Summary
Background and objectives
The vast majority of US dialysis facilities are for-profit and profit status has been associated with processes of care and outcomes in patients on dialysis. This study examined whether dialysis facility profit status was associated with the rate of hospitalization in patients starting dialysis.
Design, setting, participants, & methods
This was a retrospective cohort study of Medicare beneficiaries starting dialysis between 2005 and 2008 using data from the US Renal Data System. All-cause hospitalization was examined and compared between for-profit and nonprofit dialysis facilities through 2009 using Poisson regression. Companion analyses of cause-specific hospitalization that are likely to be influenced by dialysis facility practices including hospitalizations for heart failure and volume overload, access complications, or hyperkalemia were conducted.
Results
The cohort included 150,642 patients. Of these, 12,985 (9%) were receiving care in nonprofit dialysis facilities. In adjusted models, patients receiving hemodialysis in for-profit facilities had a 15% (95% confidence interval [95% CI], 13% to 18%) higher relative rate of hospitalization compared with those in nonprofit facilities. Among patients receiving peritoneal dialysis, the rate of hospitalization in for-profit versus nonprofit facilities was not significantly different (relative rate, 1.07; 95% CI, 0.97 to 1.17). Patients on hemodialysis receiving care in for-profit dialysis facilities had a 37% (95% CI, 31% to 44%) higher rate of hospitalization for heart failure or volume overload and a 15% (95% CI, 11% to 20%) higher rate of hospitalization for vascular access complications.
Conclusions
Hospitalization rates were significantly higher for patients receiving hemodialysis in for-profit compared with nonprofit dialysis facilities.
Introduction
There has been considerable debate about whether and the extent to which the profit status of a health care organization is linked to quality of care or outcomes in the United States. Persuasive arguments can be made for either a detrimental or favorable influence of for-profit status on outcomes. The economic incentives inherent to for-profit organizations may not align with delivery of high-quality care, but alternatively, for-profit organizations may provide more efficient, innovative care and invest capital to achieve these goals (1). This debate is particularly relevant to the care of patients on dialysis, a unique health care sector in which >80% of dialysis facilities are for-profit (2) and in which the Prospective Payment System and Quality Incentive Program implemented by the Centers for Medicare and Medicaid Services (CMS) are likely to influence the delivery of dialysis care.
Several prior studies have examined the association between dialysis facility profit status and processes of care or selected outcomes. A systematic review and meta-analysis examining data from 1973 through 1997 found for-profit hemodialysis care to be associated with a higher risk of mortality (3). When more recent data from 2004 through 2006 were examined, Zhang et al. also found a higher risk of mortality among patients on hemodialysis receiving care at for-profit, free-standing dialysis facilities (4). Although several studies have focused on the relation between dialysis ownership and death, few studies have focused on other important outcomes such as hospitalization and referral for, or receipt of, kidney transplantation.
Hospitalization is a particularly important outcome to consider because ESRD requiring dialysis is associated with high rates of hospitalization, with a median of two hospitalizations per year and 12 days spent in the hospital annually (5). Care at for-profit dialysis facilities has been associated with more hospital days (6) and lower likelihood of being placed on the waiting list for kidney transplantation (7). However, to our knowledge, no studies of hospitalization have been reported since the ownership of dialysis facilities has been largely consolidated by two large, for-profit entities. Our study sought to examine whether dialysis facility profit status was associated with the rate of hospitalization after accounting for geographic region and patient characteristics.
Materials and Methods
Study Design and Participants
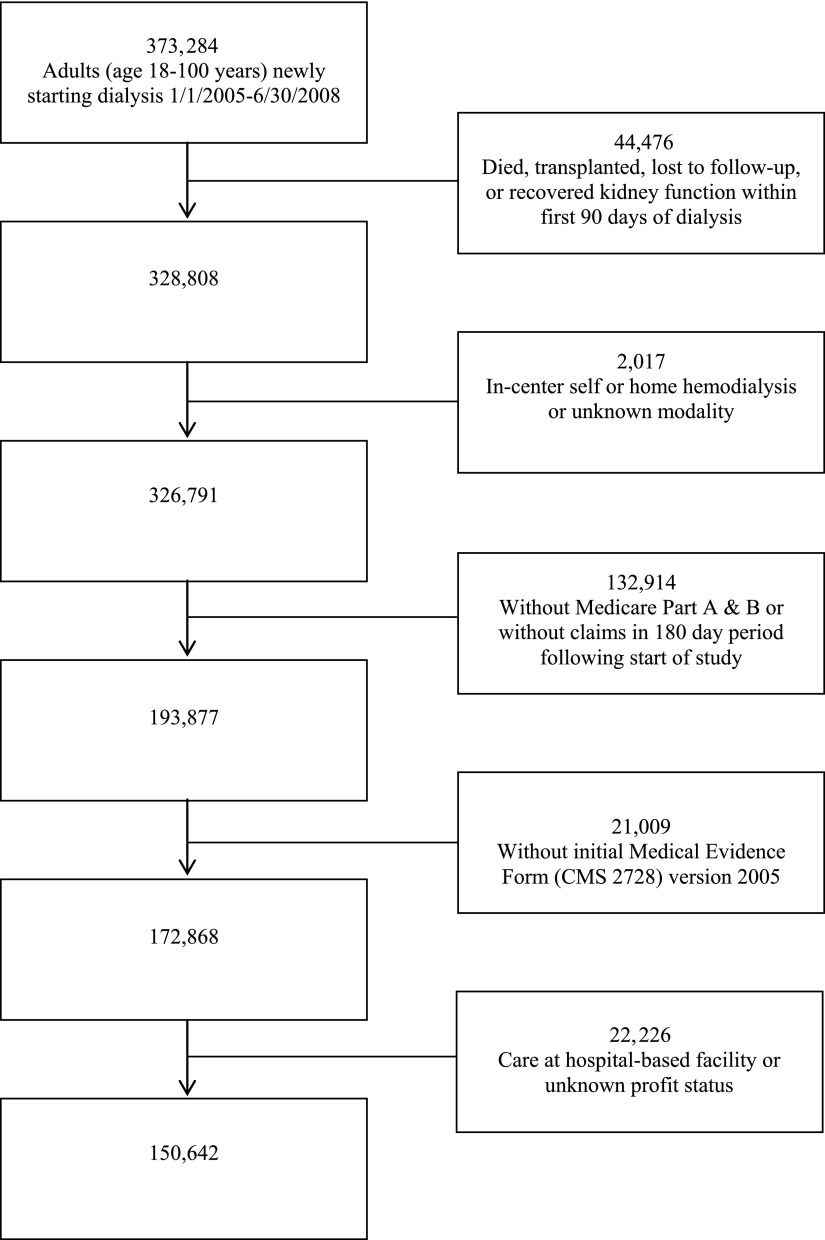
