Abstract
Herein we report that infection of a murine macrophage cell line with Bacillus anthracis results in the production of tumor necrosis factor alpha and interleukin-12 (IL-12). When infected with B. anthracis spores in combination with lipopolysaccharide, macrophages release increased amounts of IL-12. We found no evidence of inhibition of cytokine responses in macrophages infected with B. anthracis spores.
Anthrax is a zoonotic disease caused by infection of the mammalian host with Bacillus anthracis, a gram-positive, aerobic, spore-forming, rod-shaped bacterium (17; for reviews, see references 22 and 26). Anthrax is acquired when spores enter the host via the cutaneous, gastrointestinal, or inhalational routes. Inhalational anthrax, a rare event, rapidly leads to a highly lethal systemic infection (2, 7, 8, 16, 19, 27). B. anthracis carries two plasmids required for full virulence: pXO1, which encodes the components that combine to form the lethal and edema toxins (lethal factor, edema factor, and protective antigen), and pXO2, which carries the genes necessary for the expression of an antiphagocytic capsule (for reviews, see references 6 and 18).
The macrophage is thought to play a pivotal role in the early steps of anthrax pathogenesis. In inhalational anthrax, spores are phagocytosed by alveolar macrophages (3, 9, 11, 24, 25), which subsequently transport the spores to the regional lymph nodes. Spores germinate and multiply within the macrophages, eventually resulting in lysis of the macrophage (3, 9-11, 14). Vegetative cells multiply within the mediastinal lymph node and gain entry into the bloodstream (20, 24).
Hanna et al. demonstrated that the macrophage is essential to lethal toxin (LeTx) toxicity in vivo (12). When mice were depleted of macrophages by silica treatment, they became insensitive to LeTx. Hanna and colleagues showed at a cellular level that sublytic levels of LeTx trigger the production of tumor necrosis factor alpha (TNF-α) and interleukin-1β (IL-1β) by the macrophage cell line RAW 264.7 and that anti-IL-1 antibody or an IL-1 antagonist protected mice from toxin lethality. Subsequent publications have described studies that have contradicted this finding, reporting that purified LeTx inhibits cytokine responses to lipopolysaccharide (LPS) and postulating that this activity may play a role in the early stages of infection by dampening the immune response and permitting early replication (1, 4, 15, 21, 23).
In this study, we present the first report of the cytokine response to infection of a murine macrophage cell line with purified B. anthracis spores. We examined the responses of 10 cytokines (TNF-α, IL-6, IL-1β, granulocyte-macrophage colony-stimulating factor, IL-2, IL-4, IL-5, IL-10, IL-12, and gamma interferon [IFN-γ]) to infection of macrophages with two strains of B. anthracis. The B. anthracis 7702 strain carries the pXO1 plasmid but not the pXO2 plasmid, and therefore this strain produces LeTx but not a capsule. The B. anthracis 9131 strain carries neither the pXO1 nor the pXO2 plasmid and is therefore lacking both the LeTx and the capsule. We selected J774A.1 cells as an example of a LeTx-sensitive cell line (13). J774A.1 macrophages were maintained in high-glucose Dulbecco minimal essential medium containing 10% fetal calf serum, l-glutamine, and phenol red at 5% CO2. Spores were prepared by the method described by Finlay et al. (5). Spore preparations were heat treated at 65°C for 30 min to kill any remaining vegetative cells. Spore material was purified by centrifugation through Renografin (Renocal-76; Bracco Diagnostics, Princeton, N.J.). The purified spore pellet was washed once with cold distilled water and stored at 4°C. A viability count was performed on the spore preparation, and the preparation was adjusted to 109 CFU/ml. Modified Ziehl-Neelsen staining revealed that the preparations contained 100% spores.
