Abstract
Purpose
As therapy for non-small cell lung cancer (NSCLC) patients becomes more personalized, additional tissue in the form of core needle biopsies (CNBs) for biomarker analysis is increasingly required for determining appropriate treatment and for enrollment into clinical trials. We report our experience with small-caliber percutaneous transthoracic (PT) CNBs for the evaluation of multiple molecular biomarkers in BATTLE (Biomarker-integrated Approaches of Targeted Therapy for Lung Cancer Elimination), a personalized, targeted therapy NSCLC clinical trial.
Methods
The medical records of patients who underwent PTCNB for consideration of enrollment in BATTLE, were reviewed for diagnostic yield of 11 predetermined molecular markers, and procedural complications. Univariate and multivariate analyses of factors related to patient and lesion characteristics were performed to determine possible influences on diagnostic yield.
Results
One hundred and seventy PTCNBs were performed using 20-gauge biopsy needles in 151 NSCLC patients screened for the trial. 82.9% of the biopsy specimens were found to have adequate tumor tissue for analysis of the required biomarkers. On multivariate analysis, metastatic lesions were 5.4 times more likely to yield diagnostic tissue as compared to primary tumors (p = 0.0079). Pneumothorax and chest tube insertion rates were 15.3% and 9.4%, respectively.
Conclusions
Image-guided 20-gauge PTCNB is safe and provides adequate tissue for analysis of multiple biomarkers in the majority of patients being considered for enrollment into a personalized, targeted therapy NSCLC clinical trial. Metastatic lesions are more likely to yield diagnostic tissue as compared to primary tumors.
Keywords: research biopsy, biomarker analysis, percutaneous transthoracic biopsy
INTRODUCTION
Lung cancer is the most common cause of cancer-related death for men and women and represents about 28% of all cancer deaths.1,2 Despite advances in cancer therapy, the overall 5-year survival rate remains poor with less than 30% of patients being eligible for curative resection at the time of diagnosis.3,4,5 Treatment advances for cancer therapy are now predicated on an understanding of the molecular basis of cancer which may provide the opportunity to develop novel treatment strategies. Since targeted agents are known to be effective against specific mutations, molecular characterization of the tumor and the development of prognostic and predictive biomarkers are critical to guiding clinical decision-making in the pursuit of personalized cancer therapy. As a result, tissue, sufficient not only for tumor classification by cytology, histology, but also molecular characteristics (e.g. epidermal growth factor receptor (EGFR) mutation, anaplastic lymphoma kinase (ALK) translocation), is important to determine whether standard chemotherapy versus targeted therapy would be the most appropriate treatment for the patients.6
Image-guided percutaneous transthoracic core needle biopsy (PTCNB) is a standard diagnostic procedure which is now being used to obtain tissue for research protocols where molecular biomarker analysis rather than histology is the ultimate goal.7–10 However, little has been written about the safety and adequacy of the techniques used for tissue acquisition in research biopsies.11,12,13 In addition, factors such as tumor histology and previous anti-cancer treatments, that could potentially influence the diagnostic yield in a research setting have not been studied. The BATTLE (Biomarker-integrated Approaches of Targeted Therapy for Lung Cancer Elimination) trial was the first completed prospective, biopsy-mandated, biomarker-based, adaptively randomized phase II clinical trial in patients with pretreated, advanced lung cancer.14 This study demonstrated for the first time that PTCNBs of non-small cell lung cancers (NSCLCs) could provide biomarker information that may be used to predict response to a particular targeted therapy. The purpose of this paper is to report on the safety and reliability of using image-guided small-caliber PTCNBs for multiple molecular marker analysis in patients with NSCLC being considered for enrollment in the BATTLE trial. We also analyzed the patient and biopsy-related factors to determine possible influences on diagnostic yield.
MATERIALS AND METHODS
This was a HIPPA compliant, subset analysis of patients who underwent PTCNB for consideration of enrollment in the BATTLE trial; the study was approved by the institutional review board, and we followed the recommendations of the Declaration of Helsinki for biomedical research. Of the total 324 patients who were biopsied in the BATTLE trial, 151 patients (not all of whom were randomized to treatment) underwent 170 PTCNBs and represent the subset of BATTLE patients analyzed in this study.14 Nineteen patients underwent a repeat biopsy: eighteen patients who were assigned to a treatment arm and progressed while on protocol underwent repeat biopsy for consideration of re-enrollment into the trial. The last patient underwent a second optional biopsy for investigational purposes of the protocol.
