Summary
Background and objectives
The relative merits of buttonhole (or blunt needle) versus rope ladder (or sharp needle) cannulation for hemodialysis vascular access are unclear.
Design, setting, participants, & measurements
Clinical outcomes by cannulation method were reviewed in 90 consecutive home hemodialysis patients. Initially, patients were trained in rope ladder cannulation. From 2004 on, all incident patients were started on buttonhole cannulation, and prevalent patients were converted to this cannulation method. Coprimary outcomes were arteriovenous fistula-attributable systemic infections and a composite of arteriovenous fistula loss or requirement for surgical intervention. Secondary outcomes were total arteriovenous fistula-related infections and staff time requirements. Additionally, a systematic review evaluating infections by cannulation method was performed.
Results
Seventeen systemic arteriovenous fistula-attributable infections were documented in 90 patients who were followed for 3765 arteriovenous fistula-months. Compared with rope ladder, buttonhole was not associated with a significantly higher rate of systemic arteriovenous fistula-attributable infections (incidence rate ratio, 2.71; 95% confidence interval, 0.66 to 11.09; P=0.17). However, use of buttonhole was associated with a significantly higher rate of total arteriovenous fistula infections (incidence rate ratio, 3.85; 95% confidence interval, 1.66 to 12.77; P=0.03). Initial and ongoing staff time requirements were significantly higher with buttonhole cannulation. Arteriovenous fistula loss or requirement for surgical intervention was not different between cannulation methods. A systematic review found increased arteriovenous fistula-related infections with buttonhole compared with rope ladder in four randomized trials (relative risk, 3.34; 95% confidence interval, 0.91 to 12.20), seven observational studies comparing before with after changes (relative risk, 3.15; 95% confidence interval, 1.90 to 5.21), and three observational studies comparing units with different cannulation methods (relative risk, 3.27; 95% confidence interval, 1.44 to 7.43).
Conclusion
Buttonhole cannulation was associated with higher rates of infectious events, increased staff support requirements, and no reduction in surgical arteriovenous fistula interventions compared with rope ladder in home hemodialysis patients. A systematic review of the published literature found that buttonhole is associated with higher risk of arteriovenous fistula-related infections.
Introduction
Vascular arteriovenous fistulae (AVF) -related complications remain an important cause of morbidity and health care usage in hemodialysis service provision. AVFs are the preferred access modality and associated with the lowest rates of access-related events (1–4).
Cannulation of AVF is by the traditional rope ladder (RL; also known as sharp needle) technique, using venepuncture with sharp needles at a new site during each dialysis session, or the buttonhole (BH; also known as blunt needle) technique, involving repeated punctures with blunt needles through established tissue tunnel tracts. The BH technique was initially introduced with hopes of preserving access in short AVFs (5). The perceived benefits of reduction in problematic cannulation episodes (4,6–8) and patient discomfort and lower requirement for AVF interventions have led to a resurgence in the use of BH cannulation, specifically in the home hemodialysis (HHD) setting (6,7,9–13). Recent studies have suggested increased infections in patients using BH cannulation; however, definitive evidence is lacking (8,10,14).
We, therefore, wished to test the hypothesis that BH cannulation was associated with increased AVF infections and better fistula preservation and establish the relative cost of home training time by cannulation method. We conducted a retrospective review in a single HHD unit using both cannulation techniques. In addition, we conducted a systematic review of the available literature to further examine the impact of BH cannulation on infection rates in maintenance hemodialysis patients. Given the paucity of the randomized evidence in terms of total participant number and follow-up, we included both randomized controlled trials (RCTs) and observational studies to comprehensively present the sum of the current literature.
Materials and Methods
Current Observational Study
All consecutive end stage kidney disease patients trained by a single HHD training unit with at least one dialysis session at home between January 1, 2003 and December 31, 2009 were included. Patients were identified using records of dialysis machine delivery and confirmed with the HHD unit records.
Inclusion Criteria
Patients were included in the study if (1) they dialyzed one time at home, (2) they were metropolitan residents, (3) their renal physician was appointed to one of two feeder hospitals to the HHD, and (4) their vascular access was an AVF.
Home and Cannulation Training
All patients were trained in the RL technique until mid-2004, when the unit policy changed such that all incident HHD patients were trained in BH; additionally, prevalent patients were gradually converted to the BH technique. Additional information on the procedures of the home training unit is detailed in Supplemental Appendix.
Data Collection
Data were collected through a review of medical records in the HHD unit and its two hospitals, contemporaneous unit reports to the national registry, nephrologist letters, and internal and external pathology results. Data were collected on all patients dialyzing with an AVF from the date of the first HHD training session until the occurrence of a censoring event, such as when the patient ceased HHD, relocated outside the unit’s catchment area, received a kidney transplant, or died or the study ended (December 31, 2010). Data were collected by two investigators (C.A.M. and S.S.K.), uncertainties were reviewed by a third investigator (M.J.J.), and discrepancies were resolved by consensus.
