SUMMARY
Objective
Although the advent of ablation technology has simplified and shortened surgery for atrial fibrillation, only bipolar clamps have reliably been able to create transmural lesions on the beating heart. Currently there are no devices capable of reproducibly creating the long linear lesions in the right and left atria needed to perform a Cox-Maze procedure. This study evaluated the performance of a novel suction-assisted radiofrequency device that uses both bipolar and monopolar energy to create lesions from an epicardial approach on the beating heart.
Methods
Six domestic pigs underwent median sternotomy. A dual bipolar/monopolar radiofrequency ablation device was used to create epicardial linear lesions on the superior and inferior vena cavae, right and left atrial free walls, and right and left atrial appendages. The heart was stained with 2,3,5-triphenyl-tetrazolium chloride and each lesion was cross-sectioned at 5mm intervals. Lesion depth and transmurality were determined.
Results
Transmurality was documented in 94% of all cross-sections, and 68% of all ablation lines were transmural along their entire length. Tissue thickness was not different between transmural and non-transmural cross-sections (3.1 ± 1.3 and 3.4 ± 2.1, p=0.57, respectively), nor was the anatomic location on the heart (p=0.45 for the distribution). Of the cross-sections located at the end of the ablation line, 11% (8/75) were found to be non-transmural, whereas only 4% (8/195) of cross-sections located within the line of ablation were found to be non-transmural (p=0.04). Logistic regression analysis demonstrated that failure of the device to create transmural lesions was associated with low body temperature (p=0.006), but not with cardiac output (p=0.54).
Conclusions
This novel device was able to consistently create transmural epicardial lesions on the beating heart, regardless of anatomic location, cardiac output or tissue thickness. The performance of this device was improved over most devices previously tested, but still falls short of ideal clinical performance. Transmurality was lower at the end of the lesions, highlighting the importance of overlapping lines of ablation in the clinical setting.
Keywords: arrhythmia therapy, epicardial ablation, radiofrequency device, transmurality
INTRODUCTION
The Cox-Maze (CM) procedure was first performed in 1987 by Dr. James L. Cox.1 After several iterations, the Cox-Maze III procedure was introduced, and became the gold standard operation for the treatment of atrial fibrillation (AF).2 Despite its success, this traditional “cut and sew” CM procedure was not widely adopted due to its technical complexity and required time on cardiopulmonary bypass.
The development of surgical ablation technologies has simplified the surgical treatment of AF. With the advent of ablation technology, it has become possible to replace most of the standard lesions of the original CM procedure with lines of ablation, making the procedure simpler and faster to perform.3 Multiple energy sources, including radiofrequency (RF), microwave, cryoablation, and high intensity focused ultrasound, have been used to create lesions with varying degrees of success.4–8 Our group has demonstrated the ability of bipolar RF clamps to reliably create transmural lesions in chronic animal models and, as such, has predominantly used this technology in the clinical setting.9–13
The Cox-Maze IV (CMIV) procedure, which combines bipolar radiofrequency (RF) ablation and cryoablation to replace most of the traditional atrial incisions of the CM lesion set, was introduced by our group in 2002.14 The utilization of ablation technology simplified the procedure, shortened operative duration, allowed for minimal-access techniques, and maintained the success of the CM III, with 89% freedom from AF and 78% freedom from AF off of antiarrhythmic medications at one year.3 However, despite its many improvements, the CMIV still requires cardiopulmonary bypass since the bipolar clamps require an arrested heart to create the left atrial lesion set.
The introduction of epicardial ablation technology attempts to address these issues by allowing linear lines of ablation to be placed through minimal-access techniques on the epicardial surface of the beating heart. Unfortunately, the inability of these devices to reliably create transmural lesions on the beating heart has limited their clinical application.7 Unlike the bipolar RF clamps, these technologies have been ineffective for a number of reasons. One major problem is that the endocardial surface is protected from thermal injury due to the heat sink of the circulating cavitary blood pool.15 Other issues that have been implicated in the shortcomings of epicardial ablation technology include the anatomic variability of pathologic atria, poor tissue-device contact, and the deficiencies of the particular technology.
