Abstract
Purpose:
High-Performance System (HPS) laser photo vaporization of the prostate (PVP) is a widely used procedure nowadays. The safety and efficacy of the procedure has been affirmed in general patients with benign prostatic hyperplasia (BPH), but data on the safety and efficacy in specific situations, such as in patients with a large prostate, patients taking anticoagulant or 5-alpha reductase inhibitor (5-ARI) medication, and patients with a history of acute urinary retention (AUR) or previous transurethral resection of the prostate (TURP), is lacking. We investigated the safety and efficacy of HPS laser PVP in these unique patient groups.
Methods:
The study was conducted from March 2009 to February 2012 among patients for lower urinary tract symptoms. Patients in whom BPH was diagnosed and who were treated with 120-W HPS GreenLight PVP were selected. Patients were divided into groups of prostate size above and below 80, anticoagulant medication, 5-ARI medication, AUR history, and TURP history on the basis of the preoperative history and physical examination.
Results:
A total of 533 patients observable for a follow-up period of more than 6 months were enrolled as the study population. The patients’ mean preoperative prostate size was 51.0±32.7 mL and their mean prostate-specific antigen was 4.5±27.9 ng/mL. The average operating time was 24.5±12.2 minutes and the average applied energy during surgery was 152,184±89,495 J. Postoperative objective and subjective parameters in all groups were significantly improved compared with preoperative values.
Conclusions:
Laser resection of the prostate is safe and effective. The results of HPS laser PVP were not influenced by prostate size, the use of anticoagulants, the intake of 5-ARI for BPH management, a history of AUR, a history of TURP, or other factors. Thus, this study was able to reconfirm the efficacy and safety of laser resection of the prostate.
Keywords: Lasers, Prostatic hyperplasia, Anticoagulants, 5-Alpha reductase inhibitors, Retention, Transurethral resection of prostate
INTRODUCTION
Benign prostatic hyperplasia (BPH) is a disease exhibiting one of the fastest surging incidences because the elderly population is rapidly growing [1]. The complications of BPH, including urinary retention, urinary infection, reduced renal function, and indwelling urinary catheter, eventually lead to reduced social activities in particular [2]. These problems brought a rapid increase in social expenses from 4 billion to 26 billion dollars annually, a trend that is continuously increasing at the moment [3]. This fact implies that medical costs could be saved to a great extent if BPH were properly managed in our society.
Various treatment methods have been introduced and implemented from medications regulating BPH symptoms to medications reducing the size of the prostate to surgical methods of removing the enlarged part of the prostate. Transurethral resection of the prostate (TURP) is the gold standard for surgically removing the enlarged part of the prostate. Nowadays, however, laser surgical procedures are frequently used.
After the first laser resection of the prostate was implemented, the efficacy and safety of the procedure were reported in numerous studies. Among the currently reported laser surgical methods, the efficacy and safety of High-Performance System (HPS) laser therapy, in particular, have been verified through many studies. However, most previous studies comprised ordinary BPH patients. Hence, studies on rare cases that could be encountered in the actual clinical field are still inadequate in number. The results of 120-W HPS laser photo vaporization of the prostate (PVP) are vague in cases with larger sized prostates, the use of anticoagulants, the intake of 5-alpha reductase inhibitor (5-ARI) for prostate enlargement regulation, a history of acute urinary retention (AUR) owing to preoperative prostate enlargement, and a medical record of BPH-related surgery. The authors of this study intended to investigate the postoperative progress of patients who were observable for a follow-up period of more than 6 months and who fell under the above conditions owing to our performance of more than 500 HPS laser surgeries over the last 3 years.
MATERIALS AND METHODS
1. Study population
The study was conducted from March 2009 to February 2012 among patients who visited a Urology Clinic for lower urinary tract symptoms (LUTS). Patients in whom BPH was diagnosed and who were treated with 120-W HPS GreenLight PVP were selected. Operative indications were based the American Urological Association and European Urological Association guidelines on BPH, maximum urinary flow (Qmax) <15 mL/sec, postvoiding residual volume (PVR) >100 mL, and International Prostate Symptom Score (IPSS) >7. Also, symptom persistence despite proper management, avoidance of proper medication, severe bladder outlet obstruction (BOO) revealed by urodynamic study, bladder stones, recurrent urinary tract infections, and persistent hematuria from the prostate were added as operative indications.