Outcome Measures
Two coprimary outcome event types were prespecified. The first type was the number of systemic AVF-related infection events (blood culture-positive sepsis or complicated infection [e.g., endocarditis] in the absence of an identifiable non-AVF source) by cannulation method. The second type was the number of fistula loss/surgical intervention requirement events (defined using a composite end point of any surgical revision or episode requiring permanent abandonment of the AVF and/or creation of a new AVF) by cannulation method. To avoid any single event contributing to both outcomes, we specifically excluded infection-associated fistula loss from the fistula loss/surgical intervention outcome. Radiologic interventions were excluded, because the availability of these techniques increased throughout the follow-up period and would be overly subject to era bias. Local AVF infections defined as erythema, pain, or swelling of the fistula site requiring treatment with oral antibiotics with negative blood cultures in the absence of systemic symptoms were also recorded. The unit policy for management of infections is detailed in Supplemental Appendix.
Length of initial home training required to establish dialysis in the home setting was measured in days by cannulation method. Total service requirement by cannulation technique in terms of face-to-face encounter per 1000 AVF-days after completion of initial home training (encounter defined as any day on which a dialysis nurse provided a home visit or a patient dialyzed in the home training unit) was also compared. Ethics approval was gained from the local hospital ethics committees (CH 62/2/2010–085). The requirement for consent was waved in the setting of a retrospective study.
Statistical Analyses
Baseline characteristics were compared using chi-squared and t tests. The rates of events were calculated as the total numbers of events divided by the follow-up period for each cannulation method and compared using chi-squared tests. The primary outcomes (infections and fistula loss/surgical interventions) were analyzed as multiple independent events using Poisson regression analysis. Incidence rate ratios (IRRs) and 95% confidence intervals (95% CIs) according to contemporaneous cannulation technique were calculated using Poisson regression analysis. The Andersen–Gill technique was used in sensitivity analyses. Both techniques are appropriate for analyzing multiple events that occur infrequently in time, with the difference being in the underlying assumptions on event distribution (Poisson distribution for Poisson analysis and Cox proportional hazards for the Andersen–Gill technique). Both analysis methods calculate the risk of an event within multiple time intervals defined as commencing with the initiation of each cannulation method in an AVF or the day after the last instance of an event type for each patient. Each time period concludes with the event of interest or a censoring event. Analyses were performed using the Stata cluster option to create clusters of individual patients, acknowledging that events occurring in an individual patient are not necessarily independent. Multivariable Poisson analyses were adjusted for cannulation technique, patient’s age, and diabetes status. Exploratory analyses were performed in parallel using dialysis vintage, history of cardiovascular disease, median weekly dialysis hours, and calendar year. In additional sensitivity analyses, proportional hazard models were used to estimate the hazard ratios (HRs) of a first event of each outcome for each patient according to each cannulation method. Statistical analysis was performed using Stata 11. For all comparisons, the level of significance was set to P<0.05.
Systematic Review Methods
A systematic review was performed according to a prespecified protocol (available on request). Medline, EMBASE, COCHRANE, SCOPUS, AMED, Cinahl, and Clinical Trials Registry (www.clinicaltrials.gov) between 1950 and May 15, 2013 were searched for all studies involving BH cannulation in hemodialysis patients without a language restriction (Supplemental Figure 1). RCTs and observational studies were included. Reference lists of relevant trials and review articles were also reviewed. The primary outcome was AVF-related infections. Where alternative definitions of AVF-related infections were reported, we selected all AVF-related infections (local and systemic), AVF-related systemic infections, and AVF-related local infections in order of priority for analysis. Data were extracted independently by two investigators (C.A.M. and S.S.K.) into a prespecified spreadsheet, and discrepancies were resolved by consensus or arbitrated by a third investigator (M.J.J.). Data on baseline characteristics were extracted along with follow-up duration, outcome events, and study method details.
We used random effects models to calculate relative risks (RRs) with 95% CIs. Analyses were performed using reported raw event counts, where possible or reported RR or IRR estimates. If no events were recorded in one group, we added 0.5 to the numerator and denominator to enable inclusion.
Analyses were conducted separately according to study design type. Study quality was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria as suggested by the Cochrane collaboration (15). Heterogeneity in the risk estimate according to study design was estimated by the Cochran I2, with studies weighted using the inverse variance method.
Results
Study Participants
Ninety patients successfully completed home training and dialyzed at home. The total follow-up period was 3765 AVF-months (998 months of RL and 2767 months of BH); 60 patients were initially trained with BH cannulation, and 30 patients were initially trained with RL cannulation. Twelve patients using RL cannulation were converted to the BH technique, with no conversions from BH to RL cannulation taking place.
The study population was predominantly men (74%) and Caucasian (63%), with a median age of 52 years (interquartile range [IQR]=39.4–57.2) (Table 1).
Table 1.
