Abstract
Background
The primary objective of this study was to determine the efficiency of a pneumatic device in controlling cuff pressure (Pcuff) in patients intubated with polyurethane-cuffed tracheal tubes. Secondary objectives were to determine the impact of continuous control of Pcuff, and cuff shape on microaspiration of gastric contents.
Methods
Prospective randomized controlled study. All patients requiring intubation and mechanical ventilation ≥48 h were eligible. The first 32 patients were intubated with tapered polyurethane-cuffed, and the 32 following patients were intubated with cylindrical polyurethane-cuffed tracheal tubes. Patients randomly received 24 h of continuous control of Pcuff using a pneumatic device (Nosten®), and 24 h of routine care of Pcuff using a manometer. Target Pcuff was 25 cmH2O. Pcuff was continuously recorded, and pepsin was quantitatively measured in all tracheal aspirates during these periods.
Results
The pneumatic device was efficient in controlling Pcuff (med [IQ] 26 [24, 28] vs 22 [20, 28] cmH2O, during continuous control of Pcuff and routine care, respectively; p = 0.017). In addition, percentage of patients with underinflation (31% vs 68%) or overinflation (53% vs 100%) of tracheal cuff, and percentage of time spent with underinflation (0.9 [0, 17] vs 14% [4, 30]) or overinflation (0 [0, 2] vs 32% [9, 54]) were significantly (p < 0.001) reduced during continuous control of Pcuff compared with routine care.
No significant difference was found in microaspiration of gastric content between continuous control of Pcuff compared with routine care, or between patients intubated with tapered compared with cylindrical polyurethane-cuffed tracheal tubes.
Conclusion
The pneumatic device was efficient in controlling Pcuff in critically ill patients intubated with polyurethane-cuffed tracheal tubes.
Trial registration
The Australian New Zealand Clinical Trials Registry (NCT01351259)
Keywords: Intubation, Polyurethane, Tracheal cuff, Microaspiration, Tracheal injury, Pneumonia
Background
Microaspiration of contaminated oropharyngeal secretions and gastric content frequently occurs in intubated critically ill patients, and plays a major role in the pathogenesis of ventilator-associated pneumonia (VAP) [1]. Aspiration of contaminated secretions is followed by tracheobronchial colonization that might progress into VAP depending on quantity, and virulence of microorganisms, and local and general defense mechanisms [2].
During the last decade, significant progress has been achieved in the field of prevention of microaspiration, and VAP [3,4]. Polyurethane-cuffed tracheal tubes were reported to significantly reduce leakage in in vitro studies, and microaspiration in intubated critically ill patients [5-7]. In addition, three clinical studies reported significant reduction in VAP, and nosocomial pneumonia rate in patients intubated with polyurethane-cuffed tracheal tubes compared with those intubated with standard polyvinyl chloride-cuffed tracheal tubes [8-10]. However, limitations of these studies, including the use of subglottic aspiration in the intervention group in one study, clinical definition of nosocomial pneumonia, and before-after design should be taken into account. Recent data coming from in vitro studies also suggested a beneficial effect of tapered-shaped tracheal cuff in reducing microaspiration [11-13].
Underinflation, and overinflation of tracheal cuff are major risk factors for microaspiration, VAP, and tracheal injury [14-16]. Despite routine control of cuff pressure (Pcuff) using a manometer, patients intubated with polyvinyl-chloride or polyurethane-cuffed tracheal tubes spend a large amount of time with underinflation and overinflation of tracheal cuff [6,17]. Continuous control of polyvinyl chloride-cuffed tracheal tubes using a pneumatic device was found to be associated with significantly reduced microaspiration of gastric content, and VAP incidence [18]. However, there are several differences between polyvinyl chloride and polyurethane, including thickness and physicochemical properties. Condensation formation in the pilot external balloon is very frequent in patients intubated with polyurethane-cuffed tracheal tubes. Whether condensation formation or other physicochemical properties of polyurethane could influence the efficiency of a pneumatic device in continuously controlling Pcuff is unknown. To our knowledge, no study has evaluated the efficiency of a pneumatic or an electronic device in continuously controlling Pcuff in patients intubated with polyurethane-cuffed tracheal tubes. Therefore, we conducted this randomized controlled trial to determine the efficiency of a pneumatic device in controlling Pcuff in critically-ill patients intubated with polyurethane-cuffed tracheal tube compared with routine care using a manual manometer. The secondary objectives were to determine the impact of continuous control of Pcuff, and cuff shape, i.e. tapered versus cylindrical, on microaspiration of gastric content.
Methods
The local institutional review board of the Lille University Hospital approved this study. The patients provided their written consent before randomization. In unconscious patients who were not able to give consent for inclusion in the study at randomization, relatives (next-of-kin) gave assent on every patient’s behalf, and patients were later given the opportunity to withdraw from the study. The study was registered at clinicaltrial.gov (NCT01351259).
Study design
This prospective randomized controlled cross-over study was conducted in a single 10-bed medical ICU during a 17-month period. Inclusion criteria were age >18 years, intubation in the ICU, and expected duration of invasive mechanical ventilation ≥48 hours. Exclusion criteria were enrolment in another trial, contraindication for semirecumbent position or for enteral nutrition, and intubation before ICU admission.
