Abstract
Objective
The most rapidly growing population of patients undergoing total knee arthroplasty (TKA) is under the age of 65. The objective of this study was to gain insight into the factors influencing physicians’ recommendations for persons in this age group with moderate osteoarthritis (OA).
Methods
Rheumatologists and orthopedic surgeons attending national meetings were asked to complete a survey including a standardized scenario of a 62 year old person with knee OA who has moderate knee pain limiting strenuous activity despite medical management. We used an experimental 2×2×2 design to examine the effects of gender, employment status and severity of radiographic OA on physicians’ recommendations. Each physician was asked to rate a single scenario.
Results
The percent of physicians recommending TKA varied from 30% to 55% for scenarios describing a patient with mild radiographic OA, and from 39% to 71% for scenarios describing a patient with moderate radiographic OA. Surgeons were less likely to recommend TKA for women compared to men of the same age, employment status, symptom severity and functional status, and x-rays. Rheumatologists practicing in academic settings were more likely to recommend TKA compared to those practicing in non-academic settings, and American surgeons were more likely to recommend TKA compared to their European counterparts.
Conclusion
Orthopedic surgeons and rheumatologists vary significantly in their recommendations for patients with moderate knee pain and functional limitations. Both patient and physician characteristics influence physicians’ recommendations and rheumatologists and orthopedic surgeons display different patterns of decision-making.
Keywords: Total Joint Arthroplasty, Practice Patterns, Physician Bias, Unwarranted Variability
Total knee arthroplasty (TKA) is an effective treatment option for patients with knee osteoarthritis (OA) and is currently one of the most commonly performed elective surgical procedures worldwide (1). The number of TKAs performed in the US per year has been rising substantially since 1990 (2, 3). This rise was anticipated given the increasing prevalence of older adults in the population. However, while rates of TKA are increasing among all age groups, the most rapidly growing population of patients undergoing this procedure are those under the age of 65 years (3).
Because there is no consensus regarding the indications for TKA, the number of procedures performed varies significantly across geographic regions (1). Whereas rates are expected to vary based on patients’ preferences, disease severity and comorbidity, the number of TKAs performed is also influenced by unwarranted sources of variability such as patient ethnicity, gender (with women being less likely to be offered TKA) and motivation to improve function (4–8). Not surprisingly, physicians’ opinions (9) are also influential. For example, Wright et al. (10) found that orthopedic surgeons’ enthusiasm for TKA was a strong determinant of geographic variation in TKA rates in Canada. Moreover, in this study surgeons’ opinion was the only statistically significant modifiable predictor identified (p=0.0001) (10).
Given that physicians’ opinions explain a significant amount of the variability observed in TKA rates (9), and the rising rates of TKA in persons under the age of 65, the aim of this study was to identify patient and provider differences driving decisions to recommend TKA in standardized patient scenarios for whom there was uncertainty regarding the appropriateness of surgery.
METHODS
We composed scenarios to represent patients for whom there was uncertainty regarding the appropriateness criteria for TKA: i.e., patients who had moderate (that is, neither mild nor severe) pain and limitations in function and had exhausted a reasonable number (but not all) medical treatment options. Using an experimental 2×2×2 design (11), we examined the effects of gender, employment status and severity of radiographic OA on physicians’ recommendations.
We examined decision making among two groups of physicians: orthopedic surgeons and rheumatologists. We chose to include orthopedic surgeons and rheumatologists in order to permit a direct comparison between physicians that have a comparable level of expertise in the care of patients with OA. Moreover, because rheumatologists and surgeons generally act as consultants for patients with knee OA, they may approach the trade-offs between the escalating use of analgesics and TKA differently than primary care providers do.
A single research assistant approached physicians before or after concurrent oral and plenary sessions held at the American College of Rheumatology Annual Meeting (November 2011) and the American Academy of Orthopedic Surgeons Annual Meeting (February 2012). Physicians who were able to speak English were asked to complete a paper survey including a standardized scenario of a 62 year old person with knee OA who has moderate knee pain limiting strenuous activity despite medical management (Appendix A). Physicians were not informed of the purpose of the survey and were not offered any incentives. Each physician completed a single, randomly assigned scenario. Randomization was determined using a computer generated list of random numbers in blocks of 24. The scenarios were identical (in terms of pain, functional status and co-morbidities) and varied only by patient gender, employment status (business manager versus retired/housewife), and x-ray (mild versus moderate OA). The x-rays used are included in Appendix A.