Baseline characteristics of included patients
| Characteristic | Cannulation Method | Overall | ||
|---|---|---|---|---|
| RL Only | Both Methodsa | BH Only | ||
| No. of patients | 18 | 12 | 60 | 90 |
| Age (yr) | 48.7 (37.5–54.7) | 53.7 (45.4–58.5) | 51.6 (39.5–59.6) | 51.6 (39.4–57.2) |
| Men (%) | 78 | 83 | 70 | 73 |
| Ethnicity (%) | ||||
| Caucasian | 83 | 42 | 62 | 63 |
| Asian | 6 | 58 | 18 | 21 |
| Other/missing | 11 | 0 | 20 | 16 |
| Cause of ESKD (%) | ||||
| GN | 28 | 50 | 43 | 41 |
| Diabetes | 17 | 25 | 18 | 19 |
| Hypertension | 6 | 0 | 7 | 6 |
| Polycystic kidney disease | 28 | 8 | 10 | 13 |
| Other | 11 | 17 | 12 | 12 |
| Comorbidity (%) | ||||
| Ischemic heart disease | 6 | 0 | 23 | 17 |
| Peripheral vascular disease | 6 | 0 | 12 | 9 |
| Diabetes (%) | 22 | 25 | 30 | 28 |
| RRT vintage (mo) | 3.8 (1.8–6.4) | 4.1 (2.6–8.8) | 4.1 (1.4–9.0) | 4.1 (1.5–8.9) |
| RRT before HHD (%) | ||||
| In center | 100 | 100 | 83 | 89 |
| Satellite dialysis | 0 | 0 | 2 | 1 |
| Peritoneal dialysis | 0 | 0 | 4 | 2 |
| Transplant | 0 | 0 | 12 | 8 |
| Dialysis session duration (median, IQR) | 5 (5–5.67) | 5 (5–5) | 5 (5–5) | 5 (5–5.5) |
| Dialysis session duration (mean, SD) | 5.12 (0.68) | 4 (0.43) | 5.18 (0.69) | 5.17 (0.63) |
| Sessions/wk | 3 (3–3) | 3 (3–3) | 3 (3–4) | 3 (3–4) |
Values expressed as medians (interquartile ranges). RL, rope ladder; BH, buttonhole; ESKD, end stage kidney disease; RRT, renal replacement therapy; HHD, home hemodialysis.
Started HHD with RL and later converted to BH.
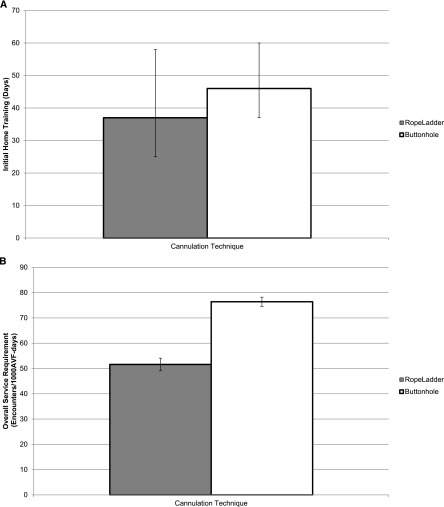
Systemic AVF-Attributable Infections
Seventeen AVF-related systemic infections were recorded: fifteen with BH cannulation and two with RL cannulation (Figure 1). Systemic AVF-related infections were nonsignificantly elevated by 270% using BH cannulation compared with RL cannulation (IRR, 2.71; 95% CI, 0.66 to 11.09; P=0.17) (Table 2). Multivariate Poisson regression analysis controlling for patient’s age and diabetes did not significantly alter the results (IRR, 2.52; 95% CI, 0.63 to 10.16; P=0.19), and analyses controlling for sex, cardiovascular disease, weekly dialysis hours, and calendar year (data not shown) also did not significantly alter the results. The results were not markedly different using the Andersen–Gill method (unadjusted IRR, 2.56; 95% CI, 0.59 to 11.16; P=0.21; adjusted IRR, 2.50; 95% CI, 0.57 to 11.04; P=0.23). Proportional hazards models based on the time to first systemic AVF-related infection were nonsignificantly elevated with BH compared with RL (unadjusted HR, 2.35; 95% CI, 0.53 to 10.36; P=0.26; adjusted HR, 2.41; 95% CI, 0.54 to 10.77; P=0.25) (Supplemental Table 1).
Figure 1.
Rate of AVF-attributable infections per 1000 AVF-days by cannulation technique in a single home hemodialysis unit. The lines represent the 95% confidence intervals around the infection rate. *Significant difference in total infection rate between the BH and RL techniques (P≤0.05). AVF, arteriovenous fistula; BH, buttonhole; RL, rope ladder.
Table 2.
Rate difference of arteriovenous fistula events by cannulation technique
| Risk Associated with BH Compared with RLa | ||||
|---|---|---|---|---|
| AVF Events | Univariate Analysis | Adjusted Analysisb | ||
| IRR (95% CI) | P Value | IRR (95% CI) | P Value | |
| Systemic infections | 2.71 (0.66 to 11.09) | 0.17 | 2.52 (0.63 to 10.16) | 0.19 |
| Local infections | 6.13 (0.72 to 52.0) | 0.09 | 6.27 (0.72 to 54.95) | 0.10 |
| All AVF infections | 3.85 (1.66 to 12.77) | 0.03 | 3.75 (1.10 to 12.79) | 0.04 |
| Surgical interventions (including AVF loss) | 1.08 (0.33 to 3.55) | 0.90 | 0.87 (0.26 to 2.97) | 0.82 |
AVF, arteriovenous fistula; BH, buttonhole; RL, rope ladder; IRR, incidence rate ratio; 95% CI, 95% confidence interval.