Primary objective was to determine the efficiency of a pneumatic device in controlling Pcuff in patients intubated with polyurethane-cuffed tracheal tubes compared with routine care using a manual manometer. Secondary objectives were to determine the impact of continuous control of Pcuff, and cuff shape, i.e. tapered versus cylindrical, on microaspiration of gastric contents.
All patients were intubated with polyurethane-cuffed tracheal tubes. Tracheal tube size was 7.5 and 8 in women and men, respectively. The first 32 patients were intubated with a tapered-cuffed tracheal tube (SealGuard®, Mallinckrodt, Athlone, Ireland), and the 32 following patients were intubated with a cylindrical-cuffed tracheal tube (Microcuff®, Kimberly-Clark, Georgia, USA). Patients were randomly assigned to receive continuous control of Pcuff for 24 hours followed by routine care for 24 hours, or routine care for 24 hours followed by continuous control Pcuff for 24 hours. The target Pcuff was 25 cm H2O during the two 24-hour periods. A computer-generated random assignment list in balanced blocks of four was used. Sealed opaque individual envelopes containing treatment assignments were numbered sequentially. All caregivers were blinded to the randomization schedule and the block size. Because of the nature of the intervention, physicians and nurses could not be blinded to the randomization arm. However, engineer who performed the analysis of Pcuff recording (JD) and physicians who performed pepsin measurement (FZ, and MB) were blinded to study group assignment.
Tracheal cuff management
Routine care of tracheal cuff was managed according to an internal procedure adapted from the Société de Réanimation de Langue Française recommendations [19]. A manual manometer (Ambu® Cuff Pressure Gauge, Ambu A/S, Ballerup, Denmark) was used to check and adjust Pcuff every 8 hours. Continuous control of Pcuff was performed using a pneumatic device (Nosten®, Leved, St-Maur, France) [20].
Outcome measurement
In all patients, Pcuff and airway pressure were continuously recorded (Physiotrace®, CHRU, Lille, France) at a digitizing frequency of 100 Hz during the 48 hours following randomization, including 24 hours of continuous control of Pcuff, and 24 hours of routine care. Nurses were blinded to recording data. Pepsin was quantitatively measured in all tracheal aspirates during the same two 24-hour periods. In order to avoid overlap in pepsin results between the two 24-hour periods, tracheal suctioning was always performed at the end of the first periods of Pcuff control. Tracheal aspirates were stored at -20°C. Quantitative pepsin measurement was performed by an ELISA technique [18].
Study population
Measures aiming at preventing microaspiration were used in all patients including protocolized enteral nutrition, and sedation, minimal positive end expiratory pressure of 5 cm H2O, and semirecumbent position. Continuous subglottic suctioning was not utilized. Nurses performed tracheal suctioning every 3 hours or more if clinically indicated, using an open tracheal suction system.
Definitions
The primary end point was the percentage of patients with underinflation (Pcuff <20 cm) H2O or overinflation (Pcuff >30 cm H2O) of tracheal cuff. Secondary outcomes included duration of underinflation and overinflation of Pcuff, coefficient of variation of Pcuff, and microaspiration of gastric content. Pcuff continuous recording data were used to determine the time spent with normal Pcuff, underinflation, and overinflation of tracheal cuff. The coefficient of variation of Pcuff was calculated as standard deviation/mean Pcuff × 100. Microaspiration of gastric content was defined by the presence of pepsin at significant level (>200 ng/mL) in at least one tracheal aspirate.
Statistical analyses
Based on the incidence of underinflation or overinflation of tracheal cuff in patients intubated with polyurethane-cuffed tracheal tubes and receiving routine care of Pcuff in our ICU (70%), we estimated an incidence of underinflation or overinflation in patients intubated with polyurethane-cuffed tracheal tubes and receiving continuous control of Pcuff of 30%. Randomly assigning 32 patients to two 24-hour periods of Pcuff control would allow detection of this difference with 80% power and a two-tailed significance level of 0.05. To determine the impact of cuff shape on microaspiration of gastric content, two groups of 32 patients intubated with tapered or cylindrical-cuffed tracheal tubes were required.
All P values were two-tailed. Categorical variables were described as frequencies (%). Because they were not normally distributed, continuous variables were described as median (interquartile range). McNemar’s test and Wilcoxon rank test were used to compare qualitative and quantitative variables between the two 24-hour periods, respectively. For comparisons between subgroups (tapered versus cylindrical-cuffed tracheal tubes), χ2 test or Fisher exact test were used to compare qualitative variables, and Mann–Whitney U test was used to compare continuous variables.
To determine the impact of high airway pressures on the efficiency of the pneumatic device, we compared the time spent with underinflation and overinflation of Pcuff during continuous control of tracheal cuff between patients with high airway pressures (≥ 75th quartile of airway pressures in the cohort), and those with lower airway pressures (<75th quartile of airway pressures in the cohort).
Results
Patient characteristics
Sixty four patients were included in this study, including 32 intubated with tapered-cuffed tracheal tube, and 32 with cylindrical-cuffed tracheal tube. Study flow chart is presented in Figure 1. Median time from intubation to randomization was 3 days (1, 7). Median tracheal tube size was 8 mm (7.5-8). No significant difference was found in median time from intubation to randomization (4 [1,8] vs 2 days [1,5]), p = 0.470; or tracheal tube size (8 [7.5-8] vs 8 mm [7.5-8], p = 0.456) between patients intubated with tapered-cuffed tracheal tubes and those intubated with cylindrical-cuffed tracheal tubes, respectively. No significant difference was found in patient characteristics between the two periods of continuous control of Pcuff and routine care, or between patients intubated with tapered-cuffed tracheal tubes, and those intubated with cylindrical-cuffed tracheal tubes (Tables 1, and 2).
