Abstract
Objective
The objective was to assess processes of care for patients with diabetes undergoing elective surgery.
Methods
A retrospective review of medical records was conducted to determine frequency of perioperative glucose monitoring, changes in glucose control, and treatment of intraoperative hyperglycemia.
Results
A total of 268 patients underwent 287 elective procedures. Mean age was 67 years, 63% were men, 97% had type 2 diabetes, and most (57%) were treated with oral hypoglycemic agents. Average perioperative time was approximately 8 h. Mean preoperative hemoglobin A1c was 7.0%; however, this value was checked in only 52% of cases. A glucose measurement was obtained in 89% of cases in the preoperative area and in 87% in the postanesthesia care unit, but in only 33% of cases did a value get checked intraoperatively. Average glucose was 139 mg/dl preoperatively, increasing to 166 mg/dl postoperatively (p <.001). Glucose levels increased regardless of type of outpatient medical therapy used to treat hyperglycemia, except for those on combination oral agents plus insulin (p =.06).
Conclusions
These data indicate suboptimal documentation of outpatient hemoglobin A1c. Intraoperative glucose monitoring seldom occurred, despite prolonged periods under anesthesia and perioperative deterioration of glycemic control. Standards need to be developed and interventions are needed to enhance management of diabetes patients undergoing elective procedures.
Keywords: diabetes, hyperglycemia, perioperative, surgical
Introduction
Diabetes mellitus continues to increase in prevalence, with nearly 8% of the United States population now carrying the diagnosis.1 Patients with diabetes have a higher risk of requiring surgery than do persons without diabetes, and surgery in these patients has been associated with increased morbidity and mortality.2–4 Current research indicates that outpatient glycemic control (as assessed by hemoglobin A1c) and perioperative hyperglycemia contribute to poorer surgical outcomes in patients undergoing cardiac surgery.5–8 multiple studies on the effects of hyperglycemia in persons with or without diabetes who are undergoing cardiac or vascular surgery have shown a link between perioperative hyperglycemia and worse patient outcomes.9–13 In addition, the development of perioperative hyperglycemia has been correlated with an increased rate of surgical site infections.14–16
Multiple mechanisms may explain how hyperglycemia can lead to poorer outcomes among patients undergoing surgery. Perioperative hyperglycemia has been associated with abnormalities in granulocyte adherence, impaired phagocytosis, delayed chemotaxis, and depressed bactericidal capacity, all of which could lead to a greater susceptibility to wound infection.17 Hyperglycemia has been shown to increase generation of reactive oxygen species and inflammatory cytokine concentrations.17
Successful control of hyperglycemia during the perioperative phase of patient care can ensure a successful glucose transition either to the health team caring for the individual in the hospital (if the patient is admitted) or to the patient and family (if the patient is discharged home immediately after the procedure). We previously reported on an analytic approach to evaluate the different segments of perioperative management of patients with diabetes on insulin pump therapy.18 Because little data exist on the perioperative care of the more general diabetes population, we adapted this previous model to test the hypothesis that there were aspects of care in need of improvement in the perioperative care of the non-insulin-pump-managed diabetes patients undergoing elective surgery.
Methods
Case Selection
Adult patients (aged ≥18 years) with a diagnosis of diabetes who underwent an elective surgical procedure under general anesthesia between January 1, 2011, and April 30, 2011, were identified by electronic discharge data. Patients who were already hospitalized prior to a surgical procedure were not included. Our facility does not treat obstetric or pediatric patients, thus the analysis included only adult patients. Additionally, patients on outpatient insulin pump therapy for the management of diabetes were excluded from this analysis because they had been included previously in a separate review.18 The Mayo Clinic Institutional Review Board approved this study.
Data Abstraction
The electronic medical record for each patient was reviewed, and relevant data were abstracted. Demographics (age, sex, and race/ethnicity) were recorded. Also abstracted were type of diabetes, self-reported duration of diabetes, type of outpatient diabetes therapy (e.g., diet, oral agents, insulin) prior to surgery, body mass index (weight in kg/height in m2), hemoglobin A1c (HbA1c), glucose levels, American Society of Anesthesiologists’ classification, type of surgery performed, and surgical service.