Started HHD with RL and later converted to BH.
The analysis was adjusted for patient age and diabetes status using Poisson regression.
Fistula Loss/Surgical AVF Intervention
Thirty-two noninfective AVF events occurred during the study period (twenty-four in patients using BH cannulation [0.29 events/1000 AVF-days]) (Supplemental Table 2). Aforementioned AVF events included thrombosis (20 events), aneurysms (3 events), steal syndromes (2 events), and stenosis (7 events) (Supplemental Table 2). Twelve events were associated with permanent abandonment and/or creation of a new fistula (thrombosis [nine events], aneurysm [one event], steal syndrome [one event], and stenosis [one event]). The incidence rate of surgical AVF interventions (including AVF loss) did not differ significantly between cannulation methods (unadjusted IRR, 1.08; 95% CI, 0.33 to 3.55; P=0.90; adjusted IRR, 0.87; 95% CI, 0.26 to 2.97; P=0.82) (Table 2). Results were similar with the Andersen–Gill analysis (unadjusted IRR, 1.09; 95% CI, 0.32 to 3.71; P=0.89; adjusted IRR, 0.94; 95% CI, 0.29 to 3.09; P=0.92). The risk for fistula loss/surgical AVF intervention using the Cox proportional hazards model was not significantly different between cannulation techniques (unadjusted HR, 1.01; 95% CI, 0.36 to 2.83; P=0.99; adjusted HR, 0.91; 95% CI, 0.31 to 2.61; P=0.86) (Supplemental Table 1).
Overall, there were 14 AVFs lost in 11 patients during the study (12 AVFs were associated with noninfective events and included in the analysis, whereas 2 AVFs were associated with infective events and excluded) (Supplemental Table 2). The incidence rate loss of AVF did not differ between cannulation methods (unadjusted IRR, 1.08; 95% CI, 0.27 to 4.42, P=0.91; adjusted IRR, 0.86; 95% CI, 0.21 to 3.62, P=0.84).
Total AVF-Related Infections
Of a total of 35 AVF-related infections, 32 AVF-related infections occurred in patients using BH cannulation (0.39 events/1000 AVF-days), and 3 AVF-related infections occurred in patients using RL cannulation (0.10 events/1000 AVF-days). Total AVF-attributable infections were significantly elevated with BH cannulation (unadjusted IRR, 3.85; 95% CI, 1.66 to 12.77; P=0.03) (Table 2). Multivariate Poisson regression analysis controlling for patient age and diabetes did not significantly alter the results (IRR, 3.75; 95% CI, 1.10 to 12.79; P=0.04), and the Andersen–Gill results were similar (unadjusted IRR, 3.67; 95% CI, 1.09 to 12.32; P=0.04; adjusted IRR, 3.79; 95% CI, 1.07 to 13.43; P=0.04). Proportional hazards models showed a nonsignificantly increased risk with BH compared with RL (unadjusted HR, 2.63; 95% CI, 0.79 to 8.82; P=0.12; adjusted HR, 2.87; 95% CI, 0.85 to 9.69; P=0.09) (Supplemental Table 1).
Service Provision Requirement
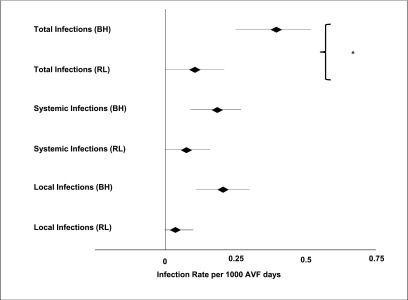
Initial home training using the BH technique required significantly more days than the RL technique (median=46 days; IQR=37–60 and median=37 days; IQR=25–58, respectively; P=0.01) (Figure 2A). Overall service requirements were also significantly increased (mean=76.4 encounters per 1000 AVF-days; 95% CI, 74.6 to 78.2 and mean=51.6 per 1000 AVF-days; 95% CI, 49.1 to 54.1 for BH and RL cannulation, respectively) (Figure 2B), which equates to 1 encounter per 13.2 AVF-days for BH cannulation compared with 1 encounter per 19.0 AVF-days for RL cannulation.
Figure 2.
Initial training time and overall service requirements by cannulation technique in a single home hemodialysis unit. (A) Length of initial home training (days) by cannulation technique in a single home hemodialysis unit. The error bars indicate the interquartile range in days (P<0.01). (B) Ongoing support requirements (in encounters [including training, home visits, and dialysis sessions in the home training center] per 1000 AVF-days) by cannulation technique in a single home hemodialysis unit (P<0.01). AVF, arteriovenous fistula.
Systematic Review Results
In total, 15 studies satisfied our inclusion criteria (all were published since 2007). Of these studies, eight studies reported total infections (6,7,14,16–20), five studies reported systemic infections only (21–25), and one study reported only local infections (8). There were four RCTs (16,17,19,20) and three observational studies comparing units with different cannulation methods (7,14,23), and the remaining eight studies were observational studies comparing before and after changes (6,8,18,21,22,24,25) (Table 3). Most of the studies were single-center, observational studies, and all were published after 2007; the total number of patients included was greater than 1612 in the majority of the studies. The studies were conducted in the United States, Europe, Canada, and Australia; four studies were conducted in an HHD setting (8,14,22–25), seven studies were conducted in an in-center hemodialysis setting (6,7,17–21), and four studies were conducted in both settings (16). Most of the studies were graded as low level of evidence (Supplemental Table 3).