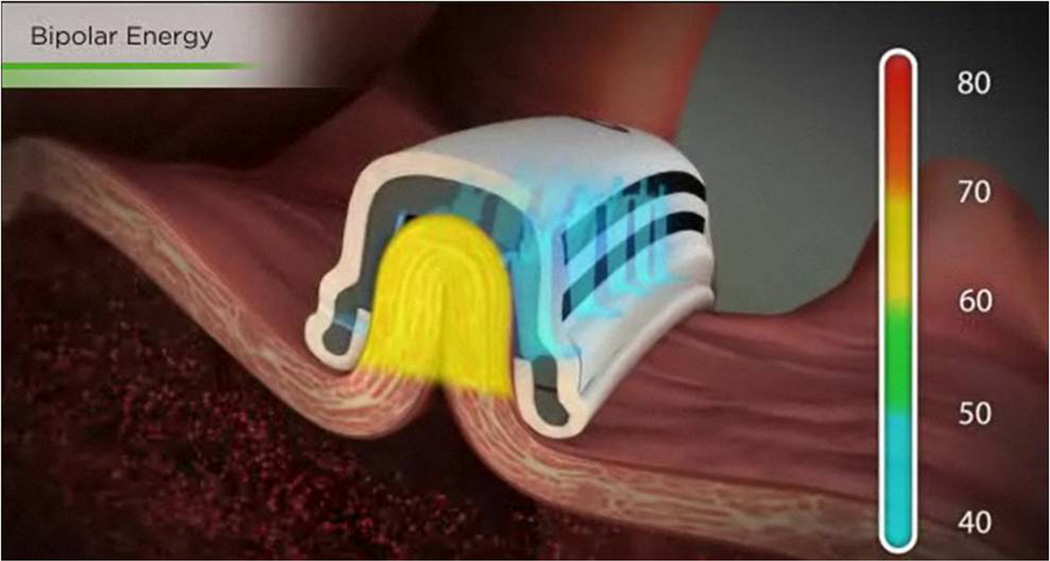
To overcome these shortcomings, a novel epicardial RF ablation system (Cobra Fusion™, Estech, San Ramon, CA USA) was developed (Figure 1). Unlike previous devices, this technology delivers both monopolar and bipolar energy via a temperature-controlled ablation algorithm in an attempt to eliminate the heat sink of the endocavitary blood pool from an epicardial approach. The present study was designed to test the ability of this novel RF ablation device to create contiguous linear lines of ablation on the beating heart in an acute porcine study using an epicardial approach.
Figure 1.
The Cobra Fusion Surgical Ablation System is a suction-assisted epicardial ablation system that delivers both monopolar and bipolar radiofrequency energy via a temperature-controlled ablation algorithm.
METHODS
This study was approved by the Washington University School of Medicine institutional review board for animal research. All animals received humane care in compliance with the “Guide for the Care and Use of Laboratory Animals” published by the National Institutes of Health (publication no. 85-23, revised 1985).
Device Specifications
The Cobra Fusion Surgical Ablation System™ (Estech, San Ramon, CA USA) consists of two suction-assisted epicardial RF ablation catheters that deliver both monopolar and bipolar energy. Two ablation systems are available: a six-electrode 150 mm ablation catheter designed to position the device around the pulmonary veins, and a 50 mm ablation catheter, which contains two 50-Watt electrodes that terminate 5 mm from the end of the suction chamber. In this study, the 50 mm catheter was used because the 150 mm device does not conform to the anatomic constraints of the porcine atria. The ablation system also includes an Electrosurgical Unit (ESU), which provides power to the ablation catheter via a cable permanently attached to the handle, as well as a vacuum source controlled via a three-way stopcock that attaches to the ablation catheter via accessory tubing. Once the ablation catheter is affixed to the tissue, suction is maintained at −500 mm Hg throughout the ablation algorithm.
Unlike other commercially-available RF ablation devices which use impedance algorithms, this device uses a temperature-controlled heating algorithm that employs two thermocouples per electrode, sampled at 20ms intervals with real-time feedback to power, in order to attain and maintain the target temperature of 70°C.16 Further, using temperature-controlled ablation prevents char formation on the tissue-electrode interface, which can limit lesion depth. The settings employed in this investigation were identical to those recommended clinically by the manufacturer and included two separate 60-second tissue ablations, the first of which consisted of bipolar RF energy directed from the active RF electrodes toward the integrated indifferent electrodes on the other side of the device (Figure 2). Without disrupting the suction, the indifferent electrode pads are plugged into the receptacles on the ESU, and the device is then switched to monopolar mode by selecting the corresponding button on the device handle. Monopolar RF energy is subsequently directed from the active RF electrodes on the device toward the indifferent electrode pads on the subject’s back.
Figure 2.
When the device handle is set to bipolar mode, RF energy is directed from the active electrodes of the ablation catheter toward the integrated indifferent electrodes on the other side of the suction chamber.
Experimental Design
Six domestic pigs weighing between 70–90 kg were used for this study. Each animal was premedicated with intramuscular ketamine (2.2 mg/kg), telazole (4.4 mg/kg), and xylazine (2.2 mg/kg), intubated, and anesthetized with 2–4% inhaled isoflurane. The animals were maintained on a volume-limited respirator, and end-tidal carbon dioxide, body temperature, heart rate, respiratory rate, blood pressure, and oxygen saturation were continuously monitored. Indifferent electrodes for use with monopolar ablation were placed on the posterior aspect of the torso. Arterial blood gases, blood counts, and electrolytes were monitored every 30 minutes, and as needed throughout the procedure, via catheters in the femoral artery and vein.
A median sternotomy was performed and the heart supported in a pericardial cradle. The azygous vein was isolated and ligated, the ascending aorta was exposed, and flow probes were placed around the superior and inferior vena cavae for continuous monitoring of cardiac output. A baseline activated clotting time was measured before a heparin bolus was administered, and heparin was redosed as needed to maintain an activated clotting time >350 throughout the procedure. Amiodarone was administered via bolus and subsequent constant infusion (10–12 mg/kg and 0.5 mg/kg/hr, respectively) for episodes of stable AF. Direct current cardioversion was performed for episodes of unstable AF. Phenylephrine was administered via bolus and/or constant infusion (100µg and 1 µg/kg/min, respectively) to maintain systolic blood pressure in the acceptable range throughout the procedure.