Figure 1.
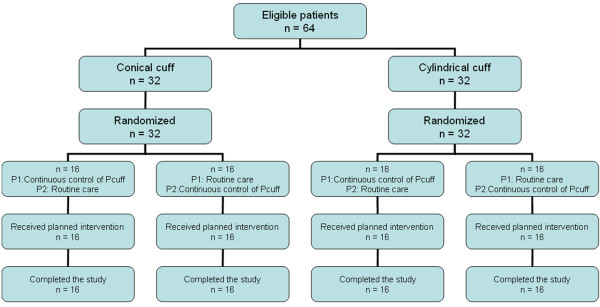
Study flowchart. Pcuff, cuff pressure; P1, period 1; P2, period 2.
Table 1.
Patient characteristics at ICU admission
| Variables | All patients n = 64 | Tapered cuff n = 32 | Cylindrical cuff n = 32 | P* |
|---|---|---|---|---|
| Age |
66 (55–75) |
66 (58–77) |
66 (54–72) |
0.330 |
| Male gender |
43 (67) |
20 (62) |
23 (71) |
0.594 |
| SAPS II |
45 (32–62) |
45 (29–62) |
42 (37–62) |
0.289 |
| LOD score |
6 (3–9) |
6 (2–10) |
6 (4–9) |
0.818 |
| Comorbidities |
|
|
|
|
| Diabetes mellitus |
16 (25) |
10 (31) |
6 (18) |
0.386 |
| COPD |
23 (35) |
11 (34) |
12 (37) |
>0.999 |
| Cardiovascular disease |
12 (18) |
7 (21) |
5 (15) |
0.749 |
| Cirrhosis |
1 (1) |
1 (3) |
0 |
>0.999 |
| Causes for ICU admission |
|
|
|
|
| Acute exacerbation of COPD |
18 (28) |
10 (31) |
8 (25) |
0.781 |
| ARDS |
7 (10) |
3 (9) |
4 (12) |
>0.999 |
| Septic shock |
15 (23) |
10 (31) |
5 (15) |
0.238 |
| Community-acquired pneumonia |
19 (29) |
8 (25) |
11 (34) |
0.584 |
| Hospital acquired pneumonia |
24 (37) |
16 (50) |
8 (25) |
0.071 |
| Congestive heart failure |
4 (6) |
2 (6) |
2 (6) |
>0.999 |
| Neurologic failure |
7 (10) |
2 (6) |
5 (15) |
0.426 |
| Poisoning |
3 (4) |
2 (6) |
1 (3) |
>0.999 |
| Soft tissue infetion | 2 (3) | 0 | 2 (6) | 0,492 |
Data are frequencies (%) or median (Interquartile range).
SAPS, simplified acute physiology score; LOD, logistic organ dysfunction; COPD, chronic obstructive pulmonary disease; ARDS, acute respiratory distress syndrome. Some patients had more than one cause for ICU admission.
*P values are for comparisons of tapered with cylindrical cuff.
Table 2.
Patient characteristics during the 48 hours following randomization
|
Variables |
Continuous control of P
cuff
n = 64 |
Routine care n = 64 |
p |
Continuous control of P
cuff
n = 64 |
p |
Routine care n = 64 |
p |
||
|---|---|---|---|---|---|---|---|---|---|
| Tapered cuff n = 32 | Cylindrical cuff n = 32 | Tapered cuff n = 32 | Cylindrical cuff n = 32 | ||||||
| Quantity of enteral nutrition, ml/day |
1000 |
1000 |
0.433 |
1000 |
1000 |
0.960 |
1000 |
1000 |
0.241 |
| (500–1000) |
(500–1500) |
(500–1000) |
(500–1000) |
(500–1000) |
(500–1500) |
||||
| Gastric residual volume, ml |
0 (0–20) |
0 (0–20) |
0.871 |
0 (0–15) |
0 (0–27) |
0.726 |
0 (0–60) |
0 (0–5) |
0.294 |
| Sedation |
28 (43) |
29 (45) |
> 0.999 |
14 (43) |
14 (43) |
>0.999 |
15 (46) |
14 (43) |
>0.999 |
| Ramsay score |
2 (2–3) |
2 (2–3) |
0.641 |
2 (2–3) |
2 (2–3) |
0.718 |
2 (2–3) |
2 (2–3) |
0.729 |
| Neuromuscular blocking agent use |
6 (9) |
7 (10) |
> 0.999 |
3 (9) |
3 (9) |
>0.999 |
3 (9) |
4 (12) |
>0.999 |
| Glasgow coma score |
14 (10–15) |
15 (10–15) |
0.310 |
13 (10–15) |
14 (8–15) |
0.738 |
14 (10–15) |
15 (8–15) |
0.908 |
| PEEP |
6 (5–8) |
6 (5–9) |
0.943 |
6 (5–8) |
7 (5–9) |
0.234 |
6 (5–9) |
7 (5–9) |
0.166 |
| Ventilatory mode |
|
|
0.329 |
|
|
0.885 |
|
|
0.433 |
| ACV |
36 (56) |
37 (57) |
|
18 (56) |
18 (56) |
|
21 (65) |
16 (50) |
|
| PSV |
23 (35) |
25 (39) |
|
11 (34) |
12 (37) |
|
10 (31) |
15 (46) |
|
| BPPV |
5 (7) |
2 (3) |
|
3 (9) |
2 (6) |
|
1 (3) |
1 (3) |
|
| Stress ulcer prophylaxis or treatment |
|
|
>0.999 |
|
|
0.688 |
|
|
0.109 |
| Sucralfate |
32 (50) |
32 (50) |
|
15 (46) |
17 (53) |
|
13 (40) |
19 (59) |
|
| Proton pump inhibitors |
25 (39) |
25 (39) |
|
13 (40) |
12 (37) |
|
13 (40) |
12 (37) |
|
| Prokinetic drugs |
12 (18) |
12 (18) |
> 0.999 |
6 (18) |
6 (18) |
>0.999 |
7 (21) |
5 (15) |
0.749 |
| Vomiting |
3 (4) |
1 (1) |
0.625 |
0 |
3 (9) |
0.237 |
1 (3) |
0 |
>0.999 |
| Head-of-bed position | 40 (35–40) | 40 (35–40) | 0.846 | 40 (35–45) | 40 (35–40) | 0.602 | 40 (35–40) | 40 (35–45) | 0.244 |
Data are frequencies (%) or median (Interquartile range).