Each physician was asked to rate their recommendation for TKA on a 6-point scale (1 = Very strongly recommend having a TKA and 6 = Very strongly recommend against having a TKA). Recommendation was treated as a dichotomous variable (strongly or very strongly recommend versus other). Subjects were also asked to report their age, gender, number of years in practice, country of residence, and primary practice setting. Surgeons also reported the number of TKAs performed per year (less than 15, 15–19, 20–24, or 25 or more) and rheumatologists reported the number of OA patients seen per month (less than, 10–20, more than 20). We examined the likelihood of recommending TKA among rheumatologists versus orthopedists. We used chi-square statistics to examine the associations between patient and physician characteristics with recommendations for TKA. Logistic regression models were subsequently used to determine the independent impact of each predictor on rheumatologists’ and orthopedic surgeons’ recommendations.
This study was determined by our institution’s Human Investigation Committee to be exempt from IRB approval.
ROLE OF FUNDING SOURCE
Dr. Fraenkel is supported by NIAMS K24 AR060231-01. Dr. Suter is supported in part by the Centers for Medicare and Medicaid Services Contract Number HHSM-500-2008-0025I/HHSM-500-T0001, Modification No. 000008. The funding sources had no role in the design, conduct, analyses of the study or in the preparation of the manuscript.
RESULTS
We surveyed 896 physicians (494 rheumatologists and 406 orthopedic surgeons). Among orthopedic surgeons, 54% performed 25 or more TKAs per year. About half (52%) reported practicing in a solo or group practice, 23% in a hospital/medical center-based practice, 4% in a VA hospital and 0.5% on a Prepaid Plan or HMO setting. Among rheumatologists surveyed, 54% reported seeing over 20 patients with knee OA per month. About half (51%) practice primarily in a community-based solo or group practice setting, 27% in a hospital/medical center-based practice, and 2% in a VA hospital. Additional characteristics by physician specialty are presented in Table 1. Overall, the same percent (51%) of surgeons and rheumatologists recommended TKA. However, both groups of physicians’ recommendations for TKA varied significantly across scenarios (Figure 1).
Table 1.
Rheumatologists’ and Orthopedic Surgeons’ Characteristics
| Rheumatologists (N = 494) |
Orthopedic Surgeons (N = 406) |
|
|---|---|---|
| Mean (SD) age | 48.4 (11.4) | 48.9 (10.5) |
| Mean (SD) years in practice | 17.1 (11.1) | 17.2 (10.7) |
| Female (%) | 218 (44) | 18 (4) |
| Academic Practice (%) | 98 (20) | 53 (13) |
| Practice Site (%) | ||
| Africa | 9 (2) | 4 (1) |
| Asia | 50 (10) | 24 (6) |
| Australia | 9 (2) | 4 (1) |
| Europe | 122 (25) | 68 (17) |
| Central America | 5 (1) | 6 (1) |
| Canada | 23 (5)( | 9 (2) |
| Mexico | 6 (1) | 4 (1) |
| United States | 211 (43) | 265 (65) |
| South America | 40 (8) | 19 (5) |
| Other | 15 (3) | 2 (0.5) |
Figure 1.
