Abstract
Alentejo covers a third of Portugal, yet it is home to only 5% of the population. Residents of the region are poorer, older, and less educated than the rest of the country. There is a shortage of physicians in several specialties. The low population density, a concentration of specialized services, and a poor public transportation network all create barriers to access. Telemedicine was introduced in 1998 to help address these challenges. In this article, we provide an overview of the program and its current status, focusing on infrastructure, services, and activity volume. We also discuss the impact the program has had from the perspectives of patients and healthcare professionals. From 1998 to 2011, there were 132,546 episodes of service using telemedicine, including real-time teleconsultations, teleradiology, teleultrasound, and telepathology. At present, the network includes 20 primary care units and five hospitals, covering almost 30,000 km2 and 500,000 people. Units have high-resolution videoconferencing equipment, access to patients' clinical records, an image archive, and peripherals, such as electronic dermatoscopes and phonendoscopes. Teleconsultations are available in 15 medical specialties and areas, ranging from neurology to pediatric surgery. In 2008, regional health authorities started a tele-education program, and by the end of 2011, 876 healthcare professionals, across 52 locations, had participated in remote learning sessions. More than a decade since telemedicine was introduced in Alentejo, it is now an integral part of everyday service provision. A comprehensive assessment of the costs and consequences of the program is currently underway.
Key words: : telemedicine, teleradiology, distance learning
Introduction
Alentejo represents approximately one-third of Portugal's continental territory but is home to only 5% of its population (499,038 people). There are 18.3 people/km2, a sixth of the national average.1 A quarter of the inhabitants are over 65 years old, and only 5% have a higher education degree. Mean monthly earnings are around 10% lower than the national average. These factors all interact to create significant social and economic challenges for local health authorities. To exacerbate these difficulties, the supply of healthcare services is severely constrained. There is a shortage of hospital consultants in several specialties, and these are often concentrated in the region's main hospital, in Évora (e.g., there are three dermatologists in the region, all working in the Hospital do Espírito Santo de Évora). The population is dispersed, and local healthcare units can be hundreds of kilometers away from the main hospitals. The public transportation network is poor, and services to district capitals—where hospitals are located—are infrequent. It is not unusual for patients, and often their family members, to take an entire day off to attend a hospital appointment. In 1998, the regional health authorities started a telemedicine program in order to better meet the needs of the population with their limited resources. It has since become the largest telemedicine initiative in Portugal.
In this article we provide an overview of the use of telemedicine in Alentejo, with brief descriptions of the infrastructure and organization, services provided, activity volume, and impact. A larger study assessing the costs and consequences of teleconsultations is currently underway.
The Alentejo Telemedicine Programme
Objectives
The Programme is based on the premise that patients should be seen, diagnosed, and treated as close as possible to where they live and work. Its main objectives are to increase the accessibility of specialist healthcare services through a reduction in travel distances for patients, to reduce waiting times, to ensure equity in the access to the best available care for patients in remote underserved locations, and to reduce the costs of providing healthcare services through avoidance of unnecessary care.
Organization and Infrastructure
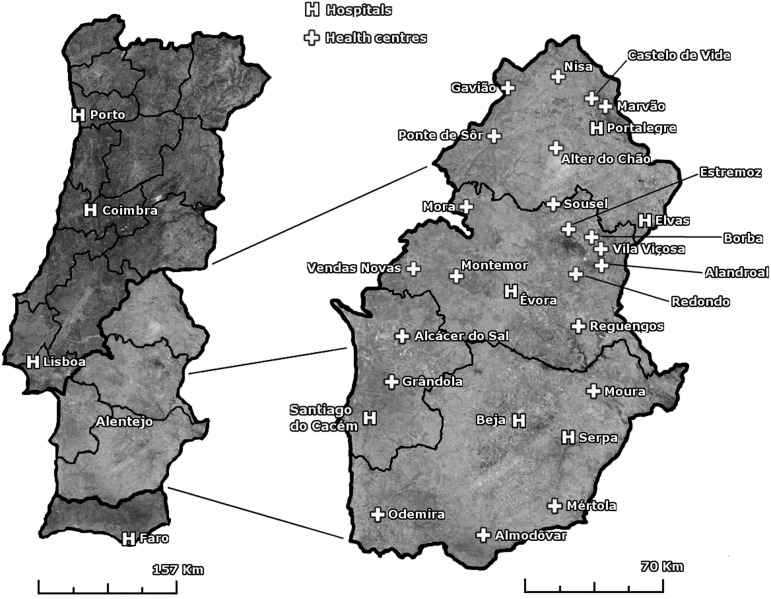
There are 26 telemedicine platforms distributed among 20 primary care units and five hospitals, covering four districts (Fig. 1). These communicate over the Health Information Network (Rede Informática de Saúde), a high-speed virtual private network managed by the Ministry for Health. The network is provided free of charge to healthcare units in the Portuguese National Health Service. The telemedicine platforms include high-resolution videoconferencing equipment, access to electronic patient records and picture archive, and peripherals such as electronic dermatoscopes and phonendoscopes (availability varies between units).