Pcuff, cuff pressure; PEEP, positive end-expiratory pressure; ACV, assist-control ventilation; PSV, pressure support ventilation; BPPV, bilevel positive pressure ventilation.
Continuous control versus routine care of tracheal cuff
The pneumatic device was efficient in controlling Pcuff. Percentage of patients with underinflation or overinflation of tracheal cuff, coefficient of variation of Pcuff, and percentage of time spent with underinflation and overinflation of tracheal cuff were significantly lower during continuous control of Pcuff compared with routine care. Pcuff, and percentage of time spent with Pcuff 20–30 cmH2O were significantly higher during continuous control of Pcuff compared with routine control. No significant difference was found in rate of microaspiration of gastric content, mean pepsin level, or percentage of tracheal aspirates positive for pepsin between continuous control of Pcuff and routine care (Table 3). No significant interaction was found between continuous control of Pcuff and cuff shape (p = 0.93).
Table 3.
Impact of the pneumatic device on tracheal cuff pressure and microaspiration of gastric content
| Variables | Continuous control of P cuff n = 64 | Routine care n = 64 | p | OR (95% CI) |
|---|---|---|---|---|
| Recording duration, h |
24 (23–24) |
24 (23–24) |
0.198 |
|
| Mean airway pressure, cm H2O |
13 (11–18) |
13 (11–17) |
0.216 |
|
| Mean Pcuff, cm H2O |
26 (24–28) |
22 (20–28) |
0.017 |
|
| Coefficient of Pcuff variation, % |
5 (3–12) |
19 (15–30) |
<0.001 |
|
| Pcuff 20-30 cm H2O |
|
|
|
|
| yes |
64 (100) |
64 (100) |
NA |
|
| % of recording time |
95 (70–99) |
44 (30–59) |
<0.001 |
|
| Pcuff <20 or >30, cm H2O |
|
|
|
|
| Yes |
41 (66) |
64 (100) |
<0.001 |
|
| Duration >30 min |
33 (51) |
64 (100) |
<0.001 |
|
| Pcuff <20, cm H2O |
|
|
|
|
| Yes |
19 (29) |
60 (93) |
<0.001 |
1.46 (1.23-1.73) |
| Duration > 30 min |
16 (25) |
57 (89) |
<0.001 |
2.63 (1.11-6.21) |
| % of recording time |
0.01 (0–2) |
32 (9–54) |
<0.001 |
|
| Pcuff >30, cm H2O |
|
|
|
|
| Yes |
33 (51) |
62 (96) |
0.001 |
1.57 (1.10-2.24) |
| Duration >30 min |
25 (39) |
54 (84) |
<0.001 |
1.50 (1.11-2.20 |
| % of recording time |
0.9 (0–17) |
14 (4–30) |
<0.001 |
|
| Microaspiration of gastric content |
32 (50) |
38 (59) |
0.238 |
|
| Pepsin, ng/mL |
185 (113–296) |
203 (120–338) |
0.171 |
|
| % of tracheal aspirates positive for pepsin | 29 (0–74) | 45 (0–100) | 0.162 |
Data are frequencies (%) or median (Interquartile range). Pcuff, cuff pressure.
Yes indicates that a patient had the variable at least once.
Tapered versus cylindrical cuff shape during continuous control of Pcuff
During continuous control of Pcuff, percentage of patients with underinflation of tracheal cuff >30 minutes was significantly lower in patients intubated with tapered-cuffed tracheal tubes compared with those intubated with cylindrical-cuffed tracheal tubes. No significant difference was found in terms of Pcuff, percentage of patients with underinflation or overinflation, coefficient of variation of Pcuff, and percentage of time spent with underinflation or overinflation between the two groups during the same period (Table 4).
Table 4.