Table 3.
Baseline characteristics of included studies comparing infection rates according to buttonhole and rope ladder cannulation
| Ref. | Type of Study and Patients | Description | Total Patients | BH | RL | Age in BH (yr) | Age in RL (yr) | Men in BH | Men in RL | Diabetes in BH | Diabetes in RL | CVD in BH | CVD in RL | Follow-Up (patient yr) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 17 | Randomized trial in CHD | Compared RL with BH at baseline and then rates of BH pre- and posteducation sessions | 56 | 28 | 28 | 61a | 60a | NR | NR | 9 (32%) | 10 (36%) | NR | NR | 28 |
| 16 | Randomized trial in CHD and HHD | Compared BH with RL in HHD and CHD patients | 70 | 34 | 35 | NR | NR | 21 (62%) | 27 (77%) | 17 (50%) | 14 (40%) | 19 (56%) | 9 (26%) | 35 |
| 19 | Randomized trial in CHD | CHD patients BH versus RL | 140 | 70 | 70 | 70.3a | 66.7a | 51 (73%) | 46 (66%) | 33 (47%) | 39 (56%) | 31 (44%) | 28 (40%) | 23 |
| 20 | Randomized trial in CHD | Compared BH with usual practice (sharp needle cannulation) | 140 | 70 | 70 | 62a | 64a | 47 (67%) | 44 (63%) | NR | NR | NR | NR | 140 |
| 8 | Pre–post comparison in HHD | Patients were changed to BH; comparison with baseline RL rates | 33 | 33 | 33 | 49a | 49a | 24 (73%) | 24 (73%) | NR | NR | NR | NR | 30 |
| 21 | Pre–post comparison in HHD and CHD | Compared rates before and after implementation of nursing practice changes | 8 | 8 | 8 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| 6 | Pre–post comparison in CHD | Conducted nursing surveys for pain and chart review for complications | 29 | 29 | 95 | 62.9a | 65.9a | 18 (62%) | 55 (58%) | NR | NR | NR | NR | NR |
| 22 | Pre–post comparison in NHD | Compared rates of infection before and after instituting mupirocin prophylaxis | 56 | 56 | 56 | 51.5a | 51.5a | 35 (63%) | 35 (63%) | NR | NR | NR | NR | NR |
| 18 | Pre–post comparison in CHD | Compared RL with BH at baseline and then rates of BH pre- and posteducation sessions (compared RL [period 1] with BH posteducation session [period 4] to be conservative) | 177 | 85 | 105 | 70.5 | 69.8 | 79 (66%) | 52 (60%) | 36 (30%) | 33 (38%) | NR | NR | 469 |
| 24 | Pre–post comparison | Introduced BH and compared infection rates with RL | 31 | 13 | 18 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| 25 | Pre–post comparison in CHD and HHD | Retrospective review; patient choice of technique | 127 | 74 | 53 | 50b | 68b | 58 (78%) | 29 (55%) | 7 (9%) | 10 (18%) | NR | NR | 762 |
| This study | Pre–post comparison in HHD | Compared rates between RL and BH after BH commenced in unit | 90 | 72c | 30 | 51.6b | 48.7b | 42 (70%) | 23 (78%) | 18 (30%) | 7 (22%) | 14 (23%) | 2 (6%) | 314 |
| 23 | Observational in CHD | Compared two groups (BH versus RL) over 12 months prospectively | 1492 occasions of BH access | 587 episodes | 905 episodes | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| 14 | Observational in NHD | Compared NHD patients using BH with CHD patients using RL | 235 | 63 | 172 | 51.7 | 58.3 | 50 (79%) | 102 (59%) | 21 (33%) | 67 (39%) | NR | NR | 86.2 |
| 7 | Observational in CHD | Compared CHD patients between three centers (two used RL and one used BH) | 145 | 75 | 70 | 67a | 65a | 44 (59%) | 47 (67%) | 20 (27%) | 15 (21%) | 46 (61%) | 56 (80%) | 109 |
BH, buttonhole cannulation; RL, rope ladder cannulation; CVD, cardiovascular disease; CHD, conventional hemodialysis; NR, not reported; HHD, home hemodialysis; NHD, nocturnal hemodialysis.
Mean age reported.
Median age reported.
Twelve participants were cannulated with RL first and then BH during the study, and therefore, they contributed data to both RL and BH analyses.
Compared with RL cannulation, infection risk was approximately threefold higher with BH cannulation in RCTs (RR, 3.34; 95% CI, 0.91 to 12.20; P=0.07), studies comparing before and after changes (RR, 3.15; 95% CI, 1.90 to 5.21; P<0.001), and observational studies comparing units with different cannulation methods (RR, 3.27; 95% CI, 1.44 to 7.43; P=0.005) (Figure 3). There was no evidence of heterogeneity of effect within each class of study (I2=14.5%, P=0.32 for RCTS; I2=0.0%, P=0.75 for studies comparing before and after changes; I2=0.0%, P=0.46 for observational studies comparing units with different cannulation methods). When risk estimates were combined across study types for a sensitivity analysis, BH cannulation resulted in a threefold (combined RR, 3.18; 95% CI, 2.12 to 4.77; P<0.001) higher infection risk with no statistical evidence of significant heterogeneity across study type (I2=0.00%, P=0.81), despite the varying methodologies.