We conducted a retrospective cohort study using the US Renal Data System (USRDS), an administrative database that includes the vast majority of patients receiving care for ESRD in the United States. We included all adults (aged 18–100 years) starting dialysis between January 1, 2005 and June 30, 2008. Patients who died, received a kidney transplant, recovered kidney function, or were lost to follow-up in the first 90 days of dialysis were excluded. We limited the cohort to patients with Medicare as the primary payer (Part A and Part B) on day 91 of dialysis and with at least one institutional claim, which includes dialysis-related claims, during the 180-day period after the start of our study. The cohort was further restricted to patients receiving in-center hemodialysis or peritoneal dialysis at a free-standing dialysis facility with known profit status on day 91 of dialysis (i.e., excluding patients receiving care at hospital-based facilities and the <1% of patients on home hemodialysis), and with available data from the Medical Evidence Form (CMS 2728) version 2005 (Figure 1).
Figure 1.
Cohort selection. The figure shows inclusion and exclusion criteria and selection of the cohort. CMS, Centers for Medicare and Medicaid Services.
Data Collection
Patient- and facility-level data were collected from the USRDS Standard Analytic Files (8). Patient-level data included demographics, comorbidities, vascular access type at start of dialysis, selected laboratory measures obtained before the start of dialysis, residence at an assisted living, skilled nursing or other facility, nephrology care before ESRD, and dialysis modality on day 91. Facility-level characteristics included profit status (for-profit, nonprofit), chain ownership defined by the USRDS as ≥20 facilities in ≥2 states owned by the same corporation (8), state, and ESRD Network. We defined region based on ESRD networks as follows: Northeast, networks 1, 2, 3, and 4; South, networks 5, 6, 7, 8, 13, and 14; Midwest, networks 9, 10, 11, and 12; and West, networks 15, 16, 17, and 18.
Exposure and Outcome
The primary exposure of interest was facility profit status. The primary outcome of interest was the rate of all-cause hospitalization after the first 90 days of dialysis. The cohort was followed longitudinally for all-cause hospitalization(s) through December 31, 2009. Patients were censored at the time of transfer to a facility associated with a change in profit status or region (n=13,913), transfer to a hospital-based facility (n=28,553), or change in dialysis modality (n=9054). Patients were followed until transplant (n=3778), recovery of kidney function (n=2121), loss to follow-up (n=973), death (n=45,792), or study end (n=46,458).
Statistical Analyses
We compared baseline characteristics using the t test or the chi-squared test. All analyses were stratified based on dialysis modality: in-center hemodialysis or peritoneal dialysis. First, we examined unadjusted all-cause hospitalization rates per 100 person-years for nonprofit and for-profit dialysis facilities by region. The relative rate (RR) or risk of hospitalization(s) in for-profit compared with nonprofit facilities was modeled using Poisson regression adjusted for patient-level factors including demographics (age, sex, race, ethnicity), comorbidities (congestive heart failure, atherosclerotic heart disease, cerebrovascular disease, peripheral vascular disease, hypertension, amputation, diabetes, chronic obstructive pulmonary disease, cancer, inability to ambulate or transfer), residence at a skilled nursing, assisted living, or other facility, current tobacco use, prior nephrology care, and estimated GFR (eGFR) based on the four-variable Modification of Diet in Renal Disease study equation (9) and region. Because a large proportion of participants had missing data on serum albumin (23% and 22% for hemodialysis and peritoneal dialysis, respectively), we performed analyses with and without serum albumin. We examined Poisson models with and without accounting for overdispersion and also explored generalized linear mixed Poisson models with facility-specific random intercepts to account for facility (cluster) effects. The results and conclusions were similar across each of the models, so we selected the Poisson model accounting for overdispersion as the primary model. Overdispersion is typical in count data and was evident with our data; thus, we accounted for overdispersion in our modeling to provide valid inference. Only those patients with complete data on the variables of interest were included in the multivariable models. An additional 533 hemodialysis and 30 peritoneal dialysis patients with missing eGFR were not included in the final multivariable models.
