Abstract
Pathogenic spirochetes cause clinically relevant diseases in humans and animals, such as Lyme disease and leptospirosis. The causative agent of Lyme disease, Borrelia burgdorferi, and the causative agent of leptospirosis, Leptospria interrogans, encounter reactive oxygen species (ROS) during their enzootic cycles. This report demonstrated that physiologically relevant concentrations of pyruvate, a potent H2O2 scavenger, and provided passive protection to B. burgdorferi and L. interrogans against H2O2. When extracellular pyruvate was absent, both spirochetes were sensitive to a low dose of H2O2 (≈0.6 µM per h) generated by glucose oxidase (GOX). Despite encoding a functional catalase, L. interrogans was more sensitive than B. burgdorferi to H2O2 generated by GOX, which may be due to the inherent resistance of B. burgdorferi because of the virtual absence of intracellular iron. In B. burgdorferi, the nucleotide excision repair (NER) and the DNA mismatch repair (MMR) pathways were important for survival during H2O2 challenge since deletion of the uvrB or the mutS genes enhanced its sensitivity to H2O2 killing; however, the presence of pyruvate fully protected ΔuvrB and ΔmutS from H2O2 killing further demonstrating the importance of pyruvate in protection. These findings demonstrated that pyruvate, in addition to its classical role in central carbon metabolism, serves as an important H2O2 scavenger for pathogenic spirochetes. Furthermore, pyruvate reduced ROS generated by human neutrophils in response to the Toll-like receptor 2 (TLR2) agonist zymosan. In addition, pyruvate reduced neutrophil-derived ROS in response to B. burgdorferi, which also activates host expression through TLR2 signaling. Thus, pathogenic spirochetes may exploit the metabolite pyruvate, present in blood and tissues, to survive H2O2 generated by the host antibacterial response generated during infection.
Introduction
Lyme disease, the most common vector born disease in the United States, is a chronic, system wide infection caused by the pathogen Borrelia burgdorferi (B. burgdorferi) [1]–[3]. B. burgdorferi transmission occurs from its arthropod tick vector, Ixodes sp., during feeding on its human host. Ixodes ticks have a usual two-year life cycle that includes three distinct stages: larvae; nymph; and adult. At each developmental stage, ticks will feed once on a warm-blooded host and undergo a molting process that may proceed for a period of months. Small rodents (especially the white-footed mouse, Peromyscus leucopus) are the primary reservoirs for B. burgdorferi and sources for the bloodmeal during the larvael and nymphal stages of the tick vector. P. leucopus mice infected with B. burgdorferi exhibit minimal tissue pathology and no protective immune response, which demonstrates the susceptibility of this host to chronic infection. In order to survive in both hosts, B. burgdorferi must be able to overcome multiple host defense mechanisms, one of which is bacteriocidal reactive oxygen species (ROS) produced by host cells from both ticks and mammals. In this regard, it has been shown that tick salivary proteins provide significant protection to B. burgdorferi against ROS at the site of tick feeding [4]–[8]. How B. burgdorferi defends against H2O2 after dissemination to systemic sites during mammalian infection remains largely unknown.
As an obligated parasite, B. burgdorferi has a reduced genome and limited enzymes that defend against host ROS attack. B. burgdorferi encodes a superoxide dismutase (Mn-SOD) that supports rapid conversion of superoxide anion radical (O2 −) to hydrogen peroxide (H2O2) [9], [10], but lacks genes encoding catalase or hydroperoxidase that defend against H2O2. This predicts that, in general, Borrelia spp. are inept at defending against H2O2. Although the NADH-dependent Coenzyme A disulphide reductase (CoADR) has been implicated in H2O2 defense [11], deletion of this gene (bb0728) does not influence H2O2 sensitivity [12]. Reports have been conflicting with respect to the sensitivity of B. burgdorferi to H2O2. Some suggest that B. burgdorferi is resistant to H2O2 killing [13], [14], perhaps due to low intracellular iron that prevents DNA damage due to the Fenton reaction [15]. Yet other studies report that B. burgdorferi is sensitive to H2O2 [16], [17]. Thus, the response of B. burgdorferi to H2O2 remains controversial.
Leptospirosis is a multisystem disease caused by Leptospira interrogans (L. interrogans) and exists in nature within a zoonotic cycle. Similar to the enzootic cycle of B. burgdorferi, small rodents, especially rats, are considered critical hosts in the spread of L. interrogans since rats can shed the pathogen in urine and exist as asymptomatic carriers [18]. L. interrogans encodes a functional catalase that is homologous to the heme-dependent KatE family [19], [20]. During interaction with host innate immune cells, transcription of katE is enhanced suggesting an importance during infection [21]. Recent work demonstrates the importance of katE during infection of hamsters [22] implying that H2O2 is a bacteriocidal component of the host defense against L. interrogans.
Pyruvate is a fundamental compound within central carbon metabolism. For over a century, it also has been known that pyruvate can be oxidatively decarboxylated by H2O2 to produce CO2 and acetate [23], [24]. In fact, when peroxide is present it interferes with enzymatic assays that utilize pyruvate [25]. Therefore, pyruvate and other related metabolites have been shown to protect the cell from ionizing radiation, a stress that generates ROS and H2O2 in vitro [24]–[31]. Furthermore, pyruvate can ameliorate the pathological inflammation associated with kidney failure in vivo [32]. Pyruvate is a common additive to the medium for cultivation of eukaryotic cells. During in vitro cultivation cells are exposed to higher O2 concentrations and greater H2O2 stress than that in vivo (21% O2 in vitro versus ≈4–7% O2 in vivo) [33], [34], Indeed, the importance of pyruvate in the cultivation medium is independent of its role as a carbon source, but is due to its potent H2O2-scavenging ability [30], [35]. Given that the standard Barbour-Stoenner-Kelly (BSK-II) medium for cultivation of B. burgdorferi contains 7 mM pyruvate and that the addition of pyruvate to the cultivation medium of L. interrogans enhances cultivation [36], pyruvate present in the medium may serve a beneficial role by scavenging H2O2 that accumulates in complex growth media [37], [38]. Moreover, pyruvate may account for the conflicting results in previous reports on the sensitivity of B. burgdorferi to H2O2.
This study demonstrates that B. burgdorferi and L. interrogans were sensitive to a low dose of H2O2 killing generated by the enzyme glucose oxidase (GOX); however, both pathogens were protected by physiologically relevant concentrations of extracellular pyruvate. The Lyme disease spirochete requires DNA repair pathways to repair H2O2-damaged DNA since mutants within the nucleotide excision repair (NER) and the DNA mismatch repair (MMR) pathways exhibited enhanced sensitivity to H2O2 killing; however, the presence of pyruvate fully protected ΔuvrB and ΔmutS from H2O2 killing further demonstrating the important role of pyruvate in survival. Exogenous pyruvate reduced the ROS production by peripheral blood human neutrophils upon stimulation with the Toll-like receptor 2 (TL2) agonists, B. burgdorferi or zymosan. These results demonstrate that the ubiquitous metabolite, pyruvate, which is present in blood and other tissues, had a previously unappreciated role in protecting the extracellular pathogens B. burgdorferi and L. interrogans from H2O2 stress and may protect these pathogens during their enzootic cycles.
Materials and Methods
Bacterial Strains, Growth Conditions, and Reagents
B. burgdorferi and L. interrogans strains used throughout are listed below. Infectious strain 5A4NP1 is a B31-A3 derived strain (a gift from Drs. H. Kawabata and S. Norris, University of Texas Health Science Center at Houston), which contains a kanamycin resistant gene that disrupts the restriction modification gene bbe02 located on linear plasmid 25 (lp25) [39]. Strain AH130 is an infectious 297 derived strain recovered from an infected patient [40], which has been passed once through laboratory mice [41], [42]. Infectious strain B31-A3 is a clonal isolate from B31-MI [43], which was originally isolated from Ixodes dammini ticks on Shelter Island, New York, USA [44].
B. burgdorferi were grown in BSK medium prepared and supplemented with 6% heat inactivated rabbit serum as described previously ([45], BSK-II) at 37°C in a 5% CO2 incubator. L. interrogans strains were cultivated in liquid Ellinghausen-McCullough-Johnson-Harris (EMJH) medium at 30°C [46], [47].
Sodium pyruvate, H2O2, streptomycin, and kanamycin sulfate (used at 300 µg ml−1) were purchased from Fisher Scientific. Glucose oxidase (E.C. 1.1.3.4, β-D-glucose:oxygen 1-oxidoreductase, GOX), bovine catalase (E.C. 1.11.1.6, H2O2:H2O2 oxidoreductase), and N-acetyl cysteine (NAC) were purchased from Sigma-Aldrich (St. Louis, MO).