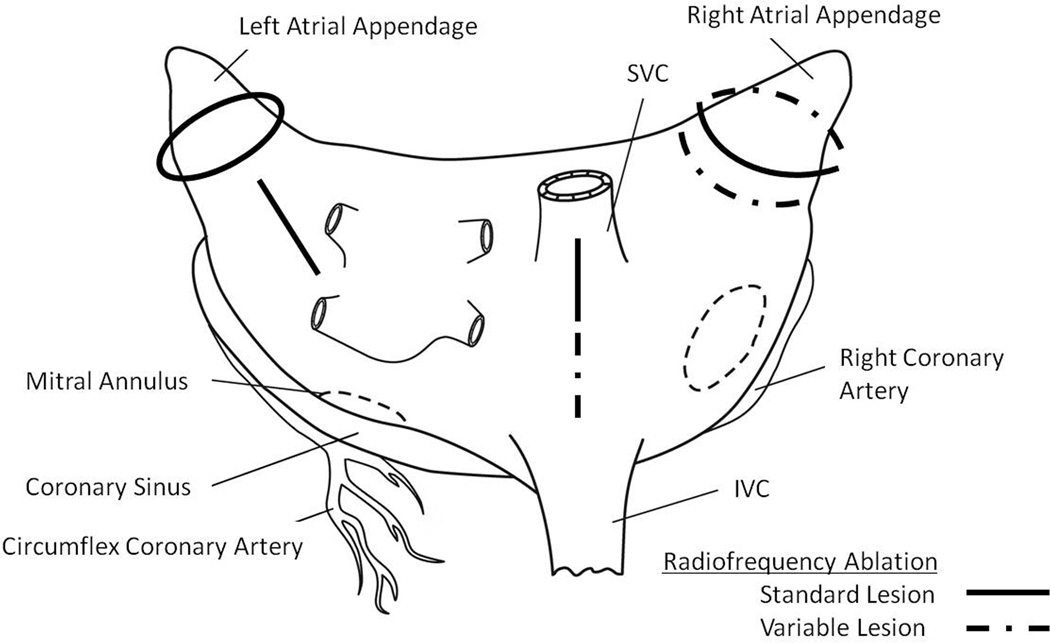
The experimental lesion set (Figure 3) was carried out using the Cobra Fusion 50mm Surgical Ablation System (Estech, San Ramon, CA USA) as described above. Five standard lesions were created in the following locations in every animal: anterior left atrial appendage, posterior left atrial appendage, left atrial free wall, posterior right atrial appendage and superior vena cava. In several animals, the anatomy was such that the superior vena cava lesion extended on to the superior portion of the inferior vena cava. According to the specific anatomy of the animal, an additional lesion was variably created either on the posterior right atrial appendage or, if space allowed, on the anterior right atrial appendage. Two 60-second tissue ablations were performed at each site as described previously. The goal temperature during both ablations was 70°C, and suction was maintained at −500 mm Hg throughout the ablation time. The maximum power obtained, the maximum and minimum temperatures obtained, and the presence of any temperature discrepancy >5°C between electrodes as measured by the ablation system were recorded for each ablation.
Figure 3.
Schematic diagram of the experimental lesion set. Solid black lines represent lesions that were performed in all animals. Dashed lines represent lesions that were performed variably on the animals, depending on individual anatomic considerations. IVC, inferior vena cava; SVC, superior vena cava
After the ablations were completed, the ends of each lesion were marked on the epicardial surface with 4-0 Prolene suture for later identification. The aorta was subsequently crossclamped and 60 ml of 2% 2, 3, 5-triphenyl-tetrazolium chloride solution (TTC) was perfused through the coronary circulation via infusion into the root of the aorta. The animal was then euthanized with antegrade infusion of 3M KCl. Postoperatively, the heart was excised en bloc and soaked in 1% TCC for 6–12 hours at 4°C in order to stain any viable myocardium.
After staining, the heart was evaluated macroscopically for evidence of charring, tissue rupture and blood coagulation. The individual lesions were excised and gross digital photography of the epicardial and endocardial surfaces was carried out in proximity to a caliper for later calibration. Large intracavitary trabeculae were divided prior to analysis. The lesions were subsequently cross-sectioned at 5mm intervals in a plane perpendicular to the long axis of the ablation line. The individual cross-sections were again digitally photographed in proximity to a caliper for later calibration. Lesion depth, lesion width, and tissue thickness were determined with commercial software (Adobe Photoshop, San Jose, CA USA).17 Tissue thickness was measured at the site of transmurality or at the site of deepest lesion penetration in the case of nontransmural lesions. Measurements of lesion depth and width included all of the unstained area, starting at the border of the pink halo region surrounding each lesion. Both the transmurality of each individual tissue cross-section and the transmurality of each 5 cm lesion created by the device were examined.