We conducted multiple sensitivity analyses to assess the robustness of our findings. First, we conducted a sensitivity analysis that included an indicator of socioeconomic status, dual Medicare and Medicaid eligibility, to assess whether the findings changed when considering socioeconomic status. To examine whether discontinuation of patient follow-up at the time of change in profit status, transfer to a hospital-based facility, change in dialysis modality, or transfer to a new region introduced bias into our estimates, we conducted a sensitivity analysis that did not censor follow-up time when these events occurred.
In companion analyses, from the 15 leading causes of hospitalization, we identified types of hospitalizations that may potentially be modifiable by facility practices: congestive heart failure and volume overload, dialysis access related, and hyperkalemia. We identified International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes consistent with these diagnoses and expanded the ICD-9-CM codes examined to ensure complete ascertainment of these types of hospitalizations (see the Supplemental Material). We examined the principal discharge diagnosis to determine cause-specific hospitalization. We then compared patients in for-profit facilities with patients in nonprofit facilities, to see whether there were significant differences in the RRs of cause-specific hospitalizations after adjusting for region, demographics, coexisting illnesses, tobacco use, prior nephrology care, institutionalization, and baseline eGFR. The study was approved by the University of California Davis Institutional Review Board.
Results
After exclusions, the final cohort included 150,642 patients. Of these, 12,985 patients (9%) were receiving care in nonprofit dialysis facilities at day 91. Patient characteristics are shown in Table 1. In adults on hemodialysis, baseline characteristics differed among those in for-profit compared with nonprofit facilities. The proportion of patients with hemodialysis catheters at the start of dialysis was higher in for-profit facilities, whereas the prevalence of atherosclerotic heart disease, cerebrovascular accident or transient ischemic attack, cancer, pulmonary disease, and inability to ambulate or transfer was significantly higher in nonprofit facilities. The proportion of patients with reported nephrology care before ESRD was higher in nonprofit facilities, and the distribution of patients by profit status differed by region. In adults on peritoneal dialysis, the prevalence of baseline chronic diseases was similar among patients in for-profit and nonprofit dialysis facilities. In patients on hemodialysis or peritoneal dialysis, a larger proportion of Hispanic adults received care in for-profit facilities and there was no difference in dual Medicare and Medicaid eligibility by profit status. The median follow-up time for patients on hemodialysis and peritoneal dialysis was 478 and 391 days, respectively, in our primary analysis.
Table 1.
Baseline characteristics of patients with Medicare initiating dialysis according to dialysis modality and facility profit status
| Characteristic | Hemodialysis (n=140,665) | Peritoneal Dialysis (n=9977) | ||||
|---|---|---|---|---|---|---|
| For-Profit (n=128,576) | Nonprofit (n=12,089) | P Value | For-Profit (n=9081) | Nonprofit (n=896) | P Value | |
| Region | <0.001 | <0.001 | ||||
| Midwest | 28,925 (22) | 3270 (27) | 2286 (25) | 190 (21) | ||
| Northeast | 19,766 (15) | 1958 (16) | 1098 (12) | 101 (11) | ||
| South | 59,468 (46) | 3981 (33) | 4264 (47) | 298 (33) | ||
| West | 20,417 (16) | 2880 (24) | 1433 (16) | 307 (34) | ||
| Age (yr) | 65.5±14.8 | 65.4±14.9 | 0.77 | 61.2±15.8 | 60.9±15.7 | 0.56 |
| Male | 69,685 (54) | 6688 (55) | 0.02 | 5029 (55) | 511 (57) | 0.34 |
| Race | <0.001 | <0.001 | ||||
| White | 83,833 (65) | 7883 (65) | 6908 (76) | 647 (72) | ||