Generation of mutS and uvrB Deletions in B. burgdorferi
The mutS gene (bb0797) was deleted from B. burgdorferi strain B31-A3 by homologous recombination with the suicide vector pPCR-Script Cam::ΔmutS::aadA (pCm::ΔmutS-aadA) using a strategy described previously [48]. Briefly, PCR products encoding 1 kb regions upstream and downstream of mutS were amplified from DNA isolated from B. burgdorferi strain B31-A3 with La Taq polymerase (Takara Bio, Madison, WI), while the aadA streptomycin resistance cassette under the control of a flgB promoter (flgBP-aadA) was amplified from the vector pKFSS1 [49] using primers encoding restriction sites for downstream cloning ( Table 1 ) into pPCR-Script CamSK(+) (Agilent Technologies, Cedar Creek, TX). The PCR products were directionally cloned into pPCR-Script Cam SK(+) using restriction enzymes and T4 DNA ligase (New England Biolabs, Ipswich, MA). Electrocompetent B. burgdorferi B31-A3 cells [50] were transformed with 40 µg of pCm::ΔmutS-aadA and mutS mutants were selected for by plating on BSK-II plating medium supplemented with 40 µg ml−1 streptomycin. Deletion of mutS was verified by PCR using primers listed in Table 1 .
Table 1. Primers used in this study.
| Primer name | Sequence (5′-3′) | Reference |
| mutS-KpnI-F | ACTGTAGGTACCTGTAAATACTGTGCAGATATC | This study |
| mutS-EcoRI-R | ACTGTAGAATTCTCTTGATATCTAAATACTGC | This study |
| mutS-EcoRI-F | ACTGTAGAATTCTCAGTCCAGTTAGTATGAGC | This study |
| mutS-SacI-R | ACTGTAGAGCTCATTCCTGGAGTAGAAAGCTC | This study |
| aadA-EcoRI-F | ACTGTAGAATTCTACCCGAGCTTCAAGGAA | This study |
| aadA-EcoRI-R | ACTGTAGAATTCTATTTGCCGACTACCTTG | This study |
H2O2 Killing Assays
Strains 5A4NP1 and AH130 were grown in BSK-II medium to late log phase. Five×107 cells ml−1 were centrifuged at 10,000×g for 10 minutes and thrice washed with 0.9% NaCl. Samples were resuspended to 5×107 cells ml−1 in either BSK-II or modified BSK-II that did not contain pyruvate. Bacteria were challenged with 1 or 2.5 mM H2O2 for 1 hour at 37°C in a 5% CO2 incubator. The reaction was stopped by the addition of 1,000 U ml−1 of bovine catalase and bacteria were centrifuged as above. Cell pellets were washed twice in BSK-II medium containing 1,000 U ml−1 of catalase and resuspended in 1 ml of BSK-II medium. Quantification of viability was determined by limiting dilution in 96-well plates (Fisher Scientific, Pittsburgh, PA) following incubation at 37°C/5% CO2 for 14 days [51]. Controls were incubated in BSK-II and BSK-II without pyruvate and treated with catalase for comparison with H2O2 treated samples.
Alternatively, the viability of wild-type B. burgdorferi B31-A3 and the isogenic ΔmutS and ΔuvrB strains following challenge with H2O2 in the presence or absence of pyruvate was determined by enumerating colony-forming units (CFU) on BSK-II plates. Briefly, strains were grown in BSK-II medium under microaerobic conditions 3% O2, 5% CO2 at 34°C to late log phase. Cell cultures were pelleted by centrifugation at 1200 g for 10 min, washed twice in HN buffer (20 mM NaCl, 50 mM Hepes, pH 7.6) and resuspended in HN buffer +0.2% glucose to a cell density of ≈5×107 cells ml−1. One ml aliquots of cells were transferred to 5 ml polypropylene culture tubes, followed by the addition of sodium pyruvate and/or H2O2. Cultures were incubated at 34°C for 2 h followed by serial dilution in HN buffer and plating on BSK-II. Plates were incubated under microaerobic conditions 3% O2, 5% CO2 at 34°C for 7–14 days to allow for enumeration of CFU. Percent survival for each strain was calculated by dividing the CFU from plates with treated samples by the CFU from plates with untreated samples.
GOX Treatment of Spirochetes
To determine H2O2 production by GOX in BSK-II medium, 0.32 mU ml−1 of GOX was added to sterile BSK-II containing or lacking pyruvate and incubated at 37°C/5% CO2. H2O2 was measured using a commercially available kit ([52] National Diagnostics, Atlanta, Georgia, USA) for 100 h at 37°C/5% CO2. Samples of H2O2 in BSK-II media were diluted 5-fold prior to quantification of H2O2 [52]. A standard curve of (see below) H2O2 was run in parallel. In sterile BSK-II medium without pyruvate, the rate of H2O2 production was linear for ≈24 h and maintained the concentration of H2O2 above 10 µM for 100 h.
To determine the influence of pyruvate on GOX activity in sterile BSK-II medium, 10 units of GOX was added to BSK-II that contained and lacked pyruvate. Samples were incubated as above and the concentration of glucose was measured for 6 h using a commercially available kit (R-BioPharm, Marshall, Michigan, USA).
Strains 5A4NP1 and AH130 were grown as above and inoculated into BSK-II medium containing or lacking pyruvate (7 mM) to 105 cells ml−1. A concentrated preparation of GOX, in 50 mM sodium acetate buffer pH 5.1, was diluted in BSK-II to a final concentration of 0.32 mU ml−1. Growth of spirochetes was monitored by quantification using dark field microscopy over time. Subsequent experiments utilized a relevant concentration of pyruvate, 100 µM. L. interrogans serovars Manilae L495 and Lai 56601 [46], [47] were inoculated to 106 spirochetes ml−1 in EMJH medium plus glucose (2 g L−1) with or without sodium pyruvate (910 µM). Medium without added glucose was used as a control. After 1.5 days of growth, GOX was added to the medium at a final concentration of 0.32 mU ml−1. Growth was monitored by counting spirochetes by dark-field microscopy. Three independent experiments were performed with two or three replicates for each treatment.
Reaction of H2O2 with Pyruvate
The kinetics of the reaction of H2O2 with pyruvate was determined as follows. A sample of H2O2 was prepared, in 50 mM phosphate buffer pH 7.0, by determining the concentration of a 100-fold dilution of a concentrated stock (Fisher Scientific, Pittsburgh, PA). The absorbance at 240 nm was determined and the concentration was determined using a molar extinction coefficient of 43.6 M−1 cm−1 [53]. A standard curve of 1–100 µM H2O2 was prepared and run in parallel. One mM of H2O2 from this solution was added to media that contained or lacked pyruvate at 7 mM and samples were removed and H2O2 was quantified as above.
The reciprocal version of this experiment was performed by measuring the concentration of pyruvate using a commercially available kit (Abcam, Cambridge, Massachusetts, USA). BSK-II medium was prepared without added pyruvate then 7 mM H2O2 was added. One mM of pyruvate was added, samples were removed over time and added to a sample of catalase to stop the reaction. A standard of sodium pyruvate was prepared as previously described by measuring absorbance at 316 nm with an extinction coefficient of 18 M−1 cm−1 [54]. A standard curve of pyruvate was quantitated in parallel with unknown samples.
To calculate the half-life (t1/2) of the reaction in BSK-II medium, the concentration of pyruvate was an excess of 7-fold compared to H2O2 (pseudo-first order reaction). The concentration of H2O2 was measured over time as above. A plot of Ln[H2O2] versus time revealed a straight line within the first 5 minutes of the reaction; the negative slope of this line is equal to the rate constant (k). Data from the linear portion of this graph (0 to 5 minutes) were used to calculate the t1/2 using the equation t1/2 = Ln2/k. The same experiment was performed with the concentration of H2O2 present in excess of 7-fold of pyruvate. Pyruvate was measured over time as above and the t1/2 was determined as above.
Production of Acetate from the Reaction of Pyruvate with H2O2
A solution of H2O2 was prepared as above and 1 mM was added to BSK-II medium. Over time, aliquots were removed and added to tubes containing 200 U ml−1 of bovine catalase to stop the reaction. The concentration of acetate produced from the reaction was determined using a commercially available kit from R-Biopharm. To confirm the reaction was pyruvate-dependent, H2O2 was added to BSK-II medium that lacked pyruvate. To confirm that H2O2 is required, H2O2 was added to BSK-II medium that contained bovine catalase. Also, in a separate experiment, the concentration of pyruvate was manipulated in BSK-II medium that was prepared without the addition of pyruvate. Bovine catalase was used to stop the reactions that contained different equimolar concentrations of pyruvate/H2O2 and the concentration of acetate was determined as above.
Stimulation of Superoxide Production in Human Neutrophils by B. burgdorferi
This study was approved by Indiana University School of Medicine Institute Review Boards, and written informed consent was obtained from donors. Human neutrophils were isolated from heparin-anticoagulated venous blood using Polymorphprep (AXIS-SHIELD PoC, Oslo, Norwary). Superoxide production by neutrophils stimulated with live or heat-inactivated B. burgdorferi, with or without pyruvate, was measured by luminol chemiluminescence assay [55]. Specifically, 2.5×105 human neutrophils were plated into a well of a 96-well plate (COSTAR, Corning, NY) in PBSG (PBS plus 0.9 mM CaCl2, 0.5 mM MgCl2, 20 mM dextrose) in the presence of 50 µM luminol and horseradish peroxidase (HRP; final concentration: 20 U ml−1), without or with superoxide dismutase (SOD; final concentration: 75 µg ml−1) and kept on ice for 10 minutes prior to the assay. B. burgdorferi (2.5×106 cells) in 25 µl of PBS were added to wells, and the plate was spun down at 800 r.p.m. for 1 min immediately prior to reading. Relative light units (RLU) were monitored at 60-second intervals for up to one hour by the Long Kinetic module in an Lmax microplate luminometer (Molecular Devices, Sunnyvale, CA). Integrated RLU values were calculated by SOFTmax software (Molecular Devices).