Patients were divided into groups of prostate size above and below 80, anticoagulant medication none/yes, 5-ARI medication none/yes, AUR history none/yes, and TURP history none/yes on the basis of the preoperative history and physical examination results.
This study was conducted under Seoul St. Mary’s Hospital Institutional Review Board (IRB) approval. The IRB approval number is KC12RISI0800.
2. Operative technique
After general or spinal anesthesia, the operation was done by a single surgeon. A continuous running irrigation system with a 22-Fr resectoscope with a 30-degree lens and a 75-degree laser fiber was used. Normal saline (0.9%) was used for irrigation. The 120-W HPS GreenLight laser PVP was done at a 1-mm distance from the prostate tissue for optimal vaporization effect. Vaporization was initiated at the bladder neck in a clockwise direction, pulling the resectoscope out and rotating the laser fiber simultaneously. An 18-Fr urethral catheter was placed after the operation and removed the next day, taking into consideration the degree of hematuria.
3. Follow-up
The patients visited the outpatient clinic 1, 3, 6, 9, and 12 months after the operation. At every visit, the patients completed IPSS questionnaires and Qmax and PVR were checked. In addition, the presence of postoperative complications was verified at every follow-up visit.
4. Statistical analysis
A Student t-test was used to compare the preoperative intergroup differences and repeated-measures analysis of variance (ANOVA) was used to compare the preoperative and postoperative values. P-values of less than 0.05 were defined as statistically significant.
RESULTS
A total of 533 patients observable for a follow-up period of more than 6 months were enrolled as the study population. The mean age of the subjects was 70.8±8.1 years. Their mean preoperative prostate size was 51.0±32.7 mL, and their mean prostate-specific antigen (PSA) concentration was 4.5±27.9 ng/mL. Concerning significant medical history, 5 cases of 120-W HPS laser PVP were performed owing to severe dysuria after a patient was diagnosed with prostate cancer.
The average operating time was 24.5±12.2 minutes and the average applied energy during surgery was 152,184±89,495 J. The average catheterization time was 1.39±3.48 days.
Significant differences were observed in prostate size, PSA, Qmax, and PVR in the groups formed according to preoperative prostate size. However, no significant differences were found except for age in the comparison of the use of anticoagulant medication. A significant difference was shown for PSA only in the comparison of the use of 5-ARI medication. According to the comparison of AUR history, significant differences were identified in age, transrectal ultrasound, PSA, and PVR. Moreover, significant differences were detected in age and PVR in the comparison of previous history of TURP (Table 1).
Table 1.