Fig. 1.
Telemedicine network in Alentejo, Portugal.
The most specialized care is provided in Évora. District hospitals in Beja, Portalegre, Elvas, and Litoral Alentejano provide specialized services, but several specialties are not available (e.g., dermatology). Patients from as far as Odemira may need to travel approximately 165 km each way for an outpatient face-to-face appointment in Évora. Although teleconsultations involve only facilities in Alentejo, teleradiology depends on hospitals in Lisbon and Oporto.
In Portugal, general practitioners act as gatekeepers: to see an National Health Service specialist, a patient must be referred by a general practitioner. Primary care units that are part of the telemedicine network must refer their patients to teleconsultations. Subsequent face-to-face appointments may then be arranged. Teleconsultations are real time with the presence of a general practitioner. Some primary care units appoint a coordinator who is present in every teleconsultation for a specific specialty; in others, the patient's own general practitioner is present. Treatment is usually prescribed by the general practitioner, except when special rules apply (e.g., neurological drugs, which must be prescribed by a qualified neurologist). Prescriptions written by specialists are mailed to patients. Besides managing schedules, support staff operate the videoconferencing equipment during teleconsultations, so that physicians can focus on the patient.
Services Provided
Teleconsultations are available in several specialties and clinical areas: diabetes, traumatology, orthopedics, general and pediatric surgery, respiratory medicine, urology, gastroenterology, clinical oncology, cardiology, dermatology, physical medicine and rehabilitation, pain, neurology, thyroid, and obesity. Besides real-time teleconsultations, the platforms are also used for teleradiology (computed tomography and x-rays), teleultrasound, and tele-education. Tele-education courses have covered such topics as informed consent, infection control, and bronchial asthma.
Impact of the Programme
Following the positive experience of the pilot phase (1998–2000), the use of the technology spread. As of 2011, a total of 132,546 episodes of service had been provided using telemedicine (Table 1). Dermatology accounted for more than a third of all teleconsultations performed, followed by neurology and cardiology. In recent years, the number of teleconsultations in physical medicine and rehabilitation and respiratory medicine has risen significantly. Fewer appointments were performed by urology and psychiatry. Since the start of the tele-education sessions in 2008, 876 professionals have participated in courses, with as many as 10 sites connected simultaneously.
Table 1.
Number of Episodes of Service Using Telemedicine, 1998–2011
| |
MODALITY |
|
||
|---|---|---|---|---|
| YEAR | TELECONSULTATIONS | TELERADIOLOGY | TELEULTRASOUND | TOTAL |
| 1998 |
30 |
35 |
0 |
65 |
| 1999 |
70 |
987 |
0 |
1,057 |
| 2000 |
181 |
1,702 |
0 |
1,883 |
| 2001 |
361 |
1,828 |
0 |
2,189 |
| 2002 |
963 |
2,279 |
0 |
3,242 |
| 2003 |
1,714 |
4,718 |
0 |
6,432 |
| 2004 |
2,562 |
6,126 |
0 |
8,688 |
| 2005 |
2,683 |
7,976 |
0 |
10,659 |
| 2006 |
2,886 |
9,555 |
0 |
12,441 |
| 2007 |
2,677 |
12,422 |
0 |
15,099 |
| 2008 |
3,717 |
13,031 |
0 |
16,748 |
| 2009 |
3,294 |
10,565 |
0 |
13,859 |
| 2010 |
3,479 |
16,140 |
767 |
20,386 |
| 2011 |
3,235 |
15,389 |
1,174 |
19,798 |
| Total | 27,852 | 102,753 | 1,941 | 132,546 |
Data are from the Administração Regional de Sáude do Alentejo, I.P.2
The Perspective of Patients
To assess the impact of teleconsultations on patient experience, in early 2012, 200 patients (100 teleconsultation patients and 100 face-to-face patients) were surveyed by the Patient Management Department of the Hospital do Espírito Santo de Évora. The results indicate teleconsultation has a positive impact on patient experience, expenses, and quality of service (a selection of results appears in Table 2). The average distance traveled was 6 km for a teleconsultation compared with 47 km for a face-to-face appointment. The average time taken to attend an appointment (i.e., return traveling time plus physical waiting time plus appointment duration) was 93 min for a teleconsultation compared with 190 min for a face-to-face appointment. The average waiting time (i.e., the time between the day the patient is referred for an outpatient appointment and the day the appointment takes place) for a teleconsultation was 26 days compared with 74 days for a face-to-face consultation.
