Providers in all settings are increasingly aware of the need to focus on transitional care needs and services across health care settings to improve quality of life, maintain optimal health, and prevent unnecessary hospitalizations. Homecare is an essential piece of the transitional care puzzle, especially in providing services to support older adults with chronic co-morbid conditions to remain at home safely with optimal health and psycho-social well-being. Homecare is essential in bridging the gap from acute hospital care to home; however, little is known about the needs of older adults after discharge from homecare. Our study investigated the perceptions of older adults with chronic health conditions after discharge from home care regarding their daily activities and health care needs and identified how these needs were met.
Due to increasing co-morbidities in the aging population and the high cost of hospitalization, it is critical to address the continuing care needs of patients in the community after discharge from homecare and to prevent problems such as re-hospitalization. It is estimated that by 2050, there will be 80 million people 65 or older, which is more than double the projected 2010 rate of 40 million older adults (Vincent & Velkoff, 2010). The majority of older adults have at least one chronic health condition and two thirds of Medicare homecare beneficiaries have two or more diseases (McLaughlin, Connell, Heeringa, Li, & Roberts, 2010; U.S. Census Bureau., 2008). The estimated rise in the number of older adults, combined with the increasing number of chronic health conditions with aging, suggest that healthcare management and community-based care will be paramount issues in the coming years. In fact, it is already established that a higher proportion of health care dollars is spent on care of the elderly (Agency for Healthcare Research and Quality (AHRQ), 2006). At present, the rising costs of health care have led to legislation that improves care coordination for chronically ill persons with an emphasis on community-based care (Crabtree et al., 2010; Kocher, Emanuel, & DeParle, 2010).
Homecare is an affordable way to meet the needs of older adults (National Association for Home Care & Hospice, 2010); however, to reimburse homecare, Medicare requires patients to be homebound with intermittent skilled services (Lehning & Austin, 2010). When a patient is no longer homebound, Medicare coverage must be discontinued or homecare agencies risk fraud charges. On average, Medicare patients receive intermittent services over a 31 day period. This short time period results in the discharge of some patients before outcomes are improved or even stabilized (Armstrong, Stolee, Hirdes, & Poss, 2010). Re-hospitalization is a costly adverse event estimated at $27 billion for Medicare patients alone (Dartmouth Atlas Project & PerryUndem Research & Communications, February 2013) . Patients discharged from homecare are potential key informants regarding the type and amount of ongoing services that could prevent rehospitalization and optimize quality of life.
Aims and Methods
The aim of the study was to investigate the perceptions of chronically-ill, older adults recently discharged from homecare about their ongoing daily activities and health needs and how these were addressed. After approval by the University and Home Health Care System Institutional Review Boards, semi-structured interviews were conducted with 30 older adults within two to six weeks after discharge from a Midwestern urban homecare agency. Older adults for this study represent a convenience sample of the first 30 patients discharged from home care that met the inclusion criteria and agreed to participate in the study. Criteria for selection included 65 years of age or older, had a primary diagnosis of a chronic illness as the reason for homecare, received skilled care, lived in the community and within the geographical region serviced by the homecare agency, were able to speak and understand English, and were mentally and physically capable to participate in the study. Capability to participate in the study was based on the discharge OASIS assessment and judgment of the home care clinician. Homecare patients with post-surgical care as the primary reason for homecare were excluded. A semi-structured interview guide was used during a single session conducted in the participant's home by a research assistant with prior home care experience. Questions focused on the reason for homecare, daily life after homecare, ongoing needs and services after homecare discharge, and additional services that may be helpful. The interviews were audio taped and transcribed for analysis in NVivo 10 qualitative software. Criteria for trustworthiness of results included in this study were line by line coding using, review of codes and categories by an investigator experienced in qualitative analysis (Westra), and multiple team meetings with all investigators to review the analysis based on the emerging themes and supporting quotations (Polit & Beck, 2008).
Study Limitations
This study was limited to one Midwestern homecare agency as well as a homogenous population in terms of race/ ethnicity, gender, and economic status. Due to these limitations, findings may not be generalizable beyond this study.