Preoperative demographic data of each group
| Variable | No. | Age (yr) | TRUS | PSA (ng/mL) | IPSS total | IPSS voiding | IPSS storage | IPSS QoL | Qmax (mL/sec) | PVR (mL) |
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 533 | 70.8±8.1 | 51.0±32.7 | 4.5±27.9 | 21.0±8.0 | 12.3±5.3 | 8.5±3.8 | 4.1±1.2 | 9.1±22.2 | 119.8±194.2 |
| Prostate size | ||||||||||
| Under 80 | 458 | 70.5±8.1a) | 43.5±14.8a) | 3.6±20.7a) | 20.9±7.9 | 12.3±5.3 | 8.5±3.8 | 4.1±1.1 | 9.6±23.8a) | 115.4±199.2a) |
| Over 80 | 75 | 73.2±8.0 | 111.1±62.5 | 25.1±59.9 | 21.1±7.8 | 12.6±5.4 | 8.5±3.5 | 3.8±1.6 | 5.5±5.8 | 154.6±163.6 |
| Anticoagulant | ||||||||||
| None | 411 | 70.3±8.3a) | 50.2±34.2 | 4.9±30.7 | 21.1±7.8 | 12.5±5.1 | 8.5±3.8 | 4.2±1.1 | 9.1±22.0 | 113.2±164.8 |
| Yes | 122 | 72.4±7.5 | 53.3±27.3 | 3.9±14.9 | 20.4±8.6 | 11.7±5.9 | 8.5±3.6 | 3.9±1.4 | 9.1±22.8 | 139.5±263.3 |
| 5-ARI medication | ||||||||||
| None | 512 | 70.7±8.1 | 51.0±33.0 | 9.7±28.4a) | 21.0±8.1 | 12.3±5.3 | 8.5±3.8 | 4.1±1.2 | 9.2±22.7 | 120.1±196.1 |
| Yes | 21 | 73.1±7.9 | 50.4±25.3 | 3.5±4.1 | 20.8±6.3 | 12.4±5.2 | 8.1±3.4 | 3.5±1.2 | 7.6±5.6 | 115.0±154.7 |
| AUR Hx | ||||||||||
| None | 432 | 70.3±7.8a) | 48.4±23.4a) | 3.8±26.2a) | 20.9±8.0 | 12.2±5.2 | 8.5±3.8 | 4.1±1.1 | 9.9±24.3 | 106.3±184.9a) |
| Yes | 101 | 72.2±9.3 | 62.4±57.0 | 16.5±33.4 | 21.5±8.2 | 12.9±5.9 | 8.5±3.8 | 4.2±1.4 | 5.5±5.5 | 180.0±222.5 |
| TURP Hx | ||||||||||
| None | 488 | 70.6±8.2a) | 51.6±33.5 | 3.4±27.5 | 20.8±8.1 | 12.3±5.3 | 8.4±3.8 | 4.1±1.1 | 8.6±19.8 | 123.9±200.1a) |
| Yes | 47 | 73.2±7.0 | 43.7±20.6 | 4.1±32.4 | 22.3±7.5 | 12.9±5.5 | 9.2±3.6 | 4.3±1.15 | 15.5±41.7 | 68.4±76.5 |
Values are presented as mean±standard deviation.
TRUS, transrectal ultrasonography of prostate; PSA, prostate-specific antigen; IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum urinary flow; PVR, post-voided residual urine; 5-ARI, 5-alpha reductase inhibitor; AUR, acute urinary retention; Hx, history ; TURP, transurethral resection of the prostate.