Table 2.
Selected Patient Survey Results
| VARIABLE | TELEMEDICINE | FACE-TO-FACE |
|---|---|---|
| Means of transportation | ||
| Car |
57 |
76 |
| Bus |
2 |
9 |
| Taxi |
0 |
2 |
| Ambulance |
2 |
8 |
| Walk |
39 |
5 |
| Total |
100 |
100 |
| Satisfaction | ||
| Very satisfied |
42 |
26 |
| Somewhat satisfied |
54 |
68 |
| Indifferent |
2 |
3 |
| Somewhat unsatisfied |
2 |
3 |
| Total |
100 |
100 |
| Patient came accompanied | ||
| Yes |
46 |
67 |
| No |
54 |
33 |
| Total |
100 |
100 |
| Occupation of companion | ||
| Active (employed) |
16 |
40 |
| Inactive (retired, unemployed, student) |
30 |
27 |
| Total | 46 | 67 |
Because of the characteristics of the population (e.g., age, health status, and income), some patients are entitled to National Health Service–paid transportation to outpatient appointments by ambulance. Although 8% of face-to-face survey respondents traveled in an ambulance, only 2% of teleconsultation patients did so. Most significant is that 39% of teleconsultation patients walked to their appointment, avoiding costs and emissions but also potentially promoting their own health.3 The average cost for teleconsultation patients in the survey was estimated at ”9.31 compared with ”25.32 for face-to-face patients, a reduction of 63% (costs included the co-payment and traveling and time-off-work costs for both patients and those accompanying, estimated from survey data on average income and means of transportation). For patients living in remote locations (e.g., Odemira is 100 km distant from Évora), savings were considerably bigger.
The Perspective of Clinicians
In late 2010, a group of general practitioners (n=4), consultants (n=6), and primary care managers (n=2) involved in the Telemedicine Programme participated in interviews concerning the impact of teleconsultations in the region. The majority (n=11) would encourage colleagues to use teleconsultations, with one consultant considering that face-to-face care is preferable when available. Asked about the disadvantages of telemedicine, half of the respondents mentioned not being able to physically touch the patient, with the other half considering there were none. As for the benefits, participants mentioned improvements to service capacity, productivity, and efficiency due to quicker consultations and better scheduling, patient benefits from increased geographical access and reductions in traveling time and associated costs, avoidance of unnecessary visits to the hospital, and, finally, continual medical education of general practitioners and consequently fewer referrals.
In the end of 2010, 32 participants from four tele-education sessions were surveyed on several issues, using a 5-point Likert scale. The majority of participants were either very satisfied (n=20) or somewhat satisfied (n=7), and 30 reported they would encourage colleagues to participate in future sessions. Items concerning the quality and performance of trainers were considered either good or very good by all respondents. Ten respondents were participating in tele-education sessions for the first time.
Looking to the Future
We are currently conducting a comprehensive evaluation to quantify the economic impact as well as assess unintended effects from the use of teleconsultations in Alentejo. The findings will be used to clarify how the technology can be used to provide maximum benefit at lowest cost to all stakeholders, as well as to inform future implementations of teleconsultations at a national level.
At present, the use of telemedicine in other regions of Portugal is extremely limited compared with Alentejo. In 1998, the same year the Alentejo Telemedicine Programme was created, the pediatric hospital in Coimbra started a telecardiology consultation in association with hospitals in Leiria and Porto.4 Since then, other hospitals (Santa Maria da Feira, Lisboa, and Covilhã in Portugal, Mindelo in Cape Verde, Luanda in Angola, and Madrid in Spain) have joined the service. From 1998 to 2006, the pediatric hospital in Coimbra provided 4,741 teleconsultations, although there is no information regarding which hospitals were involved.5 Based on the few available studies, most projects are either small or in early stages of implementation.5–7
In July 2012, the Ministry for Health set up a working group to develop a national telemedicine program drawing on the experience of the Alentejo Telemedicine Programme. The group has identified the following priorities: advance the use of teleconsultation in other regions of Portugal; pilot a remote monitoring solution for chronic obstructive pulmonary disease patients; and ensure that lawmakers and payers develop legislation and policies that allow for the spread of telemedicine.8 In Alentejo, the regional health authorities are currently undertaking an ISO 9001 certification of teleconsultations, and tele-education is expected to receive the same certification by end of the year.