Statistical Analyses
Statistical significance was determined using a Student’s t test and when multiple comparisons were made the p value was corrected using the Bonferroni correction. When comparing three or more groups to a control value, One way Analysis of Variance (ANOVA) was used. Because data expressed as percent impart a fixed range on the data (0–100%), the percent values were transformed to arcsine values using the formula SIN−1(√(%/100)) prior to One way ANOVA testing. A post-hoc test (Dunnett’s multiple comparisons) was used to test significance. Some experiments used a Two-way ANOVA to determine significance.
Results
Pyruvate Protects Borrelia burgdorferi against H2O2
B. burgdorferi encounters ROS stress during its infectious cycle. H2O2 diffuses across prokaryotic and eukaryotic cell membranes with the permeability much like H2O to impair cellular functions [56]–[60]. Conflicting results have been reported on the response of B. burgdorferi to H2O2 [13], [14], [16], [17]. We noticed that an important distinction among these reports is the difference in methodology; when B. burgdorferi is challenged with H2O2 in BSK-II medium it is highly resistant [13], [14], but when challenged in minimal buffers it is sensitive [16], [17]. We hypothesized that pyruvate (7 mM) present in BSK-II medium may account for the previous observations of H2O2 resistance [13], [14], [16].
To test the hypothesis that the presence of pyruvate in BSK-II medium protects against H2O2, we compared spirochete killing by H2O2 in either standard BSK-II medium or in BSK-II medium which lacked pyruvate. Two infectious strains of B. burgdorferi, 5A4NP1 (an isolate of strain B31) and AH130 (an isolate of strain 297), were incubated with various concentrations of H2O2 for one hour and cell viability was assessed by limiting dilution method. Similar to the work of others [13],[14], when cultured in BSK-II media with pyruvate the spirochetes were resistant to H2O2 treatment ( Fig. 1 ). However, when pyruvate was excluded from the medium, 1 mM H2O2 was sufficient to reduce spirochete viability by over 1 log, and spirochete killing by H2O2 was dose dependent (Fig. 1AB). Thus, we conclude that pyruvate passively protects B. burgdorferi from H2O2.
Figure 1. Pyruvate Protects Borrelia burgdorferi From H2O2 Stress.
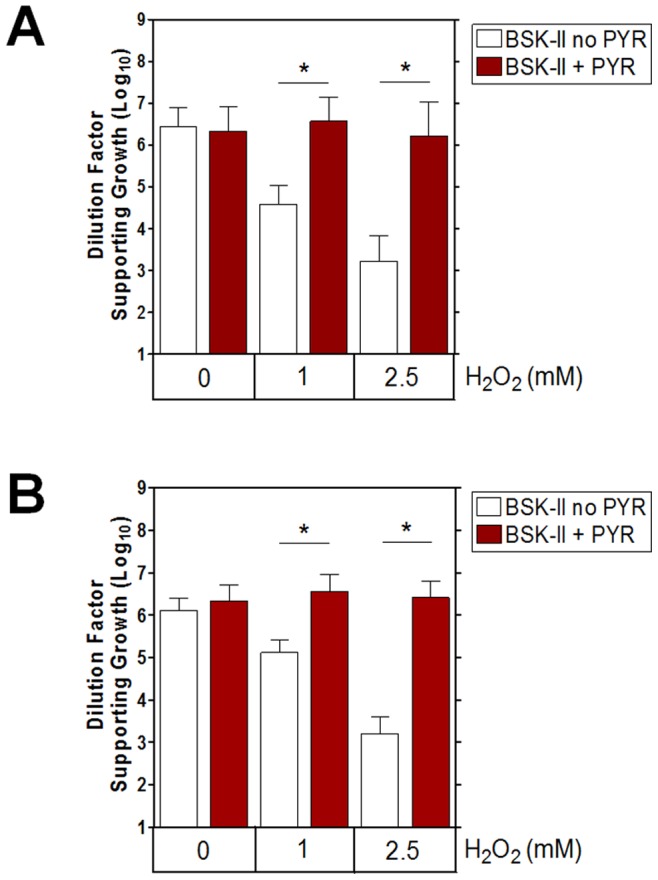
(A) 5A4NP1 and (B) AH130 were challenged in BSK-II medium for 1 h with various concentrations of H2O2 in the presence or absence of pyruvate. Viability was determined by limiting dilution. Data shown are mean +/− SD from three separate experiments. A paired Student’s t test determined significance (* p≤0.025, corrected by Bonferroni adjustment).
Experiments from Fig. 1 demonstrate the protective role of pyruvate in preserving borrelial viability during exposure to a single pulse of H2O2. Although such an approach is commonly used to assess H2O2 sensitivity for many cell types, this experimental design does not recapitulate the scenario of H2O2 stress in vivo where pathogens often encounter low doses of sustained H2O2 production [61]. For instance, the ex vivo rate of H2O2 produced by activated macrophages has been measured at ≈0.15 nmol h−1 per 105 macrophages [62]. To expose B. burgdorferi to a steady, low dose concentration of H2O2, glucose oxidase (GOX) from Aspergillus niger was used. This flavoenzyme allowed steady production of H2O2 and D-glucono-δ-lactone from glucose and O2. GOX activity was not influenced by pyruvate, as the presence or absence of pyruvate had no influence on the glucose consumption by GOX in BSK-II medium ( Fig. 2A ). The presence of 0.32 mU ml−1 of GOX in BSK-II medium (lacking pyruvate) was sufficient to generate a rate of H2O2 at 0.62±0.1 µM per h (or 0.62 nmoles ml−1) ( Fig. 2B ) and maintained the concentration of H2O2 above 10 µM for 100 h (data not shown). The addition of pyruvate to BSK-II medium significantly reduced the detection of H2O2. Thus, such a system (BSK-II minus pyruvate plus GOX) allowed us to determine the prolonged impact of steady low levels of H2O2 on the growth of B. burgdorferi. When cultivated within such medium, B. burgdorferi exhibited a significant growth defect ( Fig. 2C ). Pyruvate is a ubiquitous metabolite. In human blood, pyruvate is typically within a range of ≈50 to 300 µM, but is subject to significant flux [63]–[67]. BSK-II medium contains 7 mM pyruvate, which is substantially higher than concentrations of pyruvate in vivo. Therefore, to determine the relevance of the protection against H2O2 by pyruvate, we repeated the experiments shown in Fig. 2C with a physiologically relevant concentration of pyruvate, 100 µM. Using strain 5A4NP1, it is apparent that 100 µM protects against a low dose of H2O2 generated by GOX ( Fig. 2D ). These results indicate that B. burgdorferi is sensitive to the physiological relevant concentration of H2O2 and that a relevant concentration of pyruvate allows uninhibited growth in the presence of H2O2.
Figure 2. B. burgdorferi Are Sensitive to a Low Dose of H2O2 Produced by Glucose Oxidase (GOX).
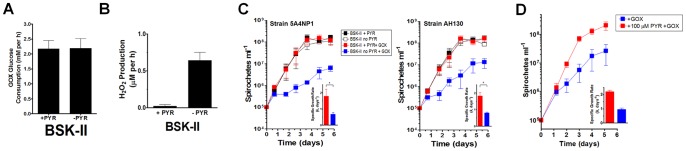
(A) Pyruvate does not alter GOX activity in BSK-II medium. Ten units of GOX were added to BSK-II medium containing or lacking pyruvate. Glucose was measured for 6 h to determine GOX activity. Data shown are mean +/− SD (n = 2). (B) The presence of pyruvate reduces the presence of H2O2 in BSK-II medium. GOX (0.32 mU ml−1) was added to BSK-II medium containing or lacking pyruvate and H2O2 was measured for 100 h. The linear rate of H2O2 production over 24 h is shown. Data are from 2 separate experiments performed in 2 separate batches of medium. (C) 5A4NP1 (left panel) and AH130 (right panel) were inoculated in BSK-II medium containing or lacking pyruvate in the presence or absence of GOX. Data shown are mean +/− SD from three separate experiments. The inset shows the specific growth rate (k, days−1) during cultivation in GOX-containing BSK-II with (red bar) and without (blue) pyruvate. GOX was added at 0.32 mU ml−1. A paired Student’s t test determined significance (* p≤0.05). (D) Experiments from (C) were repeated with strain 5A4NP1 using a physiologically relevant concentration of sodium pyruvate (100 µM) with GOX treatment. Data shown are from two separate experiments and the inset shows the specific growth rate (k, days−1) during cultivation in GOX-containing BSK-II with (red bar) and without (blue) pyruvate. GOX was added at 0.32 mU ml−1.