P<0.05 compared with intragroup comparison.
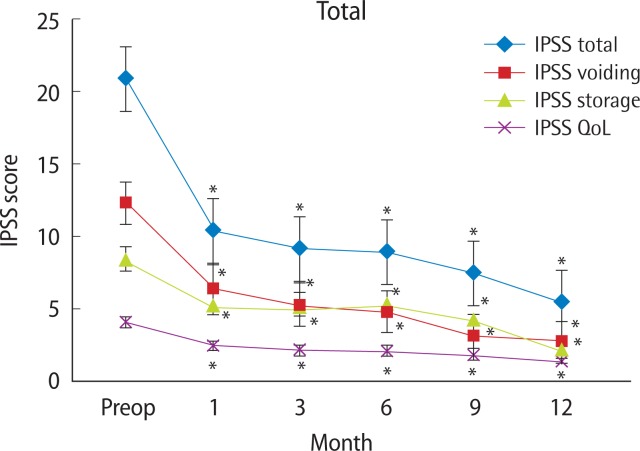
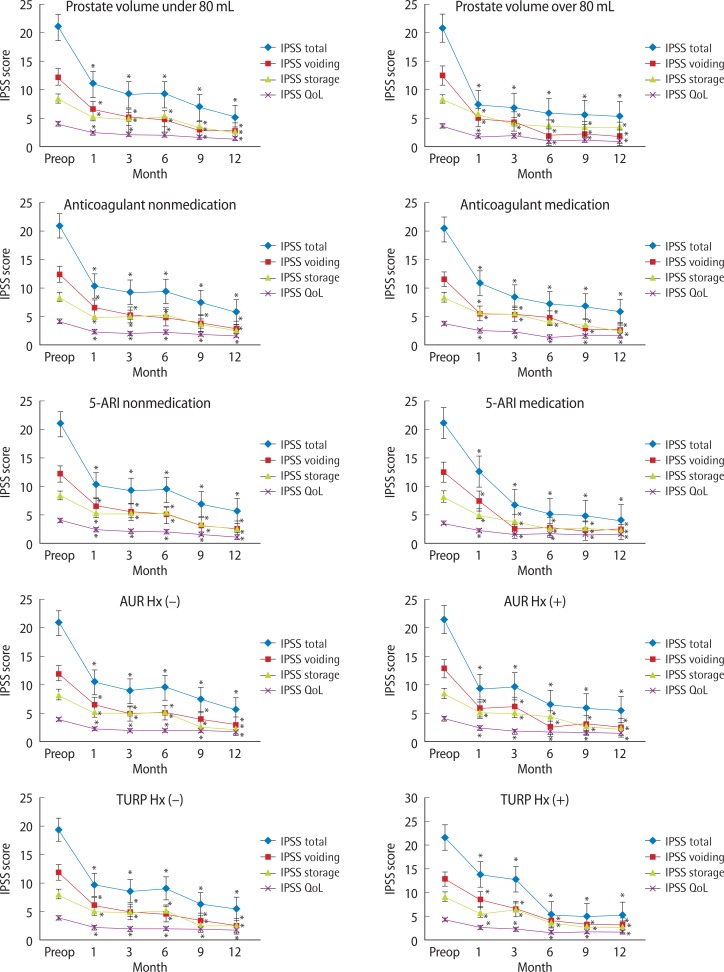
The results of the IPSS questionnaire completed by all patients at postoperative months 1, 3, 6, 9, and 12 are shown in Fig. 1. A significant difference from preoperative values was observed in the IPSS questionnaire during the follow-up period (P<0.05 compared with preoperative value). Moreover, the results of the IPSS questionnaire conducted on each group at postoperative months 1, 3, 6, 9, and 12 are shown in Fig. 2.
Fig. 1.
Changes in International Prostate Symptom Score (IPSS) after 120-W GreenLight High-Performance System laser photo vaporization of the prostate in the total group of patients. QoL, quality of life. *P<0.05 compared with preoperative (Preop) value.
Fig. 2.
Changes in International Prostate Symptom Score (IPSS) after 120-W GreenLight High-Performance System laser photo vaporization of the prostate in each group. QoL, quality of life; 5-ARI, 5-alpha reductase inhibitor; AUR, acute urinary retention; Hx, history; TURP, transurethral resection of the prostate. *P<0.05 compared with preoperative (Preop) value.
IPSSs decreased compared with preoperative values in all groups (P<0.05). Moreover, an increase in postoperative Qmax and a decrease in postoperative PVR were observed. The results of the repeated-measures ANOVA are shown in Table 2. Most postoperative IPSS, Qmax, and PVR values were found to be changed. However, no significant change was observed in postoperative PVR scores in the group who had undergone TURP before. Discriminating variables were insignificant in most cases in the subgroup analysis. However, a difference was identified in quality of life (QoL) in case of prostate volume above or below 80. A difference was found in the IPSS total score in the case of a presence of AUR history. Furthermore, a lack of significant difference was confirmed in the results verified by time-adjusted P-value.
Table 2.