As previously described, the perioperative period was defined as the time from admission to the preoperative unit through discharge from the postanesthesia care unit.18 The perioperative period was further divided into preoperative, intraoperative, and postanesthesia care unit phases, and the duration of each phase was recorded for every patient. Additionally, the duration of the surgical procedure itself was calculated. Preoperative, intraoperative, and postanesthesia care unit records were reviewed for each patient. The following variables were recorded from each chart: time in specific perioperative phases; preoperative, intraoperative, and postoperative blood glucose levels; type of blood glucose monitoring; and perioperative treatment of blood glucose.
Data Analysis
Several patients underwent multiple operations during the review period, so each individual surgical case was treated as an independent observation. Data are reported as mean (standard deviation (SD)) or as number (percentage), as applicable. Differences in HbA1c and glucose levels were initially evaluated using both parametric and nonparametric methods; since both methods revealed identical findings, statistical differences are reported using paired or unpaired t tests, or χ2 as appropriate. If multiple glucose values were obtained within a perioperative segment, they were averaged prior to making statistical comparisons.
Results
Characteristics of Patients
Data were analyzed for a total of 268 unique patients with diabetes who underwent a total of 287 elective surgical procedures; 17 patients had 2 procedures, 1 had 3, and the rest had only 1. Mean (SD) age of the 268 patients was 67 (11) years. Most patients were male, white, and identified as having type 2 diabetes. On the basis of body mass index, most were obese, and the mean (SD) self-reported duration of diabetes was 12 (12) years. Preoperatively, most patients were treated with oral medications only, followed by insulin only, diet, and a combination of insulin and oral medications. Preoperative medical evaluations were conducted in 192 (68%) of cases. Mean (SD) preoperative HbA1c was 7.0% (1.4%); however, a preoperative HbA1c was obtained in only 52% (n = 149) of the 287 cases, with average interval being 13 (18) days prior to surgery. In instances where HbA1c was checked, 53 (36%) of values were 7.0%, and 21 (14%) were 8.0%. Patients taking combination oral agents plus insulin had significantly higher HbA1c values than persons on diet therapy, oral agents only, or insulin alone (all p < .01 for combination therapy versus other therapies). There were no differences in HbA1c among patients managed with diet, oral agents, or insulin. Most cases had an American Society of Anesthesiologists’ physical status of 3, connoting severe, systemic disease. After most [219/287 (76%)] surgical procedures, patients required admission (Table 1).
Table 1.
Characteristics of 268 Patients with Diabetes Undergoing 287 Surgical Proceduresa
| Characteristic | N (%)b |
|---|---|
| Age, mean (SD), years | 67 (11) |
| White race | 239 (89) |
| Male sex | 170 (63) |
| BMI, mean (SD) | 31.3 (6.7) |
| DM, type 2, mean (SD) | 259 (97) |
| Preoperative medical evaluations | 192 (68) |
| Hemoglobin A1c, mean (SD) | 7.0 (1.4) |
| Outpatient DM medication | |
| Oral and insulin | 16 (6) |
| Diet | 38 (14) |
| Insulin | 60 (23) |
| Oral | 153 (57) |
| Duration of DM, mean (SD), years | 12 (12) |
| ASA level 3 | 187 (70) |
| Admitted after procedure | 219 (76) |
ASA, American Society of Anesthesiology; BMI, body mass index (weight in kg/height in m2); DM, diabetes mellitus.
Data are number (percentage) unless indicated otherwise.
Characteristics of Surgical Procedures
Perioperative times are summarized as mean (SD) and range in Figure 1. The average time of the surgical procedure was 127 (101) min, and 205 (72%) operations lasted 60 min or longer. The most common types of surgery were urologic [62/287 (22%)], orthopedic [59/287 (21%)], and general surgery [43/287 (15%)], with the rest representative of other surgical specialties (Table 2).
Figure 1.
