Abstract
Introduction: Failure to attend medical appointments among persons living with human immunodeficiency virus (HIV) has been associated with poor health outcomes. Text message appointment reminders are a novel tool to potentially improve appointment attendance, but the feasibility of this tool among persons living with HIV in the United States is unknown. Subjects and Methods: We conducted a randomized, controlled trial of text message reminders in a large HIV clinic. Patients who declined enrollment were asked for reasons for declining. For all patients randomized, demographic and clinical data were collected from medical records. Results: Of 94 patients screened for the study, 42 (45%) did not elect to participate; the most common reason for declining participation was the lack of either a cell phone or text messaging service. Cost, comfort with text messaging, and privacy were other major barriers to study enrollment. Among the 25 subjects randomized to receive text messages, 6 (24%) had their phones disconnected prior to the appointment reminder date. Ultimately, there were no differences in clinic attendance rates between the group that received text reminders versus the group that did not (72% versus 81%, p=0.42) in an intention-to-treat analysis. Conclusions: Although text message reminders may be successful in certain groups of patients, barriers must be addressed before they are used as a universal approach to improve clinic attendance.
Key words: : human immunodeficiency virus, text message appointment reminder, mobile phone, clinic attendance
Introduction
Failure to attend medical appointments is associated with poor outcomes among persons with human immunodeficiency virus (HIV) infection, associated with detectable viral loads and AIDS-defining CD4 counts.1 “Forgetting” and confusion over dates and times are prominent reasons for poor compliance with clinic attendance.2–4 Text message appointment reminders have been shown to improve attendance in multiple outpatient settings, although many of these studies were done in subspecialty clinics, such as ear-nose-throat or ophthalmology, or among middle- to high-income patients.4–8 The acceptability and feasibility of this tool among persons living with HIV in the United States are unknown. Therefore we conducted a randomized, controlled trial of text message reminders in a large HIV clinic.
Subjects and Methods
Study Population
Subjects were recruited from the Duke University Medical Center (Durham, NC) Adult Infectious Diseases Clinic from June 2010 to August 2010. Inclusion criteria included (1) HIV infection, (2) age >17 years, (3) mobile phone ownership with a text messaging plan, and (4) ability to provide written, informed consent. Subjects were randomized, using a computer-generated random number list with a 1:1 allocation ratio. Patients were randomized to a text message reminder about their upcoming clinic appointment (in addition to standard of care) or to standard of care, which consists of an automated reminder call to the patient's home phone (only if a home phone exists). Potential subjects with access to a text messaging service who declined enrollment were asked to anonymously explain reasons for nonparticipation. The study was approved by the Duke University Medical Center Institutional Review Board.
Intervention and Data Abstraction
After consenting, participants had to opt-in by sending a text message from their cell phones to an online texting service, “Call-em-All.” Study personnel provided an explanation to patients about how to accomplish the opt-in process, but study personnel did not specifically watch them complete this process. Messages were sent 1 day prior to the appointment date and read “Remember: you have a doctor's appointment tomorrow.” Eleven of 25 (45%) participants did not correctly perform the opt-in text to the commercial service; these participants had text message reminders manually entered via an investigator's mobile phone. Appointment attendance was verified by checking the medical record. Sociodemographic information and clinical data were abstracted from the medical record. Patients were not told to which group they were randomized, and their follow-up appointments were at least 1 month after study enrollment. Patient allocation was concealed from all physicians caring for the patient participants, as well as the study personnel determining patient attendance or no attendance.
Data Analysis
The primary outcome was attendance or no attendance at the next scheduled clinic appointment. Differences in categorical variables were assessed using Fisher's exact test, and differences in continuous variables were assessed using the Kruskal–Wallis test. In an intention-to-treat analysis we excluded the patients who were randomized to the texting arm but did not actually receive a text message because of a disconnected phone or wrong number (7 patients).