The medical records of these patients were reviewed for the following parameters: biopsy site, imaging findings, needle size, image-guidance, diagnostic yield, previous treatments, and procedural complications. Univariate and multivariate analyses of following factors were performed to determine possible influences on diagnostic yield: age, gender, tumor histology, history of previous radiation treatment to biopsied lesion, primary versus metastatic nature of the biopsied lesion, lesion depth from the pleura, lesion size (maximum diameter on computed tomography (CT) images with standard lung window settings), location and morphology, availability of a fluorodeoxyglucose positron-emission tomography/computed tomography (FDG-PET/CT) within 6 months prior to biopsy. A biopsy that yielded sufficient tumor tissue for evaluation of all 11 biomarkers required for enrollment in the protocol was considered a diagnostic biopsy. Lesion morphology was categorized as solid mass, consolidation (areas of parenchymal opacification obscuring underlying lung markings with or without air bronchograms), or cavitary lesion (presence of air-filled cavity within lung lesion). Bivariate analyses were conducted using Fisher’s exact tests to explore the association of diagnostic yield with several patient and lesion characteristics. A multivariate logistic regression was fitted to the data to investigate the presence of higher dimension associations (SAS 9.2, SAS Institute Inc., Cary, NC). A p-value ≤ 0.05 was considered statistically significant.
The BATTLE trial required patients to undergo a mandatory baseline biopsy consisting of at least 2 fresh PTCNBs prior to treatment randomization. The samples were assessed visually by the interventional radiologist (IR) performing the procedure, and if the initial two specimens were small or fragmented, additional samples were obtained if the size and location of the lesion permitted additional sampling in a safe manner.
The tumor tissue was immediately fixed in formalin and embedded in paraffin within 24-hours. A hematoxylin-and-eosin-stained histological section was used to assess the presence, quantity, quality and histological type of tumor tissue. Each histology section considered adequate for biomarker analysis had at least 200 malignant cells.14 Using at least 12 histology sections, the tumor tissue was tested for 11 different biomarkers: gene mutation analysis by polymerase chain reaction based sequencing for EGFR exons 18–21, KRAS codons 12, 13, and 61 and BRAF exons 11 and 15; two copy number analyses by fluorescent in situ hybridization of EFGR and Cyclin D1; and, six protein analyses (vascular endothelial growth factor (VEGF), VEGFR-2, retinoid X receptors (RXRs) α, β and γ, and Cyclin D1) by immunohistochemistry. Confirmation of the presence of adequate tumor tissue in the formalin-fixed and paraffin-embedded tissue specimens by histology examination was performed within 24–48 hours, and analysis of the 11 molecular biomarkers was performed, completed and reported within 14 days. Based on the molecular characteristics, patients were assigned to one of four biomarker groups (EGFR, KRAS/BRAF, VEGF or RXR/Cyclin D1) to receive different therapies (erlotinib, vandetanib, erlotinib and bexarotene or sorafenib).14
All PTCNB procedures were performed under CT guidance by a board-certified IR. Written informed consent for the procedure was obtained. Accepted coagulation parameters included platelet levels of at least 75 X 109L and an INR ≤1.5. All biopsies were performed using a coaxial technique which allowed acquisition of multiple biopsy samples using only one transgression through the pleura: an 18- or 19-gauge guide needle (Cook Inc., Bloomington IN) was inserted through the skin and directed to the periphery of the lesion; subsequently, a 20-gauge core biopsy needle (Quikcore, Cook Inc., Bloomington IN) was inserted through the guide needle, and samples obtained after CT confirmation of the needle tip’s position. Following the biopsy, serial inspiratory chest radiographs with the patient in an erect position were obtained over a three-hour observation period. A chest tube with a Heimlich valve was inserted if the pneumothorax size was >30% of lung volume, the pneumothorax increased in size, or patients experienced pain, dyspnea or a decrease in oxygen saturation. Patients who had chest tubes placed were treated as outpatients, returning the next day for chest tube removal.15 Patients with persistent air leaks or those with severe pain were admitted to the hospital for management.
RESULTS
All patients had a diagnosis of metastatic NSCLC and had been previously treated with chemotherapy (Table 1). All patients underwent PTCNB successfully and at least 2 PTCNBs of the tumor were obtained in each patient: 82.9% (n=141) of the biopsy samples had sufficient tissue for the required biomarker analysis. Univariate analyses showed biopsy of metastatic lesions were more likely to yield diagnostic tissue than biopsy of primary tumors (Table 2) (94.7% versus 76.9%; p = 0.0042). Biopsy of cavitary lesions were less likely to yield diagnostic tissue as compared to biopsy of masses or consolidations (50% versus 86.7% and 77.8%, respectively, p = 0.0315). The diagnostic yield was 73%, 84% and 84% for lesions <2 cm, 2–5 cm, and >5 cm in size, respectively; the differences in size were not statistically significant. There was no difference (p=0.54) in diagnostic yield between the cases that had a FDG-PET/CT within 6 months of biopsy versus those that did not. On multivariate logistic regression analysis, only one of the variables evaluated was found to be predictive: metastatic lesions were 5.4 times more likely to yield diagnostic tissue as compared to primary tumors (p = 0.0079).
Table 1.