Results
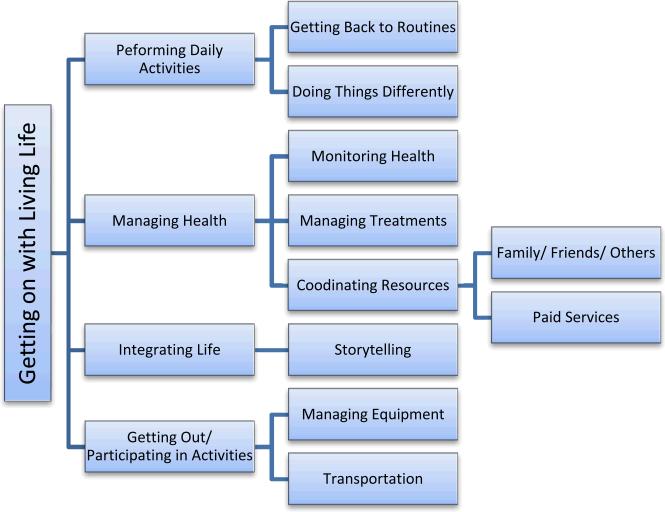
Participants were Caucasian (n=30) and predominantly female (n=27). Primary reasons for homecare were congestive heart failure (n = 9), other cardiac/ circulatory problems (n = 5), diabetes (n = 5), chronic respiratory diseases (n = 4), hypertension (n=3) and other chronic conditions (n=4). The overall experience of participants after discharge from homecare services were captured in the phrase getting on with living life. Two major themes were identified: getting around at home and expanding life beyond self and home. Getting around at home included two subthemes: performing daily activities and managing health. Expanding life beyond self and home required integrating the past and present circumstances and getting out of the house to participate in activities. Participants got on with living life through use of a variety of strategies shown in Figure 1.
Figure 1.
Strategies Used by Older Adults to Get on With Living Life
As participants got stronger and were able to get around at home and out into the community, most expressed that they were getting on with living life. For some, this meant living life as they had before receiving homecare. For others, it was establishing a new normal due to health and functional limitations, “I never got to the point that I was at...so I'm still using the walker and I still have good days and I have bad days.” Some said they didn't expect to ever get better, “I'm existing.” Some participants identified that they gradually improved by performing daily activities and managing their health. Getting on with living life also meant expanding their lives beyond their immediate settings and home environment by integrating their past and present circumstances through story telling. It also involved getting out of the home and participating in community activities. Getting on with living life required taking action by changing routines, monitoring health, and using resources such as friends/family, services, and equipment.
Performing Daily Activities
Performing daily activities included a variety of tasks. Three activities, however, were most prominent: bathing, preparing meals, and laundry/ house cleaning. Bathtubs were identified as the most unsafe place in the home due to fear of falling. “I have a chair in my bathtub but who is going to lift their leg over the edge of the bathtub to get to it and I am not going to take chances. I am not getting up and getting into a bathtub but just getting a sponge bath.” Two strategies for bathing included having help from either paid aides or family members, or using assistive equipment. One woman stated, “[I have] my bath lady.” Other older adults described assistive equipment such as hand or grab bars, shower chairs, and hand sprayers. Even with equipment, however, getting in and out of the tub was problematic. “The only thing that I have a problem with, I love to take a bath. And I can't get in and out of the tub anymore. So I have to take a shower, and I'm very careful when I go in because this knee has buckled on me a few times.” Bathing was one of life's pleasures for some; however, fear of falling resulted in changing to a shower or sponge bath.
Many older adults no longer prepared large meals as they had in the past. Instead, they managed by eating fewer meals, having help with food preparation, cooking meals already prepared by others such as a daughter or other family member, purchasing frozen foods, or having meals delivered. Even when they could no longer cook, some described helping with what little they could do in the kitchen. A husband stated, “She does help with the cooking, if we are making meat loaf or something. I will bring out the ingredients. I will chop the stuff like onions, give her the hamburger and she mixes it up.” Some participants were fortunate to have family living nearby who prepared meals for them. “My son's wife makes meals and then she saves some up for me and sends it over. We freeze them up over here. Otherwise I make a grocery list and they.... pick up these packaged foods.” While assistive equipment was helpful for getting around, at times, equipment also interfered with activities. For example, several older adults who received continuous oxygen noted concerns about cooking because they had received conflicting information about whether they could cook safely while using their oxygen.
Several participants described needing considerable help with laundry and cleaning. When laundry facilities were on the main floor or if participants had help, they could manage. Only one participant indicated she could go down stairs to do laundry. For some, declining function interfered with housework. “A lady comes in to do the laundry and cleaning, because I'm not supposed to do laundry because of the oxygen. And the cleaning was getting difficult too.” A few were no longer able to do any cleaning. “[My daughter] cleans my bathroom and cleans my room and does my laundry. I don't do anything, I hardly do anything.” However, some participants who could no longer do laundry or cleaning independently described themselves as still “able” by doing what they could with help from others. “I can fold my clothes if someone helps with the rest.” One participant noted that at some point, most older adults would no longer be able to perform these tasks without help, so it was important to plan for that time.