Pyruvate Protects B. burgdorferi DNA Repair Mutants from Oxidative Stress
Because of B. burgdorferi’s lack of intracellular iron that could participate in the Fenton reaction, B. burgdorferi was predicted to be resistant to oxidative DNA damage when treated with H2O2 [15]. This prediction was supported by the observation that B. burgdorferi challenged with high concentrations of H2O2 were resistant to killing and did not show evidence of DNA damage [13]. However, recent studies have shown that B. burgdorferi strains harboring mutations in NER genes (uvrA, uvrB and uvrC) are hypersensitive to killing and DNA damage following exposure to either ROS or RNS [48], [68], [69]. These observations suggest that the lack of DNA damage in ROS-challenged wild-type cells is likely due to efficient DNA repair. To determine whether exogenous pyruvate could protect B. burgdorferi from H2O2-mediated DNA damage, we compared the sensitivity of strain B31-A3 and isogenic mutants in the NER gene uvrB and the MMR gene mutS to increasing concentrations of H2O2 in HN buffer supplemented with 0.2% glucose. Both the uvrB and mutS-deficient mutant displayed significant reductions in survival compared to wild-type cells when challenged with either 100 or 500 µM H2O2 ( Fig. 3A ). The addition of 500 µM H2O2 reduced the survival of wild-type cells to 44% following 2 h of exposure, while only 1% of uvrB or mutS-deficient cells survived. This supports a crucial role for both the NER and MMR pathways in the repair of oxidative DNA damage. Despite the hypersensitivity of the uvrB or mutS-deficient strains to oxidative stress, the addition of 2.5 mM pyruvate completely protected both from the lethal effects of 100 and 500 µM H2O2 ( Fig. 3B ). Collectively, these data support the H2O2-scavenging role for pyruvate and demonstrate the necessity of both the NER and MMR pathways for protection of the B. burgdorferi genome from potential lethal oxidative DNA lesions.
Figure 3. Pyruvate Protects DNA Repair Mutants Strains From ROS.
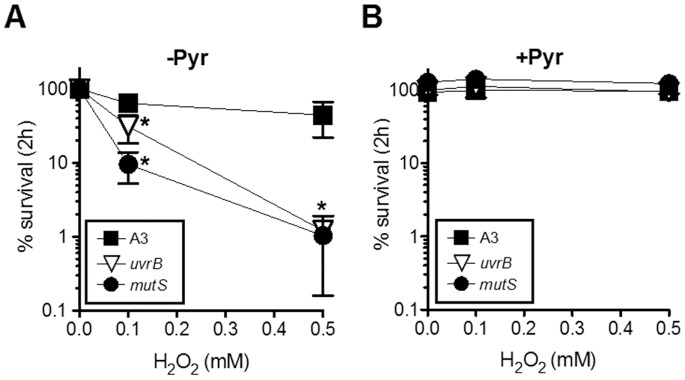
Wild-type B. burgdorferi B31 A3 and the isogenic DNA repair mutants ΔuvrB and ΔmutS were exposured to 0, 0.1 or 0.5 mM H2O2 in HN buffer +0.2% glucose in the (A) absence or (B) presence of 2.5 mM pyruvate for 2 h. Percent survival was calculated by enumerating CFU. Data represent the mean +/− SD (n = 4). Two-way ANOVA was used to determine significance (* p<0.01).
Pyruvate Reacts Directly with H2O2
BSK-II medium is a complex medium that contains 6% rabbit serum, 5% BSA, and other ingredients. To determine whether pyruvate in BSK-II protects B. burgdorferi by scavenging H2O2 and if so, how fast the reaction between H2O2 and pyruvate occurs in BSK-II, and whether other ingredients of BSK-II significantly react with H2O2, we measured the degradation of 1 mM of H2O2 in BSK-II medium containing or lacking 7 mM pyruvate. The result showed that the half-life of H2O2 was 1.7 minutes in BSK-II, but 989 minutes in BSK-II medium lacking pyruvate, a difference of 580-fold ( Fig. 4A ). This result indicates that pyruvate is a primary factor that promotes the breakdown of H2O2 in BSK-II medium. We also measured the consumption of pyruvate in BSK-II medium containing and lacking 7 mM H2O2, and the result confirmed the reaction between pyruvate and H2O2 ( Fig. 4B ).
Figure 4. Pyruvate and H2O2 Produce Acetate.
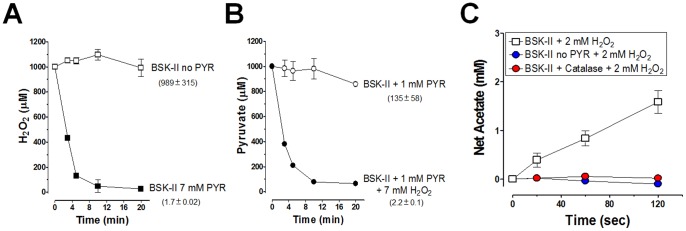
(A) One mM H2O2 was added to pyruvate-free BSK-II and standard BSK-II and H2O2 was measured over time using the xylenol orange/ferric iron assay [52]. (B) One mM pyruvate was added to pyruvate-free BSK-II. H2O2 (7 mM) was added and pyruvate was measured over time using a commerically available kit. Data shown are mean +/− SD (n = 3). The half-life values, in minutes, are shown in parentheses. (C) Production of acetate by pyruvate and H2O2 requires both reactants in BSK-II medium. The production of acetate was measured over time in BSK-II medium that contained pyruvate (7 mM), lacked pyruvate, and contained pyruvate with the addition of bovine catalase (200 U ml−1).
The reaction between pyruvate and H2O2 generates CO2 and acetate [24]. To confirm this reaction occurred in BSK-II medium, acetate production was measured over time. The production of acetate occurred when both pyruvate and H2O2 were present in BSK-II medium ( Fig. 4C ). Furthermore, the production of acetate was blocked by catalase, indicating the dependence of this reaction on H2O2 ( Fig. 4C ). Thus, pyruvate protects B. burgdorferi against H2O2 by a non-enzymatic reaction between pyruvate and H2O2 to produce acetate (and CO2).
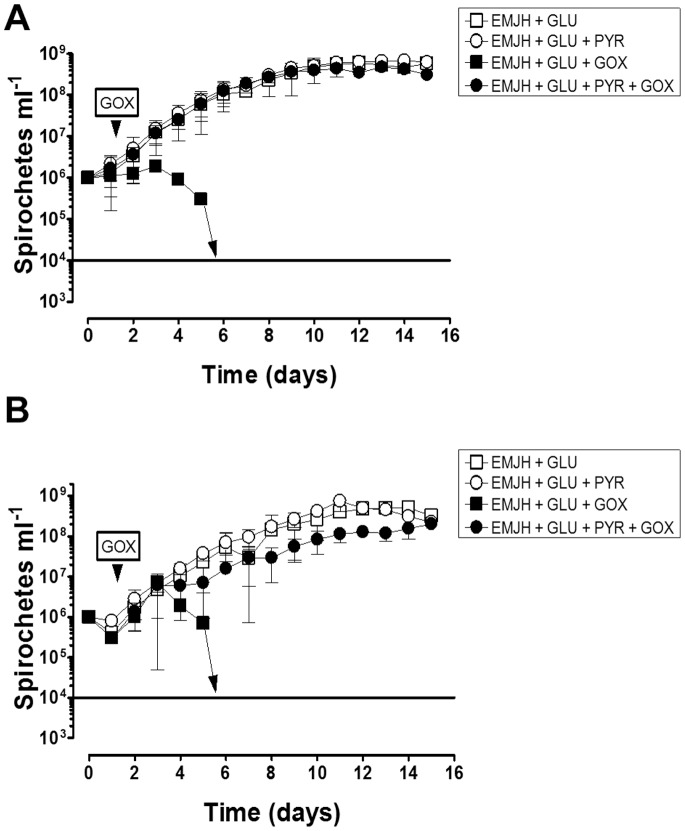
Pyruvate Protects Pathogenic Leptospira interrogans against H2O2 Killing
Because pathogenic spirochetes exist mainly as extracellular pathogens in vivo and pyruvate exists in extracellular fluids in vivo, it is possible that spirochetes other than B. burgdorferi are protected against H2O2 with relevant concentrations of pyruvate. To test this, two pathogenic strains of L. interrogans serovar Manilae L495 ( Fig. 5A ) and serovar Lai 56601 ( Fig. 5B ) were tested for growth defects in the presence of GOX with and without added pyruvate. Strains were cultivated in EMJH medium with added glucose (GLU) with or without added pyruvate. As with B. burgdorferi, the addition of pyruvate did not influence the growth of either L. interrogans serovar in liquid cultures (Fig. 5AB). Following the addition of GOX to cultures that lacked added pyruvate, the concentration of serovars Manilae L495 and serovar Lai 56601 spirochetes decreased appreciably until day 6 when no detectable spirochetes were present (limit of detection is 104 spirochetes ml−1, Fig. 5AB). This demonstrates a decrease of ≥3 orders of magnitude of spirochete cell density from days 3 to 6. However, the presence of pyruvate protected both pathogenic strains from GOX challenge (Fig. 5AB). Despite the presence of catalase within these pathogenic strains, both were sensitive to a low dose of H2O2 generated by GOX, which was abrogated by the addition of pyruvate to the culture medium. Thus, pyruvate protects both catalase positive (L. interrogans) and catalase negative (B. burgdorferi) spirochetes from H2O2 killing.