Macrophages were seeded at 106/ml and were allowed to attach to 24-well plates for 2 h prior to infection. Monolayers were infected at a multiplicity of infection of 1:1 and were incubated for 30 min at 37°C. Gentamicin (10 μg/ml) was added to remove extracellular B. anthracis. After an additional 30-min incubation, monolayers were washed, and fresh complete medium (without antibiotics) was added. For all experiments, this was considered to be the zero time point. For cytokine determinations, J774A.1 cells were cultured in phenol-red-free and high-glucose Dulbecco minimal essential medium containing 10% serum and l-glutamine. For cultures that were treated with LPS, Escherichia coli O111:B4 LPS (1 μg/ml; Sigma Chemical Co.) was added to the cell monolayers at the zero time point. Samples of supernatant were taken at 2.5, 5, and 7.5 h postinfection. Aliquots were stored at −70°C until analysis was performed. Cytokine concentrations in culture supernatants were measured with a mouse cytokine Ten-Plex antibody bead kit (Biosource International, Camarillo, Calif.) and a Luminex model 100 analyzer (Luminex Corporation, Austin, Tex.).
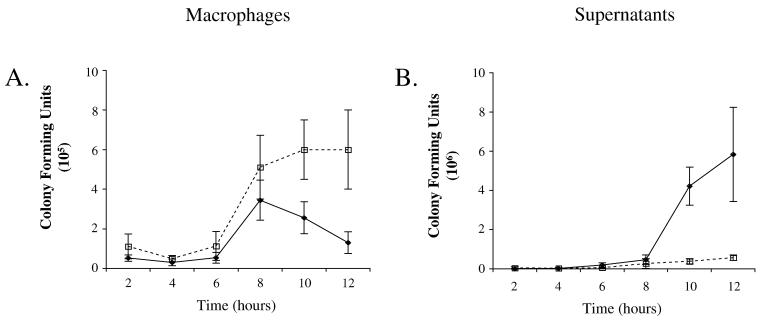
Initial experiments were performed to study the growth of B. anthracis within J774A.1 macrophages. Measurements were made by counting viable B. anthracis organisms in macrophages and supernatant samples at 2, 4, 6, 8, 10, and 12 h postinfection (Fig. 1). After an initial lag phase of approximately 4 h, B. anthracis strain 7702 multiplies within J774A.1 macrophages until 8 to 10 h postinfection, at which time the cells lyse, releasing B. anthracis into the supernatant. In contrast, after the initial lag phase, B. anthracis strain 9131 multiplies within the macrophage but fails to cause cell lysis. The termination time of cytokine experiments at 7.5 h was therefore chosen to measure cytokine release prior to cell lysis. These experiments confirmed the sensitivity of the J774A.1 cell line to lysis after infection with a pXO1+ strain of B. anthracis.
FIG. 1.
Growth of B. anthracis strains 7702 and 9131 in J774 macrophages. Macrophages were infected with B. anthracis spores prepared from B. anthracis strain 7702 (filled diamonds) and B. anthracis strain 9131 (open squares), as described in the text. CFU were determined and are shown as a function of time postinfection. At each time point, the numbers of CFU present inside the macrophages (A) and in the supernatant (B) were determined. Four experiments were performed, and the results of a representative experiment are shown. Each value reported is the average for three samples ± the standard deviation.
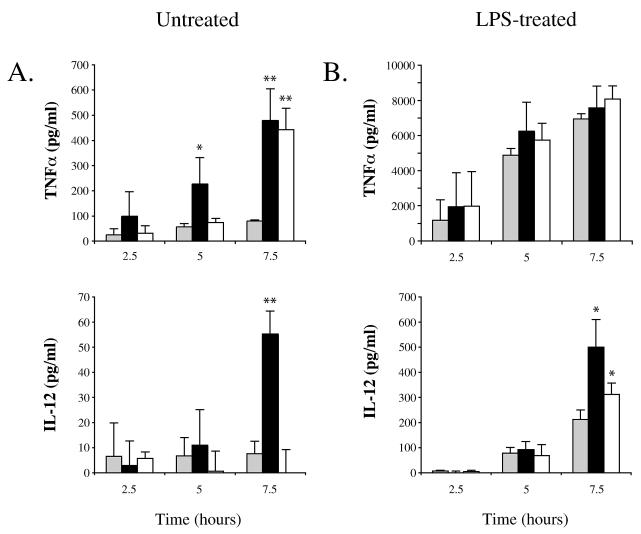
When macrophages were infected with purified B. anthracis spores alone, TNF-α was released as early as 5 h following infection, and its level continued to increase up to 7.5 h postinfection (Fig. 2A). The pXO1+ strain caused an earlier release of higher levels of TNF-α than the pXO1− strain did. No other cytokines were induced upon infection of macrophages by B. anthracis spores alone (Table 1) with the exception of IL-12, which increased significantly between 5 and 7.5 h postinfection with spores from strain 7702 (Fig. 2A).