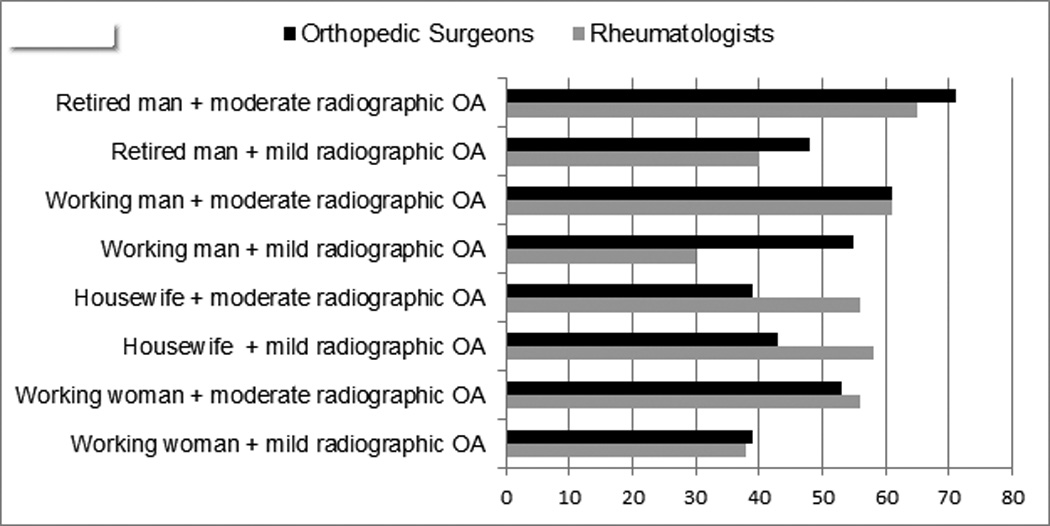
Percent of Physicians Recommending TKA for Each Scenario
Influence of patient characteristics on TKA recommendations (Table 2)
Table 2.
Influence of Patient Characteristics on Physicians’ Recommendations for TKA
| Patient Characteristics | Percent of Rheumatologists Recommending TKA | Percent of Orthopedic Surgeons Recommending TKA |
|---|---|---|
| Moderate vs. mild radiographic changes | 60 vs. 41, p<0.0001 | 56 vs. 47, p=0.05 |
| Male vs. female | 49 vs. 52, p=0.5 | 59 vs. 44, p=0.002 |
| Working outside of the home vs. retired / housewife | 47 vs. 55, p=0.07 | 52 vs. 51, p=0.8 |
As expected, both groups recommended TKA more frequently for scenarios including more severe radiographic OA; however, this feature had a greater influence among rheumatologists (difference = 19%, χ2 = 16.3, p<0.0001) than orthopedic surgeons (difference = 9%, χ2 = 3.91, p=0.048). Patient gender did not influence rheumatologists’ recommendations. In contrast, orthopedic surgeons were less likely to recommend TKA for female compared to male patients. Male rheumatologists recommended TKA for 49% of the male patient scenarios versus 50% of the female patient scenarios (p=0.8); whereas male orthopedic surgeons recommended TKA for 59% of the male compared to 43% of the female patient scenarios (p=0.001). Gender bias was not observed among female rheumatologists. The number of female orthopedic surgeons was too small (n=18) to examine the influence of patient gender on their recommendations. Patient employment status did not significantly influence rheumatologists’ or orthopedic surgeons’ recommendations.
Influence of physician characteristics on TKA recommendations (Table 3)
Table 3.
Influence of Physician Characteristics on Recommendations for TKA
| Physician Characteristics | Percent of Rheumatologists Recommending TKA | Percent of Orthopedic Surgeons Recommending TKA |
|---|---|---|
| Age (≤ 40 vs. > 40) | 61 vs. 46, p=0.002 | 60 vs. 48, p=0.03 |
| Practice Setting (Academic vs. non-academic) | 63 vs. 48, p=0.006 | 43 vs. 53, p=0.2 |
| Site (United States vs. Europe) | 52 vs. 49, p=0.6 | 52 vs. 34, p=0.007 |
Physicians’ demographic characteristics had variable influence on TKA recommendations. Younger physicians, regardless of specialty, were more likely to recommend TKA (Figure 2). The mean (SD) age of rheumatologists of those who did versus did not recommend TKA was and 46.8 (11.6) and 50.1 (11.0), p=0.002, respectively. The mean (SD) age of orthopedic surgeons for and against TKA was 47.8 (11.0) and 50.1 (9.8) p=0.026, respectively. The effect of physician gender could not be definitively examined among orthopedic surgeons because of the small number of female orthopedic surgeons. Nonetheless, we found no effect of physician gender among rheumatologists. Academic rheumatologists were more likely to recommend TKA compared to rheumatologists working primarily in non-academic settings; whereas academic orthopedic surgeons were less likely. The latter did not, however, reach statistical significance. Rheumatologists’ recommendations for TKA did not vary by geographic location. In contrast, American surgeons were substantially more likely to recommend TKA compared to their European counterparts. Other countries could not be examined because of the small number of participants (see Table 1).
