Abstract
Study objective
Patients with minor traumatic intracranial hemorrhage are frequently admitted to the ICU, although many never require critical care interventions. To describe ICU resource use in minor traumatic intracranial hemorrhage, we assess (1) the variability of ICU use in a cohort of patients with minor traumatic intracranial hemorrhage across multiple trauma centers, and (2) the proportion of adult patients with traumatic intracranial hemorrhage who are admitted to the ICU and never receive a critical care intervention during hospitalization. In addition, we evaluate the association between ICU admission and key independent variables.
Methods
A structured, historical cohort study of adult patients (aged 18 years and older) with minor traumatic intracranial hemorrhage was conducted within a consortium of 8 Level I trauma centers in the western United States from January 2005 to June 2010. The study population included patients with minor traumatic intracranial hemorrhage, defined as an emergency department (ED) Glasgow Coma Scale (GCS) score of 15 (normal mental status) and an Injury Severity Score less than 16 (no other major organ injury). The primary outcome measure was initial ICU admission. The secondary outcome measure was a critical care intervention during hospitalization. Critical care interventions included mechanical ventilation, neurosurgical intervention, transfusion of blood products, vasopressor or inotrope administration, and invasive hemodynamic monitoring. ED disposition and the proportion of ICU patients not receiving a critical care intervention were compared across sites with descriptive statistics. The association between ICU admission and predetermined independent variables was analyzed with multivariable regression.
Results
Among 11,240 adult patients with traumatic intracranial hemorrhage, 1,412 (13%) had minor traumatic intracranial hemorrhage and complete ED disposition data (mean age 48 years; SD 20 years). ICU use within this cohort across sites ranged from 50% to 97%. Overall, 847 of 888 patients (95%) with minor traumatic intracranial hemorrhage who were admitted to the ICU did not receive a critical care intervention during hospitalization (range between sites 80% to 100%). Three of 524 (0.6%) patients discharged home or admitted to the observation unit or ward received a critical care intervention. After controlling for severity of injury (age, blood pressure, and Injury Severity Score), study site was independently associated with ICU admission (odds ratios ranged from 1.5 to 30; overall effect P<.001).
Conclusion
Across a consortium of trauma centers in the western United States, there was wide variability in ICU use within a cohort of patients with minor traumatic intracranial hemorrhage. Moreover, a large proportion of patients admitted to the ICU never required a critical care intervention, indicating the potential to improve use of critical care resources in patients with minor traumatic intracranial hemorrhage.
INTRODUCTION
Background
Traumatic brain injury is the most common cause of death and disability in patients younger than 44 years.1 Each year, it accounts for an estimated 1.1 million emergency department (ED) visits, 235,000 hospitalizations, and 50,000 deaths in the United States.2 The presence or absence of traumatic intracranial hemorrhage is determined by cranial computed tomography (CT) imaging. Generally, patients with traumatic brain injury but without traumatic intracranial hemorrhage (ie, concussion) are discharged from the ED, whereas patients with traumatic intracranial hemorrhage are admitted to the hospital for further management.3
Patients with a traumatic intracranial hemorrhage are classified as having mild (Glasgow Coma Scale [GCS] score 13 to 15), moderate (GCS score 9 to 12), or severe injury (GCS score 3 to 8).4 Patients with moderate or severe traumatic intracranial hemorrhage have high morbidity and mortality and almost uniformly require ICU admission for neurologic monitoring and concentrated therapy.5 ICU care assists in early detection of secondary brain injury from cerebral edema, increased intracranial pressure, and cerebral ischemia.6
Importance
However, in patients with a traumatic intracranial hemorrhage and a normal mental status (GCS score=15), the rate of hematoma expansion is low and need for neurosurgical intervention is rare.7,8 Thus, the need for ICU admission in patients with mild traumatic intracranial hemorrhage is less certain, and routine ICU admission may lead to unnecessary use of critical care resources. Previous evidence from a single center indicated that 55% of adult patients with any degree of traumatic intracranial hemorrhage who were admitted to the ICU never required a critical care intervention (mechanical ventilation, neurosurgical intervention, vasopressor/inotrope use, blood product transfusion, and invasive monitoring) during hospitalization.9
Disposition of ED patients with a normal mental status and traumatic intracranial hemorrhage that does not require immediate neurosurgical operative intervention may include one of the following strategies: admission to the hospital ICU, admission to the hospital ward (non-ICU setting), monitoring within an ED observation unit, or observation in the ED and discharge home.10–12 Because of the lack of well-defined recommendations for ICU admission in alert patients with traumatic intracranial hemorrhage, there is potential for wide variability in ICU use among trauma centers.3 The degree of such variability, however, has not been assessed.
Goals of This Investigation
The objective of this study was to evaluate the variability of ICU use in adult patients with minor traumatic intracranial hemorrhage across a consortium of trauma centers and to evaluate the proportion of these patients admitted to the ICU who never receive a critical care intervention during hospitalization. In addition, we will evaluate the association between ICU admission and key independent variables.