Statistical Analysis
Continuous and categorical variables are expressed as mean ± SD and as number and percent, respectively, unless otherwise specified. Comparisons were performed using a two-tailed, Student’s t-test for normally distributed, continuous variables and a Fisher’s exact test for categorical variables. Univariate logistic regression was performed on clinically relevant variables including tissue depth, body temperature, cardiac output, heart rate, systolic blood pressure, diastolic blood pressure, oxygen saturation, the maximum and minimum temperatures reached in both the bipolar and monopolar settings, and the maximum power reached in both the bipolar and monopolar settings in order to determine independent predictors of lesion transmurality. Data analyses were performed using Systat 13 (Systat Software, Inc., San Jose, CA USA). P-values less than 0.05 were considered statistically significant.
RESULTS
Ablation Characteristics
A total of 38 lesions and 270 tissue cross-sections were examined. There was no charring of the epicardial surface and no clot identified on the endocardial surface for any ablation. There were no atrial wall perforations identified intraoperatively or on subsequent photo analysis.
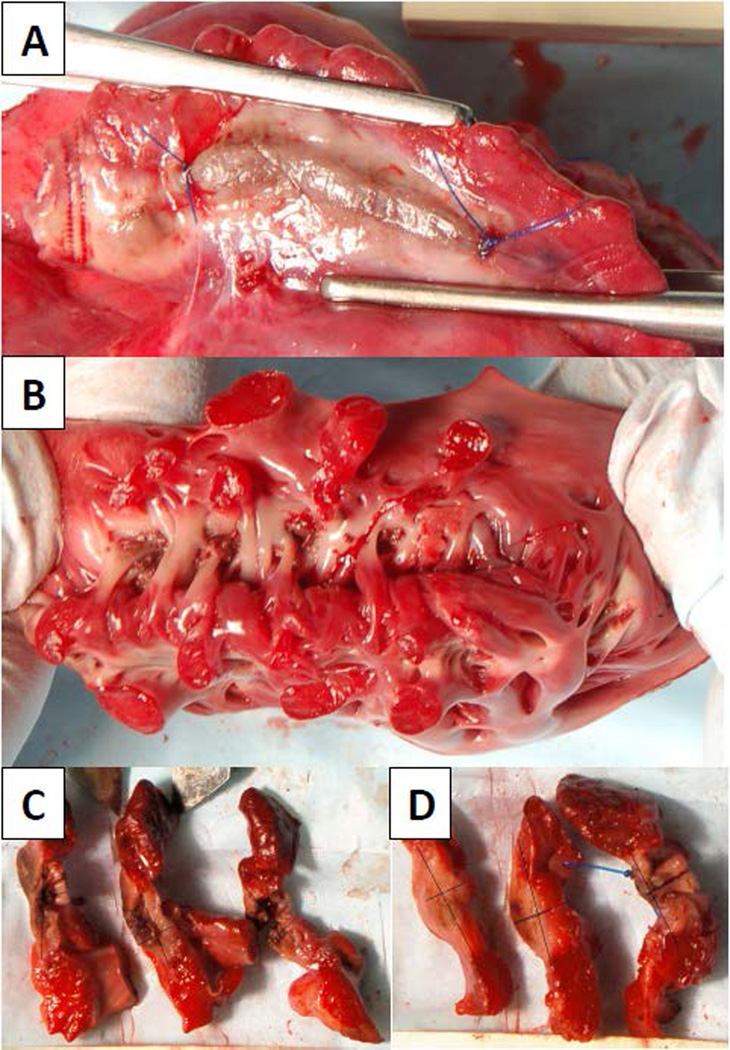
Representative photographs demonstrating the epicardial and endocardial surfaces of an intact lesion, as well as cross-sections of tissue found to have both transmural and non-transmural ablations, are demonstrated in Figure 4.
Figure 4.
Digital photographs demonstrating a representative ablation line from the (A) epicardial and (B) endocardial surfaces. After optimizing brightness and contrast, the digital photographs of the (C & D) cross-sections were marked for lesion depth and width. In total, 16 cross-sections were found to be non-trasmural (D, center cross-section).
The maximum power, and maximum and minimum temperatures obtained for each ablation were not significantly different between transmural and non-transmural lesions (Table 1). The lesion dimensions were also recorded for each ablation (Table 1). As expected, the average lesion depth was greater for transmural (3.1 ± 1.3 mm) versus non-transmural lesions (2.2 ± 1.5 mm, p = 0.02); however, the lesion width was also greater for transmural (10.6 ± 2.9 mm) versus non-transmural lesions (7.8 ± 2.8 mm, p = 0.001). The average tissue depth of transmural cross-sections was 3.1 ± 1.3 mm, while the average tissue depth of the non-transmural cross-sections was 3.4 ± 2.1 mm (p=0.57, Table 1).
Table 1.