| Black | 38,959 (30) | 3514 (29) | 1745 (19) | 176 (20) | ||
| Asian | 3140 (2) | 383 (3) | 220 (2) | 49 (5) | ||
| Native American | 1366 (1) | 200 (2) | 103 (1) | 13 (1) | ||
| Pacific Islander | 849 (1) | 68 (1) | 68 (1) | 8 (1) | ||
| Multiracial, other, unknown | 429 (0.3) | 41 (0.3) | 37 (0.4) | 3 (0.3) | ||
| Hispanic | 16,888 (13) | 830 (7) | <0.001 | 1073 (12) | 53 (6) | <0.001 |
| Medicare and Medicaid dual eligibility | 50,653 (39) | 4786 (40) | 0.68 | 2606 (29) | 243 (27) | 0.32 |
| Body mass index (kg/m2) | 28.7±8.0 | 28.4±7.8 | <0.001 | 28.4±6.9 | 28.1±6.9 | 0.18 |
| Tobacco use, current smoker | 8083 (6) | 1032 (9) | <0.001 | 650 (7) | 75 (8) | 0.18 |
| Diabetes | 76,999 (60) | 7077 (59) | <0.01 | 4812 (53) | 469 (52) | 0.71 |
| Atherosclerotic heart disease | 30,095(23) | 3276 (27) | <0.001 | 1752 (19) | 197 (22) | 0.05 |
| Cerebrovascular accident or transient ischemic attack | 13,795 (11) | 1572 (13) | <0.001 | 658 (7) | 67 (7) | 0.80 |
| Peripheral vascular disease | 20,354 (16) | 2096 (17) | <0.001 | 1088 (12) | 115 (13) | 0.45 |
| Congestive heart failure | 47,249 (37) | 4523 (37) | 0.15 | 2169 (24) | 207 (23) | 0.60 |
| Amputation | 4319 (3) | 480 (4) | <0.001 | 177 (2) | 16 (2) | 0.73 |
| Hypertension | 113,546 (88) | 10,740 (89) | 0.08 | 8015 (88) | 784 (88) | 0.50 |
| Cancer | 9284 (7) | 1108 (9) | <0.001 | 496 (5) | 58 (6) | 0.21 |
| Chronic obstructive pulmonary disease | 12,554 (10) | 1455 (12) | <0.001 | 556 (6) | 52 (6) | 0.70 |
| Etiology of renal disease | <0.001 | 0.20 | ||||
| Diabetes | 61,276 (48) | 5544 (46) | 3993 (44) | 398 (44) | ||
| Hypertension | 39,850 (31) | 3566 (29) | 2624 (29) | 239 (27) | ||
| GN | 6853 (5) | 766 (6) | 961 (11) | 86 (10) | ||
| Cystic kidney | 1803 (1) | 209 (2) | 341 (4) | 41 (5) | ||
| Other or unknown | 18,794 (15) | 2004 (17) | 1162 (13) | 132 (15) | ||
| Inability to ambulate or transfer | 9179 (7) | 1074 (9) | <0.001 | 172 (2) | 14 (2) | 0.48 |
| Institutionalization | <0.001 | 0.86 | ||||
| Assisted living | 892 (1) | 142 (1) | 18 (0.2) | 2 (0.2) | ||
| Nursing home | 8655 (7) | 948 (8) | 75 (1) | 5 (1) | ||
| Other | 530 (0.4) | 73 (0.6) | 11 (0.1) | 1 (0.1) | ||
| Prior nephrology care (mo) | <0.001 | <0.01 | ||||
| <6 | 13,147 (10) | 1443 (12) | 1245 (14) | 129 (14) | ||
| 6–12 | 30,795 (24) | 2987 (25) | 2708 (30) | 247 (28) | ||
| >12 | 29,171 (23) | 3386 (28) | 3210 (35) | 367 (41) | ||
| Unknown | 15,894 (12) | 909 (8) | 544 (6) | 34 (4) | ||
| Hemoglobin (g/dl) | 10.0±1.7 | 10.1±1.7 | 0.52 | 10.7±1.7 | 10.6±1.8 | 0.84 |
| Estimated GFR (ml/min per 1.73 m2) | 11.1±5.7 | 10.9±5.5 | <0.001 | 10.9±5.1 | 11.0±5.5 | 0.66 |
| Albumin (g/dl) | 0.28 | 0.86 | ||||
| <2.5 | 17,639 (14) | 1613 (13) | 522 (6) | 45 (5) | ||
| 2.5–2.9 | 21,364 (17) | 2048 (17) | 906 (10) | 93 (10) | ||
| 3.0–3.4 | 27,208 (21) | 2563 (21) | 1622 (18) | 148 (17) | ||
| 3.5–3.9 | 21,882 (17) | 2149 (18) | 2247 (25) | 212 (24) | ||
| ≥4.0 | 10,340 (8) | 1006 (8) | 1841 (20) | 181 (20) | ||
| Missing | 30,143 (23) | 2710 (22) | 1943 (21) | 217 (24) | ||
| Access typea | <0.001 | |||||
| Arteriovenous fistula | 17,330 (13) | 2052 (17) | ||||
| Arteriovenous graft | 5993 (5) | 549 (5) | ||||
| Catheter | 103,094 (80) | 9321 (77) | ||||
| Other | 1627 (1) | 104 (1) | ||||
| Missing | 532 (0.4) | 63 (0.5) | ||||
Data are presented as the mean ± SD or n (%).
Hemodialysis
The unadjusted hospitalization rates in nonprofit facilities and for-profit facilities were 146 and 169 per 100 person-years in patients on hemodialysis, respectively. When region-specific unadjusted rates of hospitalization were examined, higher rates of all-cause hospitalization were observed in patients on hemodialysis receiving care in for-profit facilities in all regions, although the RR did not reach statistical significance in the Northeast (Table 2).
Table 2.