Figure 5. Pyruvate Protects Pathogenic Strains of Leptospira interrogans Against H2O2.
(A) L. interrogans serovar Manilae L495 was challenged with GOX (0.32 mU ml−1) in EMJH medium with and without added pyruvate (PYR). Stationary phase cultures were diluted to 106 cells ml−1 in EMJH medium with glucose (2 g L−1) and with or without PYR (910 µM). After 1.5 days of growth, GOX was added, indicated by the arrowhead and growth was monitored by direct counting of spirochetes by dark field microscopy. The limit of detection (LOD) for direct counting is indicated by a solid line and cultures with spirochetes below the LOD are indicated by the arrow pointing to the line, which corresponds to ≈104 spirochetes ml−1. (B) L. interrogans serovar Lai 56601 was challenged with GOX as described above. Results in (A) and (B) show the mean ±1 SD from three separate experiments performed in duplicate or triplicate.
Pyruvate Reduces Reactive Oxygen Species Exposure of B. burgdorferi by Human Neutrophils
The above results demonstrate that pyruvate protects B. burgdorferi from H2O2 killing under in vitro cultivation conditions. Given that during infection, myeloid derived immune cells are potent generators of H2O2, it is unknown whether pyruvate would react with ROS produced by neutrophils in response to B. burgdorferi stimulus. Neutrophils were chosen to test this since they are recruited to sites of B. burgdorferi infection [70], [71] and are known to generate cytotoxic molecules capable of killing B. burgdorferi [17], [72]. Neutrophils from peripheral human blood were isolated, incubated with B. burgdorferi, and ROS detection was determined in the presence or absence of pyruvate using a luminol-based assay [55], [73]. Peripheral neutrophils elicit robust ROS production in response to B. burgdorferi ( Fig. 6A ). However, the presence of 0.5 mM pyruvate dramatically reduced ROS production by human neutrophils ( Fig. 6A ). Neutrophils are capable of localizing the NADPH oxidase complex to the plasma membrane [74]. Thus, we expected to see a decrease in the extracellular ROS produced by neutrophils in the presence of pyruvate. Surprisingly, intracellular ROS was also reduced by pyruvate, suggesting that pyruvate may enter neutrophil phagosomes. To characterize further the influence of pyruvate on ROS production by human neutrophils, we repeated these experiments with different concentrations of pyruvate. Results are presented as percentage of integrated RLU [55]. As a control, we used the antioxidant N-acetyl-L-cysteine (NAC), which is a known scavenger of ROS and inhibitor of mitogen-activated protein kinase (MAPK) activation of the NADPH oxidase complex [75], [76]. A potent activator of ROS production by neutrophils, serum opsonized zymosan (SOZ), through TLR2 served as the positive control [77], [78]. ROS produced by neutrophils and B. burgdorferi was set to 100% and compared to neutrophils+B. burgdorferi+antioxidant (either pyruvate or NAC). The addition of 0.2 mM of pyruvate significantly reduced the ROS production of B. burgdorferi-stimulated neutrophils by >20% compared to neutrophils stimulated in the absence of pyruvate ( Fig. 6B ). Furthermore, 5 mM pyruvate decreased the production of ROS by neutrophils stimulated B. burgdorferi by ≈50% ( Fig. 6B ). Although 0.2, 0.5, and 2 mM significantly reduced the total ROS production by neutrophils compared to no addition of pyruvate, the difference of inhibition was not significant when comparing between 0.2, 0.5, and 2 mM pyruvate. This suggests that the pyruvate-dependent decrease in production of ROS by neutrophils may exhibit a bimodal pattern of inhibition. For SOZ controls, pyruvate was capable of decreasing the ROS produced by the positive control SOZ by ≈50%. For this comparison, neutrophils+SOZ was set to 100%. Thus, pyruvate is a strong scavenger of ROS in the context of neutrophil activation by B. burgdorferi or SOZ. As expected, NAC reduced the ROS produced by B. burgdorferi stimulated neutrophils by ≈80% and by ≈65% for SOZ stimulated neutrophils ( Fig. 6B ). These data suggest that pyruvate reduces the exposure of B. burgdorferi to ROS produced by neutrophils.
Figure 6. Pyruvate Reduces the Detection of ROS Generated by Human Neutrophils.
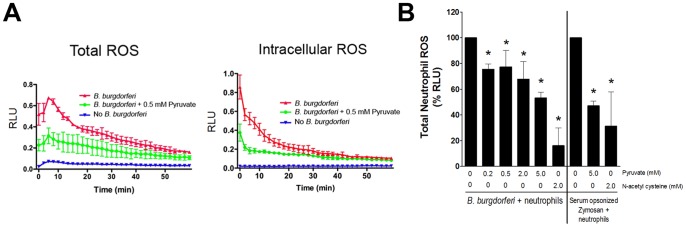
(A) Human peripheral neutrophils were incubated with B. burgdorferi 5A4NP1 strain, ratio of 10∶1 B. burgdorferi:neutrophil, and ROS generation over 1 h was determined using the luminol detection assay and are expressed as Relative Light Units (RLU). (B) Human peripheral neutrophils were incubated with 5A4NP1, ratio of 10∶1 B. burgdorferi:neutrophil, and ROS generation over 1 h was determined using the luminol detection assay. Data shown are the integrated RLU for the duration of 3 separate experiments. Zymosan (SOZ) is a positive control for neutrophil activation and N-acetylcysteine (NAC) is a positive control for reduction of ROS. ROS produced by neutrophils with B. burgdorferi was set to 100% and the significance was compared to neutrophils+B. burgdorferi+antioxidant (pyruvate or NAC) using One-way ANOVA. Although percentages are shown, data were transformed to arcsine values using the formula SIN−1(√(%/100)) prior to One way ANOVA testing (* p<0.05). ROS produced by neutrophils with SOZ was set to 100% and significance was determined with One way ANOVA (* p<0.05) compared to the same condition with added antioxidant.
Discussion
B. burgdorferi lacks classical enzymatic defenses against H2O2, leaving this spirochete as shown here, susceptible to killing by this membrane permeable form of ROS ( Figs. 1 , 2CD, and 3). Yet, contradictory reports regarding B. burgdorferi sensitivity to H2O2 have to this point remained unexplained [13], [14], [16], [17]. The current study revealed an essential role for pyruvate in protecting B. burgdorferi from H2O2 toxicity. Despite the plethora of data demonstrating the protective role of pyruvate and related 2-oxo acids against H2O2 [23]–[32], the ability of pyruvate to protect against H2O2 killing in the context of pathogenic bacteria has been overlooked. In the complex medium of BSK-II without pyruvate, H2O2 slowly dissipated, but when pyruvate was present, it reacted with H2O2 rapidly (Fig. 4AB). Consistent with these observations prior to the development of BSK-II medium, extracellular catalase addition was noted to promote the growth of B. hermsii, a related spirochete [79].
For B. burgdorferi, H2O2 caused DNA damage since mutants deficient in the NER or MMR DNA repair pathways exhibited enhanced sensitivity to H2O2 killing. Pyruvate fully protected three wild-type strains and both DNA repair mutants (ΔuvrB and ΔmutS). Although the mechanism of H2O2 killing for L. interrogans was not examined in this study, the addition of pyruvate also protected two pathogenic strains from H2O2 despite the presence of catalase within these spirochetes. Moreover, it is apparent that L. interrogans are more sensitive to H2O2 generated by GOX treatment than B. burgdorferi. B. burgdorferi was capable of growing, although at a rate severely below their potential, in response to GOX treatment; however, the same concentration of GOX reduced L. interrogans cell density to undetectable levels (Figs. 2CD and 5). This difference may be due to the lack of iron in B. burgdorferi metabolism compared to L. interrogans, which encodes several anabolic and catabolic pathways that require iron [15], [80]. Not surprisingly, Leptospira spp. require iron for growth [81]. Thus, B. burgdorferi is inherently more resistant to H2O2 than L. interrogans.
Pyruvate was capable of reducing both the intracellular and extracellular ROS produced by human neutrophils ( Fig. 6 ). Our results suggest a possible bimodal pattern to inhibition of ROS by pyruvate; one that is more sensitive to pyruvate inhibition and another that is less sensitive. In the absence of additional data to identify and explain the cause for such a pattern of inhibition, we are reluctant to speculate on the ROS-generating factor(s) that may also be inhibited by pyruvate. Given the use of HRP in the luminol assay and the breadth of pyruvate in metabolism and immune cell regulation/activation, this is not a surprising result. Note that the ROS/neutrophil experiments conducted in this study were designed to specifically measure ROS production not killing. Preliminary data using the same MOI and conditions for measuring ROS did not reveal any difference in killing at the end of the experiment (data not shown). To completely address this issue in a rigorous manner, a detailed optimization of experiments will be needed.