Ablation Characteristics between Transmural and Non-transmural Cross-sections
| Transmural Cross-sections (N=254) |
Non-transmural Cross-sections (N=16) |
p-value | |
|---|---|---|---|
| Tissue Depth | 3.1 ± 1.3 | 3.4 ± 2.1 | 0.57 |
| Lesion Depth | 3.1 ± 1.3 | 2.2 ± 1.5 | 0.02 |
| Lesion Width | 10.6 ± 2.9 | 7.8 ± 2.8 | 0.001 |
| Bipolar Tmax (°C) | 74.9 ± 1.3 | 74.8 ± 1.7 | 0.85 |
| Bipolar Tmin (°C) | 66.9 ± 1.8 | 66.6 ± 2.3 | 0.62 |
| Bipolar Pmax (W) | 49.5 ± 9.7 | 49.6 ± 4.8 | 0.95 |
| Monopolar Tmax (°C) | 73.1 ± 1.6 | 73.5 ± 1.8 | 0.46 |
| Monopolar Tmin (°C) | 66.2 ± 2.4 | 65.6 ± 2.3 | 0.30 |
| Monopolar Pmax (W) | 56.2 ± 18.4 | 57.5 ± 19.6 | 0.80 |
Abbreviations: Pmax, maximum power; Tmax, maximum temperature; Tmin, minimum temperature
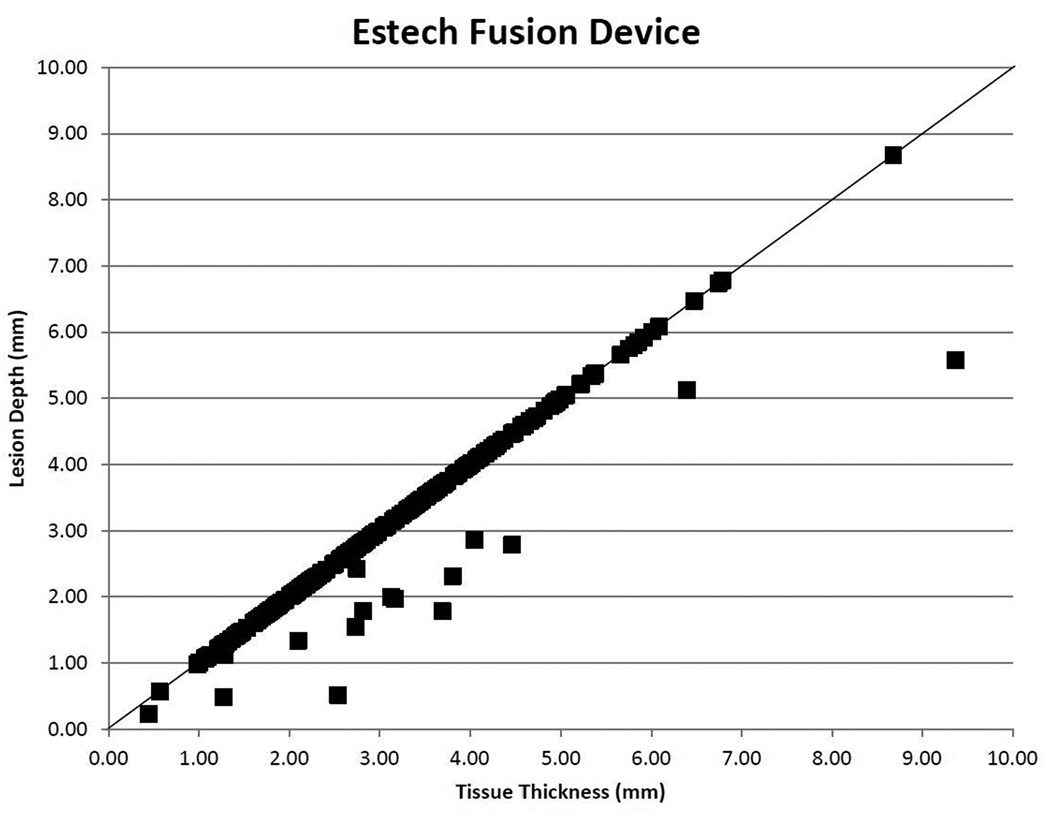
Lesion Transmurality
The efficacy of this device is depicted graphically via a scatter plot (Figure 5) of lesion depth versus tissue thickness. Transmurality was documented in 94% (254/270) of all cross-sections, and 68% (26/38) of all lesions were transmural along the entire ablation line. There was a significant difference in lesion transmurality based on where the cross-section was located within a lesion, with middle sections reaching 96% (187/195) transmurality, and end sections being 89% (67/75) transmural (p=0.04).
Figure 5.
Scatter plot representing the efficacy of the Cobra Fusion device (Estech, San Ramon, CA USA) at creating transmural lesions epicardially on the beating heart for each cross-section examined.
Anatomic Influence
No significant difference in lesion transmurality was identified based on the anatomic location of the lesion itself on the heart (Table 2, p=0.45 for the distribution).
Table 2.
Transmurality Based on Anatomical Location of Lesion*
| Transmural Cross-sections | Non-Transmural Cross-sections | |
|---|---|---|
| SVC | 92% (23/25) | 8% (2/25) |
| SVC/IVC | 86% (12/14) | 14% (2/14) |
| IVC | 100% (8/8) | 0% (0/8) |
| Anterior LAA | 88% (38/43) | 12% (5/43) |
| Posterior LAA | 96% (44/46) | 4% (2/46) |
| Left Atrial Free Wall | 98% (39/40) | 2% (1/40) |
| Anterior RAA | 92% (12/13) | 8% (1/13) |
| Posterior RAA | 96% (78/81) | 4% (3/81) |
Abbreviations: IVC, inferior vena cava; LAA, left atrial appendage; RAA, right atrial appendage; SVC, superior vena cava
p= 0.45 for the distribution
Non-transmural Lesions
Out of 270 total cross-sections, 16 were identified as being non-transmural. Of the cross-sections located at the end of the ablation line, 11% (8/75) were found to be non-transmural, whereas only 4% (8/195) of cross-sections located within the line of ablation were found to be non-transmural (p=0.04). Logistic regression analysis demonstrated that only association with failure of the device to create transmural lesions was low body temperature (p=0.015). Failure to create transmural lesions was not associated with cardiac output (p=0.54).