Impact of cuff shape on cuff pressure and microaspiration during continuous control of cuff pressure and routine care
|
Variables |
Continuous control of P
cuff
n = 64 |
p |
Routine care n = 64 |
p |
||
|---|---|---|---|---|---|---|
| Tapered cuff n = 32 | Cylindrical cuff n = 32 | Tapered cuff n = 32 | Cylindrical cuff n = 32 | |||
| Recording duration, h |
24 (23–24) |
24 (23–25) |
0.662 |
24 (23–25) |
24 (23–24) |
0.229 |
| Mean airway pressure, cm H2O |
13 (10–18) |
13 (11–16) |
0.749 |
12 (10–20) |
15 (11–15) |
0.214 |
| Mean Pcuff, cm H2O |
26 (25–28) |
25 (23–28) |
0.844 |
21 (19–26) |
24 (21–30) |
0.143 |
| Coefficient of Pcuff variation, % |
5 (3–9) |
6 (3–15) |
0.382 |
18 (15–30) |
20 (14–39) |
0.789 |
| Pcuff 20-30 cm H2O |
|
|
|
|
|
|
| yes |
32 (100) |
32 (100) |
NA |
32 (100) |
32 (100) |
NA |
| % of recording time |
97 (82–99) |
88 (56–99) |
0.147 |
42 (30–62) |
44 (29–57) |
0.811 |
| Pcuff <20 or >30 cm H2O |
|
|
|
|
|
|
| Yes |
19 (59) |
22 (68) |
0.856 |
32 (100) |
32 (100) |
>0.999 |
| Duration >30 min |
14 (43) |
19 (59) |
0.455 |
30 (93) |
32 (100) |
>0.999 |
| Pcuff <20 cm H2O |
|
|
|
|
|
|
| Yes |
6 (18) |
13 (40) |
0.116 |
29 (90) |
31 (96) |
>0.999 |
| Duration > 30 min |
3 (9) |
13 (40) |
0.011* |
29 (90) |
28 (87) |
0.371 |
| % of recording time |
0 (0–0) |
0 (0–12) |
0.549 |
41 (17–62) |
21 (8–47) |
0.049 |
| Pcuff >30 cm H2O |
|
|
|
|
|
|
| Yes |
15 (46) |
18 (56) |
0.903 |
31 (96) |
31 (96) |
>0.999 |
| Duration >30 min |
12 (37) |
13 (40) |
>0.999 |
24 (75) |
30 (93) |
0.235 |
| % of recording time |
0.6 (0–24) |
1.4 (0–48) |
0.652 |
11 (2–17) |
20 (6–18) |
0.031 |
| Microaspiration of gastric content |
13 (40) |
19 (59) |
0.211 |
18 (56) |
20 (62) |
0.799 |
| Pepsin, ng/mL |
154 (105–230) |
214 (126–466) |
0.066 |
175 (121–252) |
238 (101–664) |
0.238 |
| % of tracheal aspirates positive for pepsin | 0 (0–57) | 43 (0–100) | 0.073 | 40 (0–86) | 50 (0–100) | 0.310 |
Data are frequencies (%) or median (Interquartile range).
Pcuff, cuff pressure. Yes indicates that a patient had the variable at least once.
*OR (95% CI) 3.20 (1.12-9.12).
Tapered versus cylindrical cuff shape during routine care of Pcuff
During routine care, percentage of time spent with underinflation of tracheal cuff was significantly higher, and percentage of time spent with overinflation of tracheal cuff was significantly lower in patients intubated with tapered-cuffed tracheal tubes compared with those intubated with cylindrical-cuffed tracheal tubes. No significant difference was found in coefficient of variation of Pcuff, or percentage of patients with underinflation or overinflation of tracheal cuff between the two groups during the same period (Table 4).
Impact of cuff shape on microaspiration
No significant difference was found in microaspiration of gastric content rate, mean pepsin level or percentage of tracheal aspirates positive for pepsin between patients intubated with tapered-cuffed tracheal tubes and those intubated with cylindrical-cuffed tracheal tubes during continuous control of Pcuff or routine care (Table 4).
Other results
During continuous control of Pcuff, important condensation was observed in the pilot balloon in 7 (22%) patients intubated with tapered-cuffed tracheal tube compared with 10 (31%) patients intubated with cylindrical-cuffed tracheal tube (p = 0.571).
No significant difference was found in percentage of time spent with underinflation (median [IQR] 0.07% [0.0004-16] versus 0.01% [0.0003-0.6], p = 0.359), or overinflation of tracheal cuff (6% [0.27-37] versus 0.34% [0.02-11]) between patients with high airway pressures (n = 16) and those with lower airway pressures (n = 48), respectively.
Discussion
The percentage of patients with underinflation or overinflation of tracheal cuff, percentage of time spent with underinflation or overinflation of tracheal cuff, and coefficient of variation of Pcuff were significantly lower during continuous control of Pcuff compared with routine care. Further, percentage of time spent with Pcuff 20–30 cmH2O, and mean Pcuff were significantly higher during continuous control of Pcuff compared with routine care. However, no significant difference was found in the incidence of microaspiration of gastric content between continuous control of Pcuff compared with routine care or between patients intubated with tapered-cuffed tracheal tubes and those intubated with cylindrical-cuffed tracheal tubes.