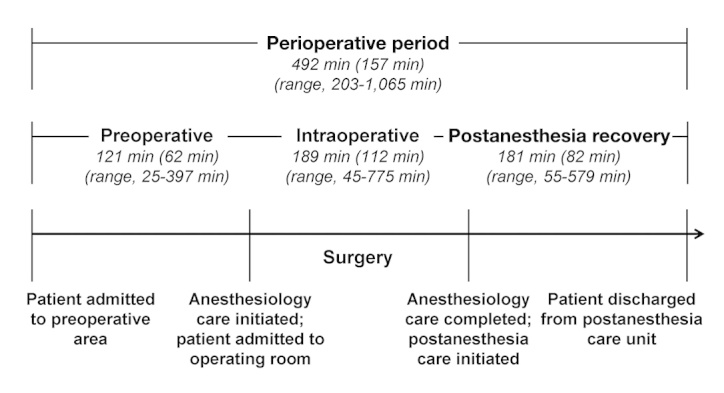
Phases of perioperative care defined by location. Time data are shown in minutes as mean (standard deviation) and range. (Adapted from Nassar and colleagues,18 with permission from the American Association of Clinical Endocrinologists.)
Table 2.
Distribution of 287 Surgical Procedures by Type of Surgical Service
| Type of surgical service | Procedures, n (%) |
|---|---|
| Urology | 62 (22) |
| Orthopedic | 59 (21) |
| General | 43 (15) |
| Transplant | 29 (10) |
| Otolaryngology | 26 (9) |
| Vascular | 20 (7) |
| Neurosurgery | 13 (4) |
| Gynecology | 12 (4) |
| Plastics | 10 (4) |
| Colorectal | 9 (3) |
| Cardiothoracic | 4 (1) |
Perioperative Glucose Monitoring
In most cases, glucose was checked during the preoperative and postanesthesia care unit phases of care (Figure 2). In the preoperative area, 254 of the 287 cases (89%) had glucose monitoring performed ; of these, 229 (90%) had point-of-care (POC) blood glucose (BG) levels only, 4 (2%) had venous measurements, and 21 (8%) had both POC BG and venous samples. Intraoperatively, glucose was checked in only 95 (33%) cases. Of all 287 cases, 30 (10%) had POC BG values alone, 47 (16%) had blood gas sampling, and 18 (6%) had POC BG plus blood gas sampling. In the postanesthesia care unit, 251 (87%) of all 287 cases had glucose levels obtained: 217 (86%) were POC BG values alone, 3 (1%) were venous, and 31 (12%) had both.
Figure 2.
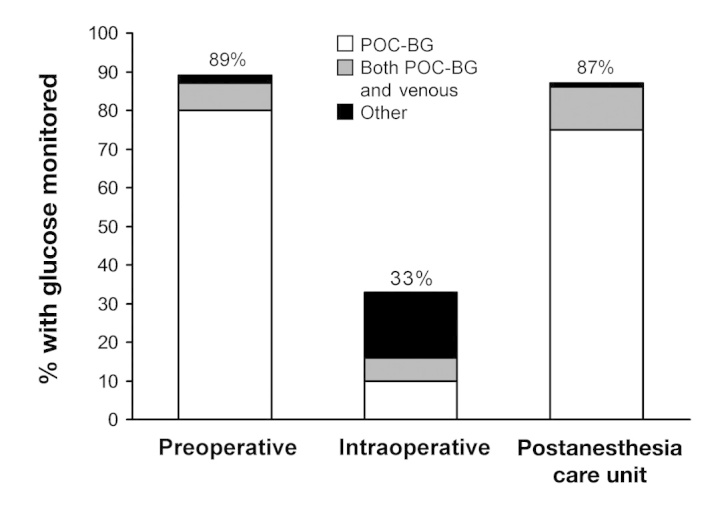
Blood glucose monitoring defined by perioperative phase and type of monitoring performed. Other denotes a laboratory test other than a point-of-care blood glucose measurement.
More patients had glucose measurements obtained the longer the procedure (p < .01). For procedures lasting 61 to 120 min, 23% (20/87) had a glucose measured, while 44% (26/59), 52% (16/31), and 86% (24/28) of cases with procedures lasting 121 to 180, 181 to 240, and >240 min, respectively, had at least one glucose measurement. The intraoperative monitoring frequency for patients on diet, combined oral agents plus insulin, insulin, and oral agents was 7%, 8%, 35%, and 51%, respectively (p < .01; not shown).