DISCUSSION
In the surgical treatment of AF, the ability to consistently create transmural lesions is critical to preventing AF recurrence. Although previous studies of ablation technologies have demonstrated success in consistently creating transmural lesions with the use of cardiopulmonary bypass, epicardial ablation devices have historically had difficulty in creating transmural lesions on the beating heart.7 A previous epicardial ablation device, for example, was tested in our laboratory and demonstrated 67% transmurality when tested on the beating heart in an acute animal model.17 In a chronic study with this device, only 8% of the lesions were transmural along their entire length, and no lesion was able to create lasting conduction block.18 Microwave epicardial ablation devices also were tested on the beating heart in acute animals, creating transmural lesions only 36% and 38% of the time, respectively.17, 19 The poor efficacy of these devices is one of the factors which have contributed to the often disappointing results with minimally-invasive, off-pump surgical approaches for AF.20 Although bipolar RF clamping devices have been shown to reliably create transmural lesions around the pulmonary veins from a completely epicardial approach, completion of the full CMIV lesion set requires that one jaw of the clamp be inserted into the atrium, risking air embolism if performed without cardiopulmonary bypass. This has limited these clamps to performing only pulmonary vein isolation on the beating heart, which has had poor efficacy, particularly in patients with longstanding persistent AF.21 These results highlight the need for a novel epicardial device for the completion of the CMIV lesion set on the beating heart, and for the refinement of minimally invasive techniques.
This study investigated the ability of a novel RF ablation system, the Estech Cobra Fusion™, to reliably create transmural lesions on the beating heart from an epicardial approach in an acute porcine model. Our results show that this device allows for epicardial ablation on the beating heart without the use of CPB, with a success rate that is better than most previous devices that we have tested.13, 22 This device was able to create transmural ablation in 94% of the cross-sections tested, with 68% of lesions being transmural across their entire length, without significant discrepancies in performance based on anatomic location of the lesion on the heart, cardiac output, or the thickness of the target tissue.
The improved success of this device compared to other epicardial linear devices may be due to several features that distinguish it from other devices tested in our laboratory. Instead of using one mode of energy, the Cobra Fusion combines both bipolar and monopolar energy. Furthermore, the suction-assistance offered by this device helps to ensure contiguous linear tissue-device contact, which has been difficult for handheld epicardial devices without a mechanism such as clamping. Similarly, whereas clamping devices have addressed the heat sink of the endocavitary blood pool by isolating the target tissues inside the jaws of the clamp, epicardial ablation devices have typically employed unidirectional energy transfer in direct apposition to circulating endocavitary blood at 37°C. This design excludes the endocavitary blood by isolating the target tissue inside the suction chamber of the ablation catheter. In order to ensure that suction is maintained throughout the ablation time, the device also features an alarm to alert the user to a loss of contact.
Unlike other epicardial devices tested by our laboratory, adverse events such as atrial perforation or charring were not observed in any of the lesions tested. This is credited to the heating algorithm of this device, which uses temperature feedback control to determine the amount of energy delivered to target tissues. This mechanism delivers less energy to thinner tissues, which reach the target temperature of 70°C more rapidly than thicker tissues, while achieving good rates of lesion transmurality with a single application.
Although the overall transmurality achieved by this device was one of the highest of any epicardial ablation device tested by our laboratory, 32% of lesions were not transmural along their entire length. This still falls short of the desired clinical performance, and of the results obtained when using bipolar clamps.13 Several factors were identified which may improve the performance of this device. Non-transmural cross-sections were significantly associated with low body temperature of the animal. This could be related to suboptimal performance of the device heating algorithm at lower tissue temperatures that thus require additional energy to achieve a target temperature of 50°C, which has been shown to produce myocardial cell death. This problem could be avoided clinically by carefully maintaining the patient at normothermia during a procedure. However, we did not specifically test the effect of body temperature on the performance of the device, and thus further investigation is needed to clarify this relationship. Additionally, there was a significant difference in transmurality based on the location of the cross-section within a lesion, with end sections being more often non-transmural. This is likely due to the fact that the electrodes terminate 5 mm from the end of the suction chamber, further highlighting the importance of overlapping ablation lines in the clinical setting, as even a 1 mm gap is sufficient for conduction of both sinus and fibrillatory wavefronts.15
LIMITATIONS
There are several weaknesses of this study. The present study was performed on normal healthy porcine atria. Although several steps were taken to minimize the impact of anatomic differences between the porcine atria used in this study and human atria, important differences still exist. The pathologic human atrial wall has been shown to differ significantly from healthy atrial myocardium in thickness, fibrosis, and amount of epicardial fat, all of which could impact energy delivery and affect lesion transmurality.23, 24 Thus, surgeons need to be aware of these differences when utilizing this device in diseased human hearts.