To our knowledge, our study is the first to demonstrate the efficiency of the pneumatic device in controlling Pcuff in critically-ill patients intubated with polyurethane-cuffed tracheal tubes. Previous studies found similar results in animals and humans intubated with polyvinyl chloride-cuffed tracheal tubes [20,21]. The percentage of patients with underinflation of tracheal cuff >30 minutes during continuous control of Pcuff was relatively high (25%). This could be explained by the physicochemical characteristics of polyurethane, namely its hydrophilic aspect, resulting in condensation formation especially during continuous control of Pcuff. In our study, small condensation formation was rarely observed in the pilot balloon during routine care of Pcuff. However, important condensation formation filling the whole pilot balloon was frequently observed during continuous control of Pcuff. The fact that evaporation is probably reduced in closed circuit during continuous control of Pcuff might explain this difference in condensation formation between routine care and continuous control of Pcuff. Further studies directly comparing efficiency of the pneumatic device in polyurethane and polyvinyl chloride-cuffed tracheal tubes are needed to confirm our results. Although previous studies have demonstrated the efficiency of the pneumatic device in controlling Pcuff in patients intubated with PVC-cuffed tracheal tubes, the current study allow the generalization of this observation to patients intubated with polyurethane-cuffed tracheal tubes. Given the growing evidence supporting the use of polyurethane-cuffed tracheal tubes to prevent microaspiration and VAP, our results are necessary before performing further studies aiming to evaluate the combined beneficial effects of using polyurethane-cuffed tracheal tubes and continuous control of Pcuff in preventing VAP.
In spite of efficient control of Pcuff, no significant difference was found in microaspiration of gastric content between continuous control of Pcuff and routine care. One potential explanation for this result is the optimal routine care provided during the study, and the use of polyurethane-cuffed tracheal tubes. These tubes have been demonstrated to significantly reduce microaspiration in critically ill patients [5,6]. Further, our study is probably underpowered to detect such an effect, since microaspiration of gastric content was a secondary outcome and the number of included patients was calculated based on the primary outcome. Further studies are needed to determine the impact of continuous control of Pcuff on the incidence of microaspiration, and VAP. However, whilst our study was underpowered to detect a difference in microaspiration, it was correctly powered to draw a valuable conclusion on primary outcome, i.e. the efficiency of the pneumatic device in controlling Pcuff. In fact, the number of patients required to detect the estimated difference in percentage of patients with underinflation or overinflation of Pcuff, with an alpha risk of 5% and a power of 80%, was 32 per group. As 32 patients were included in each study group, our study is sufficiently powered to conclude that the pneumatic device is efficient in controlling Pcuff. This result would allow future studies to evaluate the impact of the pneumatic device on the prevention of complications related to underinflation and overinflation of Pcuff. Although our previous study has already suggested beneficial effects of continuous control of Pcuff in reducing microaspiration and VAP [18], it was conducted in patients intubated with PVC-cuffed tracheal tubes. Therefore, these results could not be generalized to patients intubated with polyurethane-cuffed tracheal tubes. Further studies with larger sample size are required in these patients to determine the impact of continuous control of Pcuff on prevention of cuff-related complications such as microaspiration, and VAP.
Some significant differences, including percentage of time with underinflation and overinflation were found between patients intubated with tapered-cuffed tracheal tubes compared with those intubated with cylindrical-cuffed tracheal tubes. These differences could be explained by different cuff shape between the two groups. No significant effect was found of tracheal cuff shape on microaspiration of gastric content. However, during continuous control of Pcuff a trend towards lower pepsin level and percentage of tracheal aspirates positive for pepsin was found in patients intubated with tapered-cuffed tracheal tubes compared with those intubated with cylindrical-cuffed tracheal tubes. Further, in spite of significantly higher percentage of time spent with underinflation of tracheal cuff in patients intubated with tapered-cuffed tracheal tubes compared with those intubated with cylindrical-cuffed tracheal tubes during routine care, microaspiration of gastric content rate was similar in the two groups. This result also suggests better sealing with tapered compared with cylindrical tracheal cuffs. However, our study was probably underpowered to detect a significant difference in microaspiration rate between the two groups.
Two recent in vitro studies found tapered-shaped tube cuff to considerably improve sealing characteristics of polyvinyl chloride tube cuffs [11,13]. However, no significant effect of the tapered-shaped cuff was found in polyurethane tube cuffs. In contrast, another in vitro study reported that tapered polyurethane cuff was more efficient than cylindrical polyurethane cuff in larger tracheal diameter in preventing fluid leakage [12]. Different study design might explain these conflicting results. In a prospective observational before-after study, our group found no significant difference in microaspiration of gastric content between patients intubated with tapered polyurethane-cuffed tracheal tubes compared with those intubated with cylindrical polyurethane-cuffed tracheal tubes [6]. Further clinical studies are required to determine the impact of tracheal cuff shape on the incidence of microaspiration, and VAP.
No significant difference was found in airway pressures between patients intubated with tapered compared with those intubated with cylindrical tracheal cuffs. Previous studies demonstrated that Pcuff was tightly correlated to airway pressure [22,23]. The relatively low airway pressures found in study patients were similar as those previously reported in other ICU patients [6,24,25]. This might strengthen our findings, since these results could be generalized to patients with similar airway pressure. Percentage of time spent with underinflation, and overinflation of Pcuff during continuous control of Pcuff was not significantly different between patients with high airway pressures and those with lower airway pressures, suggesting that the pneumatic device is efficient in patients with high airway pressures, such as those with severe asthma or ARDS. However, no definite conclusion could be drawn in this subgroup because of the small number of patients (n = 16).