The results of repeated-measures analysis of variance comparing the difference in preoperative and postoperative parameters in each group
| Variable | IPSS total | IPSS voiding | IPSS storage | IPSS QoL | Qmax | PVR |
|---|---|---|---|---|---|---|
| Prostate size 80 | ||||||
| P-value | 0.014a) | 0.001a) | 0.001a) | 0.001a) | 0.002a) | 0.024a) |
| Intergroup comparison | 0.851 | 0.506 | 0.230 | 0.045a) | 0.770 | 0.991 |
| Adjusted P-value | 0.487 | 0.553 | 0.391 | 0.747 | 0.506 | 0.854 |
| Anticoagulant medication | ||||||
| P-value | 0.001a) | 0.03a) | 0.015a) | 0.001a) | 0.001a) | 0.001a) |
| Intergroup comparison | 0.271 | 0.866 | 0.988 | 0.755 | 0.698 | 0.240 |
| Adjusted P-value | 0.862 | 0.431 | 0.665 | 0.691 | 0.936 | 0.067 |
| 5-ARI medication Hx | ||||||
| P-value | 0.003a) | 0.006a) | 0.001a) | 0.021a) | 0.009a) | 0.03a) |
| Intergroup comparison | 0.161 | 0.105 | 0.404 | 0.617 | 0.745 | 0.614 |
| Adjusted P-value | 0.696 | 0.762 | 0.104 | 0.103 | 0.687 | 0.758 |
| AUR Hx | ||||||
| P-value | 0.001a) | 0.001a) | 0.001a) | 0.001a) | 0.001a) | 0.001a) |
| Intergroup comparison | 0.003a) | 0.087 | 0.129 | 0.099 | 0.152 | 0.344 |
| Adjusted P-value | 0.576 | 0.621 | 0.847 | 0.389 | 0.336 | 0.570 |
| TURP Hx | ||||||
| P-value | 0.007a) | 0.037a) | 0.034a) | 0.001a) | 0.001a) | 0.620 |
| Intergroup comparison | 0.929 | 0.858 | 0.866 | 0.547 | 0.138 | 0.296 |
| Adjusted P-value | 0.098 | 0.429 | 0.547 | 0.299 | 0.311 | 0.929 |
IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum urinary flow; PVR, post-voided residual urine; 5-ARI, 5-alpha reductase inhibitor; Hx, history; AUR, acute urinary retention; TURP, transurethral resection of the prostate.
P<0.05 compared with preoperative value.
Bleeding requiring transfusion or suspension of surgery did not happen during the operation. Although some patients reported dysuria after surgery, most subjects were able to regain regular urinary function from the second urination because preoperative transrectal biopsy was simultaneously performed in patients with high PSA. During the follow-up period, no cases required reoperation due to worsened symptoms or gross hematuria. Although dysuria was observed in about 8% of the patients during the first postoperative month, the symptom disappeared after starting medication or observation in most cases. Retrograde ejaculation occurred in about 13% of patients.
DISCUSSION
BPH is one of the fastest-growing diseases in the elderly population [1]. The QoL in the elderly population has been underscored as the number of elderly people has increased along with prolonged life expectancy [4]. Voiding difficulty is a leading symptom that has a devastating effect on QoL in older people. Moreover, LUTS generated by BPH may result in mood disorders such as depression and can impair social relationships [2]. To relieve such BPH symptoms, medications are prescribed including alpha-blockers and 5-ARIs. However, medical treatment focuses on improving symptoms instead of resolving the main causes of BPH. Medical treatment may require long-term intake of medication, may result in the recurrence of symptoms upon the suspension of medication, and may take a long time to alleviate symptoms.
For the treatment of mechanical obstruction due to the enlarged prostate, surgical treatment is the fundamental method. Hence, TURP has been recommended as one of the standard choices [5]. However, TURP has the potential risk of operative site bleeding or delayed bleeding and requires a long postoperative hospitalization period. In addition, the occurrence of postoperative complications such as retrograde ejaculation has been pointed out [6–8]. To resolve such shortcomings, different surgical procedures and instruments have been devised. Among these, laser resection of the prostate has drawn attention recently. Laser resection of the prostate using the neodymium-doped:YAG (Nd:YAG) laser converts most of the energy into heat. However, this procedure performed in the early stages may require long bladder drainage and hospitalization periods; its shortcomings also include a higher risk of reoperation [9]. The 80-W potassium-titanyl-phosphate (KTP) laser introduced afterwards has a shorter wavelength than the Nd:YAG laser. Moreover, the laser is more favorable for removing prostate adenoma without bleeding during the TURP procedure owing to its photo-selectivity and high reactivity to heme protein [10]. However, the 80-W KTP laser has the shortcoming of a long operating time owing to insufficient output-generating capacity. The 120-W GreenLight laser used by the authors has a more powerful output generating capacity compared with the 80-W laser, which enables the removal of large amounts of tissue in a shorter time. Moreover, its postoperative efficacy has been verified by numerous studies [4].