Conclusions
The Alentejo Telemedicine Programme is now more than a decade old. Patients and providers in the region believe the Programme promotes equity and reduces barriers to access to outpatient care. Regional health authorities consider it essential to address the region's challenges.2 The Programme is now an integral part of everyday healthcare provision, and the experience acquired in the region is currently informing a national program for telemedicine. The experiences of other international initiatives is also being taken into account.9–11 Notwithstanding the general positive impact to date, future work should focus on establishing a high-quality economic evidence base for the use of telemedicine services. Despite a large and growing number of studies concerned with the economic impact of telemedicine, there is still little robust evidence of its cost-effectiveness.12,13 If we are to sustain and realize the promise of telemedicine, whether in Alentejo or elsewhere, it is essential that, whenever possible, we conduct evaluation studies that are in accordance with best practices and guidelines for economic evaluation. The evaluation of costs and consequences that is currently underway in Alentejo should contribute to that objective.
Acknowledgments
We are grateful to Manuela Rosado, José António Estrompa, Rosa Matos, Sónia Martins, Fernando Miranda, Maria José Branquinho, José Robalo, Horácio Feiteiro, Penalva Santos, Hugo Quintino, Fátima Breia, Fátima Ferreira, and Manuel Murta for their support and collaboration. This research is partly funded by a doctoral grant from the Fundação para a Ciência e a Tecnologia, Portugal (grant SFRH/BD/66305/2009 to T.C.O.). We also acknowledge the support of the United Kingdom Engineering and Physical Science Research Council's Health and Care Infrastructure Research and Innovation Centre.
Disclosure Statement
L.G. is director of the Telemedicine Programme in Alentejo and Chair of the national Telemedicine Working Group. T.C.O., J.B., and S.B. are members of the United Kingdom Engineering and Physical Science Research Council's Health and Care Infrastructure Research and Innovation Centre.
References
- 1.Instituto Nacional de Estatística, I.P. Anuário estatístico da região Alentejo 2010. Lisboa: Instituto Nacional de Estatística I.P., 2010 [Google Scholar]
- 2.Administração Regional de Sáude do Alentejo, I.P. Telemedicina—Actividade 1998–2011. Évora, Portugal: Administração Regional de Sáude do Alentejo, I.P., 2012 [Google Scholar]
- 3.Jarrett J, Woodcock J, Griffiths UK, et al. . Effect of increasing active travel in urban England and Wales on costs to the National Health Service. Lancet 2012;379:2198–2205 [DOI] [PubMed] [Google Scholar]
- 4.Castela E, Ramalheiro G, Pires A, et al. . Five years of teleconsultation: the experience of the Cardiology Deparment of Coimbra Pediatric Hospital [in English, Portuguese]. Rev Port Cardiol 2005;24:835–840, [PubMed] [Google Scholar]
- 5.Associação Portuguesa para a Promoção e Desenvolvimento da Sociedade da Informação and Associação para o Desenvolvimento da Telemedicina. Telemedicina—Onde estamos e para onde vamos. Lisbon, Portugal: Associação Portuguesa para a Promoção e Desenvolvimento da Sociedade da Informação and Associação para o Desenvolvimento da Telemedicina, 2007 [Google Scholar]
- 6.Costa PD, Reis AH, Rodrigues PP.Clinical and economic impact of remote monitoring on the follow-up of patients with implantable electronic cardiovascular devices: An observational study. Telemed J E Health 2013;19:71–80 [DOI] [PubMed] [Google Scholar]
- 7.Burnay E, Cruz-Correia R, Jacinto T, Sousa AS, Fonseca J.Challenges of a mobile application for asthma and allergic rhinitis patient enablement—Interface and synchronization. Telemed J E Health 2013;19:13–18 [DOI] [PubMed] [Google Scholar]
- 8.Administração Central do Sistema de Saúde Grupo de trabalho para a telemedicina. November15, 2012. Available at www.min-saude.pt/portal/conteudos/a+saude+em+portugal/informatizacao/grupos+trabalho.htm (last accessed January24, 2013)
- 9.The Scottish Centre for Telehealth and Telecare. SCTT. Available at http://www.sctt.scot.nhs.uk/index.html (last accessed January24, 2013)
- 10.Ontario Telemedicine Network OTN | Ontario Telemedicine Network (OTN). Available at http://otn.ca/en/ (last accessed January24, 2013)
- 11.Department of Health Whole System Demonstrator Programme—Headline Findings—December 2011. December5, 2011. Available at www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_131684 (last accessed January24, 2013)
- 12.Bergmo TS.Economic evaluation in telemedicine—Still room for improvement. J Telemed Telecare 2010;16:229–231 [DOI] [PubMed] [Google Scholar]
- 13.Centre for Reviews and Dissemination Evidence briefing on teleconsultation. September2012. Available at hwww.york.ac.uk/inst/crd/pdf/Teleconsultation.pdf (last accessed January24, 2013)