Perioperative Glucose Control
The average intraoperative POC BG was 168 (46) mg/dl, and the mean glucose value obtained from other methods was 176 (48) mg/ dl. Glucose control was compared between preoperative and postanesthesia care unit phases of care. Only POC BG values were considered because they constituted the majority of measurements. In paired analysis (n = 222 pairs), the mean (SD) overall preoperative glucose was 139 (45) mg/dl, which increased to 166 (45) mg/dl in the postanesthesia care unit (p < .01; Figure 3). Patients whose diabetes was managed with oral agents, insulin, or diet alone as outpatients had higher glucose levels (all p < .01) in the postanesthesia care unit than in the preoperative area (Figure 3).
Figure 3.
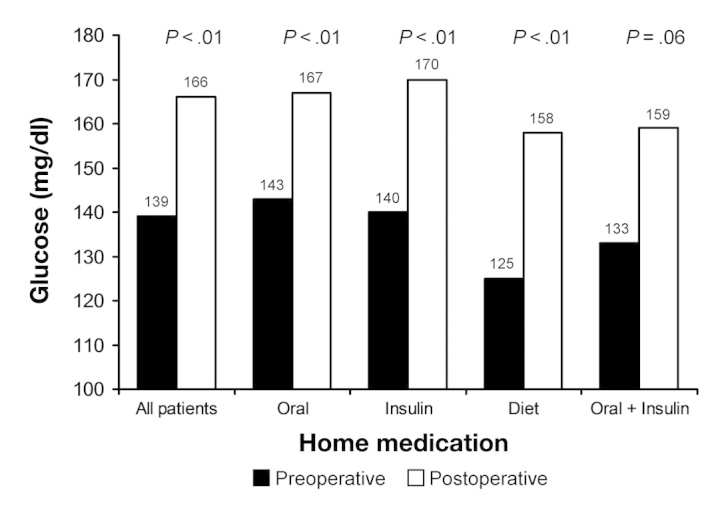
Preoperative versus postoperative blood glucose. Preoperative and postoperative blood glucose values are stratified by type of home medication.
Perioperative Glucose Management
Perioperatively, the 287 cases were given insulin as follows: 6 (2%) cases received insulin preoperatively, 35 (12%) received insulin intraoperatively, and 87 (30%) received it in the postanesthesia care unit. Intraoperatively, 7 of the 35 cases were placed on insulin infusions. Otherwise, insulin was given as either an intravenous or subcutaneous bolus.
Discussion
Patients with diabetes are known to have worse morbidity and mortality when undergoing surgery, and hyperglycemia is associated with worse patient outcomes. Currently, little detail is available about how patients with diabetes are being managed as they transition through the various phases of perioperative care. The purpose of this study was to better define current practice for these patients undergoing elective surgery, with the goal of identifying aspects of care that could be targeted for improvement.
Additionally, the analysis also helped characterize our surgical patient population with diabetes. Most were older, had type 2 diabetes, had fair glucose control preoperatively based on HbA1c values (at least among those who had measurements), and were American Society of Anesthesiologists’ class 3. Most procedures were urologic or orthopedic. Most patients required outpatient pharmacologic treatment for hyperglycemia, and approximately one-fourth were on insulin, either alone or in combination with oral agents. The high prevalence of pharmacologic treatment for diabetes underscores the need to have guidelines for patients on how to adjust their diabetes treatment in the days leading up to surgery.
Long-term glycemic control may be measured preoperatively using HbA1c. Studies have shown an association between elevated HbA1c and decreased insulin sensitivity,19 as well as an increase in morbidity, in patients undergoing surgery.5–8 In a study of patients with diabetes undergoing noncardiac surgery, HbA1c <7% was associated with decreased complications due to infections (16).5–8 Another study of patients who underwent vascular surgery indicated a significant (p < .05) increase in risk for cardiac ischemic events among persons with HbA1c >7% (17). Halkos and coauthors7,8 evaluated patients undergoing coronary artery bypass grafting and found that an elevated HbA1c was associated with greater mortality, higher risk of myocardial infarction, and more deep sternal wound infections.
