Abstract
Purpose/Objectives
To examine how family members of patients with a primary malignant brain tumor transition into the caregiver role and how their perceptions of this transition change over time.
Research Approach
Descriptive, qualitative.
Setting
Neurosurgery and neuro-oncology clinics of a regional medical center.
Participants
10 family caregivers of patients with a primary malignant brain tumor.
Methodologic Approach
A series of 11 open-ended questions addressing various aspects of the care situation were administered to each caregiver. The same questions were asked at baseline (within one month of the patient’s diagnosis) and four months later. Content analysis was performed to identify themes among interviews.
Main Research Variables
Patient changes, caregiver adjustments, and accessing support.
Findings
Caregivers described difficulties stemming from the patient’s tumor-related dysfunction and changes in their familial, occupational, and social roles. Support from family and friends was vital to caregivers’ emotional health, but shock and fear were evident in all interviews. Becoming subsumed in the care situation was described as enmeshment. Caregivers reported difficulty in communicating with healthcare providers. When looking at change over time, three major themes emerged: Patient Changes: The New Normal; Caregiver Adjustments; and Accessing Support.
Conclusions
Caregivers require support in handling neurologic and physical sequelae, transitioning into new roles, and avoiding becoming enmeshed in the care situation.
Interpretation
This study underlines the importance of continuing research in this area to provide the necessary interventions that will assist caregivers and provide support throughout their loved one’s disease trajectory.
Primary malignant brain tumors (PMBTs) have a unique treatment and disease trajectory as compared to other cancers. Having a brain tumor not only subjects the patients to issues inherent in a cancer diagnosis (e.g., side effects from chemotherapy and radiation) but often causes significant neurologic deficits that interfere with daily life and function. Neurologic deficits can include physical deficits as well as cognitive decline in memory, attention, language and communication, executive function, reasoning, judgment, and mental flexibility (Sherwood et al., 2006).
The presence of these complications leads to many difficulties for family caregivers of those with PMBT. For example, patients often are forced to quit their jobs upon diagnosis, which requires the family caregivers to maintain employment to ensure medical benefits. Neurologic dysfunction, such as memory loss or inappropriate behavior, may limit the number of social activities the dyad may engage in and typically increases household responsibilities, such as managing finances, for the caregiver. To provide the best possible care to the patient, caregivers’ needs and concerns must be acknowledged to minimize the stress and burden they experience. Research has shown that providing care for patients with dementia produces negative psychological and behavioral (psychobehavioral) responses, such as depressive symptoms, caregiver burden, and altered sleep patterns (Brummett et al., 2006). However, the majority of the studies have been cross-sectional and do not address how and when caregiver distress emerges in the care situation. In addition, almost no attention has been paid to caregivers of patients with PMBT. The purpose of the current study was to examine the transition from family member to caregiver and to explore changes in caregivers’ perceptions of that transition during the first four months following diagnosis. These data are vital for implementing the most efficient and effective interventions to improve caregiver health by providing the necessary support during the transition of becoming a family caregiver.
Background
Although PMBTs are relatively rare, the mortality rate is high, accounting for more than 12,000 deaths per year in the United States (Chandana, Movva, Arora, & Singh, 2008). Glioblastoma multiforme tumors are the most frequently diagnosed PMBTs, with a survival rate often less than one year (Ishihara et al., 2008). PMBTs may cause severe physical, neuropsychological, and neurologic dysfunction, reducing the patient’s ability to perform usual activities and meet occupational, financial, familial, and social roles (Sherwood et al., 2006). Decline in memory, information processing, and attention are a few of the cognitive changes that may occur when undergoing treatment for PMBTs. Even after aggressive treatment, cognitive dysfunction is likely to persist (Chandana et al., 2008) as a result of permanent neuronal damage from surgery, cerebral edema during treatment, radiation necrosis, or other factors. Such deterioration in cognitive functioning affects the patient’s ability to fulfill his or her previously held roles (Fox, Mitchell, & Booth-Jones, 2006). Caregivers often assume additional roles to ensure financial, familial, and household stability.