It was expected that extracellular ROS produced by the plasma membrane localized NADPH oxidase complex would be quickly scavenged by extracellular pyruvate. Yet, intracellular ROS production was also diminished by pyruvate addition suggesting that pyruvate can efficiently enter neutrophil phagosomes. The extracellular addition of pyruvate to neutrophils is known to increase intracellular pyruvate concentrations [82]. Moreover, it is known that another ROS scavenger, NAC, reduces ROS and inhibits mitogen-activated protein kinase (MAPK) activation of the NADPH oxidase complex [75], [76]. Small molecular antioxidants may act by directly scavenging ROS or via regulating signal pathways dependent on ROS. NFκB and AP-1 are redox-dependent transcription factors that activate many antibacterial processes within immune cells and their functions are reduced by the antioxidant NAC [83], [84]. Furthermore, pyruvate reduced the ROS production in response to TLR2 activation by SOZ in human neutrophils. The host inflammatory response to B. burgdorferi lipoproteins requires TLR2 [85]. Moreover, upon interaction with host monocytes B. burgdorferi induces expression of host TLR2 and enters monocytes through a TLR2-dependent mechanism [86]. Because pyruvate reduces the ROS production by human neutrophils in response to both SOZ and B. burgdorferi it suggests that TLR2 expression or function may be perturbed. Additional work is needed to elucidate the precise mechanism of the role of pyruvate upon TL2-mediated inflammation in response to stimulus. Because pyruvate directly scavenges H2O2, a signal that activates host transcription factors NFκB and AP-1, pyruvate could reduce the activation of antibacterial pathways and protect pathogens against H2O2 damage.
Monocytes and neutrophils are competent to kill B. burgdorferi in vitro and in vivo [17], [72], [86], [87]. Despite the sensitivity of B. burgdorferi to ROS and RNS in vitro, there are no differences in B. burgdorferi burden within wild-type mice compared to mice lacking either the phagocytic NADPH oxidase [88] or the inducible nitric oxide synthase (iNOS) [89]. Because B. burgdorferi exploits salivary proteins in the tick vector for protection against ROS and host complement [4]–[8], it is likely that B. burgdorferi exploits additional factors to allow persistent infection. Pyruvate may be a factor within the host that B. burgdorferi utilizes for protection against ROS. Pyruvate can also scavenge RNS generated by the host. Peroxynitrite is a potent antimicrobial compound generated by the reaction between superoxide and nitric oxide and pyruvate scavenges peroxynitrite through a non-enzymatic reaction [90]. Similar to H2O2, peroxynitirite has been implicated in NFκB and AP-1 activation within neutrophils [91], [92]. Although the role of peroxynitrite in the host response against B. burgdorferi or L. interrogans is unknown, peroxynitrite is implicated in the host defense against bacterial pathogens [93], [94]. Thus, host pyruvate may scavenge H2O2 and additional reactive compounds during infection that modulate the host response to B. burgdorferi or L. interrogans.
Pyruvate is a ubiquitous metabolite. In human blood, pyruvate is typically within a range of ≈50 to 300 µM, but is subject to significant flux [63]–[67]. The concentration of pyruvate in blood and tissues colonized by B. burgdorferi during infection of the murine model of Lyme disease is currently unknown. In the guinea pig heart, pyruvate inhibits the ROS formation and cardiac NADH oxidase activity during ischemia/reperfusion events [95]. In the clinical setting, either bacterial-initiated sepsis or febrile bacterial infection increases blood pyruvate concentrations [96], [97]. During spirochete infection, the blood pyruvate concentration of laboratory rats infected with the relapsing fever spirochete, B. recurrentis, increase 3-fold during the peak of spirochetemia [98]. However, the physiological relevance and mechanism for this increase is unknown.
In conclusion, this work shows that B. burgdorferi and L. interrogans are sensitive to H2O2 killing. This work clarifies the discordant data from separate groups regarding sensitivity of B. burgdorferi to H2O2 killing, and further demonstrated the critical role of pyruvate in protection from H2O2 damage for both pathogenic spirochetes B. burgdorferi and L. interrogans. Finally, this work implies that extracellular pathogens may exploit pyruvate in host blood and tissue for protection against H2O2.
Acknowledgments
We thank Drs. Steve Norris, H. Kawabata, and Patti Rosa for providing strains 5A4NP1 and B31 A3. We thank Dr. Ryan Fink for advice on statistical analysis.
Funding Statement
Funding for this work was partially provided by NIH grant R01 AI083640, Indiana INGEN and METACyt grants of Indiana University, funded by the Lilly Endowment, Inc. (to XFY), National Center for Research Resources (5P20RR016469) and the National Institute for General Medical Science (NIGMS) (5P20GM103427) (to TJB). A component of the National Institutes of Health (NIH) and its contents are the sole responsibility of the authors and do not necessarily represent the official views of NIGMS or NIH. BT and MYZ were supported by NIH T32 training grant 5T32AI060519. This investigation was partially conducted in a facility constructed with support from research facilities improvement program grant number C06 RR015481-01 from National Center for Research Resources, NIH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Steere AC, Grodzicki RL, Kornblatt AN, Craft JE, Barbour AG, et al. (1983) The spirochetal etiology of Lyme disease. N Engl J Med 308: 733–740. [DOI] [PubMed] [Google Scholar]
- 2. Benach JL, Bosler EM, Hanrahan JP, Coleman JL, Habicht GS, et al. (1983) Spirochetes isolated from the blood of two patients with Lyme disease. N Engl J Med 308: 740–742. [DOI] [PubMed] [Google Scholar]
- 3. Burgdorfer W, Barbour A, Hayes S, Benach J, Grunwaldt E, et al. (1982) Lyme disease-a tick-borne spirochetosis? Science 18: 1317–1319. [DOI] [PubMed] [Google Scholar]
- 4. Guo X, Booth CJ, Paley MA, Wang X, DePonte K, et al. (2009) Inhibition of neutrophil function by two tick salivary proteins. Infect Immun 77: 2320–2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dai J, Wang P, Adusumilli S, Booth CJ, Narasimhan S, et al. (2009) Antibodies against a tick protein, Salp15, protect mice from the Lyme disease agent. Cell Host Microbe 6: 482–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schuijt TJ, Hovius JW, van Burgel ND, Ramamoorthi N, Fikrig E, et al. (2008) The tick salivary protein Salp15 inhibits the killing of serum-sensitive Borrelia burgdorferi sensu lato isolates. Infect Immun 76: 2888–2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Narasimhan S, Sukumaran B, Bozdogan U, Thomas V, Liang X, et al. (2007) A tick antioxidant facilitates the Lyme disease agent's successful migration from the mammalian host to the arthropod vector. Cell Host Microbe 2: 7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ramamoorthi N, Narasimhan S, Pal U, Bao F, Yang XF, et al. (2005) The Lyme disease agent exploits a tick protein to infect the mammalian host. Nature 436: 573–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Troxell B, Xu H, Yang XF (2012) Borrelia burgdorferi, a pathogen that lacks iron, encodes manganese-dependent superoxide dismutase essential for resistance to streptonigrin. J Biol Chem 287: 19284–19293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Esteve-Gassent MD, Elliott NL, Seshu J (2009) sodA is essential for virulence of Borrelia burgdorferi in the murine model of Lyme disease. Mol Microbiol 71: 594–612. [DOI] [PubMed] [Google Scholar]
- 11. Boylan JA, Hummel CS, Benoit S, Garcia-Lara J, Treglown-Downey J, et al. (2006) Borrelia burgdorferi bb0728 encodes a coenzyme A disulphide reductase whose function suggests a role in intracellular redox and the oxidative stress response. Mol Microbiol 59: 475–486. [DOI] [PubMed] [Google Scholar]
- 12. Eggers CH, Caimano MJ, Malizia RA, Kariu T, Cusack B, et al. (2011) The coenzyme A disulphide reductase of Borrelia burgdorferi is important for rapid growth throughout the enzootic cycle and essential for infection of the mammalian host. Mol Microbiol 82: 679–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Boylan JA, Lawrence KA, Downey JS, Gherardini FC (2008) Borrelia burgdorferi membranes are the primary targets of reactive oxygen species. Mol Microbiol 68: 786–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hyde JA, Shaw DK, Smith R 3rd, Trzeciakowski JP, Skare JT (2010) Characterization of a conditional bosR mutant in Borrelia burgdorferi . Infect Immun 78: 265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Posey JE, Gherardini FC (2000) Lack of a role for iron in the Lyme disease pathogen. Science 288: 1651–1653. [DOI] [PubMed] [Google Scholar]