Unadjusted hospitalization rates by profit status and region
| Region | For-Profit Rate per 100 Person-Years | Nonprofit Rate per 100 Person-Years | Relative Rate (95% Confidence Interval) | P Value |
|---|---|---|---|---|
| Hemodialysis | ||||
| Overall | 169 | 146 | 1.16 (1.12 to 1.18) | <0.001 |
| Northeast | 170 | 162 | 1.05 (0.99 to 1.11) | 0.09 |
| South | 171 | 153 | 1.12 (1.08 to 1.16) | <0.001 |
| Midwest | 177 | 151 | 1.17 (1.12 to 1.22) | <0.001 |
| West | 155 | 123 | 1.26 (1.20 to 1.32) | <0.001 |
| Peritoneal dialysis | ||||
| Overall | 110 | 99 | 1.12 (1.02 to 1.22) | 0.02 |
| Northeast | 117 | 118 | 0.99 (0.77 to 1.28) | 0.97 |
| South | 115 | 97 | 1.19 (1.01 to 1.39) | 0.03 |
| Midwest | 117 | 118 | 0.99 (0.82 to 1.20) | 0.93 |
| West | 81 | 85 | 0.96 (0.81 to 1.14) | 0.62 |
In fully adjusted models, patients on hemodialysis in for-profit facilities had a 15% (95% confidence interval [95% CI], 13% to 18%) higher RR of hospitalization compared with those in nonprofit facilities (Table 3). As expected, the presence of comorbidities such as diabetes, heart failure, and chronic obstructive pulmonary disease, inability to ambulate or transfer, residence in a care facility, and higher eGFR at the start of dialysis were associated with a higher risk of hospitalization (Table 3). Nephrology care before hemodialysis was associated with a 12% lower rate of hospitalization.
Table 3.
Multivariable Poisson regression and relative rate of all-cause hospitalization in patients on hemodialysis (n=140,132)
| Variable | Relative Rate (95% Confidence Interval) | P Value |
|---|---|---|
| For-profit | 1.15 (1.13 to 1.18) | <0.001 |
| Region | ||
| Northeast | 1.08 (1.05 to 1.10) | <0.001 |
| South | 1.10 (1.08 to 1.12) | <0.001 |
| Midwest | 1.06 (1.04 to 1.09) | <0.001 |
| West | Reference | |
| Age (yr) | ||
| 18–44 | 1.17 (1.15 to 1.19) | <0.001 |
| 45–64 | Reference | |
| 65–74 | 0.99 (0.98 to 1.01) | 0.29 |
| 75–84 | 1.06 (1.04 to 1.08) | <0.001 |
| ≥85 | 1.14 (1.11 to 1.17) | <0.001 |
| Male | 0.83 (0.82 to 0.84) | <0.001 |
| Race | ||
| Black | 0.92 (0.91 to 0.93) | <0.001 |
| Other | 0.84 (0.82 to 0.87) | <0.001 |
| White | Reference | |
| Hispanic | 0.93 (0.91 to 0.94) | <0.001 |
| Congestive heart failure | 1.13 (1.12 to 1.15) | <0.001 |
| Atherosclerotic heart disease | 1.03 (1.02 to 1.05) | <0.001 |
| Cerebrovascular disease | 1.07 (1.05 to 1.09) | <0.001 |
| Peripheral vascular disease | 1.09 (1.07 to 1.11) | <0.001 |
| Hypertension | 0.90 (0.88 to 0.91) | <0.001 |
| History of amputation | 1.11 (1.08 to 1.15) | <0.001 |
| Diabetes mellitus | 1.18 (1.16 to 1.19) | <0.001 |
| Chronic obstructive pulmonary disease | 1.22 (1.20 to 1.24) | <0.001 |
| Tobacco use, current smoker | 1.15 (1.12 to 1.17) | <0.001 |
| Cancer | 1.12 (1.09 to 1.15) | <0.001 |
| Inability to ambulate or transfer | 1.11 (1.08 to 1.13) | <0.001 |
| Residence in skilled nursing facility, assisted living, or other | 1.19 (1.17 to 1.22) | <0.001 |
| Prior nephrology care | ||
| Yes | 0.88 (0.86 to 0.89) | <0.001 |
| Unknown | 1.06 (1.04 to 1.08) | <0.001 |
| No | Reference | |
| Estimated GFR (per 5 ml/min per 1.73 m2) | 1.08 (1.07 to 1.09) | <0.001 |
Data are adjusted for all variables shown.
Peritoneal Dialysis
The unadjusted hospitalization rates in nonprofit and for-profit facilities were 99 and 110 per 100 person-years, respectively, among patients starting peritoneal dialysis (Table 2). Adjusted analyses showed nominally higher rates of hospitalization in for-profit facilities that did not reach the level of significance (RR, 1.07; 95% CI, 0.97 to 1.17) (Table 4). Similar to observations in patients on hemodialysis, comorbidities including heart failure, diabetes, and chronic obstructive pulmonary disease, higher eGFR at the start of dialysis, and an inability to ambulate or transfer were associated with higher hospitalization rates.
Table 4.