Carter (2006) has described the care situation as a “biopsychosocial process,” meaning that caregiver perceptions of the care situation, as well as the ability to fulfill the caregiver role, will directly affect psychological health. The distress that accompanies demands placed on caregivers of those with cancer has been well documented (Schumacher et al., 2008). Family members often assume multiple responsibilities, such as providing physical care and emotional support, managing symptoms, and coordinating healthcare appointments (Stajduhar, Martin, Barwich, & Fyles, 2008). Unfortunately, many family members feel inadequately prepared to cope with care demands (Schumacher, Beidler, Beeber, & Gambino, 2006). Schumacher et al. (2006) described the dual meaning of care demands. A care demand may not necessarily act as a stressor; instead, demands are relabeled as care needs that may or may not act as stressors for the caregiver. Whether something is viewed as a stressor depends on the degree to which caregivers are prepared for given situations as well as their ability to cope. Stajduhar et al. (2008) examined caregivers’ ability to cope during end-of-life care of a loved one with cancer. Caregivers reported that they were better able to cope when patients were aware and accepting of their illness and when they demonstrated appreciation for their work. Other factors that influenced caregivers’ ability to cope were having a supportive social network, having early access to information, and knowing that the home healthcare system would support them in difficult times.
Literature has shown that physical health can be affected by an individual’s accessibility and quality of social support networks. The risk of mortality may be lower for those with a wider network of high-quality social support. However, the type of support needed within networks may depend on the situation (Reblin & Uchino, 2008). In Australia, Janda, Eakin, Bailey, Walker, and Troy (2006) used qualitative analysis to examine responses from patients diagnosed with a brain tumor and caregivers who were using a support service and inquired about what services would have been helpful and whether they had difficulty obtaining information about caring for a loved one with a brain tumor. Caregivers reported that they wanted help in the following areas but were unable to obtain assistance: acquiring information about the diagnosis and treatment process, methods of coping, support from family and friends, and support with financial issues and preparing for long-term care. In neuro-oncology, caregiver support varies in the disease trajectory. Janda et al. (2006) found that patients who survived one year following diagnosis became better able to complete tasks and resume some of their personal care needs. Although the findings are similar to the needs that are addressed by other cancer populations, some are unique to the brain tumor population, such as managing difficult behaviors and emotional lability.
Previous studies in neuro-oncology family caregiving (and in most family caregiving in other populations) have been quantitative. The nature of quantitative research precludes a deeper understanding of caregiver stress—data that are vital for planning and implementing interventions. Research has shown that the use of qualitative analysis gives more detailed insight to the lived experience and may demonstrate the limitations of global clinical outcome measures (Happ, DeVito-Dabbs, Tate, Hricik, & Erlen, 2006). The use of qualitative data supports the quantitative findings by providing a more detailed explanation of the caregivers’ experiences. That information would be influential when developing future interventions for caregivers to target specific needs throughout the patient’s disease trajectory. Although the previous studies have provided much-needed information regarding perspectives of caregivers’ stress and needs, information is limited about how distress emerges during the care trajectory. Without understanding the timing and initiators of caregiver distress, interventions to reduce distress are likely to be ineffective. The purpose of this analysis was to examine how caregiver responses to open-ended questions changed from the time of diagnosis to four months after diagnosis. The theoretical framework for this study was the Pittsburgh Mind-Body Center’s common pathways model adapted by Sherwood et al. (2008). In this model, the patient’s disease characteristics and caregivers’ personal characteristics determine the degree to which caregivers will perceive negative psychological outcomes during the care situation. These negative psychological outcomes may, in turn, affect the physiologic stress response and ultimately lead to poor overall health. Content analysis was used to identify themes and subjects of common interest across caregivers (Patton, 2002).
Methods
Design
A prospective longitudinal descriptive design was used for this study to provide rich information on the needs of caregivers and how those needs may change over time. Family caregivers and patients were recruited within a month of diagnosis, and data were collected at baseline and four months following diagnosis to allow evaluation of changes in caregivers’ perceptions.
Sample
Content analysis was performed on an inception cohort of 10 family caregivers of patients with PMBT who were recruited as part of an ongoing descriptive study. Caregivers were approached for recruitment within one month of the patient’s diagnosis from the neurosurgery and neuro-oncology clinics of a regional medical center. The study was described to the patient by a research staff member, at which time they were asked to identify a person who they would consider their primary caregiver. Once the caregiver was identified, the patient and caregiver provided informed consent. If the caregiver was not present during the clinic visit with the patient, the recruiter provided the patient with a toll-free number for the caregiver to contact study personnel and follow-up was performed with patients. If the caregiver was interested in participating, the consent form was mailed to the caregiver or signed during a baseline data collection time point. To be eligible for participation, caregivers had to be at least 21 years of age, caring for someone with PMBT (verified by a pathology report), and able to read and speak English. Because one of the main goals of the study was to understand the onset and trajectory of emotional distress on becoming a caregiver, individuals were excluded if they were currently providing care for anyone other than children.