FIG. 2.
Release of selected cytokines by macrophages in response to infection by B. anthracis strains 7702 and 9131. (A) Macrophages were left untreated (gray bars) or infected with B. anthracis spores prepared from B. anthracis strain 7702 (black bars) or B. anthracis strain 9131 (white bars), as described in the text. (B) Macrophages were treated with LPS alone (gray bars) or in combination with infection with B. anthracis spores prepared from B. anthracis strain 7702 (black bars) or B. anthracis strain 9131 (white bars), as described in the text. In all cases, cytokine concentrations were determined at the indicated time points. Four experiments were performed, and the results of a representative experiment are shown. Each value reported is the average for three samples ± the standard deviation. Statistical significance was determined using Student's t test analysis. In all cases, means were compared to those of the uninfected control groups. *, P < 0.05; **, P < 0.01.
TABLE 1.
Expression of cytokines by B. anthracis-infected macrophages
| Cytokineb | Concn (pg/ml) after indicated treatmenta
|
|||||
|---|---|---|---|---|---|---|
| None | 7702 infection | 9131 infection | LPS | LPS + 7702 infection | LPS + 9131 infection | |
| IL-6 | 49 ± 34 | 28 ± 55 | 6 ± 26 | 5,380 ± 750 | 7,152 ± 1,703 | 8,178 ± 1,828 |
| IL-10 | 14 ± 7 | 1 ± 4 | 2 ± 1 | 82 ± 10 | 93 ± 17 | 84 ± 16 |
| IL-1β | 18 ± 15 | 4 ± 35 | 1 ± 30 | 119 ± 26 | 114 ± 16 | 128 ± 13 |
| GM-CSF | 72 ± 37 | 64 ± 34 | 60 ± 22 | 97 ± 32 | 110 ± 21 | 91 ± 13 |
Macrophages were infected with B. anthracis spores with and without LPS-treatment, as described in the text. Cytokine concentrations are reported for each treatment group at 7.5 h postinfection. Four experiments with infections were performed, and the results of a representative experiment are presented. Each reported value represents the average for three samples ± 1 standard deviation.
The limit of detection of the assay for IL-6, IL-1β, and granulocyte-macrophage colony-stimulating factor (GM-CSF) was 10 pg/ml, and that for IL-10 was 15 pg/ml.
We observed the expected strong induction of TNF-α and IL-6 and the induction of IL-1β, IL-10, and IL-12 in response to the addition of LPS alone (Fig. 2B and Table 1). Our results indicate that the IL-12 response to LPS treatment was enhanced in B. anthracis-infected cells relative to uninfected cells (Fig. 2B and Table 1). Under all conditions studied, the cytokines IFN-γ, IL-2, IL-4, and IL-5 were produced at levels at or below the detection limit of the assay (data not shown). In contrast to previously reported results with purified LeTx (1, 4, 15, 21, 23), we found no evidence of an inhibitory effect on cytokine production by the macrophages in response to infection with spores from B. anthracis strain 7702 or 9131. LeTx-expressing strain 7702 caused a more rapid TNF-α response than did strain 9131. In addition, cells infected with spores from strain 7702 produced a small amount of IL-12, while cells infected with spores from the LeTx-deficient strain 9131 produced none. The absence of an IL-12 response to infection with strain 9131 spores may indicate that a factor encoded by plasmid pXO1 mediates IL-12 stimulation, either directly or through a regulatory pathway.
In this study, we present results indicating that a live infection of a mouse macrophage cell line with B. anthracis spores triggers TNF-α and IL-12 responses and enhances the LPS-induced production of IL-12. The stimulation of proinflammatory cytokines such as TNF-α is an important step in the activation of inflammatory pathways such as cellular recruitment, adhesion, and coagulation. The production of IL-12 may direct the immune system toward a cell-mediated helper T-cell response.