Our study has some limitations. First, this study was performed in a single ICU. Therefore, our results could not be generalized to other ICU patients. Second, our study did not evaluate the impact of continuous control of Pcuff on outcomes such as VAP or tracheal injury. However, in order to adjust for patient-related confounders, such as tracheal size and aspect, airway pressures, and tracheal tube size, continuous control and routine care of Pcuff were performed in the same patient. Therefore, it was not possible to evaluate these outcomes. Further, it was mandatory to evaluate the efficiency of the device in controlling Pcuff before performing studies on its impact on prevention of complications. Finally, randomization for tracheal cuff shape was performed per period and not per patient. However, intubation is often an urgent procedure. Therefore, it is very difficult to perform randomization per patient in such a study. In addition, the impact of cuff shape on microaspiration was a secondary outcome.
Conclusion
We conclude that the pneumatic device is efficient in controlling Pcuff in critically ill patients intubated with polyurethane-cuffed tracheal tube. Further studies are needed to determine the impact of continuous control of Pcuff and tracheal cuff shape on microaspiration, VAP, and tracheal injury.
Key messages
• The pneumatic device is efficient in controlling Pcuff in critically ill patients intubated with polyurethane-cuffed tracheal tube.
• Conical cuff shape could be beneficial in preventing microaspiration in critically ill patients.
• Further studies are needed to determine the impact of continuous control of Pcuff and tracheal cuff shape on microaspiration, and VAP in patients intubated with polyurethane-cuffed tracheal tubes.
Abbreviations
ICU: Intensive care unit; Pcuff: Cuff pressure; VAP: Ventilator-associated pneumonia.
Competing interests
SN: Covidien (advisory board), other authors: none.
Authors’ contribution
EJ, ADur, and SN designed this study. EJ, FZ, JD, MB, and SN collected the data. ADuh performed statistical analyses. EJ, and SN wrote the manuscript, and all authors participated in its critical revision. EJ, and SN had full access to all data in the study and had final responsibility for the decision to submit for publication. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Emmanuelle Jaillette, Email: emmanuelle.jaillette@chru-lille.fr.
Farid Zerimech, Email: farid.zerimech@chru-lille.fr.
Julien De Jonckheere, Email: j.dejonckheere@hotmail.fr.
Demosthenes Makris, Email: appollon7@hotmail.com.
Malika Balduyck, Email: malika.balduyck@chru-lille.fr.
Alain Durocher, Email: alain.durocher@chru-lille.fr.
Alain Duhamel, Email: ALAIN.DUHAMEL@UNIV-LILLE2.FR.
Saad Nseir, Email: s-nseir@chru-lille.fr.
Acknowledgements
The authors would like to thank Mrs. Catherine Lelorne, Mrs. Véronique Lemaire and Mrs. Nadine Parsy for their skilful assistance in pepsin measurement.
Financial support
Covidien and Kimberly-Clark donated tracheal tubes used in this study. None of these companies had any role in the design, study conduct, data analyses or reporting.
References
- Nseir S, Zerimech F, Jaillette E, Artru F, Balduyck M. Microaspiration in intubated critically ill patients: diagnosis and prevention. Infect Disor Drug Target. 2011;13:413–423. doi: 10.2174/187152611796504827. [DOI] [PubMed] [Google Scholar]
- Craven DE, Chroneou A, Zias N, Hjalmarson KI. Ventilator-associated tracheobronchitis: the impact of targeted antibiotic therapy on patient outcomes. Chest. 2009;13:521–528. doi: 10.1378/chest.08-1617. [DOI] [PubMed] [Google Scholar]
- Bouadma L, Wolff M, Lucet J-C. Ventilator-associated pneumonia and its prevention. Curr Opin Infect Dis. 2012;13:395–404. doi: 10.1097/QCO.0b013e328355a835. [DOI] [PubMed] [Google Scholar]
- Coppadoro A, Bittner E, Berra L. Novel preventive strategies for ventilator-associated pneumonia. Crit Care. 2012;13:210. doi: 10.1186/cc11225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucangelo U, Zin WA, Antonaglia V, Petrucci L, Viviani M, Buscema G, Borelli M, Berlot G. Effect of positive expiratory pressure and type of tracheal cuff on the incidence of aspiration in mechanically ventilated patients in an intensive care unit. Crit Care Med. 2008;13:409–413. doi: 10.1097/01.CCM.0000297888.82492.31. [DOI] [PubMed] [Google Scholar]
- Nseir S, Zerimech F, De Jonckheere J, Alves I, Balduyck M, Durocher A. Impact of polyurethane on variations in tracheal cuff pressure in critically ill patients: a prospective observational study. Intensive Care Med. 2010;13:1156–1163. doi: 10.1007/s00134-010-1892-7. [DOI] [PubMed] [Google Scholar]