Data Collection
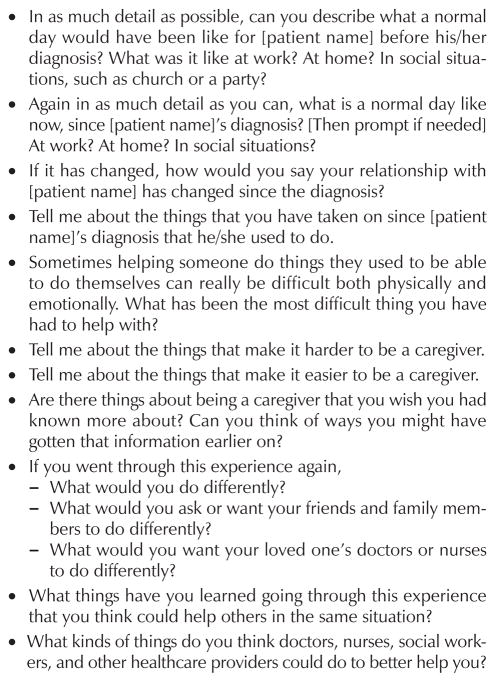
Caregivers were interviewed by a research staff member over the telephone within one month of their loved one’s diagnosis and again four months later. Interviews consisted of 11 open-ended questions (see Figure 1). The questions were developed based on the investigators’ previous experience with this population to address specific areas of concern that may affect caregiver and patient quality of life following PMBT diagnosis. Caregivers were asked permission to have their responses recorded for verbatim transcription and also were encouraged to speak freely about their feelings and experiences. The interview length varied depending on the amount of information the caregiver chose to disclose when responding to each question. The same questions were asked at baseline and at the four-month point to examine the differences in caregiver responses over time. Demographic information was collected from caregivers and patients over the phone or face-to-face in the neurosurgery clinic at each time point.
Figure 1.
Open-Ended Interview Questions
Analysis
Recorded interviews were transcribed verbatim, and interviews were deleted immediately from the recorder to ensure confidentiality. Caregivers were assigned an identification number, and any identifying information from the recorded interviews was not transcribed. Generic labels were given to represent specific names of people or places. The first step in the analysis was to identify themes of caregiver responses at baseline only. Content analysis, or analyzing text to determine what patterns of text or concepts predominate, was performed to identify recurring themes among interviews (Patton, 2002). To enhance confirmability, three research study personnel read and coded themes independently. The reviewers then met as a group and agreed on the main themes of the analysis. Any disagreements regarding theme identification or definition were discussed until consensus was reached among all three reviewers. Interviews were read until saturation was reached and no new themes were identified. Interview questions requested specific content from caregivers. For example, caregivers were asked to tell the interviewer about the things that make it harder to be a caregiver, followed by a question asking about the things that make it easier. By not asking a general question similar to “Tell me about being a caregiver,” the authors purposefully guided the interviews at both baseline and four months. The authors recognized this as a limitation, but chose to proceed to best address the research question—how do caregiver responses change over time? The second step of the analysis was to read each caregiver’s baseline and four-month interviews together to identify new themes and identify any changes in thematic definitions over time. Content analysis of the interviews at baseline plus four months was performed in a similar fashion to that at baseline alone.
Results
Sample
The majority of participants were female (80%, N = 8), Caucasian (100%, N = 10), and were the spouse of the patient (50%, N = 5) (see Table 1). Institutional review board approval was received prior to participant recruitment.
Table 1.
Sociodemographic Characteristics of the Caregivers and Patients
| Characteristic | X̄ | Range |
|---|---|---|
| Caregiver age (years) | 48 | 21–63 |
| Patient age (years) | 50.3 | 26–75 |
| Characteristic | n | % |
|---|---|---|
| Caregiver’s relationship to the patient | ||
| Spouse | 5 | 50 |
| Parent | 2 | 20 |
| Other (child, nephew, or friend) | 3 | 30 |
| Caregiver ethnicity | ||
| Caucasian | 10 | 100 |
| Patient tumor type | ||
| Glioblastoma multiforme | 6 | 60 |
| Astrocytoma grades I–III | 4 | 40 |
N =10
Content analysis of caregiver responses at baseline revealed six major areas of concern for caregivers: tumor-related dysfunction, role changes, social support, shock and fear, enmeshment, and communication. Themes at baseline represent the initial transition into the caregiver role within a month after the patient’s diagnosis. Caregivers described concerns stemming from tumor-related dysfunction in the patient, such as personality changes and difficulty performing daily functions. Caregivers also described changes in their familial, occupational, and social roles and responsibilities. Support from family and friends was vital to caregivers’ emotional health, but shock and fear were evident in all interviews. Becoming consumed in the care situation was labeled as enmeshment. Finally, caregivers reported difficulty in communicating, particularly with healthcare providers.