Figure 2.
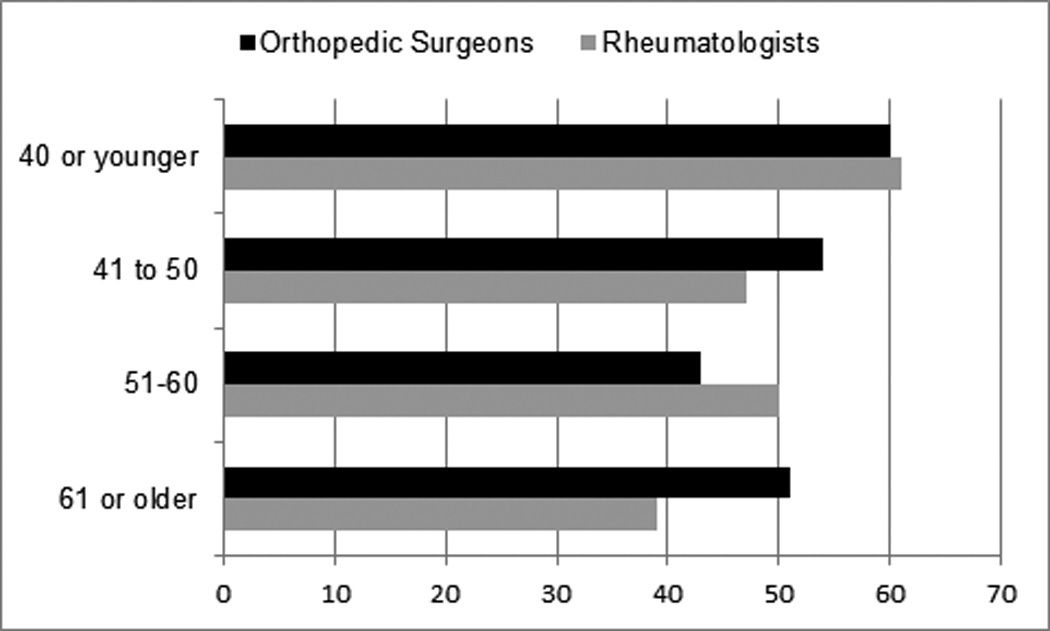
Percent of Physicians by Age Group Recommending TKA
Multivariate Analysis
Rheumatologists’ recommendations for TKA were independently and significantly associated with younger physician age, academic setting and greater radiographic severity in a logistic regression model including all three variables (Table 4). Among orthopedic surgeons, male patients, greater radiographic severity and practicing in the US, remained significantly associated with recommendation for TKA in a multivariable model; whereas physician age was of borderline significance.
Table 4.
Influence of Patient and Physicians Characteristics on Recommendations for TKA (Multivariate analyses)
| Adjusted Odds Ratio (95% Confidence Interval) |
|
|---|---|
| Rheumatologists1 | |
| Moderate vs. mild radiographic changes | 2.15 (1.49 – 3.11) |
| Age of surgeon, per year increase | 0.98 (0.96 – 0.99) |
| Academic vs. non-academic practice | 1.75 (1.09 – 2.82) |
| Orthopedic Surgeons2 | |
| Female vs. male patients | 0.55 (0.37 – 0.82) |
| Moderate vs. mild radiographic changes | 1.51 (1.01 – 2.26) |
| Age of surgeon, per year increase | 0.98 (0.96 – 1.00) |
| European vs. American | 0.42 (0.24 – 0.74) |
Model contains the three variables found to be significant in unadjusted analyses: radiographic severity, age of surgeon, practice site.
Model contains the four variables found to be significant in unadjusted analyses: patient gender, radiographic severity, age of surgeon, geographical location.