Additionally, the present study was an acute animal study, and it is possible that transmurality could be different both in a chronic animal model, and in the clinical population. However, unlike other studies that have used conduction block to demonstrate transmurality in the acute setting, which is known to be unreliable, our study used vital staining.18 Because a lesion was judged to be transmural only if the tissue did not take up any of the vital stain, our assessment represents a conservative estimation of the efficacy of this device in this model. Furthermore, previous studies in our laboratory have shown a good correlation between acute and chronic histology using this methodology.
The experimental design of this study was not meant to replicate the full CMIV lesion set. Our experimental lesion set was designed to test the device over a range of atrial tissues, and was further refined based on the anatomic considerations of the porcine model. Specific lesions of the CMIV lesion set that were not tested include the box lesion around the pulmonary veins, the lesion to the mitral annulus, and the lesion to the tricuspid annulus. Further clinical investigation is needed to determine the efficacy of this device in these areas.
Clinical Perspective.
"Performance of a Novel Bipolar/Monopolar Radiofrequency Ablation Device on the Beating Heart in an Acute Porcine Model" (Damiano)
This is an acute animal model evaluating the efficacy of the Fusion device in producing linear, transmural lesions from an epicardial approach. The histologic assessments support that the device is generally effective in producing the desired effect. However, there are several serious limitations to this study that should temper the enthusiasm of the surgeon considering using this device in the clinical setting. First and foremost, there is no correlation between tissue thickness and transmurality of the lesion. In addition, the 3 mm thickness of the porcine atrial tissue tested is often much thinner than the often pathologic human atrial tissue encountered in clinical practice. It would be helpful if future animal studies utilize a chronic model with assessment of electrical isolation, as that is really the final arbiter in judging the success of a lesion. Finally, though animal studies are valuable in evaluating the efficacy of ablative power sources for AF, decisions regarding the possible use of these devices in one's practice should be predicated on sound clinical results reported in peer-reviewed journals and meetings. Once again, Dr. Damiano and his colleagues have made a valuable contribution in our understanding of the performance of a power source for surgical ablation
Acknowledgments
This work was supported by grants from the National Institutes of Health (R01 HL032257 and 5 T32 HL007776), and by a research grant from Estech, San Ramon, CA USA.
Ralph J. Damiano, Jr., MD, receives research funding from Edwards Lifesciences, Corp., Irvine, CA USA, and Atricure, Inc., West Chester, OH USA, and acts as a consultant to Atricure, Inc., West Chester, OH USA, and Medtronic, Inc., Minneapolis, MN USA. Richard B. Schuessler receives research funding from Atricure, Inc., West Chester, OH USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the Annual Scientific Meeting of the International Society for Minimally Invasive Cardiothoracic Surgery, June 12 – 15, 2013, Prague, Czech Republic.
Disclosures: Lindsey L. Saint, MD, Christopher P. Lawrance, MD, Shoichi Okada, MD, Toshinobu Kazui, MD, PhD, Jason O. Robertson, MD, declare no conflicts of interest.
REFERENCES
- 1.Cox JL, Schuessler RB, D'Agostino HJ, Jr, et al. The surgical treatment of atrial fibrillation. Iii. Development of a definitive surgical procedure. The Journal of thoracic and cardiovascular surgery. 1991;101:569–583. [PubMed] [Google Scholar]
- 2.Prasad SM, Maniar HS, Camillo CJ, et al. The cox maze iii procedure for atrial fibrillation: Long-term efficacy in patients undergoing lone versus concomitant procedures. The Journal of thoracic and cardiovascular surgery. 2003;126:1822–1828. doi: 10.1016/s0022-5223(03)01287-x. [DOI] [PubMed] [Google Scholar]
- 3.Damiano RJ, Jr, Schwartz FH, Bailey MS, et al. The cox maze iv procedure: Predictors of late recurrence. The Journal of thoracic and cardiovascular surgery. 2011;141:113–121. doi: 10.1016/j.jtcvs.2010.08.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gammie JS, Laschinger JC, Brown JM, et al. A multi-institutional experience with the cryomaze procedure. The Annals of thoracic surgery. 2005;80:876–880. doi: 10.1016/j.athoracsur.2005.03.075. [DOI] [PubMed] [Google Scholar]
- 5.Gillinov AM, Smedira NG, Cosgrove DM., III Microwave ablation of atrial fibrillation during mitral valve operations. The Annals of thoracic surgery. 2002;74:1259–1261. doi: 10.1016/s0003-4975(02)03760-8. [DOI] [PubMed] [Google Scholar]