MATERIALS AND METHODS
Study Design and Setting
This multicenter, historical cohort study was approved by the institutional review boards at all sites. The study was conducted at 8 academic sites across the western United Stataes (Denver Health Medical Center; Oregon Health & Sciences University; Stanford University; University of California, Davis; San Francisco General Hospital; University Medical Center of Southern Nevada; University of Utah; and University of Washington). Participating sites are part of the Western Emergency Services Translational Research Network, a consortium of academic centers linked through Clinical and Translational Science Award centers.13,14 All participating hospitals are American College of Surgeons accredited Level I trauma centers. All trauma centers have trauma registry programs that collect a uniform set of trauma registry variables in accordance with the National Trauma Data Standard Data Dictionary.15 Inclusion and exclusion criteria for all trauma registries were similar (Table E1, available online at http://www.annemergmed.com).16 None of the sites have a formal policy of ICU admission for patients with traumatic intracranial hemorrhage. The primary advantage of using this consortium rather than a national trauma database is the ability to ascertain key variables at each site and direct contact with individual sites to ensure accuracy, reliability, and appropriate interpretation of the data.16
Selection of Participants
The population of primary interest was adult subjects with traumatic intracranial hemorrhage and an initial ED GCS score of 15 (normal mental status) and an Injury Severity Score less than 16. This cohort represents subjects with a similar severity of injury who were at low risk for requiring neurosurgical interventions and may be potentially managed outside of the ICU.7,8 Injury Severity Score is calculated at discharge and is routinely dichotomized at 16 or greater (severe trauma) and less than 16 (nonsevere trauma).17,18 An Injury Severity Score less than 16 also serves as a surrogate for isolated head trauma because these patients cannot have both a traumatic intracranial hemorrhage and a severe nonhead injury (other major organ injury).
Trauma registries at all sites were searched from January 1, 2005, to June 30, 2010, for adult ED subjects (aged 18 years and older) with International Classification of Diseases, Ninth Revision (ICD-9) codes specific for traumatic intracranial hemorrhage (codes 851 to 854).19 ICD-9 codes with the 854 prefix (intracranial injury of other and unspecified nature) were subsequently excluded from 3 sites because on querying during validation, these codes did not correspond to actual traumatic intracranial hemorrhage visualized on cranial CT. We did not exclude patients who had preinjury anticoagulant or antiplatelet use. Given the inclusion criteria for all trauma registries (Table E1, available online at http://www.annemergmed.com), all eligible patients for this study should be included in registries.
Data Collection and Processing
Variables collected from each trauma registry included subject age, sex, initial ED GCS score, initial ED systolic blood pressure, length of hospital and ICU stay, ED and inhospital procedures, ICD-9 diagnosis codes, mortality, and ED and hospital disposition. Data on intrahospital transfers (eg, ward to ICU or observation unit to ICU) were not available. An Abbreviated Injury Score for head and neck, face, chest, abdomen, extremities, and external body regions and the overall Injury Severity Score were also collected from trauma registries.20 These calculations were previously entered into the trauma registries by data abstractors trained in performing them. The Abbreviated Injury Score and Injury Severity Score are scoring systems developed to measure injury severity according to anatomic injuries divided by body regions.20 Anonymous data files from the sites were transferred to the coordinating site.
Key variables were ascertained at each site to evaluate the reliability of the registry data and identify any potential systematic errors. Twenty-five subjects were randomly chosen from each site for manual reabstraction. The presence of traumatic intracranial hemorrhage, age, initial ED GCS score, ED disposition, presence of a critical care intervention, and mortality were abstracted from the medical record with a standardized data collection form and compared to trauma registry variables.
Outcome Measures
The primary outcome measure was initial ICU admission from the ED. The secondary outcome measure was the proportion of subjects receiving a critical care intervention at any point during ED care or hospitalization. A critical care intervention represented specific interventions or patient conditions that would warrant intensive care monitoring or management (Table 1).5,21–25 This list of interventions was derived and modified from the Task Force of American College of Critical Care Medicine Guidelines for ICU admission and has previously been used to define the need for ICU admission.9,21,26
Table 1.
List of critical care interventions.