Managing Health
Participants in this study described a number of ongoing health needs and several strategies for managing their health including monitoring their health and taking action.
Monitoring Health
Health was monitored mainly by the older adults in this study and their families. Participants observed health-related signs and symptoms such as their blood sugar, weight, blood pressure, and pain; they took actions based on their observations. Some followed previous instructions from health care providers while others used their own judgment about managing their health. “They had me on 10 [units of insulin] and I said, ‘That's not doing anything at all.’ So now I've got it at 14 and it is much better... I don't like [my blood sugar] below 100. I like it over, well even 125 or up. I know they say, oh, 80 or 90 is good. But no, that's too low for me.” They also monitored their health by improved functioning with or without supportive devices. As one woman noted, “I now walk with a cane instead of a walker.” Others noted improvement by the increasing distance that they could walk. For others, requiring less help was a sign of getting on with living life.
Managing Treatments
The major health challenges for many older adults were managing medications and exercising. Managing medications was universal among participants and the majority indicated they managed their own medications, primarily through the use of pill boxes. “I get mine together my own self for two weeks at a time. I am capable but I am on the road to 90.” For some, the inability to properly manage medications was related to poor eyesight, cognitive abilities, or the complexity of medications. “My family thought there were times that I was missing medications and that was getting to be a little stressful for them. And I take so many that it was...I think there's 23 or something like that. So it's a bunch.” Participants needed help when they had numerous medications, complex regimens, or frequent medication changes. One participant stated, “Now that's been a real complication [to manage my medications], because they do change them, especially my warfarin...They'll change that, I go for INR. Well usually I was going every week, now I go every two weeks. That's real hard to do, because they all look alike. Some of them look so much alike that I can't...I think, oh did I use that? Then I have to go look at my bottle, look at the milligrams and all that.”
Participants frequently spoke about receiving therapy during homecare and the challenge of continuing exercises after discharge. They had written lists of exercises that they posted in visible places. “I still do my exercises because I got them [list of exercises] on the counter out there.” Simple exercises were more likely to be performed when paired with other activities such as morning routines or watching television, “we have breakfast and we go in and do morning exercises.” Understanding the need for exercises and how to perform them didn't equal behavior change. “Well, I've just gotten more crippled up....the exercises, once you get going on it, you're going to have to stay with it; and I know that now but I didn't realize how badly, how fast it [being crippled] comes back.” Several participants noted that going to an exercise class was helpful physically as well as socially. “We have more fun actually waiting for the class to start than we actually do sometimes in the class. Sometimes it gets a little rowdy in the class.”
Coordinating Care
Care coordination was a potential or actual need for many participants due to the multitude of medications, appointments, and physical help needed to stay at home safely. Most older adults, with the help of their families, were able to coordinate their own care. However, those living alone or those with more complex health problems, treatments or functional disabilities required careful coordination of resources. One person living alone stated a former assistant hired through an advertisement in the paper had taken her credit card so she fired the assistant. Another woman with complex care was “kept busy” with managing appointments. “I go to a hematologist every three weeks and I go for an INR...well it depends on what my readings are. But that's usually at least once a month. And then my regular physician, I've been working with kidney and bladder problems...I went there, maybe six weeks ago.” Several people noted they anticipated needing more help in the future as they got older and a few wanted additional services now, particularly more therapy and help with following diets. Coordinating care went beyond meeting needs at home; it also involved coordinating transportation for appointments, shopping and getting out into the community.
Expanding Life
Getting on with living life for participants meant expanding their lives beyond their immediate circumstances and home environment. They expanded their lives by integrating their current circumstances with their pasts though storytelling, getting out of their homes, and participating in activities. Participants who were able to get out of their homes and engage in usual activities expressed feeling better and having a sense of freedom.
Integrating Life
Telling stories connected participants beyond the boundaries of time and place; integrating their current life with previous experiences. Pictures, memorabilia, newspapers, and familiar neighborhoods prompted story telling during interviews. Their stories depicted their former lives in the context of family, previous jobs, social events, and even the deaths of family and friends. When looking at pictures, one woman described a cabin previously owned, “We had fun. The average was 17 people to cook for on the weekends. So it was fun and I am glad, I wouldn't change a thing. We didn't make any mistakes.” Participants appeared to be re-living and attaching meaning to enjoyable and challenging times in their lives. Story telling connected their current circumstances with their past experiences; getting beyond the present moment and getting on with living life, in a transcendent sense.