Patient Demographics
| n (%) | ||
|---|---|---|
| Age (mean 61 years, range 34–81 years) | <50 | 31 (20.5) |
| 51–60 | 33 (21.9) | |
| 61–70 | 56 (37.1) | |
| >70 | 31 (20.5) | |
| Gender | Male | 86 (57) |
| Female | 65 (43) | |
| Ethnicity | Caucasian | 125 (82.8) |
| Hispanic | 6 (4) | |
| African American | 9 (6) | |
| Asian | 11 (7.2) | |
| Smoker | Current | 12 (8) |
| Former | 108 (71.5) | |
| Never | 31 (20.5) | |
| ECOG | 0 | 27 (17.9) |
| 1 | 101 (66.9) | |
| 2 | 23 (15.2) | |
| Total Patients | 151 (100) |
Table 2.
Influence of patient, lesion and biopsy variables on likelihood of obtaining diagnostic tissue sufficient for biomarker analyses: Univariate analysis
| Characteristic | Number of Biopsies, (n) | Diagnostic n, (%) | Non-Diagnostic n, (%) | P-value |
|---|---|---|---|---|
|
| ||||
| Size | 0.5842 | |||
| <2 cm | 11 | 8 (72.7) | 3 (27.3) | |
| 2–5 cm | 135 | 112 (82.9) | 23 (17.1) | |
| >5 cm | 24 | 21 (87.5) | 3 (12.5) | |
|
| ||||
| Lesion Biopsied | 0.0042 | |||
| Primary Tumor | 113 | 87 (77) | 26 (23) | |
| Metastatic Focus | 57 | 54 (94.7) | 3 (5.3) | |
|
| ||||
| History of Prior Radiation Therapy to the Lesion Biopsied | 0.5820 | |||
| Yes | 28 | 22 (78.6) | 6 (21.4) | |
| No | 142 | 119 (83.8) | 23 (16.2) | |
|
| ||||
| Lesion Morphology | 0.0315 | |||
| Mass/Nodule | 153 | 130 (84.9) | 23 (15.1) | |
| Consolidation | 9 | 7 (77.8) | 2 (22.2) | |
| Cavitation | 8 | 4 (50) | 4 (50) | |
|
| ||||
| Lesion Location | 0.1969 | |||
| Lung | 150 | 123 (82) | 27 (18) | |
| Hilum/Mediastinum | 8 | 6 (75) | 2 (25) | |
| Pleura | 12 | 12 (100) | 0 (0) | |
|
| ||||
| Lesion Depth | 0.1763 | |||
| 0–2 cm | 82 | 72 (87.8) | 10 (12.2) | |
| 2–4 cm | 66 | 53 (80.3) | 13 (19.7) | |
| >4 cm | 22 | 16 (72.7) | 6 (27.3) | |
|
| ||||
| Tumor Histology | 0.3427 | |||
| NSCLC-NOS | 31 | 28 (90.3) | 3 (9.7) | |
| NSCLC-SCC | 26 | 20 (76.9) | 6 (23.1) | |
| NSCLC-Adenocarcinoma | 103 | 86 (83.5) | 17 (16.5) | |
| Other | 10 | 7 (70) | 3 (30) | |
|
| ||||
| PET-CT within 6 months | 0.5391 | |||
| Yes | 76 | 65 (85.5) | 11 (14.5) | |
| No | 94 | 76 (80.8) | 18 (19.2) | |
NSCLC-non-small cell lung cancer; SCC-squamous cell carcinoma; NOS-not otherwise specified
Review of the imaging data in the 29 cases with non-diagnostic samples (Table 3) revealed that tissue yield in 23 of these cases potentially could have been improved. Sampling error was identified in 9 cases where a different portion of the lesion should have been sampled (Figure 1). Lesion selection was not optimal in fourteen cases: five cases demonstrated a change to the morphology of the lesion following systemic or radiation therapy with three lesions becoming smaller and two lesions obscured by the development of adjacent consolidative changes or pneumonitis in the lung parenchyma. The remaining nine cases had either a large lesion or multiple lesions. In these patients, it is possible that presence of a recent FDG-PET/CT could have helped in selecting the best lesion (lesion with highest standardized uptake value in patients with multiple lesions) or the most viable area within a large lesion for biopsy. A review of the images for the last six cases with non-diagnostic biopsies revealed that both lesion selection and biopsy technique were appropriate. In these patients, we believe that on-site cytopathologic evaluation of fine-needle aspirations or touch-preparations of core samples has the potential to improve the diagnostic yield. None of the 14 cases in which lesion selection was identified as the error category had a FDG-PET/CT within 6 months of the biopsy. Similarly, 4 cases of sampling error and 3 cases of unknown error had not had a FDG-PET/CT within 6 months of the biopsy.
Table 3.