DISCUSSION
In this study, orthopedic surgeons and rheumatologists varied significantly in their recommendations for patients with mild to moderate radiographic knee OA and moderate pain and functional limitations. Both patient and physician characteristics influenced recommendations, and rheumatologists and orthopedic surgeons displayed different patterns of decision-making.
Most of the variability between physician groups occurred for patients with mild radiographic disease. The only significant difference between rheumatologists and orthopedic surgeons for patients with moderate radiographic disease was seen in the scenario describing a housewife, for which fewer orthopedic surgeons recommended TKA compared to rheumatologists. A significant gender bias against female patients was observed among orthopedic surgeons even after controlling for radiographic severity and employment status. For example, orthopedic surgeons recommended TKA for 55% of working men and 39% of working women of the same age and having identical symptoms, functional limitations, and x-rays. Borkhoff, et al. (6) found that Canadian physicians (29 orthopedic surgeons and 38 family physicians) were less likely to recommend TKA when presented with standardized female compared to male patients. In contrast, gender bias in the present study was observed only among surgeons. Moreover, we did not detect this bias when we restricted the analyses to male rheumatologists.
Our study does not provide insights as to why rheumatologists did not exhibit the same gender bias as surgeons or as family physicians (6). Orthopedic surgeons may be more strongly influenced by the results of some studies published in subspecialty surgical journals demonstrating differences in TKA outcomes between men and women. For example, several studies have shown that, while women have similar improvements in pain and function as men following TKA, their postoperative absolute pain and function scores are poorer, because they have worse preoperative scores (12–14). Some data, suggest that women may actually fare better than men after TKA. Liebs et al (15) found that women recover more quickly following TKA, while Singh et al (16) demonstrated higher rates of wound infections, revision rates, and mortality in men compared to women. Whether these findings will alter the gender differences seen in this study should be examined in future research.
Both rheumatologists’ and orthopedic surgeons’ recommendations were influenced by radiographic changes; though, the difference between the x-rays used in this study had greater impact on rheumatologists’ than orthopedic surgeons’ recommendations. While the approaches used are different, these results are consistent with a recent survey in which 68% of orthopedic surgeons reported that their decision to perform TKA, and 77% of rheumatologists and family physicians reported that their decision to refer for TKA, was influenced by radiographic severity (9). These findings suggest that referring rheumatologists may place a higher emphasis on radiographic findings compared to surgeons, perhaps because of a perceived need to ensure that surgeons will view referred patients as appropriate candidates for surgery.
The literature examining variability in physicians’ recommendations for TKA has focused primarily on patient factors (6–9); however in this study, we found that physicians’ characteristics were also important. Younger rheumatologists and orthopedic surgeons were more likely to recommend TKA compared to their older counterparts. Whether this difference reflects a generally more conservative attitude among older physicians, or specific differences in the way older and younger physicians weigh the risks and benefits related to TKA deserves further study.
Academic rheumatologists were significantly more likely than their community-based counterparts to recommend TKA. Potential explanations include the possibility that academic rheumatologists have a more favorable view of the outcomes associated with TKA or, alternatively, a less favorable view of the medical treatment options available for knee OA. There were no differences in recommendations among rheumatologists by geographic location; however, European surgeons were much less likely to recommend TKA compared to American surgeons, suggesting that site-related factors such as practice norms, reimbursement, and/or insurance coverage may influence surgeons’ TKA recommendations.
This study has several important strengths. We were able to survey a large group of physicians. The use of a 2×2×2 design allowed us to isolate the impact of both patient and physician factors on TKA recommendations. Each subject answered a single scenario, thus our findings were not influenced by clustering or ordering effects.