The next step in the analysis was to read each caregiver’s baseline and four-month transcripts together to compare how areas of concern changed from baseline to four months. Analysis of changes in areas of concern between baseline and four months resulted in three major themes representing the caregivers’ perceptions of changes during the first four months of the patient’s illness trajectory.
Patient Changes: The New Normal
This theme represented the need for caregivers to reestablish family routines to accommodate the patient’s functional and behavioral changes. Participants described a long period of time required for the new normal to be considered routine. In some cases, family routines were reestablished rather quickly, depending on the severity of the patient’s functional status.
I care for the kids 24/7. I’ve taken on a lot of the chores around the house that include lifting, taking out the garbage, cleaning the house, and I’ve taken care of the bills and dealing with the insurance company, and making sure he gets the medication filled.
Key terms and phrases in this quote signify the new normal for this particular caregiver. Phrases such as “I have taken on” and “full responsibility” represent the transition from team parenting to more of a single- parent role. Another aspect of this theme is the uncertainty that caregivers regularly feel in terms of the ambiguity of the patient’s disease trajectory.
[The patient] said, “I turned suddenly and have a headache.” I got cold. I thought this is how the whole thing started. I thought, “He’s recurred.” I kept watching him and checking him: “How’s your head now?” I think this will probably continue forever. I think I’ll probably always be afraid of recurrence.
The caregiver goes on to talk about this fear of recurrence being something that she deals with on her own, without expressing the worry to her son.
I’m a nurse and there’s a lot of things that I understand more than someone else would. But it’s still your kid and it’s still scary…. I think that I’ll always have the concerns that I have about recurrence. I feel that’s my private concern and I have to show my “I’m OK” face to most people.
Another caregiver explains how the patient’s new daily life consists of tumor or treatment-related dysfunction.
What makes it difficult for her is having the memory problems; she doesn’t know that she can’t walk, so she gets upset that there is a seat belt on her wheelchair. Not knowing the different things that are going on with her, what’s causing them, and how to treat them.
The quotes reveal how caregivers’ lives are altered, possibly causing physical or emotional distress that would benefit from professional support.
Caregiver Adjustments
The authors labeled the feelings that caregivers experienced shortly after the diagnosis—during which they felt emotionally closer to the patient—as the honeymoon phase. During this phase, relationships within the family improved and those involved shifted priorities to value personal time.
I’d say definitely closer than before. We definitely cherish each other more and tell each other that we love each other.
Caregivers reported ongoing adjustments to the demands of the care situation four months after diagnosis. However, responses at the follow-up point suggested that the honeymoon phase had come to an end. This phenomenon was labeled as disappearance of the honeymoon phase.
I worry about him more and he doesn’t like that. When we go out to eat he has trouble if he has to calculate the tip. He has trouble writing it—he has a tremor—and so I have to write it. I’m the one who keeps track of the medications, goes to the bank, goes to the post office; I’m the one that does the things that he used to be able to do.
In this quote, the caregiver had a difficult time focusing on how her relationship with the patient had changed. She was unable to reflect on the relationship, only able to focus on the way in which the patient’s dysfunction required her to do things that he was once able to do independently. At four months, caregivers took on more responsibilities in the patient’s treatment regimen (including driving patients to appointments and providing symptom management assistance) while continuing to accumulate additional responsibilities.
Accessing Support
A noticeable transition occurred between baseline and four months in how the caregiver perceived support from friends, family, doctors, nurses, and other healthcare professionals. Caregivers stated that they wished family and friends had been more focused in their support of the needs and emotions of the patient rather than on their own grief.
What I didn’t expect is my mother-in-law and my sister-in-law being such wrecks.
I would like them to show a little more interest in him. He has always shown interest in them. They should stop being so self-centered. Give him some peace at the end of his life.
Caregivers also displayed a desire for family and friends to take more initiative.
It would be nice if they’d call up and just offer to come sit with him for a day or even a couple of hours so I could take a break. Or even someone putting a meal together and dropping it off at your house.
I would like people to take initiative and say, “Hey, Saturday I’m going to come and mow your yard.”
At the follow-up, caregivers described more interest in looking for support from others who have been in similar situations and not necessarily a close friend or relative. As the patient’s disease progressed, caregivers found more support from others who could relate to their situation and provide information, such as ways of coping.
Just talking to other people who are going through the same things that I am. Just being able to talk to them and knowing that I’m not going crazy, and that they’re going through it too, and how they cope. It has really helped a lot, just having people that know what you’re going through.