Patients with Inadequate Tissue Samples
| No. of Patients | Descriptive Reasons for Inadequate Tissue Sampling | Error Category | Recommendations |
|---|---|---|---|
| 14 | Large mass without recent PET/CT (n=4). Multiple lesions without recent PET/CT (n=5). Lesion response to therapy (radiation or chemotherapy) without recent PET/CT (n=5). |
A: Lesion selection problem | Recent functional imaging (PET/CT) would improve lesion selection:
|
| 9 | Area sampled did not show FDG activity on pre-biopsy PET/CT (n=3). Area sampled did not show contrast enhancement on pre-biopsy contrast-enhanced CT (n=3). Needle not in lesion, edge of lesion biopsied (n=3). |
B: Sampling error | Pre-biopsy review of available cross-sectional and preferably functional imaging (PET/CT) is essential to procedural planning. Areas suspected to have the most viable tumor should be targeted. |
| 6 | Needle in appropriate position within the lesion-reason for inadequate tissue sampling unknown (n=6). | C: Unknown | On-site cytologic assessment of a fine needle biopsy from the area may help to determine tissue viability and predict the adequacy of subsequent core biopsies taken from the area. |
Figure 1.
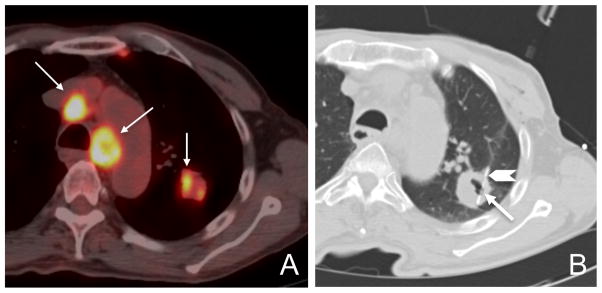
Case of sampling error resulting in insufficient tissue for biomarker analysis. Axial fused PET/CT image demonstrates FDG activity (arrows) within the mediastinal nodes and the inferior, medial border of the left upper lobe lung mass (A). Axial CT image during lung biopsy to acquire tumor tissue for enrollment into BATTLE demonstrates a coaxial technique with the tip of the 19-gauge guide needle located at the periphery of the lesion (arrowhead) and the 20-gauge core biopsy needle located in the lateral edge of the cavitary mass (arrow), an area which does not correspond to the highest area of FDG uptake on the pre-biopsy diagnostic PET/CT (B).
The overall complication rate was 15.9% (n=27), consisting of 26 cases of pneumothorax and one case of subcutaneous emphysema following lung biopsy. Chest tube placement was needed in 16 (59.2%) of 27 cases (9.4% of all biopsies). All but three of the patients requiring chest tube placement were treated as outpatients and had the chest tubes removed the next day, resulting in a minor (CTCAE Gr ≤ 2) complication rate of 14.1% (n=24). The major (all CTCAE Gr 3) complication rate was 1.8% (n=3): Two patients who required prolonged chest tube drainage for treatment of pneumothorax, one of whom required pleurodesis, and the patient who required chest tube placement for subcutaneous emphysema were admitted to the hospital.
DISCUSSION
Patients with NSCLC have therapies that can be tailored based on their molecular markers. This study demonstrates that 20-gauge PTCNB is safe and provides adequate tissue for the analysis of multiple biomarkers in 83% of patients enrolled into a personalized, targeted therapy NSCLC clinical trial. While success rates and acceptable thresholds for diagnostic yield have been well defined in the setting of diagnostic biopsy, these guidelines have yet to be established in the research setting.16 The lower diagnostic yield (83%) in this research clinical trial as compared to average yield of around 93% reported in a diagnostic setting is not surprising, since the purpose of the biopsy in a research setting is to get enough tissue sufficient not only for tumor classification by cytology and histology, but also for multiple biomarker analyses. Few studies have been conducted to analyze the adequacy of CNB for molecular profiling, and most of these studies have been limited to breast or liver tissue and l4-gauge needles.11,17,18 However, large-caliber needles are generally not used for PTCNB because of the potential for higher risk of pneumothorax and chest tube insertion. It remains questionable as to whether PTCNB using standard 20-gauge needles yields sufficient and reliable material for mutational analysis.13,19
Our experience with this study demonstrates that standard biopsy tools and techniques can be applied to acquiring tissue for research purposes. Table 4 represents a compilation of more recent experiences in using small tissue samples for the detection of mutations in NSCLC and shows a wide variation and lack of standardization with respect to the type of tissue sampled, the technique by which the tissue is acquired and the methodology used for mutation analysis.12,13,19,20–23 The current standard of practice for lung cancer clinical trials is to take samples from the original tumor for molecular analysis however, this may not be an accurate representation of the current biomarkers of the treated tumor.24–27 Furthermore, a recent article reviewing tissue sampling in lung cancer reported bronchoscopic biopsy in the MarkER Identification Trial (MERIT) yielded evaluable tissue for molecular profiling in only 50% of samples and had limited utility in other large NSCLC trials (BR.21 trial, ISEL, TRIBUTE and IPASS).7, 24–27 PTCNB offers several advantages over that of bronchoscopic biopsy: all areas of the thorax, including the mediastinum and peripheral lesions, are accessible and multiple core biopsies are possible. Three studies, only one of which was in the setting of a clinical trial,13 address the utility of percutaneous, PTCNB for mutation analysis in NSCLC.12,13,23 In comparison, our study is unique because PTCNBs of the tumor were acquired for the purpose of using the molecular profile to individualize patient therapy in a clinical trial.14 The 83% diagnostic yield seen the in the current study is lower than the 90–100% yield reported in some other studies on biopsies in a research setting;12,13,23 this is most likely related to the fact that 11 different biomarkers were analyzed in our study whereas the other studies reported on the adequacy of CNB for the analyses of one or two mutations.