Several limitations should be noted. The use of standardized scenarios, while enabling us to systematically vary patient characteristics, cannot replicate the complexity of decision making in clinical practice. Although we surveyed a large number of physicians, most of whom spend the majority of their time in clinical practice, the study population represents a convenience sample of consecutively approached volunteers which limits generalizability. Our classification of volume did not allow us to discriminate between surgeons with high volumes and those with more moderate sized practices. We chose to compare “housewife” to “retired man” in order to represent typical gender roles. These terms, as well as choice of employment (business manager) may be associated with specific socioeconomic stereotypes. This bias, however, would not have affected the gender bias seen for working male and female patients. Lastly, our results can only be generalized to the specific patient characteristics represented in the specified scenario. Whether the variability found in this study would be replicated in patients with other characteristics (for example younger than the age of 60) requires further research.
This study adds to the literature demonstrating the influence of physicians’ opinions on recommendations for TKA and improves our understanding of the physician factors underlying the unwarranted variability associated with its use. Without explicit appropriateness criteria for TKA, the recommendations that patients receive are likely to remain inconsistent.
ACKNOWLEDGEMENTS
Research reported in this publication was also supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR060231-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Suter is supported in part by the Centers for Medicare and Medicaid Services Contract Number HHSM-500-2008-0025I/HHSM-500-T0001, Modification No. 000008.
Appendix A
A 62 year old woman, who works full time as a manager of a small business, is referred to you for consideration of a total knee arthroplasty by her PCP.
She has had worsening right medial and lateral knee pain over the past 2 years and complains of moderate right knee pain on most days of the month. Her left knee is fine.
Although she did have some relief with NSAIDs when her symptoms began, she has not responded to recent trials of physical therapy, acetaminophen, NSAIDs, or intraarticular injections with cortisone or hyaluronic acid.
She denies any swelling, buckling, catching or locking of her knee.
She has found it increasingly difficult to travel for business. She has a moderate amount of difficulty going up and down stairs and a lot of difficulty doing heavy household chores.
Her BMI is 26 (overweight but not obese). She has well controlled hypertension and diabetes and no known coronary artery disease. She does not smoke. She lives with her husband who is healthy.
Her physical exam is normal except for a positive patello-femoral crunch sign and some medial joint line tenderness of her right knee.
Below are her recent x-rays (taken within the past month):
What would your recommendation be for this patient?
Very strongly recommend TKA
Strongly recommend TKA
Recommend TKA
Recommend against having a TKA
Strongly recommend against having a TKA
Very strongly recommend against having a TKA
A 62 year old woman, who works full time as a manager of a small business, is referred to you for consideration of a total knee arthroplasty by her PCP.
She has had worsening right medial and lateral knee pain over the past 2 years and complains of moderate right knee pain on most days of the month. Her left knee is fine.
Although she did have some relief with NSAIDs when her symptoms began, she has not responded to recent trials of physical therapy, acetaminophen, NSAIDs, or intraarticular injections with cortisone or hyaluronic acid.
She denies any swelling, buckling, catching or locking of her knee.
She has found it increasingly difficult to travel for business. She has a moderate amount of difficulty going up and down stairs and a lot of difficulty doing heavy household chores.
Her BMI is 26 (overweight but not obese). She has well controlled hypertension and diabetes and no known coronary artery disease. She does not smoke. She lives with her husband who is healthy.
Her physical exam is normal except for a positive patello-femoral crunch sign and some medial joint line tenderness of her right knee.
Below are her recent x-rays (taken within the past month):
What would your recommendation be for this patient?
Very strongly recommend TKA
Strongly recommend TKA
Recommend TKA
Recommend against having a TKA
Strongly recommend against having a TKA
Very strongly recommend against having a TKA
A 62 year old woman, who works full time as a manager of a small business, is referred to you for consideration of a total knee arthroplasty by her PCP.
She has had worsening right medial and lateral knee pain over the past 2 years and complains of moderate right knee pain on most days of the month. Her left knee is fine.
Although she did have some relief with NSAIDs when her symptoms began, she has not responded to recent trials of physical therapy, acetaminophen, NSAIDs, or intraarticular injections with cortisone or hyaluronic acid.
She denies any swelling, buckling, catching or locking of her knee.
She has found it increasingly difficult to travel for business. She has a moderate amount of difficulty going up and down stairs and a lot of difficulty doing heavy household chores.
Her BMI is 26 (overweight but not obese). She has well controlled hypertension and diabetes and no known coronary artery disease. She does not smoke. She lives with her husband who is healthy.