Figure 3.
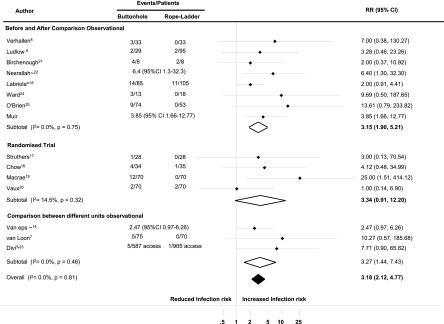
Forest plot of systematic review for total arteriovenous fistula-attributable infections.∼We used reported odds ratios and relative risks when reported. ^We compared period 1 (rope ladder cannulation only) with period 4 (buttonhole cannulation only after the education session). %This study did not report the numbers of patients but only the number of occasions that the arteriovenous fistula was accessed. 95% CI, 95% confidence interval; RR, relative risk.
Discussion
We conducted a retrospective analysis of the effect of BH compared with RL cannulation in a single unit and compared the findings with the existing literature using a systematic review. In our unit, BH cannulation was associated with a significant increase in total AVF infections in consecutive HHD patients. There was no difference in the rate of AVF loss/surgical AVF intervention. BH technique was associated with significantly greater demands on staff time (both initial and ongoing).
The systematic review of 15 studies showed a similar and roughly threefold higher infection risk with BH cannulation compared with RL. The association of higher infection risk with BH cannulation was separately significant for both types of observational studies and similar, although not statistically significant for randomized trials.
Infection rates among people using primary AVFs are low compared with people using other dialysis access types and have been comparable across varying study designs. Our study reports an infection rate of 0.39 events per 1000 AVF-days associated with BH and 0.10 events per 1000 AVF-days associated with RL. Comparable rates for BH-related infection in the literature (converted into rates per 1000 AVF-days) are 0.34 reported in a Belgian study (18), 0.43 reported among Australian HHD patients (14), and 50 per 1000 sessions of local infections reported in a Canadian conventional hemodialysis cohort (19). Although lower than the bloodstream infection rate of 1.27/1000 days associated with catheters in a American conventional hemodialysis cohort (26), any increase in AVF-related events is important because of its impact on clinical outcomes and survival (27,28). This finding is particularly concerning in an HHD population given that these patients generally have better prognostic baseline characteristics and outcomes (28), leading to the expectation of lower rates of adverse events. Additionally, AVF events can lead to discontinuation of HHD (27,28).
The interest in BH cannulation has been driven by its postulated benefits. Only one RCT has examined the impact of cannulation method on AVF survival and primary patency (AVF preservation without requirement for surgical or radiologic intervention) (20), and it found that BH cannulation was associated with lower rates of primary patency loss (HR, 0.46; 95% CI, 0.25 to 0.87) in direct contrast to our findings of no benefit for AVF preservation (IRR, 1.08; 95% CI, 0.33 to 3.55) or reduction in surgical interventions using the BH technique. Previous observational studies have found either reduced interventions in association with BH cannulation (7) or no difference (6,14). Potential explanations for the different findings between our study and the United Kingdom study include our lack of randomization, our longer observation period (mean=42 months) compared with the randomized study (minimum=12 months per patient), and our composite end point of AVF loss or surgical intervention that excluded radiologic interventions, which were included in the randomized study. This difference in definition might explain the finding of lower intervention event rates in our study (0.10 and 0.11 per AVF-year with RL and BH, respectively) compared with the United Kingdom randomized study (0.4 and 0.2 per AVF-year for RL and BH, respectively), although it does not clearly explain the difference in relative rate between the two techniques. Differences in BH tract creation may also impact early failure rates or long-term stenosis risk. The United Kingdom randomized study used the placement of a polycarbonate peg left in situ between dialysis sessions. By contrast, our study created the tract through repeated cannulation with sharp needles. Additionally, the differences found in the United Kingdom study may have been caused by poor outcomes in the control arm. The 1-year primary patency rate in the RL arm at 49% was lower than the 62.5% rate reported from a meta-analysis of 38 studies (29) including 4570 participants, whereas the rate in the BH group was higher at 74%. By contrast, the high primary patency rates (12-month rates for RL and BH were 90.9% and 93.8%, respectively) in our study may have obscured a true benefit from BH cannulation. Our high primary patency rates were no doubt because of, at least in part, conduct in home dialysis patients, a population known for their relatively good outcomes (28,30), and exclusion of radiologic interventions from our composite end point. The last and perhaps most compelling explanation is that both findings are caused by chance given the relatively small size of both studies.