Table 4.
Studies Using Small Tissue Specimens for Mutation Evaluation in NSCLC
| Author, Year | Number of Samples | Sample Type | Sample Size | Number of Samples Acquired | Mutations Evaluated | Complications | % Samples with Tissue Adequate for Mutation Analysis |
|---|---|---|---|---|---|---|---|
| Shih et al. 200619 | 63 | Formalin-fixed, paraffin embedded needle biopsy/aspirationa | NR | NR | EGFR by PCR analysis | NR | 100% |
| Otani et al. 200820 | 53 | Wash fluid from PTNB | NR | NR | EGFR by PCR analysis | NR | 100% |
| Zudaire et al. 200821 | 33 | Paraffin embedded FNA | NR | NR | 5p15, EGFR, MYC, CEPT6, P53, Ki-67 by FISH and immunocytochemistry | NR | 94% |
| Savic et al. 2008b,22 | 84 | Cytological specimens | NR | NR | EGFR by FISH | NR | 95% |
| Chen et al. 2008*,23 | 17 | Core needle biopsy (fresh frozen) | 18-gauge | 3 | EGFR | Pneumothorax 17.6% Hemoptysis 11.8% Chest tube insertion rate 6% |
100% |
| Solomon et al. 2009*,13 | 18 | Core needle biopsy | 18-gauge (n=15) 20-gauge (n=3) |
Median =2 | EGFR by direct sequencing or PCR KRAS by direct sequencing | Pneumothorax 16.7% Chest tube insertion rate 0% |
88.9% |
| Cheung et al. 201012 | 47 | Core needle biopsy | 18-gauge (n=32) 20-gauge (n=15) |
3 | EGFR by PCR analysis | Pneumothorax 12.8% Hemoptysis 6.4% Chest tube insertion rate 5.6% |
100% |
| Current Study Tam et al. 2012* | 170 | Core needle biopsy | 20-gauge | Median =3 | EGFR, KRAS, BRAF by PCR, EGFR and Cyclin D1 by FISH and six protein analyses by immunohistochemistry | Pneumothorax 15.3% Hemoptysis 0% Chest tube insertion rate 9.4% |
83% |
Samples taken from image guided core needle biopsies, endoscopic guided aspiration biopsies and effusion cell blocks. Tissues analysed included lung, liver, stomach, subcutaneous soft tissue metastasis and ascites.
Samples taken from transbronchial fine needle aspirations, bronchial washings, bronchial brushes, bronchoalevolar lavages and pleural effusions.
Indicates prospective study
NR-not reported, PTNB-percutaneous transthoracic needle biopsy, PCR-polymerase chain reaction, FNA-fine needle aspiration, FISH-fluorescent in situ hybridization
This study demonstrates the risks associated with transthoracic research biopsy are similar to those reported for transthoracic diagnostic biopsy. Pneumothorax is a common complication of transthoracic diagnostic biopsy and reported rates have ranged from 0% to 61% with most large series reporting pneumothorax rates in the range of 20–25%, with pneumothorax aspiration or chest tube insertion rates ranging from 0–17%.28–32 Our pneumothorax rate of 15.3% and chest tube insertion rate of 9.4% fall within these accepted ranges and demonstrate that patients who undergo transthoracic research biopsies are not subject to increased risk for complications.