Her physical exam is normal except for a positive patello-femoral crunch sign and some medial joint line tenderness of her right knee.
Below are her recent x-rays (taken within the past month):
What would your recommendation be for this patient?
Very strongly recommend TKA
Strongly recommend TKA
Recommend TKA
Recommend against having a TKA
Strongly recommend against having a TKA
Very strongly recommend against having a TKA
REFERENCES
- 1.Fisher ES, Bell JE, Tomek IM, Esty AR, Goodman DC. Trends and regional variation in hip, knee, and shoulder replacement. 2010 Available from: http://www.rwjf.org/content/dam/web-assets/2010/04/trends-and-regional-variation-inhip--knee-and-shoulder-replacement. [PubMed] [Google Scholar]
- 2.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz BP, Freund DA, Heck DA, et al. Demographic variation in the rate of knee replacement: a multi-year analysis. Health Serv Res. 1996;31:125–140. [PMC free article] [PubMed] [Google Scholar]
- 5.Borkhoff CM, Hawker GA, Wright JG. Patient gender affects the referral and recommendation for total joint arthroplasty. Clin Orthop Relat Res. 2011;469:1829–1837. doi: 10.1007/s11999-011-1879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, Wright JG. Patients' gender affected physicians' clinical decisions when presented with standardized patients but not for matching paper patients. J Clin Epidemiol. 2009;62:527–541. doi: 10.1016/j.jclinepi.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Dieppe P, Basler HD, Chard J, et al. Knee replacement surgery for osteoarthritis: effectiveness, practice variations, indications and possible determinants of utilization. Rheumatology. 1999;38:73–83. doi: 10.1093/rheumatology/38.1.73. [DOI] [PubMed] [Google Scholar]
- 8.Mancuso CA, Ranawat CS, Esdaile JM, Johanson NA, Charlson ME. Indications for total hip and total knee arthroplasties. Results of orthopaedic surveys. J Arthroplasty. 1996;11:34–46. doi: 10.1016/s0883-5403(96)80159-8. [DOI] [PubMed] [Google Scholar]
- 9.Wright JG, Hawker GA, Hudak PL, et al. Variability in physician opinions about the indications for knee arthroplasty. J Arthroplasty. 2011;26:569–575. doi: 10.1016/j.arth.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 10.Wright JG, Hawker GA, Bombardier C, et al. Physician enthusiasm as an explanation for area variation in the utilization of knee replacement surgery. Med Care. 1999;37:946–956. doi: 10.1097/00005650-199909000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Cohen BH, Lea RB. Essentials of statistics for the social and behavioral sciences. Hoboken, New Jersey: John Wiley & Sons, Inc; 2004. [Google Scholar]
- 12.Ritter MA, Wing JT, Berend ME, Davis KE, Meding JB. The clinical effect of gender on outcome of total knee arthroplasty. J Arthroplasty. 2008;23:331–336. doi: 10.1016/j.arth.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 13.MacDonald SJ, Charron KD, Bourne RB, Naudie DD, McCalden RW, Rorabeck CH. Gender-specific total knee replacement: prospectively collected clinical outcomes. Clin Orthop Relat Res. 2008;466:2612–2616. doi: 10.1007/s11999-008-0430-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Connor MI. Implant survival, knee function, and pain relief after TKA: Are there differences between men and women? Clin Orthop Relat Res. 2011;469:1846–1851. doi: 10.1007/s11999-011-1782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liebs TR, Herzberg W, Roth-Kroeger AM, Rüther W, Hassenpflug J. Women recover faster than men after standard knee arthroplasty. Clin Orthop Relat Res. 2011;469:2855–2865. doi: 10.1007/s11999-011-1921-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh JA, Kwoh CK, Richardson D, Chen W, Ibrahim SA. Sex and surgical outcomes and mortality after primary total knee arthroplasty: A risk-adjusted analysis. Arthritis Care Res (Hoboken) 2013;65:1095–1102. doi: 10.1002/acr.21953. [DOI] [PMC free article] [PubMed] [Google Scholar]