Getting Out and Participating in Activities
Getting out of the house was experienced as a sense of “freedom” and a form of getting back to normal life. Moving from “homebound” status to participating in usual activities was a gradual process. After homecare, many participants had to regain strength and either learn to use new equipment or graduate from use of equipment to get out. Frequently, participants in this study used equipment, particularly walkers, to assist with mobility. While walkers were essential to getting around safely, they interfered with getting out in to the community. One participant commented, “I'd rather stay at home than go out in public with a walker.” Others noted that walkers were clunky or made it difficult to ask for help with transportation from family or friends because of getting the walker in their car. A few noted that not every walker is the same and having a lighter weight walker was better for getting around as they were able to manage the equipment more easily. Oxygen was also mentioned as being cumbersome and limiting.
Getting out of the home and participating in the community was possible when “Medicare restrictions” were removed and transportation resources were adequate. Several participants commented about being restricted with homecare. “I enjoyed homecare....except I couldn't go [out] like I wanted to.” Transportation is essential for getting out into the community for activities such as shopping, going to health care appointments, church, and social events. Many participants no longer drove a car; instead, they required other transportation resources. When asked about driving, one woman stated, “I no longer drive, because my legs, well, give me a little jolt every once in a while. I don't feel as though I'm trusting them.” Family and friends frequently provided transportation. Some participants expressed concerns about imposing on others for aid with transportation because they “didn't want to be a bother”. Those who had multiple resources described “backup plans;” this meant that if one family member wasn't available, they identified someone else they called so they could still get out for appointments, shopping, or errands. Others used senior transportation services for grocery shopping or going to the pharmacy. Some seniors in this study were unfamiliar with or lacked experience with transportation resources or perceived it as inconvenient or inadequate to meet their needs. Compared to driving their own car, one participant stated, “you've got to pay them and you have to order them to come and pick you up a day ahead or something.” In the past, driving provided the freedom to come and go when and where they pleased, such as shopping from store to store. Now, even with help from others, participating in some activities remained limited.
Discussions and Conclusions
Overall, the majority of participants in this study were getting on with living life after discharge from homecare. They described performing daily activities and managing their health as essential for getting around at home. Frequently mentioned daily activities included bathing, preparing meals, and household management. Many participants described the bathtub as the most unsafe place in the home; this was related to their fear of falling. A systematic risk of the environment, particularly bathing facilities, is part of multi-factor interventions to prevent falls and keep older adults at home safely (Chase, .Mann, Wasek, & Arbesman, 2012). Our results of support needs for elderly are similar to those in other studies (Watkins, Hall, & Kring, 2012); novel however, is the ongoing need for services and support after home care discharge.
Mobility was a pervasive issue cutting across themes. Walkers frequently were used for getting around at home and out of the house. Exercising was a major issue for gaining strength and balance which influenced mobility. Clearly, finding ways to help older adults continue to gain or retain strength and balance in order to be mobile is essential for staying at home. Improvement in mobility (ambulation/ locomotion) also is one of CMS’ outcomes for comparing the quality of agencies (Centers for Medicare & Medicaid Services, 2012).
Mobility entailed more than the individual moving freely in their home; it also involved getting around via transportation outside the home. Knowing about transportation resources, providing assistance for those who are hesitant to use them, evaluating the appropriateness of equipment such as walkers and oxygen, and having backup plans can improve the ability of older adults to get out and participate in community activities (Diaz Lobato & Mayoralas Alises, 2012; Holley, 2007).
While the majority of participants could manage medications themselves, some identified several concerns or issues that influenced their ability to safely take their medications. These included cognitive functioning, visual impairments, the number of medications, and challenges when medication regimens changed. They also noted difficulties with the number of providers prescribing medications, needing help to prevent duplicate medications, and taking them at optimal times. Many older adults used pill boxes, but some had unsafe routines such as taking medications out of multiple bottles many times per day that could result in missed doses or overdose. Managing medication safely found in this study is consistent with other research in which increasing complexity requires more intense management (Dierich et al., 2008) and pill boxes are effective strategies for managing medications (Marek & Antle, 2008).