Along with the advancement of laser resection of the prostate, surgical cases that were considered inoperable or extremely high-risk in the past have been attempted. One such case is the use of laser resection of the prostate in patients administered oral anticoagulants [11]. Patients take oral anticoagulants for various reasons. However, one of the most common and critical reasons is prevention of complications when a patient has cardiovascular and related diseases as the underlying disease [12]. The bleeding risk increases when surgery is performed on a patient currently taking oral anticoagulants. To conduct the TURP procedure, the administration of oral anticoagulants is generally suspended before surgery. Consequently, this has imposed burdens on surgeons with the higher risk of potential deep vein thrombosis and cardiovascular and related problems [13]. However, the 120-W GreenLight HPS laser PVP minimizes the potential risks during the operation owing to the laser’s unique characteristic of photo-selectivity. These findings were verified through the process of examining cases requiring postoperative transfusion or reoperation because of bleeding. Significant improvement was observed in terms of postoperative storage and voiding symptoms, Qmax, and PVR from preoperative values. The outcomes were verified to align with the results of previous studies. Therefore, the 120-W laser is thought to be safe and effective for patients taking oral anticoagulants as proven by this study and others.
Longer operating hours are required as the size of the prostate gets larger, which may eventually lead to increased morbidity as a result of the delayed operating time. In the HPS laser PVP procedure, the operating time may be longer than that for conventional TURP and the efficacy may be reduced. These limitations of the HPS laser PVP procedure have been pointed out in the case of larger prostate volumes [14,15]. However, no differences were found in patients’ subjective improvement in symptoms and improvement in objective urinary indicators excluding QoL, as seen in recent data and the present study results after the HPS laser PVP procedure [16]. However, the possibilities of an effect of prostate volume on QoL have to be taken into consideration, because the classification of patients according to prostate volume includes BPH and additionally diagnosed prostate cancer. The possible influence on the QoL cannot be excluded.
5-ARIs are commonly prescribed to reduce the prostate volume of patients diagnosed with an enlarged prostate in urology clinics, primary hospitals, and nonurology clinics or to improve preoperative LUTS. This medication is known to be effective in reducing an enlarged prostate volume and the likelihood of increased Qmax and the occurrence of AUR [17–19]. Regarding the effect of 5-ARIs on surgery utilizing conventional TURP, a study reported that there were no negative effects on preoperatively reduced prostate volume, risk of operative site bleeding, or postoperative observation during the follow-up period [20]. In addition, a similar study result was acquired during prostate resection with the 80-W KTP laser [21,22]. Significant improvement in symptoms was confirmed in the comparison of preoperative and postoperative values with the use of 120-W HPS laser PVP. The postoperative improvement in symptoms was not affected by the intake of a 5-ARI before the operation. Thus, preoperative intake of a 5-ARI is thought to have no negative effects during the 120-W HPS laser PVP procedure as shown in the present study.
AUR is not only a symptom of BOO caused by BPH but can also be associated with detrusor underactivity. Although these two symptoms are usually distinctively differentiated, they are commonly associated. Hence, this may lead to LUTS or AUR, and treating BOO with the use of a laser is reported to be critical in symptom relief and improving functional impairment [23]. If AUR is left untreated, permanent damage to the detrusor muscle and upper urinary tract deterioration can occur. Thus, AUR needs to be swiftly treated. The present study confirmed improvement in all parameters upon the elimination of BOO through surgery with 120-W HPS laser PVP. A preoperative history of AUR did not seem to have a great influence on postoperative progress. If BOO is eliminated, most AUR induced by BPH can be resolved. Favorable results are anticipated regardless of the preoperative history of AUR if BOO is sufficiently treated.