Previous reports indicated that purified LeTx inhibits cytokine production in macrophages (1, 4, 15, 21, 13). In those studies, the authors suggested that the observed LeTx inhibitory activity may be relevant during the early stages of infection. However, we observed no inhibition of cytokine induction upon infection of macrophages with spores capable of expressing LeTx. The infection of macrophages by B. anthracis spores results in the expression of multiple factors by the bacterium. The expression of a combination of regulatory pathways, activating cell surface protein factors, and toxic mediators, as well as the mechanical effects of a large intracellular population of expanding vegetative cells, may effect an influence on macrophage signaling, cytokine release, and the production of bactericidal oxygen and nitrogen radicals. Our results indicate either that LeTx is not produced at sufficient levels during the initial infection of macrophages to exert an inhibitory effect on cytokine production or that the inhibitory effect is not sufficient to overcome the stimulatory effects of a replicating intracellular pathogen.
The macrophage is thought to play a central role in the progression of anthrax from a local infection to a systemic disease. This model predicts that the macrophage carries anthrax spores from the site of infection to the regional lymph nodes, where the bacterial population expands and enters the bloodstream (9, 11, 24, 25). If this model is correct, the ability of B. anthracis to transit through the macrophage is critical to its ability to cause systemic disease. A detailed analysis of the interaction between the macrophage and the pathogen is essential to our understanding of the progression of B. anthracis infection. The results of this study provide insight into the effects of B. anthracis infection of the macrophage on the host's immune response. The results reported herein indicate that during the early stages of infection, the production of cytokines by macrophages is not inhibited by the intracellular B. anthracis spores. On the contrary, our results suggest that the host is stimulated to mount a proinflammatory response and is primed to mount a cell-mediated response towards what is, at this early stage of the infection, an intracellular pathogen.
Acknowledgments
We thank Karen Elkins, Manuel Osorio, and Gopa Raychaudhuri for their critical reading of the manuscript.
Editor: J. T. Barbieri
REFERENCES
- 1.Agrawal, A., J. Lingappa, S. H. Leppla, S. Agrawal, A. Jabbar, C. Quinn, and B. Pulendran. 2003. Impairment of dendritic cells and adaptive immunity by anthrax lethal toxin. Nature 424:329-334. [DOI] [PubMed] [Google Scholar]
- 2.Barnes, J. M. 1947. The development of anthrax following administration of spores by inhalation. Br. J. Exp. Pathol. 28:385-394. [Google Scholar]
- 3.Dixon, T. C., A. A. Fadl, T. M. Koehler, J. A. Swanson, and P. C. Hanna. 2000. Early Bacillus anthracis-macrophage interactions: intracellular survival and escape. Cell Microbiol. 2:453-463. [DOI] [PubMed] [Google Scholar]
- 4.Erwin, J. L., L. M. DaSilva, S. Bavari, S. F. Little, A. M. Friedlander, and T. C. Chanh. 2001. Macrophage-derived cell lines do not express proinflammatory cytokines after exposure to Bacillus anthracis lethal toxin. Infect. Immun. 69:1175-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finlay, W. J. J., N. A. Logan, and A. D. Sutherland. 2002. Bacillus cereus emetic toxin production in cooked rice. Food Microbiol. 19:431-439. [Google Scholar]
- 6.Fouet, A., and S. Mesnage. 2002. Bacillus anthracis cell envelope components. Curr. Top. Microbiol. Immunol. 271:87-113. [DOI] [PubMed] [Google Scholar]
- 7.Friedlander, A. M., S. L. Welkos, M. L. M. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, P. Mikesell, and W. B. Lawrence. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239-1243. [DOI] [PubMed] [Google Scholar]