These studies signify the potential value of obtaining preoperative HbA1c in order to more accurately stratify the intraoperative and postoperative potential morbidity and mortality of patients. However, our data indicated that HbA1c was checked preoperatively in just over half of our patients. It is not known whether the effective lowering of HbA1c during the period leading up to surgery might reduce hyperglycemia-associated risks, which requires future investigation. Since completion of this analysis, we have modified our institutional guidelines to incorporate a preoperative HbA1c test.
Although most of our patients had glucose measurements obtained in the preoperative and postanesthesia care unit settings, ideally 100% should have values checked to allow for interventions for any extreme values. However, the area identified as in most need of improvement is intraoperative glucose monitoring, which occurred in only one-third of cases overall. The proportion of cases in which glucose measurements were obtained increased with the length of the procedure. Nonetheless, there were patients who underwent long procedures who still did not have assessment of their glycemic status.
Glycemic control deteriorated over the course of the perioperative period and was higher in the postanesthesia care unit than in the preoperative phases of care. The clinical importance of this cannot be ascertained from this analysis. Developing protocols to treat intraoperative hyperglycemia will require provisions to ensure assessment of glucose levels. Our investigation of the infrequent POC BG measurements led to the discovery that only two POC BG devices were available for 17 operating suites. Increased availability of necessary equipment should aid in enhancing intraoperative glucose monitoring. Additionally, it was revealed that, due to whole body draping of the patient during some procedures, an extremity may not be available for a POC BG test. Ongoing work with collaborators in anesthesiology will seek to develop processes to overcome this limitation.
Another finding relevant to intraoperative glucose control is the choice of sample used to make the measurement. Most values obtained during the preoperative and postanesthesia care unit segments of care were POC BG levels; however, intraoperatively, there was no consistent technology used, with half of the cases having POC BG measured and the other half having glucose measured by arterial blood gas. Studies have shown that glucose levels differ when measured by POC BG versus other methods, with results also depending on level of oxygenation.20–23 When trying to establish tight glucose control, these differences in sampling may have a substantial impact on patient care. Many patients undergoing routine elective surgery do not experience clinically significant hemodynamic compromise, and POC BG measurements may provide a reasonable estimate of glucose control. However, because there is a level of error associated with POC BG testing, any aberrant measurements should be checked with a standard laboratory test similar to protocols established for inpatients. Agreement needs to be established on the optimal method for intraoperative glucose monitoring. Ideally, the same method should be applied throughout all phases of perioperative care so that glucose levels can be compared.
Perioperative glycemic control has been studied in both cardiac and noncardiac patients, but studies are limited on efficacy of actual intraoperative glycemic control. Limited evidence supports tight glycemic control intraoperatively, although findings are not consistent.24,25 Intraoperative glucose levels were checked in a minority of our patients, which may have delayed potential treatment of hyperglycemia and led to elevated BG levels postoperatively. Therefore, we are in the process of developing standardized intraoperative guidelines to address and resolve these deficiencies in glucose monitoring and to standardize insulin treatment during the perioperative period.
There are some limitations of our findings. First, although unlikely, it is possible that POC glucose measurements were obtained but not recorded. Furthermore, no definite conclusions regarding the level of intraoperative glycemic control or treatment effectiveness of hyperglycemia can be made in our patient population, because some glucose data were missing. Third, the analysis focused strictly on outpatients undergoing elective procedures, and thus our results cannot be generalized to diabetes patients undergoing emergent procedures or to those having surgery as inpatients. Fourth, we did not examine possible intraoperative contributors to hyperglycemia (e.g., use of dextrose-containing fluids or administration of steroids). Such confounders should be part of future analyses. Finally, these data are specific to our institution. However, the method presented here, where management is defined and segmented according to different phases of perioperative care, can serve as a model for others to follow when studying the quality of care in the surgical patient.
This analysis has led to the formation of an institutional multidisciplinary team empowered to standardize the care of outpatients with diabetes undergoing elective surgical procedures to include the need for preoperative medical evaluation (lacking in many of our patients) and a requirement to obtain an HbA1c measurement. This process also included a review and revision of patient education materials provided to patients preoperatively and standardization of glucose monitoring frequency. Once approved by the organization, the impact of these standards of care will be evaluated.