Results
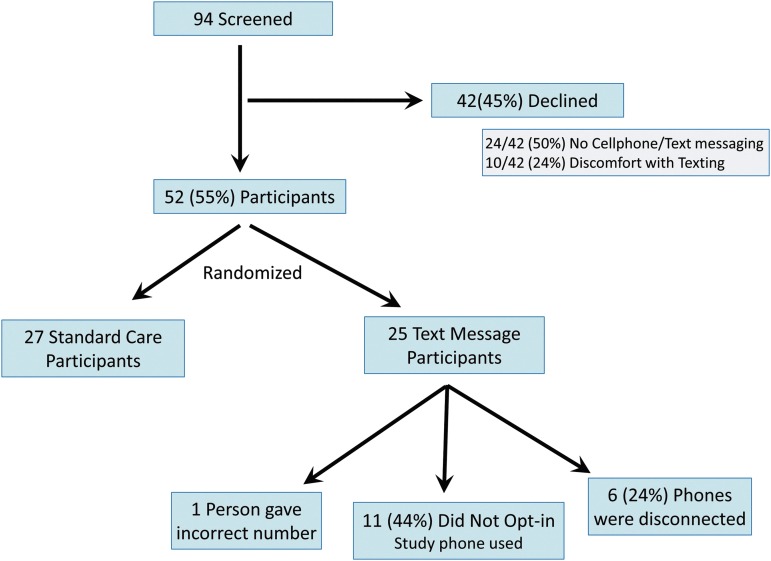
Of 94 patients screened for enrollment, only 52 (55%) elected to participate (Fig. 1). Of the patients who did not enroll, half (21/42 [50%]) were ineligible because they did not have the needed technology, either mobile phone or text messaging service. Six (29%) declined because of disinterest in study participation, 6 (29%) cited privacy concerns, 2 (10%) cited the cost of text messaging, 2 (10%) preferred not to text, 3 (14%) believed they did not need additional reminding, and 3 (14%) did not specify (one subject cited two reasons for nonparticipation, so numbers sum to 22).
Fig. 1.
Subject screening and illustration of barriers to enrollment and text messaging implementation.
Fifty-two subjects agreed to participate and were randomized. There were no differences in subject characteristics between study arms (Table 1). The appointment attendance rate for the previous year among all participants was an average of 85%. Ultimately, there was no difference in clinic attendance rates between the group that received text reminders versus the group that did not (72% versus 81%, p=0.42). Of the participants randomized to the texting group, 24% (6/25) had mobile phones that were disconnected during the study, and one person provided an incorrect mobile phone number. Eleven of 25 (44%) had difficulty with the opt-in texting process, although these subjects received a text via study personnel mobile phone. Excluding patients with disconnected phones or wrong numbers made no difference in appointment adherence rates between study arms in an intention-to-treat analysis.
Table 1.
Characteristics of Patients
| PATIENT CHARACTERISTICS | STANDARD OF CARE (N=27) | TEXT REMINDER (N=25) |
|---|---|---|
| Age (years) |
41.9±11.8 |
45.1±11 |
| Race | ||
| Black |
15 (56) |
14 (56) |
| White |
12 (44) |
11 (44) |
| Gender | ||
| Male |
19 (70) |
20 (80) |
| Female |
8 (30) |
5 (20) |
| CD4 count (cells/microliter) |
599±315 |
561±371 |
| Undetectable viral load |
19 (70) |
15 (60) |
| Mental illness |
12 (44) |
11 (44) |
| Active substance abuse |
4 (15) |
1 (4) |
| Durham residency |
11 (41) |
4 (16) |
| Insurance status | ||
| Private |
13 (48) |
11 (44) |
| Medicaid/ADAP |
12 (44) |
10 (40) |
| Medicare | 2 (8) | 4 (16) |
Data are mean±standard deviation values or number (%) as indicated.
ADAP, AIDS Drug Assistance Program.