The desired benefit of BH cannulation is a reduction in patient pain. Observational studies have predominantly reported BH as being associated with reduced pain (6,8), whereas one study showed an increase in cannulation pain (7). Three of four RCTs assessed the impact on patient comfort. Pain was found to be increased in one study (19), and no difference in pain (16) was reported with the BH technique in two of the randomized studies. In the RCT that reported a marginal increase in pain with BH cannulation, the analyses excluded the patients (8 of 70; 11%) who discontinued the technique because of pain (all in the BH group) (20).
HHD is a cost-efficient modality of dialysis service provision. In this first study reporting on the service provision requirements between cannulation methods, we report that BH cannulation increased staff time requirements. Using our results, we calculated the approximate increase in staff time requirements to be an extra 4526 encounters over 5 years to maintain 100 patients on BH.
Strengths of our observational study include the longest follow-up period in a cannulation study to date and the analysis of service requirements associated with cannulation techniques. Limitations largely result from its retrospective nature.
Limitations of the systematic review include the small number of included participants and the relatively short follow-up period. We included a range of study designs with differences in measurement methods, varying definitions of the study outcomes, and differences in outcome reporting. It is difficult to exclude publication bias, although we did not locate evidence of unpublished trials. Although the total number of participants studied in this systematic review is small, with relatively short follow-up period, it seems likely that BH cannulation increases infection risk.
There is limited information on the use of BH cannulation, the extent of the practice, and the associated patient outcomes. The addition of cannulation method to routinely collected dialysis registry data will shed light on its postulated benefits, such as AVF preservation, and patient outcomes. Any future studies evaluating potential benefits from BH cannulation must monitor AVF infection as a safety outcome.
Our study suggests that BH cannulation in HHD patients is associated with increased infection rates, a finding consistent with a systematic review of 15 studies in the field. In addition, our study did not show benefits for AVF survival or reduced surgical interventions or demands on health services with the use of BH cannulation. Viewed together, an increase in infection rates with questionable benefit in AVF preservation or surgical intervention requirements questions the use of BH cannulation in routine clinical practice.
Disclosures
C.A.M., S.S.K., C.M.H., K.P., P.S., and M.J.J. have not received any financial support for involvement in this project. S.S.K. is supported by a National Health and Medical Research Council scholarship. M.J.J. is supported by The George Institute emerging researcher award. M.P.G. has received honoraria from Amgen and Roche in the last 3 years for speaking at educational meetings but has not received any financial support for involvement with this project.
Supplementary Material
Footnotes
C.A.M. and S.S.K. contributed equally to this work.
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03930413/-/DCSupplemental.
See related editorial, “Should Buttonhole Cannulation Be Discontinued?,” on pages 3–5.
References
- 1.KDOQI: Guidelines for Vascular Access, 2006. Available at: http://www.kidney.org Accessed September 3, 2013
- 2.Patel PR, Kallen AJ, Arduino MJ: Epidemiology, surveillance, and prevention of bloodstream infections in hemodialysis patients. Am J Kidney Dis 56: 566–577, 2010 [DOI] [PubMed] [Google Scholar]
- 3.Powe NR, Jaar B, Furth SL, Hermann J, Briggs W: Septicemia in dialysis patients: Incidence, risk factors, and prognosis. Kidney Int 55: 1081–1090, 1999 [DOI] [PubMed] [Google Scholar]
- 4.Taylor G, Gravel D, Johnston L, Embil J, Holton D, Paton S, Canadian Nosocomial Infection Surveillance Program. Canadian Hospital Epidemiology Committee : Incidence of bloodstream infection in multicenter inception cohorts of hemodialysis patients. Am J Infect Control 32: 155–160, 2004 [DOI] [PubMed] [Google Scholar]
- 5.Twardowski Z: The buttonhole method of needle insertion takes center stage in the attempt to revive daily home hemodialysis. Contemp Dial Nephrol 18: 18–19, 1977 [Google Scholar]
- 6.Ludlow V: Buttonhole cannulation in hemodialysis: Improved outcomes and increased expense—is it worth it? CANNT J 20: 29–37, 2010 [PubMed] [Google Scholar]
- 7.van Loon MM, Goovaerts T, Kessels AGH, van der Sande FM, Tordoir JHM: Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol Dial Transplant 25: 225–230, 2010 [DOI] [PubMed] [Google Scholar]
- 8.Verhallen AM, Kooistra MP, van Jaarsveld BC: Cannulating in haemodialysis: Rope-ladder or buttonhole technique? Nephrol Dial Transplant 22: 2601–2604, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Murcutt G: Buttonhole cannulation: Should this become the default technique for dialysis patients with native fistulas? Summary of the EDTNA/ERCA Journal Club discussion Autumn 2007. J Ren Care 34: 101–108, 2008 [DOI] [PubMed] [Google Scholar]