Emerging models of Medicare payment may lead to better outcomes such as reduction of rehospitalization and improve quality of life. Medical home and accountable care organizations are payment models in which a health system is responsible for care of a population across settings. Providing the right care for the right amount of time in the right setting can lead to better quality and reduction of unnecessary costs. Therefore interprofessional care delivery, ongoing support services to remain at home such as housekeeping, and removing homebound could result in better outcomes for getting on with living life. The return to a healthier life might be easier and faster if older adults began getting out while still receiving homecare. If older adults were able to get out while receiving home care, potential barriers such as transportation, usability of equipment, and modifications needed to previous routines could be identified earlier and immediately be addressed by skilled and knowledgeable homecare professionals.
Overall, participants in this study were successfully getting on with living life after discharge from homecare. Their stories identified key areas which homecare providers should consider as part of discharge planning and transitional care.
Recommendations
As the investigators analyzed and synthesized findings for this study, we kept a list of recommendations from interviews. These recommendations were validated by the team, particularly those working in homecare. Recommendations are listed in Table 1 for assessing ongoing needs and services after discharge.
Table 1.
Recommendations for Transitional Care After Home Care Discharge
|
Performing Daily Activities
| |
| 1. | Discuss with older adults their fears of falling and how that influences the need to change ways of managing at home. |
| 2. | Evaluate previous bathing habits, particularly taking a tub bath, and whether there are options for ongoing support of tub baths. |
| 3. | Determine the nutritional value of foods with limited ability to prepare meals, particularly if there is a specific diet such as low sodium. |
| 4. | Provide a list of household and personal care resources for ongoing needs. |
|
Managing Health | |
| 1. | Assess older adults' vision and ability to read and follow instructions such as taking medications or exercising. |
| 2. | Evaluate whether equipment is optimal for getting around at home and getting out. |
| 3. | Provide nursing case management after discharge from home care when multiple providers or multiple or complex medications or treatments are involved, and assistance is needed to manage safely at home. |
| 4. | Investigate new payment methods (i.e. accountable care organizations) to support a multi-disciplinary approach after home care that includes physical / occupational therapy and nutritionists and focuses on lifestyle changes to maintain health. |
| 5. | Consider the use of technology such as video games to support exercising. |
| 6. | Assure follow up appointments are scheduled, including the need for transportation and the inclusion of someone during appointments to support ongoing health management activities |
| 7. | Follow up to determine barriers and supports for following treatment recommendations. |
|
Integrating Life through Storytelling | |
| 1. | Assess social contacts, particularly those in which older adults feel comfortable sharing their stories. |
| 2. | Take time to ask and listen to stories as it enables older adults to relive their lives beyond the boundaries of time and place. |
| 3. | Arrange for volunteers home visiting for socialization that encourages story telling |
|
Getting Out and Participating in Activities | |
| 1. | Provide advice on equipment such as walkers and oxygen to minimize equipment as barriers for getting out. |
| 2. | Assess older adults' transportation needs for a variety of reasons - going to medical appointments, shopping, going to church, and socialization. |
| 3. | Assess backup plans for transportation if family is not available |
| 4. | Provide written materials for public transportation. |
| 5. | Assess whether assistance is needed for using public transportation the first time to gain confidence in using public transportation. |
| 6. | Provide therapeutic support for those experiencing loss of power and autonomy when no longer able to drive and get out as they had in the past. |
Acknowledgments
This publication was supported by Grant Number 1UL1RR033183 from the National Center for Research Resources (NCRR) of the National Institutes of Health (NIH) to the University of Minnesota Clinical and Translational Science Institute (CTSI). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CTSI or the NIH. The University of Minnesota CTSI is part of a national Clinical and Translational Science Award (CTSA) consortium created to accelerate laboratory discoveries into treatments for patients.
Footnotes
Conflicts of Interest and Source of Funding:
There are no conflicts of interest for any of the authors.
Contributor Information
Bonnie L. Westra, University of Minnesota, School of Nursing, Minneapolis, MN, USA.
Nadine Paitich, HealthEast Home Care, HealthEast Care System, St. Paul, MN, USA.
Dawn Ekstrom, HealthEast Home Care, HealthEast Care System, St. Paul, MN, USA.
Susan C. Mehle, Research Department, HealthEast Care System, St. Paul, MN, USA.
Maggie Kaeding, Research Department, HealthEast Care System, St. Paul, MN, USA.
Sajeda Abdo, University of Minnesota, Institute of Health Informatics, Minneapolis, MN, USA.
Karen Monsen, University of Minnesota, School of Nursing.
