pH events that did not have a preceding or simultaneous distal reflux event were more likely to occur while subjects were supine; 63% of proximal events identified by a relative drop in pH >10% that were not associated with a drop in distal pH <4 occurred while subjects were supine. Similarly, downward drifts in pharyngeal pH while patients are supine have been previously described in studies as “pseudoreflux” and is postulated to be caused by mucosal drying or poor contact between pharyngeal mucosa and the pH sensor (36).
Two recent studies that compared oropharyngeal pH probe monitoring with concurrent esophageal pH probes in adults also found increased inconsistency between proximal and distal pH data obtained during the supine period. Golub et al (37) described a tendency for the oropharyngeal pH probe to register progressively lower pH levels and more noncorrelating pH events during sleep, and even suggested that data obtained during sleep should be excluded from analysis, to improve correlation with distal events (37). Chheda et al (38) also observed a higher rate of false-positive and noncorresponding pharyngeal events occurring in the supine position in a study of asymptomatic, normal adult volunteers.
There are some limitations to our study. First, we applied new definitions of SEGR, which were proposed for oropharyngeal pH monitoring to proximal esophageal pH data. We acknowledge that pH results can differ depending on the anatomic location of the pH sensor. The exact difference between pH monitoring in the proximal esophagus above the UES versus in the posterior oropharynx is not known, but a linear decrease in the number of reflux events and duration of acid exposure with increasingly proximal probes has been described (39). On the contrary, one of the strengths of our study was the use of manometric confirmation of the proximal pH electrode above the UES, ensuring that proximal pH measurements were truly supraesophageal. Because our pH measurements were obtained above the upper sphincter, we would expect only a small difference compared with pharyngeal monitoring.
Our study included patients who presented with gastrointestinal symptoms of pain, regurgitation, or dysphagia. We did not have a true control group composed of healthy, normal children, nor did we specifically select subjects who had extraesophageal symptoms such as chronic cough, sore throat, or wheezing. The purpose of our study, however, was not to characterize SEGR events in a particular patient group or in relation to symptoms; rather, our goal was to determine the correlation of proximal and distal events when different definitions of SEGR are used.
In conclusion, we have shown that application of newer definitions of SEGR significantly increased the diagnostic yield for proximal reflux events by dual-probe pH monitoring compared with the conventional pH threshold of <4.0. There were a significant number of proximal events however, which did not correlate with a preceding or simultaneous distal acid reflux event, especially when the newer definitions of SEGR were applied and when subjects were in the supine position. Some proximal events did correlate with drops in distal pH ranging from 4 to 7, which suggests that a proportion of SEGR events could be associated with weakly acidic reflux. Additional studies comparing proximal pH measurements with esophageal impedance data would help to clarify the relation between SEGR and nonacid reflux. Until we have a clearer understanding of the pathogenesis of SEGR events, studies that apply more liberal definitions of SEGR to stand-alone oropharyngeal pH probe monitoring need to be interpreted with caution due to the inability to confirm prior distal esophageal acidification.
Acknowledgments
The present work was supported by NIH grants T32DK007477-25 (Dr Chiou), K23DK073713 (Dr Rosen), and K24DK082792A (Dr Nurko).
Footnotes
The authors report no conflicts of interest.