Discussion
Text message reminders did not improve appointment adherence in this study, to a large degree because of logistical challenges to implementation of these reminders. Almost half of the people approached did not participate, of whom the majority had specific obstacles related to the text messaging itself. The most common reason for declining participation was the lack of a cell phone or text messaging service. Other major barriers to study enrollment were concerns regarding cost, comfort, and privacy with text messaging. Furthermore, among participants who had the technology to participate, 24% had their cell phones disconnected prior to the appointment reminder date, indicating that cell phone retention poses further complexity in this patient population.
Text message reminders have been shown to be successful for appointment adherence among certain populations. A study in London showed a 38% reduction in outpatient ophthalmology nonattendance rates when patients were given text message appointment reminders.7 Similar improvements were seen in primary care settings in Brazil and Malaysia.9 Text message appointment reminders have also been successful in improving behavior changes in disease management and prevention. Adherence to vitamin regimens, weight loss programs, smoking cessation, and diabetes management were all shown to improve with text message reminder interventions.10 Extending this technology to the U.S. HIV population, where adherence and behavior change are important, would be a natural progression.
Here, we found that the use of text messaging in an HIV population may come with distinct barriers. Despite the increase in U.S. cellphone ownership,11 we found a paucity of technology among our patients. This has been seen in other studies of HIV patients in the United States. In one cross-sectional study of 515 HIV patients in an urban U.S. clinic, only 60% of patients owned a cell phone, and only 40% of that sample reported text messaging knowledge.12 Cell phone ownership was associated with being white, being employed, having a higher income, and having a higher level of education. Knowledge of text message use was associated with being less than 40 years old, more educated, and employed. In contrast, our clinic population is older and diverse and includes many persons belonging to disadvantaged socioeconomic groups. Indeed, almost half of our patients received government-assisted insurance, for which being at or below 125% poverty level is a requirement. The results of this randomized trial echoes a previous survey conducted in the same clinic in which only 56% of patients surveyed felt it would be acceptable to receive text message reminders.13 The national HIV epidemic, although heterogeneous, is primarily apparent in a population that is low income, African American, and less educated.14,15 It is therefore difficult to conclude that while technology-based interventions have worked in some outpatient settings, they will be successful among a population of HIV patients in the United States who carry a unique set of sociodemographics that impact their use of technology. There have been very few studies evaluating this population in particular. In addition to lack of access found in our study, we also discovered that some people were uncomfortable with the potential for privacy disruptions. A diagnosis of HIV carries stigmatization and discomfort that other diseases do not possess and may lead to decreased acceptance of technology-based interventions that are not entirely confidential. Acceptance of technology in one setting may not be transferable to the HIV patient setting.
Although text messaging reminders did not increase adherence in our population, addressing certain barriers may aid in the use of text messaging. Clinics should remove any opt-in procedure for health-related text messaging, which in our study proved to be a barrier to participation. Furthermore, mobile numbers should be updated frequently and with every visit, so as to overcome the barrier of frequent cell phone number instability. Finally, although text messaging may not be successful as a universal approach among patients living with HIV, it may still be warranted in a subset of patients who specifically have poor appointment adherence but also access to this technology. The subset of patients with access to text messaging could also benefit from other health-related messages, such as result notifications, or direct questioning to physicians. Privacy should be explicitly discussed in order to assure comfort and acceptance.
This study has several limitations. The numbers of participants in each arm were small, giving rise to the potential for a type II error. The baseline attendance rate of our clinic was already quite high, making it difficult to show a significant change in appointment adherence. Furthermore, because we recruited participants while they were in the clinic, we were already selecting for a group of patients who were more likely to attend their next appointment. Ideally we would consent patients in the community who were at highest risk for nonattendance, but this methodology poses further complexity such as privacy issues. We also did not differentiate between appointments that were actively canceled by the patient and those that were missed, although there is no reason to believe that the rate of cancellation would be different between study groups.