In cases of a preoperative history of TURP, the pressure of a second operation is felt by both surgeons and patients in most cases. The burden is heavier when LUTS recur owing to BPH after TURP. In the present study, desirable results were acquired when laser resection of the prostate was conducted. The efficacy was sustained for a follow-up period of more than 1 year. Moreover, no significant differences were observed in either group categorized on the basis of a previous history of prostate resection. Thus, the results of the present study suggest that laser ablation of the prostate does not have negative effects in a second operation. A similar or lower retrograde ejaculation rate was verified in laser surgery compared with TURP [24].
This outcome suggests that laser surgery may be more desirable for preventing postoperative retrograde ejaculation after TURP.
The present study aimed to report the results of laser re-section of the prostate performed on more than 500 patients for the last 3 years. The study distinctively investigated the preoperative and postoperative effects of laser resection of the prostate on subjects including different unique cases. The safety and efficacy of laser resection of the prostate has been reconfirmed, because no cases of death, transfusion, or reoperation occurred.
There were some limitations to this study. The nature of the study was retrospective but not randomized. Moreover, there is the likelihood of bias because the research and operations were conducted in a tertiary hospital. To overcome such failings, larger prospective and randomized studies are thought to be essential. Although this study was conducted for about 3 years, the maximum follow-up period was confined to 1 year. To verify the efficacy, a longer postoperative observational period is thought to be crucial.
In conclusion, laser resection of the prostate is safe and effective. The results of the HPS laser PVP procedure were not influenced by the size of prostate, the use of anticoagulants, the intake of 5-ARI for BPH management, a history of AUR, a history of TURP, or other factors. Thus, this study was able to reconfirm the efficacy and safety of laser resection of the prostate.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Yu X, Elliott SP, Wilt TJ, McBean AM. Practice patterns in benign prostatic hyperplasia surgical therapy: the dramatic increase in minimally invasive technologies. J Urol. 2008;180:241–5. doi: 10.1016/j.juro.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 2.Schulman CC, Asplund R, Desgrandchamps F, Jonas U. The impact of nocturia on health status and quality of life in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH) Eur Urol Suppl. 2005;4:1–8. [Google Scholar]
- 3.Alivizatos G, Skolarikos A. Photoselective vaporization of the prostate: review of cost implementation to BPH treatment. Prostate Cancer Prostatic Dis. 2007;10:S15–20. [Google Scholar]
- 4.Kang SH, Choi YS, Kim SJ, Cho HJ, Hong SH, Lee JY, et al. Long-term follow-up results of photoselective vaporization of the prostate with the 120 W Greenlight HPS laser for treatment of benign prostatic hyperplasia. Korean J Urol. 2011;52:260–4. doi: 10.4111/kju.2011.52.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roehrborn CG, Bartsch G, Kirby R, Andriole G, Boyle P, de la Rosette J, et al. Guidelines for the diagnosis and treatment of benign prostatic hyperplasia: a comparative, international overview. Urology. 2001;58:642–50. doi: 10.1016/s0090-4295(01)01402-9. [DOI] [PubMed] [Google Scholar]
- 6.Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006;50:969–79. doi: 10.1016/j.eururo.2005.12.042. [DOI] [PubMed] [Google Scholar]
- 7.Horninger W, Unterlechner H, Strasser H, Bartsch G. Transurethral prostatectomy: mortality and morbidity. Prostate. 1996;28:195–200. doi: 10.1002/(SICI)1097-0045(199603)28:3<195::AID-PROS6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 8.Doll HA, Black NA, McPherson K, Flood AB, Williams GB, Smith JC. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992;147:1566–73. doi: 10.1016/s0022-5347(17)37628-0. [DOI] [PubMed] [Google Scholar]