Conclusion
This analysis provided details on the characteristics of a patient population with diabetes undergoing surgery and also provided an overview of their perioperative management. These data have allowed us to identify areas to target for improvement. Protocols need to be developed to minimize the postoperative rise in glucose. As the prevalence of diabetes continues to rise, more cases will likely be encountered in the surgical population, and improved perioperative glucose assessment and monitoring may help to treat these patients more appropriately.
Glossary
- (BG)
blood glucose
- (HbA1c)
hemoglobin A1c
- (POC)
point of care
- (SD)
standard deviation
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States Atlanta: U.S. Department of Health and Human Services. 2011 Centers for Disease Control and Prevention; 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 23, 2013. [Google Scholar]
- 2.DiNardo M, Donihi AC, Forte P, Gieraltowski L, Korytkowski M. Standardized glycemic management and perioperative glycemic outcomes in patients with diabetes mellitus who undergo same-day surgery. Endocr Pract. 2011;17(3):404–411. doi: 10.4158/EP10316.OR. [DOI] [PubMed] [Google Scholar]
- 3.Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, Hudson M, Mendoza J, Johnson R, Lin E, Umpierrez GE. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care. 2010;33(8):1783–1788. doi: 10.2337/dc10-0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg. 2013;257(1):8–14. doi: 10.1097/SLA.0b013e31827b6bbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dronge AS, Perkal MF, Kancir S, Concato J, Aslan M, Rosenthal RA. Long-term glycemic control and postoperative infectious complications. Arch Surg. 2006;141(4):375–380. doi: 10.1001/archsurg.141.4.375. [DOI] [PubMed] [Google Scholar]
- 6.Feringa HH, Vidakovic R, Karagiannis SE, Dunkelgrun M, Elhendy A, Boersma E, van Sambeek MR, Noordzij PG, Bax JJ, Poldermans D. Impaired glucose regulation, elevated glycated haemoglobin and cardiac ischaemic events in vascular surgery patients. Diabet Med. 2008;25(3):314–319. doi: 10.1111/j.1464-5491.2007.02352.x. [DOI] [PubMed] [Google Scholar]
- 7.Halkos ME, Lattouf OM, Puskas JD, Kilgo P, Cooper WA, Morris CD, Guyton RA, Thourani VH. Elevated preoperative hemoglobin A1c level is associated with reduced long-term survival after coronary artery bypass surgery. Ann Thorac Surg. 2008;86(5):1431–1437. doi: 10.1016/j.athoracsur.2008.06.078. [DOI] [PubMed] [Google Scholar]
- 8.Halkos ME, Puskas JD, Lattouf OM, Kilgo P, Kerendi F, Song HK, Guyton RA, Thourani VH. Elevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2008;136(3):631–640. doi: 10.1016/j.jtcvs.2008.02.091. [DOI] [PubMed] [Google Scholar]
- 9.Doenst T, Wijeysundera D, Karkouti K, Zechner C, Maganti M, Rao V, Borger MA. Hyperglycemia during cardiopulmonary bypass is an independent risk factor for mortality in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2005;130(4):1144. doi: 10.1016/j.jtcvs.2005.05.049. [DOI] [PubMed] [Google Scholar]
- 10.Estrada CA, Young JA, Nifong LW, Chitwood WR., Jr Outcomes and perioperative hyperglycemia in patients with or without diabetes mellitus undergoing coronary artery bypass grafting. Ann Thorac Surg. 2003;75(5):1392–1399. doi: 10.1016/s0003-4975(02)04997-4. [DOI] [PubMed] [Google Scholar]
- 11.Guvener M, Pasaoglu I, Demircin M, Oc M. Perioperative hyperglycemia is a strong correlate of postoperative infection in type II diabetic patients after coronary artery bypass grafting. Endocr J. 2002;49(5):531–537. doi: 10.1507/endocrj.49.531. [DOI] [PubMed] [Google Scholar]