References
- Agency for Healthcare Research and Quality (AHRQ) [June 3, 2013];The High Concentration of U.S. Health Care Expenditures: Research in Action. 2006 (19) from http://www.ahrq.gov/research/findings/factsheets/costs/expriach/index.html.
- Armstrong JJ, Stolee P, Hirdes JP, Poss JW. Examining three frailty conceptualizations in their ability to predict negative outcomes for home-care clients. Age & Ageing. 2010;39(6):755–758. doi: 10.1093/ageing/afq121. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services [August 23, 2012];Medicare: Home Health Compare. 2012 from http://www.medicare.gov/HHCompare. [Google Scholar]
- Chase CA, Mann K, Wasek S, Arbesman M. Systematic review of the effect of home modification and fall prevention programs on falls and the performance of community-dwelling older adults. American Journal of Occupational Therapy. 2012;66(3):284–291. doi: 10.5014/ajot.2012.005017. doi:10.5014/ajot.2012.005017. [DOI] [PubMed] [Google Scholar]
- Crabtree BF, Nutting PA, Miller WL, Stange KC, Stewart EE, Jaen CR. Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Annals of Family Medicine. 2010;8(Suppl 1):S80–90. doi: 10.1370/afm.1107. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medl&AN=20530397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dartmouth Atlas Project, & Perry Undem Research & Communications . The Revolving Door: A Report on U.S. Hospital Readmissions. () Robert Wood Johnson Foundation; Princeton, NJ: Feb, 2013. [Google Scholar]
- Diaz Lobato S, Mayoralas Alises S. Mobility profiles of patients with home oxygen therapy. Archivos De Bronconeumologia. 2012;48(2):55–60. doi: 10.1016/j.arbres.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Dierich MT, Westra BL, Marek KD, Savik K, Oancea C, Holmes JH, Mueller CA. Defining medication complexity and its effect on outcomes in community dwelling elders receiving home care. AMIA ...Annual Symposium Proceedings / AMIA Symposium.AMIA Symposium. 2008 930. [PubMed] [Google Scholar]
- Holley UA. Social isolation: a practical guide for nurses assisting clients with chronic illness. Rehabilitation Nursing Journal. 2007;32(2):51–56. doi: 10.1002/j.2048-7940.2007.tb00152.x. [DOI] [PubMed] [Google Scholar]
- Kocher R, Emanuel EJ, DeParle NA. The Affordable Care Act and the future of clinical medicine: the opportunities and challenges. Annals of Internal Medicine. 2010;153(8):536–539. doi: 10.7326/0003-4819-153-8-201010190-00274. [DOI] [PubMed] [Google Scholar]
- Lehning AJ, Austin MJ. Long-term care in the United States: Policy themes and promising practices. Journal of Gerontological Social Work. 2010;53(1):43–63. doi: 10.1080/01634370903361979. doi:10.1080/01634370903361979. [DOI] [PubMed] [Google Scholar]
- Marek KD, Antle L. Medication management of the community dwelling older adult. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: 2008. AHRQ Publication No. 08-0043. () http://www.ahrq.gov/qual/nurseshdbk/: Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- McLaughlin SJ, Connell CM, Heeringa SG, Li LW, Roberts JS. Successful aging in the United States: Prevalence estimates from a national sample of older adults. Journal of Gerontology: Social Sciences. 2010;65(B):216–226. doi: 10.1093/geronb/gbp101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association for Home Care & Hospice [August 17, 2011];Basic Statistics About Home Care. 2010 from http://www.nahc.org/facts/10HC_Stats.pdf.
- Polit DF, Beck CT. Nursing research : Generating and assessing evidence for nursing practice. 8th ed. Lippincott, Williams & Wilkins; Philadelphia: 2008. [Google Scholar]
- Census Bureau US. [March 03, 2011];An older and more diverse nation by midcentury. 2008 from http://www.census.gov/newsroom/releases/archives/population/cb08-123.html.
- Vincent GK, Velkoff VA. Current Population Reports. U.S. Census Bureau; Washington, DC.: 2010. [June 03, 2013]. The next four decades, The Older Population in the United States: 2010 to 2050; pp. P25–1138. from http://www.census.gov/prod/2010pubs/p25-1138.pdf. [Google Scholar]
- Watkins L, Hall C, Kring D. Hospital to home: A transition program for frail older adults. Professional Case Management. 2012;17(3):117–125. doi: 10.1097/NCM.0b013e318243d6a7. [DOI] [PubMed] [Google Scholar]