Multivariable Poisson regression and relative rate of all-cause hospitalization in patients on peritoneal dialysis (n=9947)
| Variable | Relative Rate (95% Confidence Interval) | P Value |
|---|---|---|
| For-profit | 1.07 (0.97 to 1.17) | 0.16 |
| Region | ||
| Northeast | 1.31 (1.19 to 1.40) | <0.001 |
| South | 1.26 (1.17 to 1.36) | <0.001 |
| Midwest | 1.25 (1.15 to 1.35) | <0.001 |
| West | Reference | |
| Age (yr) | ||
| 18–44 | 1.20 (1.11 to 1.29) | <0.001 |
| 45–64 | Reference | |
| 65–74 | 1.04 (0.98 to 1.11) | 0.23 |
| 75–84 | 1.15 (1.06 to 1.23) | <0.001 |
| ≥85 | 1.46 (1.25 to 1.69) | <0.001 |
| Male | 0.88 (0.84 to 0.93) | <0.001 |
| Race | ||
| Black | 1.12 (1.06 to 1.20) | <0.001 |
| Other | 0.74 (0.65 to 0.84) | <0.001 |
| White | Reference | |
| Hispanic | 0.89 (0.81 to 0.96) | 0.005 |
| Congestive heart failure | 1.24 (1.17 to 1.32) | <0.001 |
| Atherosclerotic heart disease | 1.05 (0.98 to 1.12) | 0.14 |
| Cerebrovascular disease | 1.09 (0.99 to 1.20) | 0.07 |
| Peripheral vascular disease | 1.08 (1.00 to 1.17) | 0.04 |
| Hypertension | 0.87 (0.81 to 0.94) | <0.001 |
| History of amputation | 1.11 (0.93 to 1.33) | 0.23 |
| Diabetes mellitus | 1.44 (1.37 to 1.52) | <0.001 |
| Chronic obstructive pulmonary disease | 1.25 (1.14 to 1.38) | <0.001 |
| Tobacco use, current smoker | 1.11 (1.02 to 1.22) | 0.02 |
| Cancer | 1.12 (1.01 to 1.24) | 0.04 |
| Inability to ambulate or transfer | 1.46 (1.23 to 1.74) | <0.001 |
| Residence in a skilled nursing facility, assisted living, or other | 1.22 (0.97 to 1.52) | 0.08 |
| Prior nephrology care | ||
| Yes | 0.97 (0.90 to 1.04) | 0.35 |
| Unknown | 1.01 (0.90 to 1.14) | 0.88 |
| No | Reference | |
| Estimated GFR (per 5 ml/min per 1.73 m2) | 1.04 (1.02 to 1.07) | 0.001 |
Data are adjusted for all variables shown.
Sensitivity Analyses
We found no substantive change in the association between profit status and risk of hospitalization when we adjusted for dual Medicare and Medicaid eligibility. Patients on hemodialysis in for-profit facilities experienced a significantly higher rate of hospitalization (RR, 1.16; 95% CI, 1.13 to 1.18), whereas patients on peritoneal dialysis did not (RR, 1.06; 95% CI, 0.97 to 1.16). Dual Medicare and Medicaid eligibility was independently associated with an 18% (95% CI, 17% to 20%) higher rate of hospitalization in patients on hemodialysis and a 24% (95% CI, 17% to 32%) higher rate of hospitalization in patients on peritoneal dialysis. In our sensitivity analysis allowing for follow-up, regardless of transfer to a facility with a different profit status, hospital-based facility, or new region or change in dialysis modality, we found that patients on hemodialysis in for-profit facilities had a significantly higher rate of hospitalization (RR, 1.08; 95% CI, 1.06 to 1.10) as did patients on peritoneal dialysis (RR, 1.08; 95% CI, 1.01 to 1.16). However, these results should be interpreted differently than those of our primary model, because the conclusions now only apply to those who start dialysis at a free-standing facility on either hemodialysis or peritoneal dialysis. For example, the findings with respect to peritoneal dialysis are likely related to hospitalization that occurs after transition from peritoneal dialysis to hemodialysis, changing the interpretation of the overall risk estimate.
Hospitalizations for Heart Failure, Vascular Access Complications, and Hyperkalemia
When we examined leading causes of hospitalization in patients on hemodialysis that would potentially be influenced by dialysis facility care or related to processes of care, we found significant differences between for-profit and nonprofit facilities in adjusted analyses. The RRs of hospitalization for congestive heart failure or volume overload and for vascular access-related complications were significantly higher in for-profit facilities, whereas rates for hyperkalemia were similar overall (Table 5). When we restricted vascular access complications to those that only included infection or inflammation (ICD-9-CM 996.62), we found that patients on hemodialysis receiving care in for-profit facilities had a 22% (95% CI, 17% to 28%) higher adjusted RR compared with patients in nonprofit facilities.
Table 5.
Rates for cause-specific hospitalization by profit status and the adjusted relative rate among patients on hemodialysis
| Cause of Hospitalization | For-Profit per 100 Person-Years | Nonprofit per 100 Person-Years | Relative Rate (95% Confidence Interval)a | P Value |
|---|---|---|---|---|
| Complications of vascular access or renal device, implant or graft | 20.7 | 17.2 | 1.15 (1.11 to 1.20) | <0.001 |
| Congestive heart failure or fluid overload | 17.2 | 12.3 | 1.37 (1.31 to 1.44) | <0.001 |
| Hyperkalemia | 2.53 | 2.45 | 1.04 (0.99 to 1.09) | 0.14 |
Comparison of for-profit versus nonprofit adjusted for region, age, race, sex, ethnicity, heart failure, atherosclerotic heart disease, cerebrovascular disease, peripheral vascular disease, hypertension, amputation, diabetes, chronic obstructive pulmonary disease, tobacco use, cancer, inability to ambulate/transfer, residence in care facility, prior nephrology care, and estimated GFR at initiation of dialysis.
Because of the relatively small number of patients on peritoneal dialysis and the lack of a statistically significant difference overall, cause-specific hospitalization rates among patients starting peritoneal dialysis were not examined.