Previous studies dealing with PTCNB in a diagnostic setting have suggested that small lesion size (lesions < 1cm) is associated with a poor diagnostic yield.32–35 Lesion size, however, was not found to a predictive factor in our study; this could be related to the fact that all of the lesions biopsied were larger than 1cm in size. In the current study, metastatic lesions were more likely to yield adequate tissue for biomarker analyses as compared to primary tumors. In addition, presence of cavitation in the biopsied lesion was associated with a poor diagnostic yield; however, on multivariate analyses this was not found to be predictive. The cases in the lesion selection problem error category represented 48% of the non-diagnostic biopsies. Although we did not find a difference in the diagnostic yield between patients with or without a recent FDG-PET-CT, we believe that FDG-PET-CT, with its ability to distinguish metabolically active disease from normal tissue, necrosis, fibrosis, or atelectasis, may be useful for optimizing lesion selection in unclear cases both by determining the best lesion for biopsy and by defining the most viable area of tumor to target during biopsy. The fact that none of the 14 cases in which lesion selection was identified as the error category had a FDG-PET/CT within 6 months of the biopsy indirectly supports this hypothesis. Emerging research where FDG-PET/CT guidance is used during biopsy to target the most avid regions may help to clarify this issue further.36–40 Sampling error was the second category affecting diagnostic yield; and, careful, pre-procedural review of the diagnostic and functional imaging, critical to procedural planning and acquiring diagnostic specimen, should be emphasized. In the six cases with no obvious source of error, the presence of on-site cytopathology assessment at the time of the biopsy procedure, for evaluation of either a fine needle aspiration sample or a touch prep of a CNB, may be helpful to determine tissue viability and predict the adequacy of subsequent CNBs taken from the area.41–45 Based on this error analysis, forthcoming clinical trials (BATTLE-2 and BATTLE-FL) have incorporated the use of real-time cytopathology assessment to determine tissue viability; and, if no clear lesion can be selected for biopsy based on the available diagnostic imaging, the IR has been requesting a FDG-PET/CT to optimize lesion selection prior to biopsy. It remains to be seen whether the implementation of these measures will improve diagnostic yield. In the future, the development of FDG-PET/CT guided biopsy techniques, the routine use of navigation devices and fusion of diagnostic and procedural images in the interventional radiology suite may also improve the likelihood of sampling viable tumor tissue.36–40
This study has limitations. First, despite the large number of biopsy cases, this study represents data from a single institution, a well-established cancer center with the requisite infrastructure and experience capable of coordinating this endeavor. Second, the error categories were assigned based on a retrospective review of the imaging of the biopsy cases making it difficult to truly establish cause and effect. In addition, our recommendations for improving the diagnostic yield in a research setting are not supported by numbers and statistical evidence. However, the purpose of analyzing the interventional radiology experience in the setting of this first large clinical trial using integral biomarker analysis from research biopsies to drive patient accrual and randomization, is in part hypothesis generating, and these ideas will be evaluated in future iterations of the BATTLE trials. Our recommendations are based partly on the results of the current study and partly on applying principles, such as on-site cytopathology assessment to improve yield, that have been tested previously in the diagnostic setting.41–45
The era of personalized therapy for lung cancer is here; and, while histological diagnosis remains important, molecular profiling, both for current treatment and most certainly for research, requires more robust tumor sampling. This study demonstrates small caliber core biopsy needles can be used to collect tissue safely and reliably during image-guided PTCNB for biomarker analysis in a clinical trial setting and validates this new paradigm for translational research in NSCLC patients.14 Multivariate analyses suggests that metastatic lesions are more likely to yield diagnostic tissue as compared to primary tumors. We believe that careful review of imaging data, especially PET-CT, if available for selecting the most appropriate biopsy site, and use of on-site cytopathology assessment have the potential of improving the diagnostic yield; however, these recommendations need to be validated in future studies.
Acknowledgments
Grant support: Department of Defense Grant W81XWH-6-1-0303 and National Institutes of Health MD Anderson Cancer Center Support Grant P30 CA016672.
ClinicalTrials.gov numbers: NCT00409968, NCT00411671, NCT00411632, NCT00410059 and NCT00410189.
References
- 1.Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer Facts & Figures 2010. http://www.cancer.org/Research/CancerFactsFigures/index.