| Critical Care Intervention | Definition |
|---|---|
| Mechanical ventilation21,25 | Use of mechanical ventilation for acute respiratory failure |
| Neurosurgical intervention21,23,24 | Use of hyperosmotic agents for elevated intracranial pressure, intracranial pressure monitoring or brain oxygen probe, intraventricular catheters, intracranial drains, placement of a burr hole, craniotomy/craniectomy |
| Vasopressor or inotropic use21,25 | Use of dopamine, norepinephrine, epinephrine, dobutamine, phenylephrine, or vasopressin for hemodynamic instability |
| Transfusion of blood products21,22,25 | Use of packed RBCs, platelets, cryoprecipitate, or fresh frozen plasma |
| Invasive monitoring21,25 | Monitoring with a central venous or arterial catheter for hemodynamic instability |
Primary Data Analysis
Data files in different formats (eg, XML, text files, comma delimited) were reformatted and recoded with standardized National Trauma Data Standard definitions and coding for variables, using Stata statistical software (version 11.0; StataCorp, College Station, TX). After checks for nonsensible values were completed, interval data were reported as the mean and SD or median with interquartile ranges. Proportions were presented with 95% confidence intervals (CIs). The variability between sites in ED disposition and ICU patients not receiving a critical care intervention was compared with descriptive statistics. Independent variables associated with ICU admission were tested for significance (P<.05) with a random-effects multivariable logistic regression model. Variables included in the regression model were age (continuous variable), male sex, initial ED systolic blood pressure less than 90 mm Hg, Injury Severity Score, and site. Indicator variables were created for categorical variables and compared with the reference standard (selected according to highest prevalence). Multiple imputation was performed for variables with greater than 1% of missing data; otherwise, missing data were handled with complete-case analysis.27,28 The postestimation overall effect of site (categorical variable) was tested with the Wald test of simple linear hypotheses. Reliability of key variables was measured with Cohen’s κ coefficient, with substantial agreement defined as a κ greater than 0.6.29
Sensitivity analyses were conducted to evaluate potential sources of biases. Analyses included (1) patient characteristic differences between included patients and those missing ED GCS or Injury Severity Score data; (2) the distribution of patients with missing ED disposition data between sites; (3) patient characteristic differences between patients with Abbreviated Injury Score head scores, missing scores, and potentially miscoded scores (Abbreviated Injury Score for the head of 2); and (4) ED disposition with expanded inclusion criteria defining minor traumatic intracranial hemorrhage (addition of patients with GCS score of 15, Injury Severity Score less than 25, and Abbreviated Injury Score for the head of 4).
RESULTS
Characteristics of Study Subjects
Of the 11,240 trauma registry adult subjects with traumatic intracranial hemorrhage from the 8 sites, 771 (6.9%) were excluded for missing ED GCS score or Injury Severity Score (Figure 1). Of the remaining subjects, 1,412 (13%) met criteria for minor traumatic intracranial hemorrhage (initial ED GCS score of 15 and an Injury Severity Score less than 16). Within the cohort of minor traumatic intracranial hemorrhage, the mean age was 48 years (SD 20 years), 67% were male patients (95% CI 65% to 70%), median Injury Severity Score was 10 (interquartile range 9 to 11), and there were 3 deaths (0.21%; 95% CI 0.04% to 0.62%). Patient characteristics and severity of injury for individual sites are detailed in Table 2.
Figure 1.
Flowchart.
*Minor traumatic intracranial hemorrhage (tICH) is defined as an initial ED GCS score of 15 and an Injury Severity Score (ISS) less than 16.
Table 2.
Characteristics of patients with minor traumatic intracranial hemorrhage, by site.
| Variable | All n=1,412 | Site
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 1, n=155 | 2, n=312 | 3, n=264 | 4, n=45 | 5, n=198 | 6, n=69 | 7, n=32 | 8, n=337 | ||
| Age, mean (SD), y | 48 (20) | 48 (21) | 54 (22) | 47 (19) | 54 (22) | 46 (20) | 58 (22) | 50 (22) | 42 (17) |
| Male (95% CI), % | 67 (65–70) | 67 (58–74) | 59 (53–64) | 71 (65–76) | 64 (49–78) | 69 (62–76) | 69 (62–76) | 69 (50–84) | 73 (68–78) |
| Initial ED SBP (SD), mean | 141 (24) | 136 (24) | 143 (23) | 137 (23) | 142 (22) | 135 (20) | 139 (22) | 145 (30) | 148 (27) |
| AIS head (IQR), median | 3 (3, 3) | 2 (2, 3) | 3 (3, 3) | 2 (2, 3) | 3 (3, 3) | n/a | 3 (3, 3) | 3 (3, 3) | 3 (3, 3) |
| ISS (IQR), median | 10 (9, 11) | 10 (9, 11) | 10 (10, 11) | 10 (6, 11) | 10 (10, 10) | 9 (9, 11) | 10 (9, 10) | 10 (10, 10) | 10 (9, 13) |
| Mortality, No. (%) | 3 (0.21) | 1 (0.64) | 0 | 0 | 0 | 2 (1.0) | 0 | 0 | 0 |
| Discharged from hospital home (95% CI), % | 88 (86–90) | 89 (83–93) | 88 (83–91) | 85 (80–89) | 87 (73–95) | 85 (79–89) | 86 (75–93) | 84 (67–95) | 93 (90–96) |
| Discharged from hospital to intermediate care facility (95% CI), % | 7.2 (5.9–8.7) | 9.1 (5.1–15) | 9.9 (6.9–14) | 6.8 (4.1–11) | 11 (3.7–24) | 13 (8.5–18) | 12 (5.1–22) | 16 (5.3–33) | 6.7 (4.3–9.9) |
| Discharged from hospital to jail/ psychiatric center/other (95% CI), % | 4.6 (3.6–5.9) | 1.3 (0.15–4.6) | 2.6 (1.1–5.0) | 8.0 (5.0–12) | 2.2 (0.05–12) | 1.5 (0.32–4.5) | 2.9 (0.35–10) | 0 (0–11)* | 0 (0–1.1)* |
| Hospital length of stay (IQR), median | 2 (1, 3) | 2 (2, 3) | 1 (1, 3) | 1 (2, 4) | 2 (1, 3) | 2 (1, 3) | 2 (1, 3) | 3 (2, 4) | 2 (1, 3) |
| ICU length of stay (IQR), median | 1 (0, 1) | 1 (1, 1) | 1 (1, 1) | 0 (0, 0) | 1 (1, 1) | 1 (1, 2) | 1 (0, 1) | 1 (1, 2) | 1 (0, 1) |
SBP, Systolic blood pressure; AIS, Abbreviated Injury Score; IQR, interquartile range.