- 9.Ruszat R, Seitz M, Wyler SF, Muller G, Rieken M, Bonkat G, et al. Prospective single-centre comparison of 120-W diode-pumped solid-state high-intensity system laser vaporization of the prostate and 200-W high-intensive diode-laser ablation of the prostate for treating benign prostatic hyperplasia. BJU Int. 2009;104:820–5. doi: 10.1111/j.1464-410X.2009.08452.x. [DOI] [PubMed] [Google Scholar]
- 10.Malek RS, Kuntzman RS, Barrett DM. Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol. 2005;174(4 Pt 1):1344–8. doi: 10.1097/01.ju.0000173913.41401.67. [DOI] [PubMed] [Google Scholar]
- 11.Ruszat R, Wyler S, Forster T, Reich O, Stief CG, Gasser TC, et al. Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol. 2007;51:1031–8. doi: 10.1016/j.eururo.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336:1506–11. doi: 10.1056/NEJM199705223362107. [DOI] [PubMed] [Google Scholar]
- 13.Bell CR, Murdock PJ, Pasi KJ, Morgan RJ. Thrombotic risk factors associated with transurethral prostatectomy. BJU Int. 1999;83:984–9. doi: 10.1046/j.1464-410x.1999.00075.x. [DOI] [PubMed] [Google Scholar]
- 14.Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004;172(4 Pt 1):1404–8. doi: 10.1097/01.ju.0000139541.68542.f6. [DOI] [PubMed] [Google Scholar]
- 15.Malek RS. Photoselective potassium-titanyl-phosphate (KTP) laser vaporization of the prostate (PVP) vs transurethral re-section of the prostate (TURP) Urology. 2008;72:718–9. doi: 10.1016/j.urology.2008.04.049. [DOI] [PubMed] [Google Scholar]
- 16.Sandhu JS, Ng C, Vanderbrink BA, Egan C, Kaplan SA, Te AE. High-power potassium-titanyl-phosphate photoselective laser vaporization of prostate for treatment of benign prostatic hyperplasia in men with large prostates. Urology. 2004;64:1155–9. doi: 10.1016/j.urology.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 17.McConnell JD. Medical management of benign prostatic hyperplasia with androgen suppression. Prostate Suppl. 1990;3:49–59. doi: 10.1002/pros.2990170506. [DOI] [PubMed] [Google Scholar]
- 18.McConnell JD, Bruskewitz R, Walsh P, Andriole G, Lieber M, Holtgrewe HL, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. Finasteride Long-Term Efficacy and Safety Study Group. N Engl J Med. 1998;338:557–63. doi: 10.1056/NEJM199802263380901. [DOI] [PubMed] [Google Scholar]
- 19.McConnell JD, Roehrborn CG, Bautista OM, Andriole GL, Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–98. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh LE, Jack GS, Lawrentschuk N, Medscape Prevention and management of TURP-related hemorrhage. Nat Rev Urol. 2011;8:504–14. doi: 10.1038/nrurol.2011.106. [DOI] [PubMed] [Google Scholar]
- 21.Araki M, Lam PN, Culkin DJ, Wong C. Decreased efficiency of potassium-titanyl-phosphate laser photoselective vaporization prostatectomy with long-term 5 alpha-reductase inhibition therapy: is it true? Urology. 2007;70:927–30. doi: 10.1016/j.urology.2007.06.1152. [DOI] [PubMed] [Google Scholar]
- 22.Bepple JL, Barone BB, Eure G. The effect of dutasteride on the efficacy of photoselective vaporization of the prostate: results of a randomized, placebo-controlled, double-blind study (DOP trial) Urology. 2009;74:1101–4. doi: 10.1016/j.urology.2009.06.067. [DOI] [PubMed] [Google Scholar]
- 23.Monoski MA, Gonzalez RR, Sandhu JS, Reddy B, Te AE. Uro-dynamic predictors of outcomes with photoselective laser vaporization prostatectomy in patients with benign prostatic hyperplasia and preoperative retention. Urology. 2006;68:312–7. doi: 10.1016/j.urology.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 24.Spaliviero M, Araki M, Wong C. Short-term outcomes of Greenlight HPS laser photoselective vaporization prostatectomy (PVP) for benign prostatic hyperplasia (BPH) J Endourol. 2008;22:2341–7. doi: 10.1089/end.2008.9708. [DOI] [PubMed] [Google Scholar]