- 3.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56:106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 4.Datta D, Lahiri B. Preoperative evaluation of patients undergoing lung resection surgery. Chest. 2003;123:2096–2103. doi: 10.1378/chest.123.6.2096. [DOI] [PubMed] [Google Scholar]
- 5.Molina JR, Yang P, Cassivi SD. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83:584–94. doi: 10.4065/83.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azzoli CG, Baker S, Jr, Temin S, et al. American Society of Clinical Oncology. Clinical Practice Guideline Update on Chemotherapy for Stage IV Non-Small Cell Lung Cancer. J Clin Oncol. 2009;27:6251–6266. doi: 10.1200/JCO.2009.23.5622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reck M, Hermes A, Tan EH, et al. Tissue sampling in lung cancer: a review in light of the MERIT experience. Lung Cancer. 2011;74:1–6. doi: 10.1016/j.lungcan.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Peppercorn J, Shapira I, Collyar D, et al. Ethics of mandatory research biopsy for correlative end points within clinical trials in oncology. J Clin Oncol. 2010;28:2635–2640. doi: 10.1200/JCO.2009.27.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daughtery CK. Impact of therapeutic research on informed consent and the ethics of clinical trials: A medical oncology perspective. J Clin Oncol. 1999;17:1601–1617. doi: 10.1200/JCO.1999.17.5.1601. [DOI] [PubMed] [Google Scholar]
- 10.Agulnik M, Oza AM, Pond GR, et al. Impact and perceptions of mandatory tumor biopsies for correlative studies in clinical trials of novel anticancer agents. J Clin Oncol. 2006;28:4801–4807. doi: 10.1200/JCO.2005.03.4496. [DOI] [PubMed] [Google Scholar]
- 11.Dowlati A, Haaga J, Remick SC, et al. Sequential tumor biopsies in early phase clinical trials of anticancer agents for pharmacodynamic evaluation. Clin Cancer Res. 2001;7:2971–2976. [PubMed] [Google Scholar]
- 12.Cheung YC, Chang JW, Hsieh JJ, et al. Adequacy and complications of computed tomography-guided core needle biopsy on non-small cell lung cancers for epidermal growth factor receptor mutations demonstration: 18-gauge or 20-gauge biopsy needle. Lung Cancer. 2010;67:166–169. doi: 10.1016/j.lungcan.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Solomon SB, Zakowski MF, Pao W, et al. Core needle lung biopsy specimens: adequacy for EGFR and KRAS mutational analysis. AJR. 2010;194:266–269. doi: 10.2214/AJR.09.2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim ES, Herbst RS, Wistuba II, et al. The BATTLE Trial: Personalizing Therapy for Lung Cancer. Cancer Discovery. 2011;1:44–53. doi: 10.1158/2159-8274.CD-10-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta S, Hicks ME, Wallace MJ, et al. Outpatient management of postbiopsy pneumothorax with small-caliber chest tubes: factors affecting the need for prolonged drainage and additional interventions. Cardiovasc Intervent Radiol. 2008;31:342–8. doi: 10.1007/s00270-007-9250-z. [DOI] [PubMed] [Google Scholar]
- 16.Gupta S, Wallace MJ, Cardella JF, et al. Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol. 2010;21:969–975. doi: 10.1016/j.jvir.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Ellis M, Davis N, Coop A, et al. Development and validation of a method for using breast core needle biopsies for gene expression microarray analyses. Clin Cancer Res. 2002;8:1155–1166. [PubMed] [Google Scholar]
- 18.Symmans WF, Ayers M, Clark EA, et al. Total RNA yield and microarray gene expression profiles from fine-needle aspiration biopsy and core-needle biopsy samples of breast carcinoma. Cancer. 2003;97:2960–2971. doi: 10.1002/cncr.11435. [DOI] [PubMed] [Google Scholar]
- 19.Shih JY, Gow CH, Yu CJ, et al. Epidermal growth factor receptor mutations in needle biopsy/aspiration samples predict response to gefitinib therapy and survival of patients with advanced nonsmall cell lung cancer. Int J Cancer. 2006;118:963–969. doi: 10.1002/ijc.21458. [DOI] [PubMed] [Google Scholar]
- 20.Otani H, Toyooka S, Soh J, et al. Detection of EGFR gene mutations using the wash fluid of CT-guided biopsy needle in NSCLC patients. J Thorac Oncol. 2008;3:472–476. doi: 10.1097/JTO.0b013e31816de2cd. [DOI] [PubMed] [Google Scholar]
- 21.Zudaire I, Lozano MD, Vazquez MF, et al. Molecular characterization of small peripheral lung tumors based on the analysis of fine needle aspirates. Histol Histopathol. 2008;23:33–40. doi: 10.14670/HH-23.33. [DOI] [PubMed] [Google Scholar]
- 22.Savic S, Tapia C, Grilli B, et al. Comprehensive epidermal growth factor receptor gene analysis from cytological specimens of non-small-cell lung cancers. Br J of Cancer. 2008;98:154–160. doi: 10.1038/sj.bjc.6604142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen CM, Chang WC, Cheung YC, et al. Computed tomography-guided core-needle biopsy specimens demonstrate epidermal growth factor receptor mutations in patients with non-small-cell lung cancer. Acta Radiol. 2008:991–994. doi: 10.1080/02841850802294410. [DOI] [PubMed] [Google Scholar]
- 24.Hirsch FR, Varella-Garcia M, Bunn PA, et al. Molecular predictions of outcome with gefitinib in a phase III placebo-controlled study in advanced non-small cell lung cancer. J Clin Oncol. 2006;24:5034–42. doi: 10.1200/JCO.2006.06.3958. [DOI] [PubMed] [Google Scholar]