- 10.Glazer S, Diesto J, Crooks P, Yeoh H, Pascual N, Selevan D, Derose S, Farooq M: Going beyond the kidney disease outcomes quality initiative: Hemodialysis access experience at Kaiser Permanente Southern California. Ann Vasc Surg 20: 75–82, 2006 [DOI] [PubMed] [Google Scholar]
- 11.End Stage Renal Disease Renal Network 11 : Buttonhole Cannulation Results, 2008. Available at: http://www.esrdnet11.org/assets/fistula_first/network11_cannulation_report.pdf Accessed September 3, 2013 [Google Scholar]
- 12.Hallan S: Indicating Direction and Angle for Cannulating of AV Fistula in Hemodialysis Patients. NCT01536548, 2012. Available at: http://www.clinicaltrials.gov/ct2/show/NCT01536548?term=buttonhole&rank=3 Accessed May 15, 2013
- 13.Bammens B: Study of Pain, Anxiety and Complications Related to Cannulation of Arteriovenous (AV) Fistula in Chronic Hemodialysis Patients. NCT00544492, 2011. Available at: http://www.clinicaltrials.gov/ct2/show/NCT00544492?term=buttonhole&rank=2 Accessed May 15, 2013
- 14.Van Eps CL, Jones M, Ng T, Johnson DW, Campbell SB, Isbel NM, Mudge DW, Beller E, Hawley CM: The impact of extended-hours home hemodialysis and buttonhole cannulation technique on hospitalization rates for septic events related to dialysis access. Hemodial Int 14: 451–463, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Schünemann H, Brożek J, Oxman A, editors: GRADE Handbook for Grading Quality of Evidence and Strength of Recommendation, Version 3.2, 2009. Available at: Available from http://www.cc-ims.net/gradepro Accessed September 3, 2013 [Google Scholar]
- 16.Chow J, Rayment G, San Miguel S, Gilbert M: A randomised controlled trial of buttonhole cannulation for the prevention of fistula access complications. J Ren Care 37: 85–93, 2011 [DOI] [PubMed] [Google Scholar]
- 17.Struthers J, Allan A, Peel RK, Lambie SH: Buttonhole needling of ateriovenous fistulae: A randomized controlled trial. ASAIO J 56: 319–322, 2010 [DOI] [PubMed] [Google Scholar]
- 18.Labriola L, Crott R, Desmet C, André G, Jadoul M: Infectious complications following conversion to buttonhole cannulation of native arteriovenous fistulas: A quality improvement report. Am J Kidney Dis 57: 442–448, 2011 [DOI] [PubMed] [Google Scholar]
- 19.MacRae JM, Ahmed SB, Atkar R, Hemmelgarn BR: A randomized trial comparing buttonhole with rope ladder needling in conventional hemodialysis patients. Clin J Am Soc Nephrol 7: 1632–1638, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaux E, King J, Lloyd S, Moore J, Bailey L, Reading I, Naik R: Effect of buttonhole cannulation with a polycarbonate PEG on in-center hemodialysis fistula outcomes: A randomized controlled trial. Am J Kidney Dis 62: 81–88, 2013 [DOI] [PubMed] [Google Scholar]
- 21.Birchenough E, Moore C, Stevens K, Stewart S: Buttonhole cannulation in adult patients on hemodialysis: An increased risk of infection? Nephrol Nurs J 37: 491–498, 2010 [PubMed] [Google Scholar]
- 22.Nesrallah GE, Cuerden M, Wong JHS, Pierratos A: Staphylococcus aureus bacteremia and buttonhole cannulation: Long-term safety and efficacy of mupirocin prophylaxis. Clin J Am Soc Nephrol 5: 1047–1053, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Divi D, Du Toit D, Hiremagalur B, Parnham A, Titus T, Kurtkoti J: Buttonhole cannulation and blood stream infection—is there a link? Nephrology (Carlton) 15: 37, 2010. 20586946 [Google Scholar]
- 24.Ward F, Holian J, Watson A: Arteriovenous fistula buttonhole cannulation: Early experience in an Irish haemodialysis unit. Nephrol Dial Transplant 26: 3825, 2011 [DOI] [PubMed] [Google Scholar]
- 25.O'Brien FJ, Kok HKT, O'Kane C, McWilliams J, O'Kelly P, Collins P, Walshe J, Magee CC, Denton MD, Conlon PJ: Arterio-venous fistula buttonhole cannulation technique: A retrospective analysis of infectious complications. Clin Kidney J 5: 526–529, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xue H, Ix JH, Wang W, Brunelli SM, Lazarus M, Hakim R, Lacson E, Jr: Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis 61: 123–130, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Komenda P, Gavaghan MB, Garfield SS, Poret AW, Sood MM: An economic assessment model for in-center, conventional home, and more frequent home hemodialysis. Kidney Int 81: 307–313, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jun M, Jardine MJ, Gray N, Masterson R, Kerr PG, Agar JW, Hawley CM, van Eps C, Cass A, Gallagher M, Perkovic V: Outcomes of extended-hours hemodialysis performed predominantly at home. Am J Kidney Dis 61: 247–253, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Rooijens PPGM, Tordoir JHM, Stijnen T, Burgmans JPJ, Smet de AA, Yo TI: Radiocephalic wrist arteriovenous fistula for hemodialysis: Meta-analysis indicates a high primary failure rate. Eur J Vasc Endovasc Surg 28: 583–589, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Weinhandl ED, Liu J, Gilbertson DT, Arneson TJ, Collins AJ: Survival in daily home hemodialysis and matched thrice-weekly in-center hemodialysis patients. J Am Soc Nephrol 23: 895–904, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.