- 12.McGirt MJ, Woodworth GF, Brooke BS, Coon AL, Jain S, Buck D, Huang J, Clatterbuck RE, Tamargo RJ, Perler BA. Hyperglycemia independently increases the risk of perioperative stroke, myocardial infarction, and death after carotid endarterectomy. Neurosurgery. 2006;58(6):1066–1073. doi: 10.1227/01.NEU.0000215887.59922.36. [DOI] [PubMed] [Google Scholar]
- 13.Gandhi GY, Nuttall GA, Abel MD, Mullany CJ, Schaff HV, Williams BA, Schrader LM, Rizza RA, McMahon MM. Intraoperative hyperglycemia and perioperative outcomes in cardiac surgery patients. Mayo Clin Proc. 2005;80(7):862–866. doi: 10.4065/80.7.862. [DOI] [PubMed] [Google Scholar]
- 14.Ramos M, Khalpey Z, Lipsitz S, Steinberg J, Panizales MT, Zinner M, Rogers SO. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591. doi: 10.1097/SLA.0b013e31818990d1. [DOI] [PubMed] [Google Scholar]
- 15.Vilar-Compte D, Alvarez de Iturbe I, Martín-Onraet A, Pérez-Amador M, Sánchez-Hernández C, Volkow P. Hyperglycemia as a risk factor for surgical site infections in patients undergoing mastectomy. Am J Infect Control. 2008;36(3):192–198. doi: 10.1016/j.ajic.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125. doi: 10.3748/wjg.15.4122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akhtar S, Barash PG, Inzucchi SE. Scientific principles and clinical implications of perioperative glucose regulation and control. Anesth Analg. 2010;110(2):478–497. doi: 10.1213/ANE.0b013e3181c6be63. [DOI] [PubMed] [Google Scholar]
- 18.Nassar AA, Boyle ME, Seifert KM, Beer KA, Apsey HA, Schlinkert RT, Stearns JD, Cook CB. Insulin pump therapy in patients with diabetes undergoing surgery. Endocr Pract. 2012;18(1):49–55. doi: 10.4158/EP11157.OR. [DOI] [PubMed] [Google Scholar]
- 19.Sato H, Carvalho G, Sato T, Lattermann R, Matsukawa T, Schricker T. The association of preoperative glycemic control, intraoperative insulin sensitivity, and outcomes after cardiac surgery. J Clin Endocrinol Metab. 2010;95(9):4338–4344. doi: 10.1210/jc.2010-0135. [DOI] [PubMed] [Google Scholar]
- 20.Pitkin AD, Rice MJ. Challenges to glycemic measurement in the perioperative and critically ill patient: a review. J Diabetes Sci Technol. 2009;3(6):1270–1281. doi: 10.1177/193229680900300606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rice MJ, Pitkin AD, Coursin DB. Review article: glucose measurement in the operating room: more complicated than it seems. Anesth Analg. 2010;110(4):1056–1065. doi: 10.1213/ANE.0b013e3181cc07de. [DOI] [PubMed] [Google Scholar]
- 22.Desachy A, Vuagnat AC, Ghazali AD, Baudin OT, Longuet OH, Calvat SN, Gissot V. Accuracy of bedside glucometry in critically ill patients: influence of clinical characteristics and perfusion index. Mayo Clin Proc. 2008;83(4):400–405. doi: 10.4065/83.4.400. [DOI] [PubMed] [Google Scholar]
- 23.Tang Z, Louie RF, Payes M, Chang KC, Kost GJ. Oxygen effects on glucose measurements with a reference analyzer and three handheld meters. Diabetes Technol Ther. 2000;2(3):349–362. doi: 10.1089/15209150050194215. [DOI] [PubMed] [Google Scholar]
- 24.Subramaniam B, Panzica PJ, Novack V, Mahmood F, Matyal R, Mitchell JD, Sundar E, Bose R, Pomposelli F, Kersten JR, Talmor DS. Continuous perioperative insulin infusion decreases major cardiovascular events in patients undergoing vascular surgery: a prospective, randomized trial. Anesthesiology. 2009;110(5):970–977. doi: 10.1097/ALN.0b013e3181a1005b. [DOI] [PubMed] [Google Scholar]
- 25.Gandhi GY, Murad MH, Flynn DN, Erwin PJ, Cavalcante AB, Bay Nielsen H, Capes SE, Thorlund K, Montori VM, Devereaux PJ. Effect of perioperative insulin infusion on surgical morbidity and mortality: systematic review and meta-analysis of randomized trials. Mayo Clin Proc. 2008;83(4):418–430. doi: 10.4065/83.4.418. [DOI] [PubMed] [Google Scholar]