Discussion
In our study, for-profit dialysis facility status was associated with higher risk of all-cause hospitalization in patients on hemodialysis starting dialysis with Medicare as the primary payer, even after accounting for geographic region and multiple patient characteristics. We conducted multiple sensitivity analyses and consistently found that patients receiving hemodialysis in for-profit facilities had a significantly higher rate of hospitalization. Furthermore, specific types of hospitalization (which we considered potentially modifiable by facility practices) were observed at higher rates in patients on hemodialysis receiving care in for-profit dialysis facilities.
Our study is one of relatively few to examine differences in hospitalization by profit status. Lee et al. found that Medicare beneficiaries in for-profit dialysis facilities spent on average 17% more days in the hospital (roughly equivalent to 3 days annually) compared with patients in nonprofit facilities (6). Other studies have examined the association between profit status and death, with mixed results (3,7,10,11). Proposed mechanisms by which profit status and organizational structure may be linked to adverse outcomes include differences in staffing, training level of staff, and specific differences in treatment or processes of care such as hemodialysis session length and medication dosing protocols (3,12). Studies conducted in the 1980s and 1990s found that for-profit dialysis facilities compared with nonprofit facilities provided a higher number of treatments after accounting for labor and capital resources and shorter dialysis treatments (13,14). These differences, in combination with other unexamined processes of care, may explain observed differences in rates of hospitalization. It is interesting that we observed significant differences in hospitalization rates related to profit status only among patients on hemodialysis, whose care might be more facility dependent than that of peritoneal dialysis patients, owing to more frequent visits.
Because for-profit facilities have changed considerably over the past decade, as a result of industry consolidation, economies of scale, and coordinated efforts to reduce errors (e.g., by establishing uniform protocols and electronic health records), we believed that re-examining outcomes was critical, because these changes might have eliminated or reversed previously reported differences between outcomes of for-profit and nonprofit dialysis care. Our findings highlight the need to examine whether there are processes of care that differ by profit status or organizational structure and whether these processes are modifiable risk factors for hospitalization, particularly among patients on hemodialysis. Clinical areas of interest include session length for patients on hemodialysis, cycler versus noncycler use for patients on peritoneal dialysis, management of volume and dry weight assessment, staffing models, physician practices, the culture of safety within dialysis facilities, and differences in preventive care within dialysis facilities. Understanding these differences may have a significant positive effect on patient outcomes and reduce the overall cost of caring for patients on dialysis. In terms of cost, inpatient services accounted for a staggering 38% of Medicare expenditures on ESRD in 2010—a higher percentage of Medicare spending than outpatient care (34%) or physician and supplier costs (21%) (5). Our study has several strengths. It is one of few studies to examine profit status and the rate (risk) of hospitalization.
Our study examined a large cohort of Medicare Part A and B beneficiaries newly starting dialysis, representing a large proportion of the current dialysis population. Furthermore, we conducted multiple sensitivity analyses to assess the robustness of our findings. In companion analyses, we also identified specific types of hospitalization in patients on hemodialysis that warrant further attention including heart failure and volume management and dialysis access-related hospitalizations.
Our study also has important limitations. We cannot exclude that some or all of the observed differences between for-profit and nonprofit facilities relate to residual confounding (unmeasured or misclassified confounders) or unmeasured disease severity among factors for which we did adjust. We only examined free-standing dialysis facilities; thus, our conclusions should not be generalized to hospital-based facilities. Our findings are only generalizable to Medicare Part A and B beneficiaries with Medicare coverage by day 91 of dialysis. Whether the same findings would be observed in patients with employer-based group health plans or those who are not eligible for Medicare is unknown. Our study cannot establish causality and cannot determine reasons for the observed differences due to limitations in administrative data. Finally, we had available data through 2009. Since 2009, practices have continued to evolve, with large for-profit dialysis organizations implementing quality improvement initiatives focused on extracellular volume management (15), reduction of tunneled dialysis catheter use, and the expansion of programs that focus on the first 120 days of dialysis as a high-risk period (16). Furthermore, a special feature (17) and commentary (18) published in CJASN in 2011 and 2012, respectively, outlined and advocated for a new pathway of care for patients on dialysis with the goal of improving outcomes and quality of life, including greater attention to volume management, reduction in tunneled catheter use, comprehensive and focused care in the first 90–120 days of dialysis, and prevention of infection. Understanding how widespread implementation of quality initiatives and changes in processes of care affect outcomes will be critical in the coming years.
Our study cannot examine in detail the process of patient selection of and physician referral to dialysis facilities. On the basis of our experience, outpatient dialysis facility selection may be influenced by the following: proximity of the dialysis facility to a patient’s home, referring physician affiliation with local dialysis facility, region and residence (with some areas having few dialysis facilities to select from), availability of the patient’s desired dialysis schedule, and facility layout and amenities (e.g., personal television). Overall, we have no reason to expect that patient choice of facility is associated with the outcomes examined herein. In our cohort, regional differences were observed with a higher percentage of patients on the West coast receiving care in nonprofit dialysis facilities. In addition, patients receiving care in nonprofit dialysis facilities appeared to have worse baseline health, a difference that would have been expected to bias our results in the opposite direction of that observed (i.e., patients in nonprofit facilities would have been expected to have higher hospitalization rates given worse baseline health).
In conclusion, care in for-profit dialysis facilities was associated with higher RRs of hospitalization in patients on hemodialysis. These findings highlight the need to carefully examine facility characteristics– in for-profit and nonprofit facilities alike– related to hospitalization. Modifying processes of care that contribute to higher rates of hospitalization should enhance the health and well-being of patients on dialysis, and should in turn reduce ESRD program expenditures.