- 16. Li X, Pal U, Ramamoorthi N, Liu X, Desrosiers DC, et al. (2007) The Lyme disease agent Borrelia burgdorferi requires BB0690, a Dps homologue, to persist within ticks. Mol Microbiol 63: 694–710. [DOI] [PubMed] [Google Scholar]
- 17. Lusitani D, Malawista SE, Montgomery RR (2002) Borrelia burgdorferi are susceptible to killing by a variety of human polymorphonuclear leukocyte components. J Infect Dis 185: 797–804. [DOI] [PubMed] [Google Scholar]
- 18. Sterling CR, Thiermann AB (1981) Urban rats as chronic carriers of leptospirosis: an ultrastructural investigation. Vet Pathol 18: 628–637. [DOI] [PubMed] [Google Scholar]
- 19. Austin FE, Barbieri JT, Corin RE, Grigas KE, Cox CD (1981) Distribution of superoxide dismutase, catalase, and peroxidase activities among Treponema pallidum and other spirochetes. Infect Immun 33: 372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rao PJ, Larson AD, Cox CD (1964) Catalase activity in Leptospira . J Bacteriol 88: 1045–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Xue F, Dong H, Wu J, Wu Z, Hu W, et al. (2010) Transcriptional responses of Leptospira interrogans to host innate immunity: significant changes in metabolism, oxygen tolerance, and outer membrane. PLoS Negl Trop Dis 4: e857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Eshghi A, Lourdault K, Murray GL, Bartpho T, Sermswan RW, et al. (2012) Leptospira interrogans catalase is required for resistance to H2O2 and for virulence. Infect Immun 80: 3892–3899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Holleman MAF (1904) Notice sur l'action de l'eau oxygénée sur les acides acétoniques et sur les dicétones 1.2. Recl Trav Chim Pays-Bas Belg 23: 169–172. [Google Scholar]
- 24. Fedotcheva NI, Sokolov AP, Kondrashova MN (2006) Nonezymatic formation of succinate in mitochondria under oxidative stress. Free Radic Biol Med 41: 56–64. [DOI] [PubMed] [Google Scholar]
- 25. Vlessis AA, Bartos D, Trunkey D (1990) Importance of spontaneous alpha-ketoacid decarboxylation in experiments involving peroxide. Biochem Biophys Res Commun 170: 1281–1287. [DOI] [PubMed] [Google Scholar]
- 26. Nath KA, Enright H, Nutter L, Fischereder M, Zou JN, et al. (1994) Effect of pyruvate on oxidant injury to isolated and cellular DNA. Kidney Int 45: 166–176. [DOI] [PubMed] [Google Scholar]
- 27. Desagher S, Glowinski J, Premont J (1997) Pyruvate protects neurons against hydrogen peroxide-induced toxicity. J Neurosci 17: 9060–9067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Giandomenico AR, Cerniglia GE, Biaglow JE, Stevens CW, Koch CJ (1997) The importance of sodium pyruvate in assessing damage produced by hydrogen peroxide. Free Radic Biol Med 23: 426–434. [DOI] [PubMed] [Google Scholar]
- 29. Ramakrishnan N, Chen R, McClain DE, Bunger R (1998) Pyruvate prevents hydrogen peroxide-induced apoptosis. Free Radic Res 29: 283–295. [DOI] [PubMed] [Google Scholar]
- 30. O'Donnell-Tormey J, Nathan CF, Lanks K, DeBoer CJ, de la Harpe J (1987) Secretion of pyruvate. An antioxidant defense of mammalian cells. J Exp Med 165: 500–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Thompson TL, Mefferd RB Jr, Wyss O (1951) The protection of bacteria by pyruvate against radiation effects. J Bacteriol 62: 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Salahudeen AK, Clark EC, Nath KA (1991) Hydrogen peroxide-induced renal injury. A protective role for pyruvate in vitro and in vivo. J Clin Invest 88: 1886–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campbell JA (1931) Gas tensions in the tissues. Physiological Reviews 11: 1–40. [Google Scholar]
- 34. Mik EG, van Leeuwen TG, Raat NJ, Ince C (2004) Quantitative determination of localized tissue oxygen concentration in vivo by two-photon excitation phosphorescence lifetime measurements. J Appl Physiol 97: 1962–1969. [DOI] [PubMed] [Google Scholar]
- 35. Krieg NR, Hoffman PS (1986) Microaerophily and oxygen toxicity. Annu Rev Microbiol 40: 107–130. [DOI] [PubMed] [Google Scholar]
- 36. Johnson RC, Walby J, Henry RA, Auran NE (1973) Cultivation of parasitic leptospires: effect of pyruvate. Appl Microbiol 26: 118–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Norrod EP, Morse SA (1982) Presence of hydrogen peroxide in media used for cultivation of Neisseria gonorrhoeae . J Clin Microbiol 15: 103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pine L, Hoffman PS, Malcolm GB, Benson RF, Franzus MJ (1986) Role of keto acids and reduced-oxygen-scavenging enzymes in the growth of Legionella species. J Clin Microbiol 23: 33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kawabata H, Norris SJ, Watanabe H (2004) BBE02 disruption mutants of Borrelia burgdorferi B31 have a highly transformable, infectious phenotype. Infect Immun 72: 7147–7154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hughes CA, Kodner CB, Johnson RC (1992) DNA analysis of Borrelia burgdorferi NCH-1, the first northcentral U.S. human Lyme disease isolate. J Clin Microbiol 30: 698–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hubner A, Yang X, Nolen DM, Popova TG, Cabello FC, et al. (2001) Expression of Borrelia burgdorferi OspC and DbpA is controlled by a RpoN-RpoS regulatory pathway. Proc Natl Acad Sci U S A 98: 12724–12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yang XF, Pal U, Alani SM, Fikrig E, Norgard MV (2004) Essential role for OspA/B in the life cycle of the Lyme disease spirochete. J Exp Med 199: 641–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Elias AF, Stewart PE, Grimm D, Caimano MJ, Eggers CH, et al. (2002) Clonal polymorphism of Borrelia burgdorferi strain B31 MI: implications for mutagenesis in an infectious strain background. Infect Immun 70: 2139–2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Burgdorfer W, Barbour AG, Hayes SF, Benach JL, Grunwaldt E, et al. (1982) Lyme disease-a tick-borne spirochetosis? Science 216: 1317–1319. [DOI] [PubMed] [Google Scholar]
- 45. Barbour AG (1984) Isolation and cultivation of Lyme disease spirochetes. Yale J Biol Med 57: 521–525. [PMC free article] [PubMed] [Google Scholar]
- 46. Ellinghausen HC Jr, McCullough WG (1965) Nutrition of Leptospira Pomona and growth of 13 other serotypes: fractionation of oleic albumin complex and a medium of bovine albumin and polysorbate 80. Am J Vet Res 26: 45–51. [PubMed] [Google Scholar]
- 47. Johnson RC, Harris VG (1967) Differentiation of pathogenic and saprophytic letospires. I. growth at low temperatures. J Bacteriol 94: 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bourret TJ, Boylan JA, Lawrence KA, Gherardini FC (2011) Nitrosative damage to free and zinc-bound cysteine thiols underlies nitric oxide toxicity in wild-type Borrelia burgdorferi . Mol Microbiol 81: 259–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Frank KL, Bundle SF, Kresge ME, Eggers CH, Samuels DS (2003) aadA confers streptomycin resistance in Borrelia burgdorferi . J Bacteriol 185: 6723–6727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Samuels DS (1995) Electrotransformation of the spirochete Borrelia burgdorferi . Methods Mol Biol 47: 253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Seshu J, Boylan JA, Hyde JA, Swingle KL, Gherardini FC, et al. (2004) A conservative amino acid change alters the function of BosR, the redox regulator of Borrelia burgdorferi . Mol Microbiol 54: 1352–1363. [DOI] [PubMed] [Google Scholar]
- 52. Jiang ZY, Woollard AC, Wolff SP (1990) Hydrogen peroxide production during experimental protein glycation. FEBS Lett 268: 69–71. [DOI] [PubMed] [Google Scholar]
- 53. Beers RF Jr, Sizer IW (1952) A spectrophotometric method for measuring the breakdown of hydrogen peroxide by catalase. J Biol Chem 195: 133–140. [PubMed] [Google Scholar]
- 54. Margolis SA, Coxon B (1986) Identification and quantation of the impurities in sodium pyruvate. Analytical Chemistry 58: 2504–2510. [Google Scholar]
- 55. Tian W, Li XJ, Stull ND, Ming W, Suh CI, et al. (2008) Fc gamma R-stimulated activation of the NADPH oxidase: phosphoinositide-binding protein p40phox regulates NADPH oxidase activity after enzyme assembly on the phagosome. Blood 112: 3867–3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Xiang TX, Anderson BD (1994) The relationship between permeant size and permeability in lipid bilayer membranes. J Membr Biol 140: 111–122. [DOI] [PubMed] [Google Scholar]
- 57. Seaver LC, Imlay JA (2001) Hydrogen peroxide fluxes and compartmentalization inside growing Escherichia coli . J Bacteriol 183: 7182–7189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ohno Y, Gallin JI (1985) Diffusion of extracellular hydrogen peroxide into intracellular compartments of human neutrophils. Studies utilizing the inactivation of myeloperoxidase by hydrogen peroxide and azide. J Biol Chem 260: 8438–8446. [PubMed] [Google Scholar]