One sided, 97.5% CI.
Interrater reliability measured between manual reabstraction and registry variables demonstrated substantial agreement (κ≥0.6) for all clinical variables (Table E2, available online at http://www.annemergmed.com). Missing variables are detailed in Table E3 A and B, available online at http://www.annemergmed.com.
Main Results
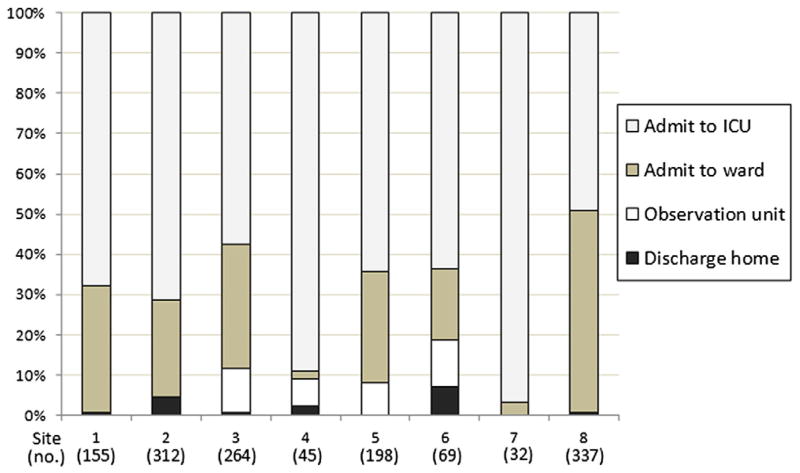
Of the 1,412 subjects, ED disposition included discharge (25 subjects; 1.8%; range between sites 0% to 7.3%), observation unit (56 subjects; 4.0%; range between sites 0% to 12%), ward admission (443 subjects; 31%; range between sites 2.2% to 50%), and ICU admission (888 patients; 63%; range between sites 50% to 97%) (Table 3 and Figure 2). Seven of 8 sites admitted more than 50% of subjects to the ICU. Two sites admitted less than 5% of patients to the ward and 5 sites discharged less than 1% of patients home. Half of the sites used an observation unit (proportion used ranged from 6.7% to 12%).
Table 3.
ED disposition by site.
| Variable | Site, No. (%)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Patients with minor tICH (% of total tICH)* | 155 (15) | 312 (9.7) | 264 (22) | 45 (6.5) | 198 (22) | 69 (17) | 32 (3.6) | 337 (18) |
| Discharged home | 1 (0.65) | 14 (4.5) | 2 (0.76) | 1 (2.2) | 0 | 5 (7.3) | 0 | 2 (0.59) |
| Admitted to observation unit | 0 | 0 | 29 (11) | 3 (6.7) | 16 (8.1) | 8 (12) | 0 | 0 |
| Admitted to the ward | 49 (32) | 75 (24) | 81 (31) | 1 (2.2) | 55 (28) | 12 (17) | 1 (3.1) | 169 (50) |
| Admitted to the ICU | 105 (68) | 223 (71) | 152 (58) | 40 (89) | 127 (64) | 44 (64) | 31 (97) | 166 (50) |
GCS score of 15 and ISS less than 16.
Figure 2.
ED disposition by site.
When independent variables were held constant in the multivariate logistic regression model, age, Injury Severity Score, and study site were significantly associated with ICU admission (Table 4). Postestimation testing evaluating the overall effect of study site on ICU admission was statistically significant (P<.001). Because only 5 subjects (0.35%) had missing data on model variables (age, male sex, initial ED systolic blood pressure <90 mm Hg, Injury Severity Score, and site), a complete-case analysis was used to handle missing data (Table E3A, available online at http://www.annemergmed.com).
Table 4.