- 25.Tsao M, Sakurada A, Cutz JC, et al. Erlotinib in lung cancer—molecular and clinical predictors of outcome. N Engl J Med. 2005;353:133–44. doi: 10.1056/NEJMoa050736. [DOI] [PubMed] [Google Scholar]
- 26.Eberhard DA, Johnson BE, Amler LC, et al. Mutations in the epidermal growth factor receptor and KRAS are predictive and prognostic indicators in patients with non-small cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J Clin Oncol. 2005;23:5900–9. doi: 10.1200/JCO.2005.02.857. [DOI] [PubMed] [Google Scholar]
- 27.Mok T, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 28.Covey AM, Gandhi R, Brody LA, et al. Factors associated with pneumothorax and pneumothorax requiring treatment after percutaneous lung biopsy in 443 consecutive patients. J Vasc Interv Radiol. 2004;15:479–83. doi: 10.1097/01.rvi.0000124951.24134.50. [DOI] [PubMed] [Google Scholar]
- 29.Swischuk JL, Castaneda F, Patel JC, et al. Percutaneous percutaneous transthoracic needle biopsy of the lung: review of 612 lesions. J Vasc Interv Radiol. 1998;9:347–52. doi: 10.1016/s1051-0443(98)70279-9. [DOI] [PubMed] [Google Scholar]
- 30.Westcott JL. Percutaneous percutaneous transthoracic needle biopsy. Radiology. 1988;169:593–601. doi: 10.1148/radiology.169.3.3055026. [DOI] [PubMed] [Google Scholar]
- 31.Hiraki T, Mimura H, Gobara H, et al. Incidence of and risk factors for pneumothorax and chest tube placement after CT fluoroscopy-guided percutaneous lung biopsy: retrospective analysis of the procedures conducted over a 9-year period. AJR. 2010;194:809–814. doi: 10.2214/AJR.09.3224. [DOI] [PubMed] [Google Scholar]
- 32.Yeow KM, Su IH, Pan KT, et al. Risk Factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004;126:748–754. doi: 10.1378/chest.126.3.748. [DOI] [PubMed] [Google Scholar]
- 33.Ohno Y, Hatabu H, Takenaka D, et al. CT-guided transthoracic needle aspiration biopsy of small (< or = 20 mm) solitary pulmonary nodules. AJR. 2003;180:1665–1669. doi: 10.2214/ajr.180.6.1801665. [DOI] [PubMed] [Google Scholar]
- 34.Priola AM, Priola SM, Cataldi A, et al. Accuracy of CT-guided transthoracic needle biopsy of lung lesions: factors affecting diagnostic yield. Radiol Med (Torino) 2007;112:1142–1159. doi: 10.1007/s11547-007-0212-y. [DOI] [PubMed] [Google Scholar]
- 35.Tsukada H, Satou T, Iwashima A, Souma T. Diagnostic accuracy of CT-guided automated needle biopsy of lung nodules. AJR. 2000;175:239–243. doi: 10.2214/ajr.175.1.1750239. [DOI] [PubMed] [Google Scholar]
- 36.Tatli S, Gerbaudo VH, Feeley CM, et al. PET/CT-guided percutaneous biopsy of abdominal masses: initial experience. J Vasc Interv Radiol. 2011;22:507–514. doi: 10.1016/j.jvir.2010.12.035. [DOI] [PubMed] [Google Scholar]
- 37.Klaeser B, Wiskirchen J, Wartenberg J, et al. PET/CT-guided biopsies of metabolically active bone lesions: applications and clinical impact. Eur J Nucl Med Mol Imaging. 2010;37:2027–2036. doi: 10.1007/s00259-010-1524-z. [DOI] [PubMed] [Google Scholar]
- 38.Werner MK, Aschoff P, Reimold M, et al. FDG-PET/CT-guided biopsy of bone metastases sets a new course in patient management after extensive imaging and multiple futile biopsies. Br J Radiol. 2011;84:e65–e67. doi: 10.1259/bjr/26998246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tatli S, Gerbaudo VH, Mamede M, et al. Abdominal masses sampled at PET/CT-guided percutaneous biopsy: initial experience with registration of prior PET/CT images. Radiology. 2010;256:305–11. doi: 10.1148/radiol.10090931. [DOI] [PubMed] [Google Scholar]
- 40.Cheebsumon P, Boellaard R, de Ruysscher D, et al. Assessment of tumour size in PET/CT lung cancer studies: PET- and CT-based methods compared to pathology. EJNMMI Res. 2012;2:56. doi: 10.1186/2191-219X-2-56. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santambrogio L, Mosotti M, Bellaviti N, et al. CT-guided fine-needle aspiration cytology of solitary pulmonary nodules: a prospective, randomized study of immediate cytologic evaluation. Chest. 1997;112:423–425. doi: 10.1378/chest.112.2.423. [DOI] [PubMed] [Google Scholar]
- 42.Küçük CU, Yilmaz A, Yilmaz A, Akkaya E. Computed tomography-guided transthoracic fine-needle aspiration in diagnosis of lung cancer: a comparison of single-pass needle and multiple-pass coaxial needle systems and the value of immediate cytological assessment. Respirology. 2004;9:392–6. doi: 10.1111/j.1440-1843.2004.00607.x. [DOI] [PubMed] [Google Scholar]
- 43.Austin JHM, Cohen MB. Value of having cytopathologist present during percutaneous fine-needle aspiration biopsy of lung: report of 55 cancer patients and meta-analysis of the literature. AJR. 1993;160:175–77. doi: 10.2214/ajr.160.1.8416620. [DOI] [PubMed] [Google Scholar]
- 44.Silverman JF, Finley JL, O’Brien KF, et al. Diagnostic accuracy and role of immediate interpretation of fine needle aspiration biopsy specimens from various sites. Acta Cytol. 1989;33:791–96. [PubMed] [Google Scholar]
- 45.Conces DJ, Schwenk GR, Jr, Doering PR, et al. Thoracic needle biopsy: improved results utilizing a team approach. Chest. 1987;91:813–16. doi: 10.1378/chest.91.6.813. [DOI] [PubMed] [Google Scholar]