- 6.Mitnovetski S, Almeida AA, Goldstein J, et al. Epicardial high-intensity focused ultrasound cardiac ablation for surgical treatment of atrial fibrillation. Heart, lung & circulation. 2009;18:28–31. doi: 10.1016/j.hlc.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Schuessler RB, Lee AM, Melby SJ, et al. Animal studies of epicardial atrial ablation. Heart rhythm : the official journal of the Heart Rhythm Society. 2009;6:S41–S45. doi: 10.1016/j.hrthm.2009.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams MR, Stewart JR, Bolling SF, et al. Surgical treatment of atrial fibrillation using radiofrequency energy. The Annals of thoracic surgery. 2001;71:1939–1944. doi: 10.1016/s0003-4975(01)02594-2. [DOI] [PubMed] [Google Scholar]
- 9.Melby SJ, Gaynor SL, Lubahn JG, et al. Efficacy and safety of right and left atrial ablations on the beating heart with irrigated bipolar radiofrequency energy: A long-term animal study. The Journal of thoracic and cardiovascular surgery. 2006;132:853–860. doi: 10.1016/j.jtcvs.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 10.Prasad SM, Maniar HS, Diodato MD, et al. Physiological consequences of bipolar radiofrequency energy on the atria and pulmonary veins: A chronic animal study. The Annals of thoracic surgery. 2003;76:836–842. doi: 10.1016/s0003-4975(03)00716-1. [DOI] [PubMed] [Google Scholar]
- 11.Prasad SM, Maniar HS, Schuessler RB, et al. Chronic transmural atrial ablation by using bipolar radiofrequency energy on the beating heart. The Journal of thoracic and cardiovascular surgery. 2002;124:708–713. doi: 10.1067/mtc.2002.125057. [DOI] [PubMed] [Google Scholar]
- 12.Voeller RK, Zierer A, Lall SC, et al. Efficacy of a novel bipolar radiofrequency ablation device on the beating heart for atrial fibrillation ablation: A long-term porcine study. The Journal of thoracic and cardiovascular surgery. 2010;140:203–208. doi: 10.1016/j.jtcvs.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Voeller RK, Zierer A, Schuessler RB, et al. Performance of a novel dual-electrode bipolar radiofrequency ablation device: A chronic porcine study. Innovations. 2011;6:17–22. doi: 10.1097/IMI.0b013e31820bc57f. [DOI] [PubMed] [Google Scholar]
- 14.Gaynor SL, Diodato MD, Prasad SM, et al. A prospective, single-center clinical trial of a modified cox maze procedure with bipolar radiofrequency ablation. The Journal of thoracic and cardiovascular surgery. 2004;128:535–542. doi: 10.1016/j.jtcvs.2004.02.044. [DOI] [PubMed] [Google Scholar]
- 15.Melby SJ, Lee AM, Zierer A, et al. Atrial fibrillation propagates through gaps in ablation lines: Implications for ablative treatment of atrial fibrillation. Heart rhythm : the official journal of the Heart Rhythm Society. 2008;5:1296–1301. doi: 10.1016/j.hrthm.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swanson DK, Smith WJ, Ibrahim T, et al. Tissue temperature feedback control of power: The key to successful ablation. Innovations (Phila) 2011;6:276–282. doi: 10.1097/IMI.0b013e31822b4d22. [DOI] [PubMed] [Google Scholar]
- 17.Lee AM, Aziz A, Sakamoto SI, et al. Epicardial ablation on the beating heart: Limited efficacy of a novel, cooled radiofrequency ablation device. Innovations. 2009;4:86–92. doi: 10.1097/IMI.0b013e3181a348a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee AM, Aziz A, Clark KL, et al. Chronic performance of a novel radiofrequency ablation device on the beating heart: Limitations of conduction delay to assess transmurality. The Journal of thoracic and cardiovascular surgery. 2012;144:859–865. doi: 10.1016/j.jtcvs.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaynor SL, Byrd GD, Diodato MD, et al. Microwave ablation for atrial fibrillation: Dose-response curves in the cardioplegia-arrested and beating heart. The Annals of thoracic surgery. 2006;81:72–76. doi: 10.1016/j.athoracsur.2005.06.062. [DOI] [PubMed] [Google Scholar]
- 20.Han FT, Kasirajan V, Wood MA, et al. Minimally invasive surgical atrial fibrillation ablation: Patient selection and results. Heart rhythm : the official journal of the Heart Rhythm Society. 2009;6:S71–S76. doi: 10.1016/j.hrthm.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 21.Edgerton JR, Edgerton ZJ, Weaver T, et al. Minimally invasive pulmonary vein isolation and partial autonomic denervation for surgical treatment of atrial fibrillation. The Annals of thoracic surgery. 2008;86:35–39. doi: 10.1016/j.athoracsur.2008.03.071. [DOI] [PubMed] [Google Scholar]
- 22.Sakamoto S, Voeller RK, Melby SJ, et al. Surgical ablation for atrial fibrillation: The efficacy of a novel bipolar pen device in the cardioplegically arrested and beating heart. The Journal of thoracic and cardiovascular surgery. 2008;136:1295–1301. doi: 10.1016/j.jtcvs.2008.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Platonov PG, Ivanov V, Ho SY, et al. Left atrial posterior wall thickness in patients with and without atrial fibrillation: Data from 298 consecutive autopsies. Journal of cardiovascular electrophysiology. 2008;19:689–692. doi: 10.1111/j.1540-8167.2008.01102.x. [DOI] [PubMed] [Google Scholar]
- 24.Platonov PG, Mitrofanova LB, Orshanskaya V, et al. Structural abnormalities in atrial walls are associated with presence and persistency of atrial fibrillation but not with age. Journal of the American College of Cardiology. 2011;58:2225–2232. doi: 10.1016/j.jacc.2011.05.061. [DOI] [PubMed] [Google Scholar]