Risk of ICU admission, n=1,407.*
| Variable | Adjusted Odds Ratio (95% CI) |
|---|---|
| Age† | 1.1 (1.0–1.1) |
| Male sex | 0.95 (0.74–1.2) |
| Initial ED SBP <90 mm Hg | 1.2 (0.22–7.1) |
| Injury Severity Score, site‡ | 1.1 (1.0–1.1) |
| 1 | 2.3 (1.5–3.4) |
| 2 | 2.3 (1.6–3.2) |
| 3 | 1.5 (1.1–2.1) |
| 4 | 7.7 (3.0–20) |
| 5 | 2.0 (1.4–2.9) |
| 6 | 1.7 (1.0–3.0) |
| 7 | 30 (4.1–226) |
Site 8 was the reference standards according to prevalence.
Per 10-year increase.
Per point increase.
Forty-four patients (3.1%) received a critical care intervention during the ED visit or hospitalization. The most common critical care interventions were mechanical ventilation (22 patients; 1.6%) and blood product transfusion (15 patients; 1.1%). Eight hundred forty-seven of 888 (95%) patients admitted to the ICU did not receive a critical care intervention, whereas 3 of 524 (0.57%) patients discharged or admitted to a non-ICU setting received a critical care intervention (all received a blood product transfusion). Critical care interventions were more likely in those admitted to the ICU (41/888; 4.6%; 95% CI 3.3% to 6.2%) than those not admitted to the ICU (3/524; 0.57%; 95% CI 0.12% to 1.7%) Critical care interventions by site are detailed in Table 5.
Table 5.
Critical care interventions by site.
| Variable | Site, No. (%)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Any CCI | 8 (5.2) | 0 | 3 (1.1) | 0 | 11* (5.6) | 9 (13) | 1 (3.1) | 12 (3.6) |
| Mechanical ventilation | 3 (1.9) | 0 | 3 (1.1) | 0 | 4 (2.0) | 2 (2.9) | 1 (3.1) | 9 (2.7) |
| Neurosurgical intervention | 1 (0.64) | 0 | 0 | 0 | 3 (1.5) | 0 | 0 | 2 (0.59) |
| Blood product transfusion | 2 (1.3) | 0 | 0 | 0 | 5 (2.5) | 7 (10) | 0 | 1 (0.30) |
| Vasopressor/inotrope use | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Invasive monitoring | 2 (1.3) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Admitted to ICU but no CCI during hospitalization | 97 (92) | 223 (100) | 149 (98) | 40 (100) | 119 (94) | 35 (80) | 30 (97) | 154 (93) |
| Disposition to home/observation unit/ward with CCI during hospitalization | 0 | 0 | 0 | 0 | 3 (4.2) | 0 | 0 | 0 |
CCI, Critical care intervention.
One patient received 2 CCIs.
Sensitivity Analyses
Patients with missing inclusion criteria data (ED GCS or Injury Severity Score) had more severe injuries (mortality 16%) compared with patients included in the primary analysis (mortality 0.21%) (Table E4A, available online at http://www.annemergmed.com). Seventeen patients with missing ED disposition data were distributed across 4 sites (11 patients from site 3, representing 4.2% of included patients from that site) (Table E4B, available online at http://www.annemergmed.com). Comparison of patients with Abbreviated Injury Score head scores included, missing, and potentially miscoded demonstrated similar patient characteristics and ED disposition proportions (Table E4C, available online at http://www.annemergmed.com). Expansion of the inclusion criteria defining minor traumatic intracranial hemorrhage demonstrated similar ED disposition proportions to the primary analysis (Tables E4D and E).
LIMITATIONS
Our results should be interpreted in the context of certain limitations. This study is retrospective and is subject to the limitations of medical record review.30 We did use a number of strategies to minimize potential biases commonly associated with trauma registries.16 An audit at each site ascertained the reliability of key variables. The importance of conducting this audit was highlighted by differences in ICD-9 coding between sites and represents a key advantage over the use of a national trauma registry.16 We also conducted analyses of missing and potentially miscoded data. Nearly 7% of patients were missing data on initial ED GCS score or Injury Severity Score; however, these patients had more severe injuries compared with patients included in the analysis (Table E4A, available online at http://www.annemergmed.com) and would likely not meet minor traumatic intracranial hemorrhage criteria. An additional 17 patients (1.2%) with minor traumatic intracranial hemorrhage were missing data on ED disposition and thus were excluded from analysis. The study conclusions, however, would not change had these patients been included (Table E4B, available online at http://www.annemergmed.com). All traumatic intracranial hemorrhage should correspond to an Abbreviated Injury Score for the head of 3 or higher20; however, the median Abbreviated Injury Score for the head at sites 1 and 3 was 2 (Table 2). Comparison of included patients with an Abbreviated Injury Score for the head of 2, greater than 2, and missing showed no significant differences in age, sex, initial ED systolic blood pressure, mortality, and ED disposition; thus, Abbreviated Injury Scores of 2 for the head are likely solely a result of a miscoded score rather than an error in the coding of traumatic intracranial hemorrhage (ICD-9 miscoded) (Table E4C, available online at http://www.annemergmed.com).