References
- 1.Toila V, Vandenplas Y. Systematic review: the extra-oesophageal symptoms of gastro-oesophageal reflux disease in children. Aliment Phamacol Ther. 2009;29:258–72. doi: 10.1111/j.1365-2036.2008.03879.x. [DOI] [PubMed] [Google Scholar]
- 2.El-Serag H, Gilger M, Keubeler M, et al. Extraesophageal associations of gastroesophageal reflux disease in children without neurologic defects. Gastroenterology. 2001;121:1294–9. doi: 10.1053/gast.2001.29545. [DOI] [PubMed] [Google Scholar]
- 3.Koufman J. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investiations of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101:1–78. doi: 10.1002/lary.1991.101.s53.1. [DOI] [PubMed] [Google Scholar]
- 4.Rudolph C. Supraesophageal complications of gastroesophageal reflux in children: challenges in diagnosis and treatment. Am J Med. 2003;115:150S–6S. doi: 10.1016/s0002-9343(03)00214-6. [DOI] [PubMed] [Google Scholar]
- 5.Wiener G, Tsukashima R, Kelly C, et al. Oropharyngeal pH monitoring for the detection of liquid and aerosolized supraesophageal gastric reflux. J Voice. 2009;23:498–504. doi: 10.1016/j.jvoice.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Ayazi S, Lipham J, Hagen J, et al. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J Gastrointest Surg. 2009;13:1422–9. doi: 10.1007/s11605-009-0915-6. [DOI] [PubMed] [Google Scholar]
- 7.Blondeau K, Dupont L, Mertens V, et al. Gastro-oesophageal reflux and aspiration of gastric contents in adult patients with cystic fibrosis. Gut. 2008;57:1049–55. doi: 10.1136/gut.2007.146134. [DOI] [PubMed] [Google Scholar]
- 8.Fathi H, Moon T, Donaldson J, et al. Cough in adult cystic fibrosis: diagnosis and response to fundoplication. Cough. 2009;18:1. doi: 10.1186/1745-9974-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sweet M, Patti M, Hoopes C, et al. Gastro-oesophageal reflux and aspiration in patients with advanced lung disease. Thorax. 2009;64:167–73. doi: 10.1136/thx.2007.082719. [DOI] [PubMed] [Google Scholar]
- 10.Halsey K, Wald A, Meyer K, et al. Non-acidic supraesophageal reflux associated with diffuse alveolar damage and allograft dysfunction after lung transplantation: a case report. J Heart Lung Transplant. 2008;27:564–7. doi: 10.1016/j.healun.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 11.Palmer S, Miralles A, Howell D, et al. Gastroesophageal reflux as a reversible cause of allograft dysfunction after lung transplantation. Chest. 2000;118:1214–7. doi: 10.1378/chest.118.4.1214. [DOI] [PubMed] [Google Scholar]
- 12.Vaezi M, Schroeder P, Richter J. Reproducibility of proximal probe pH parameters in 24-hour ambulatory esophageal pH monitoring. Am J Gastroenterol. 1997;92:825–9. [PubMed] [Google Scholar]
- 13.Shaker R, Bardan E, Gu C, et al. Intrapharyngeal distribution of gastric acid refluxate. Laryngoscope. 2003;113:1182–91. doi: 10.1097/00005537-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Bilgen C, Ogut F, Kesimli-Dinc H, et al. The comparison of an empiric proton pump inhibitor trial vs 24-hour double-probe pH monitoring in laryngopharyngeal reflux. J Laryngol Otol. 2003;117:386–90. doi: 10.1258/002221503321626438. [DOI] [PubMed] [Google Scholar]
- 15.Heine R, Cameron D, Chow C, et al. Esophagitis in distressed infants: poor diagnostic agreement between esophageal pH monitoring and histopathologic findings. J Pediatr. 2002;140:14–9. doi: 10.1067/mpd.2002.120695. [DOI] [PubMed] [Google Scholar]
- 16.McMurray J, Gerber M, Stern Y, et al. Role of laryngoscopy, dual pH probe monitoring, and laryngeal mucosal biopsy in the diagnosis of pharyngoesophageal reflux. Ann Otol Rhinol Laryngol. 2001;110:299–304. doi: 10.1177/000348940111000402. [DOI] [PubMed] [Google Scholar]
- 17.Ulualp S, Toohill R, Shaker R. Outcomes of acid suppressive therapy in patients with posterior laryngitis. Otolaryngol Head Neck Surg. 2001;124:16–22. doi: 10.1067/mhn.2001.112200. [DOI] [PubMed] [Google Scholar]
- 18.Wo J, Koopman J, Harrell S, et al. Double-blind, placebo-controlled trial with single-dose pantoprazole for laryngopharyngeal reflux. Am J Gastroenterol. 2006;101:1972–8. doi: 10.1111/j.1572-0241.2006.00693.x. [DOI] [PubMed] [Google Scholar]
- 19.Emerenziani S, Ribolsi M, Sifrim D, et al. Regional oesophageal sensitivity to acid and weakly acidic reflux in patients with non-erosive reflux disease. Neurogastroenterol Motil. 2009;21:253–8. doi: 10.1111/j.1365-2982.2008.01203.x. [DOI] [PubMed] [Google Scholar]