- 8.Fritz, D. L., N. K. Jaax, W. B. Lawrence, K. J. Davis, M. L. M. Pitt, J. Ezzell, and A. Friedlander. 1995. Pathology of experimental inhalation anthrax in the rhesus monkey. Lab. Investig. 73:691-702. [PubMed] [Google Scholar]
- 9.Guidi-Rontani, C., M. Levy, H. Ohayon, and M. Mock. 2002. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol. Microbiol. 42:931-938. [DOI] [PubMed] [Google Scholar]
- 10.Guidi-Rontani, C., Y. Pereira, S. Ruffie, J. C. Sirard, M. Weber-Levy, and M. Mock. 1999. Identification and characterization of a germination operon on the virulence plasmid pXO1 of Bacillus anthracis. Mol. Microbiol. 33:407-414. [DOI] [PubMed] [Google Scholar]
- 11.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 12.Hanna, P. C., D. Acosta, and R. J. Collier. 1993. On the role of macrophages in anthrax. Proc. Natl. Acad. Sci. USA 90:10198-10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanna, P. C., S. Kochi, and R. J. Collier. 1992. Biochemical and physiological changes induced by anthrax lethal toxin in J774 macrophage-like cells. Mol. Biol. Cell 3:1269-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ireland, J. A. W., and P. C. Hanna. 2002. Macrophage-enhanced germination of Bacillus anthracis endospores requires gerS. Infect. Immun. 70:5870-5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalns, J., J. Scruggs, N. Millenbaugh, J. Vivekananda, D. Shealy, J. Eggers, and J. Kiel. 2002. TNF receptor 1, IL-1 receptor, and iNOS genetic knockout mice are not protected from anthrax infection. Biochem. Biophys. Res. Commun. 292:41-44. [DOI] [PubMed] [Google Scholar]
- 16.Klein, F., J. S. Walker, D. F. Fitzpatrick, R. E. Lincoln, B. G. Mahlandt, W. I. J. Jones, J. P. Dobbs, and K. J. Hendrix. 1966. Pathophysiology of anthrax. J. Infect. Dis. 116:123-138. [DOI] [PubMed] [Google Scholar]
- 17.Koch, R. 1876. Die Etiologie der Milzbrand Krankheit gegrundet auf die Entwickelungsgeschichte des Bacillus anthracis. Beitr. Biol. Pflanz. 2:277-283. [Google Scholar]
- 18.Lacy, D. B., and R. J. Collier. 2002. Structure and function of anthrax toxin. Curr. Top. Microbiol. Immunol. 271:61-85. [DOI] [PubMed] [Google Scholar]
- 19.LaForce, F. M., F. H. Bumford, J. C. Feeley, S. L. Stokes, and D. B. Snow. 1969. Epidemiologic study of a fatal case of inhalation anthrax. Arch. Environ. Health. 18:798-805. [DOI] [PubMed] [Google Scholar]
- 20.Lincoln, R. E., D. R. Hodges, F. Klein, B. G. Mahlandt, W. I. Jones, Jr., B. W. Haines, M. A. Rhian, and J. S. Walker. 1965. Role of lymphatics in the pathogenesis of anthrax. J. Infect. Dis. 115:481-494. [DOI] [PubMed] [Google Scholar]
- 21.Moayeri, M., D. Haines, H. A. Young, and S. H. Leppla. 2003. Bacillus anthracis lethal toxin induces TNF-alpha-independent hypoxia-mediated toxicity in mice. J. Clin. Investig. 112:670-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 23.Pellizzari, R., C. Guidi-Rontani, G. Vitale, M. Mock, and C. Montecucco. 1999. Anthrax lethal factor cleaves MKK3 in macrophages and inhibits the LPS/IFNgamma-induced release of NO and TNFalpha. FEBS Lett. 462:199-204. [DOI] [PubMed] [Google Scholar]
- 24.Ross, J. M. 1957. The pathogenesis of anthrax following the administration of spores by the respiratory route. J. Pathol. Bacteriol. 73:485-494. [Google Scholar]
- 25.Shafa, F., B. J. Moberly, and P. Gerhardt. 1966. Cytological features of anthrax spores phagocytized in vitro by rabbit alveolar macrophages. J. Infect. Dis. 116:401-413. [DOI] [PubMed] [Google Scholar]
- 26.Turnbull, P. C. 2002. Introduction: anthrax history, disease and ecology. Curr. Top. Microbiol. Immunol. 271:1-19. [DOI] [PubMed] [Google Scholar]
- 27.Zaucha, G. M., L. M. Pitt, J. Estep, B. E. Ivins, and A. Friedlander. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch. Pathol. Lab. Med. 122:982-992. [PubMed] [Google Scholar]