We do not have data on patients at admission from the ED, which would more accurately reflect the status of the patient at admission because patients may deteriorate or improve during their ED course. In addition, we do not have data on CT characteristics, repeated CT imaging, and anticoagulation state. Because the Injury Severity Score is calculated at hospital discharge, its use as part of the inclusion criteria may exclude patients who initially may have minor traumatic intracranial hemorrhage at admission but whose hemorrhage progressed, leading to a higher Injury Severity Score. In addition, the use of an Injury Severity Score less than 16 as a surrogate for isolated head injury may exclude patients with more severe head injuries (Abbreviated Injury Score of 4 or more for the head). However, including patients with head injury and higher levels of Injury Severity Score (Table E4D, available online at http://www.annemergmed.com) or eliminating Injury Severity Score as part of the inclusion criteria (Table E4E, available online at http://www.annemergmed.com) demonstrates variability of ICU use similar to that of the study inclusion criteria (Table 3).
This study was conducted at American College of Surgeons Level I trauma centers in which the severity of injury, hospital resources, and management of traumatic intracranial hemorrhage might not be generalizable to lower-level or nontrauma centers. Additionally, individual site resources (eg, nursing to patient ratios, availability of hospital and ICU beds) and local setting (eg, volume of trauma patients, patient and physician preferences, community demographics, medicolegal risk, previous isolated adverse incidents) at each site may differ and account for variability in the ICU use we identified. However, because these sites are relatively homogenous (academic Level I trauma centers in the western United States), care would be expected to be similar. Additionally, inclusion in the trauma registry requires evaluation by the trauma service (Table E1, available online at http://www.annemergmed.com). Although it is general practice at all sites that patients with traumatic intracranial hemorrhage be evaluated by the trauma service, it is possible that very low-risk patients were not included in the trauma registry.
The use of critical care intervention as a surrogate for requiring ICU admission does have limitations. The list of critical care interventions is based on a combination of previous literature and expert opinion.9,21,26 It is possible that there are unmeasured advantages with ICU care that prevented a critical care intervention from occurring. Although this is likely for medical patients with multiple complex conditions, it is less likely in patients with traumatic intracranial hemorrhage who are simply being observed in the ICU.
DISCUSSION
Our results demonstrate wide variability in ICU use in alert, adult patients with minor traumatic intracranial hemorrhage across a consortium of Level I trauma centers. Initial ICU admission ranged from 50% to 97%, with trauma center site being independently associated with ICU admission in this population. Moreover, there was variability among sites in the use of observation units, as well as the practice of discharging these patients from the ED. Finally, and perhaps most important, a large proportion of patients admitted to the ICU never required a critical care intervention during hospitalization. This finding was consistent across all centers and suggests substantial inefficiency in ICU resource use.
Because of concerns that differences in injury severity between sites (see Table E5, available online at http://www.annemergmed.com, for patient characteristics from the entire cohort) may have accounted for the variability of ICU use (ie, sites with a higher proportion of patients with more severe traumatic intracranial hemorrhage would likely have higher ICU use), we analyzed patients with minor traumatic intracranial hemorrhage (GCS score of 15 and an Injury Severity Score less than 16). This represents a homogenous, “well-appearing” cohort of patients with minor traumatic intracranial hemorrhage who have a low prevalence of death and neurosurgical interventions.7,8 Additionally, patients with an Injury Severity Score less than 16 are likely to have an isolated head injury, thus minimizing the possibility that patients are admitted to the ICU for significant, nonhead injuries. We did not compare the variablity of ICU use among moderate or severe traumatic intracranial hemorrhage strata because these patients have higher morbidity and mortality and a much higher likelihood of requiring critical care interventions and ICU admission.5
Several factors may account for the variability of ICU use. Local admission practices may dictate that all patients with traumatic intracranial hemorrhage be admitted to the ICU. Two sites in particular admitted greater than 85% of patients to the ICU, suggesting that such a practice occurs. Although there were no differences in key variables across sites (Table 2), unmeasured differences in injury severity (including overall clinical impression), not recorded in registry data, may have existed and could account for some of the variability of ICU use. This unmeasured effect is also apparent, given that those admitted to the ICU had a higher rate of critical care interventions (4.6%) than those admitted to a non-ICU setting (0.57%). Additionally, sites with a higher proportion of well-appearing patients may be more likely to develop alternative strategies to uniform ICU admission (eg, observation units, observe and discharge from ED, admission to the hospital ward).
Variability of ICU use has important implications. ICU resources are limited (only 8% of hospital beds) and costly (one third of acute hospital charges).31 Sites with a uniform ICU admission policy for all patients with traumatic intracranial hemorrhage may admit many patients to the ICU who ultimately do not require ICU-level resources. Inappropriate ICU admissions has broad public health relevance, given its association with adverse patient outcomes for admitted patients, prolonged ED boarding times among all patients awaiting ICU admission, and ICU and ED crowding.32–34 Within our study population, more than 95% of patients admitted to the ICU never received a critical care intervention during hospitalization, suggesting room for improvement in the use of intensive care resources. Sites with the highest proportion of patients admitted to the ICU also had the highest proportion of patients admitted to the ICU who never received a critical care intervention during hospitalization.