- 59. Root RK, Metcalf J, Oshino N, Chance B (1975) H2O2 release from human granulocytes during phagocytosis. I. Documentation, quantitation, and some regulating factors. J Clin Invest 55: 945–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fettiplace R (1978) The influence of the lipid on the water permeability of artificial membranes. Biochim Biophys Acta 513: 1–10. [DOI] [PubMed] [Google Scholar]
- 61.Fang FC (2011) Antimicrobial actions of reactive oxygen species. MBio 2. [DOI] [PMC free article] [PubMed]
- 62. Vazquez-Torres A, Jones-Carson J, Mastroeni P, Ischiropoulos H, Fang FC (2000) Antimicrobial actions of the NADPH phagocyte oxidase and inducible nitric oxide synthase in experimental salmonellosis. I. Effects on microbial killing by activated peritoneal macrophages in vitro. J Exp Med 192: 227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Landon J, Fawcett JK, Wynn V (1962) Blood pyruvate concentration measured by a specific method in control subjects. J Clin Pathol 15: 579–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Huckabee WE (1958) Relationships of pyruvate and lactate during anaerobic metabolism. III. Effect of breathing low-oxygen gases. J Clin Invest 37: 264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Huckabee WE (1958) Relationships of pyruvate and lactate during anaerobic metabolism. II. Exercise and formation of O-debt. J Clin Invest 37: 255–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Huckabee WE (1958) Relationships of pyruvate and lactate during anaerobic metabolism. I. Effects of infusion of pyruvate or glucose and of hyperventilation. J Clin Invest 37: 244–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Debray FG, Mitchell GA, Allard P, Robinson BH, Hanley JA, et al. (2007) Diagnostic accuracy of blood lactate-to-pyruvate molar ratio in the differential diagnosis of congenital lactic acidosis. Clin Chem 53: 916–921. [DOI] [PubMed] [Google Scholar]
- 68. Hardy PO, Chaconas G (2013) The nucleotide excision repair system of Borrelia burgdorferi is the sole pathway involved in repair of DNA damage by UV light. J Bacteriol 195: 2220–2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sambir M, Ivanova LB, Bryksin AV, Godfrey HP, Cabello FC (2011) Functional analysis of Borrelia burgdorferi uvrA in DNA damage protection. FEMS Microbiol Lett 317: 172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Brown CR, Blaho VA, Loiacono CM (2004) Treatment of mice with the neutrophil-depleting antibody RB6-8C5 results in early development of experimental lyme arthritis via the recruitment of Gr-1- polymorphonuclear leukocyte-like cells. Infect Immun 72: 4956–4965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ritzman AM, Hughes-Hanks JM, Blaho VA, Wax LE, Mitchell WJ, et al. (2010) The chemokine receptor CXCR2 ligand KC (CXCL1) mediates neutrophil recruitment and is critical for development of experimental Lyme arthritis and carditis. Infect Immun 78: 4593–4600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Xu Q, Seemanapalli SV, Reif KE, Brown CR, Liang FT (2007) Increasing the recruitment of neutrophils to the site of infection dramatically attenuates Borrelia burgdorferi infectivity. J Immunol 178: 5109–5115. [DOI] [PubMed] [Google Scholar]
- 73. Dahlgren C, Karlsson A (1999) Respiratory burst in human neutrophils. J Immunol Methods 232: 3–14. [DOI] [PubMed] [Google Scholar]
- 74. Burritt JB, DeLeo FR, McDonald CL, Prigge JR, Dinauer MC, et al. (2001) Phage display epitope mapping of human neutrophil flavocytochrome b558. Identification of two juxtaposed extracellular domains. J Biol Chem 276: 2053–2061. [DOI] [PubMed] [Google Scholar]
- 75. Guyton KZ, Liu Y, Gorospe M, Xu Q, Holbrook NJ (1996) Activation of mitogen-activated protein kinase by H2O2. Role in cell survival following oxidant injury. J Biol Chem 271: 4138–4142. [DOI] [PubMed] [Google Scholar]
- 76. Fialkow L, Chan CK, Rotin D, Grinstein S, Downey GP (1994) Activation of the mitogen-activated protein kinase signaling pathway in neutrophils. Role of oxidants. J Biol Chem 269: 31234–31242. [PubMed] [Google Scholar]
- 77. DeChatelet LR, Long GD, Shirley PS, Bass DA, Thomas MJ, et al. (1982) Mechanism of the luminol-dependent chemiluminescence of human neutrophils. J Immunol 129: 1589–1593. [PubMed] [Google Scholar]
- 78. Sato M, Sano H, Iwaki D, Kudo K, Konishi M, et al. (2003) Direct binding of Toll-like receptor 2 to zymosan, and zymosan-induced NF-kappa B activation and TNF-alpha secretion are down-regulated by lung collectin surfactant protein A. J Immunol. 171: 417–425. [DOI] [PubMed] [Google Scholar]
- 79. Kelly R (1971) Cultivation of Borrelia hermsi . Science 173: 443–444. [DOI] [PubMed] [Google Scholar]
- 80. Nascimento AL, Ko AI, Martins EA, Monteiro-Vitorello CB, Ho PL, et al. (2004) Comparative genomics of two Leptospira interrogans serovars reveals novel insights into physiology and pathogenesis. J Bacteriol 186: 2164–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Faine S (1959) Iron as a growth requirement for pathogenic Leptospira. J Gen Microbiol 20: 246–251. [DOI] [PubMed] [Google Scholar]
- 82. Mathioudakis D, Engel J, Welters ID, Dehne MG, Matejec R, et al. (2011) Pyruvate: immunonutritional effects on neutrophil intracellular amino or alpha-keto acid profiles and reactive oxygen species production. Amino Acids 40: 1077–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kaminski MM, Sauer SW, Klemke CD, Suss D, Okun JG, et al. (2010) Mitochondrial reactive oxygen species control T cell activation by regulating IL-2 and IL-4 expression: mechanism of ciprofloxacin-mediated immunosuppression. J Immunol 184: 4827–4841. [DOI] [PubMed] [Google Scholar]
- 84. Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82: 47–95. [DOI] [PubMed] [Google Scholar]
- 85. Hirschfeld M, Kirschning CJ, Schwandner R, Wesche H, Weis JH, et al. (1999) Cutting edge: inflammatory signaling by Borrelia burgdorferi lipoproteins is mediated by toll-like receptor 2. J Immunol 163: 2382–2386. [PubMed] [Google Scholar]
- 86. Cervantes JL, Dunham-Ems SM, La Vake CJ, Petzke MM, Sahay B, et al. (2011) Phagosomal signaling by Borrelia burgdorferi in human monocytes involves Toll-like receptor (TLR) 2 and TLR8 cooperativity and TLR8-mediated induction of IFN-beta. Proc Natl Acad Sci U S A 108: 3683–3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Menten-Dedoyart C, Faccinetto C, Golovchenko M, Dupiereux I, Van Lerberghe PB, et al. (2012) Neutrophil extracellular traps entrap and kill Borrelia burgdorferi sensu stricto spirochetes and are not affected by Ixodes ricinus tick saliva. J Immunol 189: 5393–5401. [DOI] [PubMed] [Google Scholar]
- 88. Crandall H, Ma Y, Dunn DM, Sundsbak RS, Zachary JF, et al. (2005) Bb2Bb3 regulation of murine Lyme arthritis is distinct from Ncf1 and independent of the phagocyte nicotinamide adenine dinucleotide phosphate oxidase. Am J Pathol 167: 775–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Brown CR, Reiner SL (1999) Development of lyme arthritis in mice deficient in inducible nitric oxide synthase. J Infect Dis 179: 1573–1576. [DOI] [PubMed] [Google Scholar]
- 90. Vasquez-Vivar J, Denicola A, Radi R, Augusto O (1997) Peroxynitrite-mediated decarboxylation of pyruvate to both carbon dioxide and carbon dioxide radical anion. Chem Res Toxicol 10: 786–794. [DOI] [PubMed] [Google Scholar]
- 91. Zouki C, Jozsef L, Ouellet S, Paquette Y, Filep JG (2001) Peroxynitrite mediates cytokine-induced IL-8 gene expression and production by human leukocytes. J Leukoc Biol 69: 815–824. [PubMed] [Google Scholar]
- 92. Jozsef L, Filep JG (2003) Selenium-containing compounds attenuate peroxynitrite-mediated NF-kappaB and AP-1 activation and interleukin-8 gene and protein expression in human leukocytes. Free Radic Biol Med 35: 1018–1027. [DOI] [PubMed] [Google Scholar]
- 93. Henard CA, Vazquez-Torres A (2011) Nitric oxide and salmonella pathogenesis. Front Microbiol 2: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Alam MS, Akaike T, Okamoto S, Kubota T, Yoshitake J, et al. (2002) Role of nitric oxide in host defense in murine salmonellosis as a function of its antibacterial and antiapoptotic activities. Infect Immun 70: 3130–3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Bassenge E, Sommer O, Schwemmer M, Bunger R (2000) Antioxidant pyruvate inhibits cardiac formation of reactive oxygen species through changes in redox state. Am J Physiol Heart Circ Physiol 279: H2431–2438. [DOI] [PubMed] [Google Scholar]
- 96. Gore DC, Jahoor F, Hibbert JM, DeMaria EJ (1996) Lactic acidosis during sepsis is related to increased pyruvate production, not deficits in tissue oxygen availability. Ann Surg 224: 97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Gilbert VE (1968) Blood pyruvate and lactate during febrile human infections. Metabolism 17: 943–951. [DOI] [PubMed] [Google Scholar]
- 98. Fulton JD, Smith PJ (1960) Carbohydrate metabolism in Spirochaeta recurrentis. 1. The metabolism of spirochaetes in vivo and in vitro . Biochem J 76: 491–499. [DOI] [PMC free article] [PubMed] [Google Scholar]