Disclosures
L.S.D., B.G., and G.A.K. receive research funding from Dialysis Clinic Inc., a nonprofit dialysis organization. G.A.K. has received support from the Renal Research Institute, a partnership between Fresenius Medical Care and Beth Israel Medical Center. G.M.C. serves on the Board of Directors of Satellite Healthcare Inc. and the Scientific Advisory Board of DaVita Clinical Research.
Supplementary Material
Acknowledgments
An abstract based on this study was selected for an oral presentation at the American Society of Nephrology Kidney Week on November 7, 2013, in Atlanta, Georgia.
This publication was made possible by grants from the National Institutes of Diabetes and Digestive and Kidney Diseases (K23-DK093584, K24-DK085153, K24-DK085446, and R01-DK092232), the National Center for Research Resources (UL1-TR000002), and the National Center for Advancing Translational Sciences (UL1-TR000153), as well as a research grant from Dialysis Clinic Inc. The funding sources were not involved in design and conduct of the study, the collection and management of the data, data analysis, interpretation of the data, preparation, review, or approval of the manuscript. The interpretation and reporting of the data presented here are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.04200413/-/DCSupplemental.
See related editorial, “Do Health Outcomes Vary by Profit Status of Hemodialysis Units?,” on pages 1–2.
References
- 1.Rosenau PV, Linder SH: Two decades of research comparing for-profit and nonprofit health provider performance in the United States. Soc Sci Q 84: 219–241, 2003 [Google Scholar]
- 2.Medical Payment Advisory Commission (MedPAC): Outpatient Dialysis Services. Report to the Congress: Medicare Payment Policy, Washington, DC, MedPAC, 2012
- 3.Devereaux PJ, Schünemann HJ, Ravindran N, Bhandari M, Garg AX, Choi PT, Grant BJ, Haines T, Lacchetti C, Weaver B, Lavis JN, Cook DJ, Haslam DR, Sullivan T, Guyatt GH: Comparison of mortality between private for-profit and private not-for-profit hemodialysis centers: A systematic review and meta-analysis. JAMA 288: 2449–2457, 2002 [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Cotter DJ, Thamer M: The effect of dialysis chains on mortality among patients receiving hemodialysis. Health Serv Res 46: 747–767, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Renal Data System : USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012 [Google Scholar]
- 6.Lee DK, Chertow GM, Zenios SA: Reexploring differences among for-profit and nonprofit dialysis providers. Health Serv Res 45: 633–646, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garg PP, Frick KD, Diener-West M, Powe NR: Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med 341: 1653–1660, 1999 [DOI] [PubMed] [Google Scholar]
- 8.United States Renal Data System : Researcher's Guide to the USRDS Database, 2011 ADR Edition, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease, 2011 [Google Scholar]
- 9.National Kidney Foundation: Part 5. Evaluation of laboratory measurements for clinical assessment of kidney disease. Am J Kidney Dis 39: S76–S110, 2002
- 10.Brooks JM, Irwin CP, Hunsicker LG, Flanigan MJ, Chrischilles EA, Pendergast JF: Effect of dialysis center profit-status on patient survival: a comparison of risk-adjustment and instrumental variable approaches. Health Serv Res 41: 2267–2289, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Foley RN, Fan Q, Liu J, Gilbertson DT, Weinhandl ED, Chen SC, Collins AJ: Comparative mortality of hemodialysis patients at for-profit and not-for-profit dialysis facilities in the United States, 1998 to 2003: A retrospective analysis. BMC Nephrol 9: 6, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thamer M, Zhang Y, Kaufman J, Cotter D, Dong F, Hernán MA: Dialysis facility ownership and epoetin dosing in patients receiving hemodialysis. JAMA 297: 1667–1674, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Griffiths RI, Powe NR, Gaskin DJ, Anderson GF, de Lissovoy GV, Whelton PK: The production of dialysis by for-profit versus not-for-profit freestanding renal dialysis facilities. Health Serv Res 29: 473–487, 1994 [PMC free article] [PubMed] [Google Scholar]
- 14.Held PJ, Levin NW, Bovbjerg RR, Pauly MV, Diamond LH: Mortality and duration of hemodialysis treatment. JAMA 265: 871–875, 1991 [PubMed] [Google Scholar]
- 15.Parker TF, 3rd, Hakim R, Nissenson AR, Krishnan M, Bond TC, Chan K, Maddux FW, Glassock R: A quality initiative. Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrol News Issues 27: 30–32, 34–36, 2013 [PubMed] [Google Scholar]
- 16.Wingard RL, Chan KE, Lazarus JM, Hakim RM: The “right” of passage: Surviving the first year of dialysis. Clin J Am Soc Nephrol 4[Suppl 1]: S114–S120, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Parker T, 3rd, Hakim R, Nissenson AR, Steinman T, Glassock RJ: Dialysis at a crossroads: 50 years later. Clin J Am Soc Nephrol 6: 457–461, 2011 [DOI] [PubMed] [Google Scholar]
- 18.Parker TF, 3rd, Straube BM, Nissenson A, Hakim RM, Steinman TI, Glassock RJ: Dialysis at a crossroads—Part II: A call for action. Clin J Am Soc Nephrol 7: 1026–1032, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.