To our knowledge, this is the first study evaluating the variability of disease-specific ICU use across multiple sites. Although previous guidelines recommend general criteria for ICU admission,21,35 specific guidelines for ICU admission of patients with traumatic intracranial hemorrhage are vague and inconsistent.3,36
Appropriate use of ICU resources is important to provide safe and efficient health care. It is estimated that eliminating deviation from “optimal care” could cut up to 30% of health care costs in the United States without reducing quality.37 Future studies should be directed at improving ICU use for all trauma patients. Identification of a low-risk group of patients with traumatic intracranial hemorrhage who may be safely discharged home or admitted to a non-ICU setting would improve ICU use.
In conclusion, across a consortium of trauma centers we identified wide variability in ICU use within a cohort of similarly injured patients with traumatic intracranial hemorrhage. Moreover, a large proportion of patients with traumatic intracranial hemorrhage who are admitted to the ICU never required critical care intervention, indicating a need to improve use of the ICU for patients with traumatic intracranial hemorrhage.
Supplementary Material
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. This project was supported by the UC Davis Clinical and Translational Science Center (grant UL1 RR024146), Colorado Clinical and Translational Science Institute (grant UL1 RR025780), Oregon Clinical and Translational Research Institute (grant UL1 RR024140), Stanford Center for Clinical and Translational Education and Research (grant 1UL1 RR025744), Institute of Translational Health Sciences at the University of Washington (grant UL1 RR025014), University of Utah Center for Clinical and Translational Science (grants UL1-RR025764 and C06-RR11234), UCSF Clinical and Translational Science Institute (grant UL1 RR024131), and the Robert Wood Johnson Foundation (RWJF) Physician Faculty Scholars Program. All Clinical and Translational Science Awards are from the National Center for Research Resources (now National Center for Advancing Translational Sciences [NCATS]), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The NIH and the RWJF had no role in the design and conduct of the study, in the analysis or interpretation of the data, or in the preparation of the data. Dr. Nishijima had full access to all the data and had final responsibility for the decision to submit for publication. The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official view of NCATS or NIH. Information on NCATS is available at http://www.ncats.nih.gov/.Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Author contributions: DKN and JFH conceived the study, obtained research funding, and analyzed the data. All authors contributed to the design of the study. DKN, JSH, CDN, KS, DS, and CAG conducted data collection and supervised conduct of the study. DN drafted the article, and all authors contributed to its revision. DKN takes responsibility for the paper as a whole.
References
- 1.Ghajar J. Traumatic brain injury. Lancet. 2000;356:923–929. doi: 10.1016/S0140-6736(00)02689-1. [DOI] [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2004. [Google Scholar]
- 3.Vos PE, Battistin L, Birbamer G, et al. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9:207–219. doi: 10.1046/j.1468-1331.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 4.Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294:1511–1518. doi: 10.1001/jama.294.12.1511. [DOI] [PubMed] [Google Scholar]
- 5.Wang MC, Linnau KF, Tirschwell DL, et al. Utility of repeat head computed tomography after blunt head trauma: a systematic review. J Trauma. 2006;61:226–233. doi: 10.1097/01.ta.0000197385.18452.89. [DOI] [PubMed] [Google Scholar]
- 6.Graham DI, Ford I, Adams JH, et al. Ischaemic brain damage is still common in fatal non-missile head injury. J Neurol Neurosurg Psychiatry. 1989;52:346–350. doi: 10.1136/jnnp.52.3.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huynh T, Jacobs DG, Dix S, et al. Utility of neurosurgical consultation for mild traumatic brain injury. Am Surg. 2006;72:1162–1165. discussion 1166–1167. [PubMed] [Google Scholar]
- 8.Sifri ZC, Livingston DH, Lavery RF, et al. Value of repeat cranial computed axial tomography scanning in patients with minimal head injury. Am J Surg. 2004;187:338–342. doi: 10.1016/j.amjsurg.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Nishijima DK, Sena MJ, Holmes JF. Identification of low-risk patients with traumatic brain injury and intracranial hemorrhage who do not need intensive care unit admission. J Trauma. 2011;70:E101–107. doi: 10.1097/TA.0b013e3181e88bcb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hukkelhoven CW, Steyerberg EW, Habbema JD, et al. Admission of patients with severe and moderate traumatic brain injury to specialized ICU facilities: a search for triage criteria. Intensive Care Med. 2005;31:799–806. doi: 10.1007/s00134-005-2628-y. [DOI] [PubMed] [Google Scholar]
- 11.Schaller B, Evangelopoulos DS, Muller C, et al. Do we really need 24-h observation for patients with minimal brain injury and small intracranial bleeding? The Bernese Trauma Unit Protocol. Emerg Med J. 2010;27:537–539. doi: 10.1136/emj.2009.073031. [DOI] [PubMed] [Google Scholar]
- 12.Welch RD. Management of traumatically injured patients in the emergency department observation unit. Emerg Med Clin North Am. 2001;19:137–154. doi: 10.1016/s0733-8627(05)70172-3. [DOI] [PubMed] [Google Scholar]
- 13. [Accessed February 2, 2012.];Clinical and Translational Science Awards. Available at: https://www.ctsacentral.org/
- 14.Newgard CD, Zive D, Holmes JF, et al. A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213:709–721. doi: 10.1016/j.jamcollsurg.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Trauma Data Standard of the National Trauma Data Bank. [Accessed February 2, 2012.]; Available at: http://www.ntdsdictionary.org/dataElements/datasetDictionary.html.