- 20.Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004;99:2452–8. doi: 10.1111/j.1572-0241.2004.40268.x. [DOI] [PubMed] [Google Scholar]
- 21.Mainie I, Tutuian R, Agrawal A, et al. Fundoplication eliminates chronic cough due to non-acid reflux identified by impedance pH monitoring. Thorax. 2005;60:521–3. doi: 10.1136/thx.2005.040139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patterson N, Mainie I, Rafferty G, et al. Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol. 2009;43:414–9. doi: 10.1097/MCG.0b013e31818859a3. [DOI] [PubMed] [Google Scholar]
- 23.Sun G, Muddana S, Slaughter J, et al. A new pH catheter for laryngopharyngeal reflux: normal values. Laryngoscope. 2009;119:1639–43. doi: 10.1002/lary.20282. [DOI] [PubMed] [Google Scholar]
- 24.Vandenplas Y, Belli D, Boige N. A standardized protocol for the methodology of esophageal pH monitoring and interpretation of the data for the diagnosis of gastro-esophageal reflux. J Pediatr Gastroenterol Nutr. 1992;14:467–71. doi: 10.1097/00005176-199205000-00017. [DOI] [PubMed] [Google Scholar]
- 25.Chitkara DK, Fortunato C, Nurko S. Prolonged monitoring of esophageal motor function in healthy children. J Pediatr Gastroenterol Nutr. 2004;38:192–7. doi: 10.1097/00005176-200402000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Rudolph C, Mazur L, Liptak G, et al. Guidlines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 2001;32:S1–31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 27.Vela MF. Non-acid reflux: detection by multichannel intraluminal impedance and pH, clinical significance and management. Am J Gastroenterol. 2009;104:277–80. doi: 10.1038/ajg.2008.23. [DOI] [PubMed] [Google Scholar]
- 28.Johnston N, Wells CW, Samuels TL, et al. Pepsin in nonacidic refluxate can damage hypopharyngeal epithelial cells. Ann Otol Rhinol Laryngol. 2009;118:677–85. doi: 10.1177/000348940911800913. [DOI] [PubMed] [Google Scholar]
- 29.Williams R, Ali G, Wallace K. Esophagopharyngeal acid regurgitation: dual pH monitoring criteria for its detection and insights into mechanisms. Gastroenterology. 1999;117:1051–61. doi: 10.1016/s0016-5085(99)70389-6. [DOI] [PubMed] [Google Scholar]
- 30.Sifrim D, Dupont L, Blondeau K, et al. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–54. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tutuian R, Mainie I, Agrawal A, et al. Nonacid reflux in patients with chronic cough on acid-suppressive therapy. Chest. 2006;130:386–91. doi: 10.1378/chest.130.2.386. [DOI] [PubMed] [Google Scholar]
- 32.Rosen R, Lord C, Nurko S. The sensitivity of multichannel intraluminal impedance and the pH probe in the evaluation of gastroesophageal reflux in children. Clin Gastroenterol Hepatol. 2006;4:167–72. doi: 10.1016/s1542-3565(05)00854-2. [DOI] [PubMed] [Google Scholar]
- 33.Wiener GJ, Koufman JA, Wu WC, et al. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84:1503–8. [PubMed] [Google Scholar]
- 34.Shaker R, Milbrath M, Ren J, et al. Esophagopharyngeal distribution of refluxed gastric acid in patients with reflux laryngitis. Gastroenterology. 1995;109:1575–82. doi: 10.1016/0016-5085(95)90646-0. [DOI] [PubMed] [Google Scholar]
- 35.Eubanks TR, Omelanczuk PE, Maronian N, et al. Pharyngeal pH monitoring in 222 patients with suspected laryngeal reflux. J Gastrointest Surg. 2001;5:183–90. doi: 10.1016/s1091-255x(01)80032-9. [DOI] [PubMed] [Google Scholar]
- 36.Wiener G, Koufman J, Wu W, et al. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84:1503–8. [PubMed] [Google Scholar]
- 37.Golub J, Johns M, Lim J, et al. Comparison of an oropharyngeal pH probe and a standard dual pH probe for diagnosis of laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2009;188:1–5. doi: 10.1177/000348940911800101. [DOI] [PubMed] [Google Scholar]
- 38.Chheda N, Seybt M, Schade R, et al. Normal values for pharyngeal pH monitoring. Ann Otol Rhinol Laryngol. 2009;188:166–71. doi: 10.1177/000348940911800302. [DOI] [PubMed] [Google Scholar]
- 39.Weusten B, Akkermans L, Van Berge Henegouwen G, et al. Spatio-temporal characteristics of physiological gastroesophageal reflux. Am J Physiol. 1994;266:G357–62. doi: 10.1152/ajpgi.1994.266.3.G357. [DOI] [PubMed] [Google Scholar]