- Dullenkopf A, Gerber A, Weiss M. Fluid leakage past tracheal tube cuffs: evaluation of the new Microcuff endotracheal tube. Intensive Care Med. 2003;13:1849–1853. doi: 10.1007/s00134-003-1933-6. [DOI] [PubMed] [Google Scholar]
- Lorente L, Lecuona M, Jiménez A, Mora ML, Sierra A. Influence of an endotracheal tube with polyurethane cuff and subglottic secretion drainage on pneumonia. Am J Respir Crit Care Med. 2007;13:1079–1083. doi: 10.1164/rccm.200705-761OC. [DOI] [PubMed] [Google Scholar]
- Poelaert J, Depuydt P, De Wolf A, Van de Velde S, Herck I, Blot S. Polyurethane cuffed endotracheal tubes to prevent early postoperative pneumonia after cardiac surgery: a pilot study. J Thor Cardiovascular Surg. 2008;13:771–776. doi: 10.1016/j.jtcvs.2007.08.052. [DOI] [PubMed] [Google Scholar]
- Miller MA, Arndt JL, Konkle MA, Chenoweth CE, Iwashyna TJ, Flaherty KR, Hyzy RC. A polyurethane cuffed endotracheal tube is associated with decreased rates of ventilator-associated pneumonia. J Crit Care. 2011;13:280–286. doi: 10.1016/j.jcrc.2010.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madjdpour C, Mauch J, Dave MH, Spielmann N, Weiss M. Comparison of air-sealing characteristics of tapered- vs. cylindrical-shaped high-volume, low-pressure tube cuffs. Acta Anaesthesiol Scand. 2012;13:230–235. doi: 10.1111/j.1399-6576.2011.02542.x. [DOI] [PubMed] [Google Scholar]
- Dave MH, Frotzler A, Spielmann N, Madjdpour C, Weiss M. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Brit J Anaesthesia. 2010;13:538–543. doi: 10.1093/bja/aeq202. [DOI] [PubMed] [Google Scholar]
- Zanella A, Scaravilli V, Isgrò S, Milan M, Cressoni M, Patroniti N, Fumagalli R, Pesenti A. Fluid leakage across tracheal tube cuff, effect of different cuff material, shape, and positive expiratory pressure: a bench-top study. Intensive Care Med. 2011;13:343–347. doi: 10.1007/s00134-010-2106-z. [DOI] [PubMed] [Google Scholar]
- Young PJ, Rollinson M, Downward G, Henderson S. Leakage of fluid past the tracheal tube cuff in a benchtop model. Brit J Anaesthesia. 1997;13:557–562. doi: 10.1093/bja/78.5.557. [DOI] [PubMed] [Google Scholar]
- Rello J, Soñora R, Jubert P, Artigas A, Rué M, Vallés J. Pneumonia in intubated patients: role of respiratory airway care. Am J Respir Crit Care Med. 1996;13:111–115. doi: 10.1164/ajrccm.154.1.8680665. [DOI] [PubMed] [Google Scholar]
- Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Brit Med J. 1984;13:965–968. doi: 10.1136/bmj.288.6422.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nseir S, Brisson H, Marquette C-H, Chaud P, Di Pompeo C, Diarra M, Durocher A. Variations in endotracheal cuff pressure in intubated critically ill patients: prevalence and risk factors. Eur J Anaesthsiol. 2009;13:229–234. doi: 10.1097/EJA.0b013e3283222b6e. [DOI] [PubMed] [Google Scholar]
- Nseir S, Zerimech F, Fournier C, Lubret R, Ramon P, Durocher A, Balduyck M. Continuous control of tracheal cuff pressure and microaspiration of gastric contents in critically ill patients. Am J Respir Crit Care Med. 2011;13:1041–1047. doi: 10.1164/rccm.201104-0630OC. [DOI] [PubMed] [Google Scholar]
- Chastre J, Bedock B, Clair B, Gehanno P, Lacaze T, Lesieur O, Picart-Jacq JY, Plaisance P, Ravussin P, Samain E. et al. Quel abord trachéal pour la ventilation mécanique des malades de réanimation? (à l’exclusion du nouveau né) Reanimation. 1998;13:438–442. [Google Scholar]
- Duguet A, D’Amico L, Biondi G, Prodanovic H, Gonzalez-Bermejo J, Similowski T. Control of tracheal cuff pressure: a pilot study using a pneumatic device. Intensive Care Med. 2007;13:128–132. doi: 10.1007/s00134-006-0417-x. [DOI] [PubMed] [Google Scholar]
- Nseir S, Duguet A, Copin M-C, De Jonckheere J, Zhang M, Similowski T, Marquette C-H. Continuous control of endotracheal cuff pressure and tracheal wall damage: a randomized controlled animal study. Crit Care. 2007;13:R109. doi: 10.1186/cc6142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyton DC, Barlow MR, Besselievre TR. Influence of airway pressure on minimum occlusive endotracheal tube cuff pressure. Crit Care Med. 1997;13:91–94. doi: 10.1097/00003246-199701000-00018. [DOI] [PubMed] [Google Scholar]
- Blanch PB. Laboratory evaluation of 4 brands of endotracheal tube cuff inflator. Respir Care. 2004;13:166–173. [PubMed] [Google Scholar]
- Valta P, Corbeil C, Chassé M, Braidy J, Milic-Emili J. Mean airway pressure as an index of mean alveolar pressure. Am J Respir Crit Care Med. 1996;13:1825–1830. doi: 10.1164/ajrccm.153.6.8665041. [DOI] [PubMed] [Google Scholar]
- Sole ML, Su X, Talbert S, Penoyer DA, Kalita S, Jimenez E, Ludy JE, Bennett M. Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. Am J Crit Care. 2011;13:109–117. doi: 10.4037/ajcc2011661. [DOI] [PMC free article] [PubMed] [Google Scholar]