- 16.Zehtabchi S, Nishijima DK, McKay MP, et al. Trauma registries: history, logistics, limitations, and contributions to emergency medicine research. Acad Emerg Med. 2011;18:637–643. doi: 10.1111/j.1553-2712.2011.01083.x. [DOI] [PubMed] [Google Scholar]
- 17.Bolorunduro OB, Villegas C, Oyetunji TA, et al. Validating the Injury Severity Score (ISS) in different populations: ISS predicts mortality better among Hispanics and females. J Surg Res. 2011;166:40–44. doi: 10.1016/j.jss.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Salottolo K, Settell A, Uribe P, et al. The impact of the AIS 2005 revision on injury severity scores and clinical outcome measures. Injury. 2009;40:999–1003. doi: 10.1016/j.injury.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 19.US Department of Health and Human Services. International Classification of Diseases, Ninth Revision, Clinical Modification, Sixth Revision. Washington, DC: US Department of Health and Human Services; 1997. [Google Scholar]
- 20.Copes WS, Champion HR, Sacco WJ, et al. The Injury Severity Score revisited. J Trauma. 1988;28:69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Guidelines for intensive care unit admission, discharge, and triage. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med. 1999;27:633–638. [PubMed] [Google Scholar]
- 22.Mina AA, Knipfer JF, Park DY, et al. Intracranial complications of preinjury anticoagulation in trauma patients with head injury. J Trauma. 2002;53:668–672. doi: 10.1097/00005373-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. IX. Cerebral perfusion thresholds. J Neurotrauma. 2007;24(suppl 1):S59–S64. doi: 10.1089/neu.2007.9987. [DOI] [PubMed] [Google Scholar]
- 24.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007;24(suppl 1):S55–S58. doi: 10.1089/neu.2007.9988. [DOI] [PubMed] [Google Scholar]
- 25.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. I. Blood pressure and oxygenation. J Neurotrauma. 2007;24(suppl 1):S7–S13. doi: 10.1089/neu.2007.9995. [DOI] [PubMed] [Google Scholar]
- 26.Nishijima DK, Shahlaie K, Echeverri A, et al. A clinical decision rule to predict adult patients with traumatic intracranial haemorrhage who do not require intensive care unit admission. Injury. 2012;43:1827–1832. doi: 10.1016/j.injury.2011.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research—part 2: multiple imputation. Acad Emerg Med. 2007;14:669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 28.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 29.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–363. [PubMed] [Google Scholar]
- 30.Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45:448–451. doi: 10.1016/j.annemergmed.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 31.Groeger JS, Guntupalli KK, Strosberg M, et al. Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization. Crit Care Med. 1993;21:279–291. doi: 10.1097/00003246-199302000-00022. [DOI] [PubMed] [Google Scholar]
- 32.Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 33.Escher M, Perneger TV, Chevrolet JC. National questionnaire survey on what influences doctors’ decisions about admission to intensive care. BMJ. 2004;329:425. doi: 10.1136/bmj.329.7463.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robert R, Reignier J, Tournoux-Facon C, et al. Refusal of ICU admission due to a full unit: impact on mortality. Am J Resp Crit Care Med. 2012;185:1081–1087. doi: 10.1164/rccm.201104-0729OC. [DOI] [PubMed] [Google Scholar]
- 35.Bone RC, McElwee NE, Eubanks DH, et al. Analysis of indications for intensive care unit admission. Clinical efficacy assessment project: American College of Physicians. Chest. 1993;104:1806–1811. doi: 10.1378/chest.104.6.1806. [DOI] [PubMed] [Google Scholar]
- 36.Head injury: triage, assessment, investigation and early management of head injury in infants, children, and adults. National Collaborative Centre for Acute Care and National Institute for Health and Clinical Excellence; [Accessed December 12, 2010.]. Available at: http://www.nice.org.uk/nicemedia/pdf/CG56NICEGuideline.pdf. [Google Scholar]
- 37.Baker NW, Resar RK, Griffin FA, et al. Reducing Costs Through the Appropriate Use of Specialty Services. Cambridge, MA: Institute for Health Care Improvement; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.