We found that there were many barriers to the implementation of text message reminders as a strategy to improve HIV clinic attendance. The heterogeneous use of technology among the HIV population in the United States may make it difficult to implement text messaging as a universal intervention to improve engagement in care. Although text messages may be beneficial in a subset of patients, barriers will need to be addressed if text messaging is to be effective. Future studies are needed to answer these questions in the HIV population.
Acknowledgments
The authors would like to acknowledge the patients and staff of the Duke Adult Infectious Diseases Clinic. This research was conducted with the support of the Office of Research and Development, Veterans Health Administration, Department of Veterans Affairs, Agency for Healthcare Research and Quality fellowship T32 HS00079-01-31 (to B.L.N.), and National Institutes of Health AIDS Training grant 5T32 AI007392 (to A.K.P.).
Disclosure Statement
No competing financial interests exist.
References
- 1.Berg MB, Safren SA, Mimiaga MJ, Grasso C, Boswell S, Mayer KH. Nonadherence to medical appointments is associated with increased plasma HIV RNA and decreased CD4 cell counts in a community-based HIV primary care clinic. AIDS Care 2005;17:902–907 [DOI] [PubMed] [Google Scholar]
- 2.Hamilton W, Luthra M, Smith T, Evans P. Non-attendance in general practice: A questionnaire survey. Prim Health Care Res Dev 2002;3:226–230 [Google Scholar]
- 3.Neal R, Hussain-Gambles M, Allgar V, Lawlor D, Dempsey O. Reasons for and consequences of missed appointments in general practice in the UK: Questionnaire survey and prospective review of medical records. BMC Fam Pract 2005;6:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geraghty M, Glynn F, Amin M, Kinsella J. Patient mobile telephone ‘text’ reminder: A novel way to reduce non-attendance at the ENT out-patient clinic. J Laryngol Otol 2008;122:296–298 [DOI] [PubMed] [Google Scholar]
- 5.Chen ZW, Fang LZ, Chen LY, Dai HL. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: A randomized controlled trial. J Zhejiang Univ Sci B 2008;9:34–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leong KC, Chen WS, Leong KW, Mastura I, Mimi O, Sheikh MA, et al. The use of text messaging to improve attendance in primary care: A randomized controlled trial. Fam Pract 2006;23:699–705 [DOI] [PubMed] [Google Scholar]
- 7.Koshy E, Car J, Majeed A. Effectiveness of mobile-phone short message service (SMS) reminders for ophthalmology outpatient appointments: Observational study. BMC Ophthalmol 2008;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Downer SR, Meara JG, Da Costa AC. Use of SMS text messaging to improve outpatient attendance. Med J Aust 2005;183:366–368 [DOI] [PubMed] [Google Scholar]
- 9.da Costa TM, Salomao PL, Martha AS, Pisa IT, Sigulem D. The impact of short message service text messages sent as appointment reminders to patients' cell phones at outpatient clinics in Sao Paulo, Brazil. Int J Med Inform 2010;79:65–70 [DOI] [PubMed] [Google Scholar]
- 10.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lenhart A. Cell phones and American adults. 2010. Available at www.pewinternet.org/Reports/2010/Cell-Phones-and-American-Adults.aspx (last accessed November11, 2012)
- 12.Shacham E, Stamm K, Overton ET. Can you hear me now? Limited use of technology among an urban HIV-infected cohort. AIDS Care 2009;21:1000–1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Person AK, Blain ML, Jiang H, Rasmussen PW, Stout JE. Text messaging for enhancement of testing and treatment for tuberculosis, human immunodeficiency virus, and syphilis: A survey of attitudes toward cellular phones and healthcare. Telemed J E Health 2011;17:189–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas M. HIV/AIDS and xocioeconomic status: A Texas study. 2011. Available at http://ssrn.com/abstract=1767180 (last accessed November11, 2012)
- 15.Center for Disease Control and Prevention HIV in the United States: At a glance. 2011. Available at www.cdc.gov/hiv/resources/factsheets/us.htm (last accessed November11, 2012)