Discussion
The results of the analysis suggest that caregivers experience significant changes in their perception of the care situation during the first four months of the disease trajectory, data that have been missing from cross-sectional analyses. Distress arises from physical, cognitive, and psychological changes in the patient. Patients with PMBT are not only susceptible to side effects of chemotherapy, but they are also likely to face neurologic difficulties as a result of the tumor’s size and location. That results in a reframing of perspective into the new normal. Patients and caregivers are faced with new situations where symptoms and side effects of treatment may prevent normal activity and resumption of typically held roles within the home, work, and social situations. As with any change to routine functions, patients and caregivers are forced to acknowledge these changes, accept them as the new normal, and make the necessary adjustments. The relationship dynamics between the caregiver and patient may change as well. The dyad goes through the honeymoon phase soon after the diagnosis, when the caregiver and patient report feeling closer than before. However, four months after the diagnosis, the dyad may be so subsumed within the cancer trajectory that the honeymoon phase comes to an end. With survival rates for glioblastoma being about 6–12 months (Tait, Petrik, Loosemore, Bell, & Papadopoulos, 2007) and with a high rate of recurrence (Ziegler et al., 2008), the dyad has a lot to take care of in a relatively short amount of time. Tying up loose ends, such as financial planning, funeral arrangements, policy and deed transfers, and end-of-life decision making, may result in the disappearance of the honeymoon phase.
Although caregivers may report a desire for more support in dealing with the stress resulting from caregiving demands, it can be difficult for them to set aside time to access support systems, such as support groups. Schmer, Ward-Smith, Latham, & Salacz (2008) reported that some caregivers were unlikely to have time to attend support groups when care demands were high—a time when social support is vital. As patients’ diseases progressed, caregivers reported the desire to spend any available time with their loved one. Caregivers also reported that their needs for social support changed over time. At diagnosis, “just being there” appeared to fulfill caregivers’ needs for social support. As the patient’s disease progressed, caregiver needs became more specific, yet caregivers reported being unable or uncomfortable in voicing specific needs.
Limitations
Although the patients enrolled in this study were representative of the brain tumor population, one limitation of this study is the homogeneity of the caregiver sample. The majority of the sample consisted of wives of the patients, and all of the caregivers were Caucasian. It would be beneficial to look at male caregivers as well as caregivers with other relationships to the patient (e.g., adult children of the patient) to determine transferability of data. In addition, results were not shared with participants to address issues of credibility. Lastly, interviews were conducted via telephone, rather than in person. Data collectors established a relationship with participants prior to the interview; however, the use of a telephone interview, rather than using face-to-face data collection, may have limited the quality of data obtained.
Implications for Nursing
Clinical Practice
As a result of the change in expectations during the first four months (e.g., identifying the new normal), the nurse may need to have frequent contact with the dyad to help them first acknowledge the changes in their lives and relationships. Regarding relationships, practitioners may warn caregivers and patients that, although there may be a time at the beginning of the care situation when the dyad (and family) feels closer together, these feelings may change as the disease trajectory continues. Realizing ways to maintain that feeling of being closer and appreciating each other more during difficult times may offset some of the negative aspects of providing care that seem to appear within the first four months.
Data also suggest that caregivers desired social support in different ways at four months after diagnosis. Practitioners may focus caregiver instruction sessions on teaching caregivers how to identify potential sources of support, how to identify particular care needs that could be met by others, and how to communicate those needs to friends and family. Unfortunately, caregivers reported not having an adequate amount of free time to attend support groups. One way of addressing this concern would be offering support services during patient treatment regimens. Because the caregiver often transports and accompanies the patient to his or her treatment sessions, it would be beneficial to offer support services while the caregiver is waiting for the patient to finish treatment. Because of the tendency for caregivers to limit the amount of time they spend on themselves during the day to provide care, support during the patient’s clinic appointment may be a successful approach. Educators, counselors, social workers, and other supportive staff could be available to assist caregivers in addressing any needs or concerns throughout the disease trajectory.
To provide high-quality care, the accessibility of necessary support systems is essential for family caregivers. Support could be offered separately from the patient’s doctor visits as well. Practitioners could be available during certain times of the day or week to accept phone calls from caregivers who may not feel comfortable discussing their concerns during the patient’s doctor visit. Practitioners also can provide pamphlets to family caregivers to answer frequently asked questions as well as to obtain various resources within their community.
Research
Data from this analysis underscore the dynamic nature of the care situation. Longitudinal studies are vital in beginning to understand how and when caregiver needs change over time. Future qualitative research would provide additional personal accounts of the specific areas to target when intervening with family caregivers. Such areas may include financial planning, techniques to cope with the patient’s illness and problematic symptoms, support groups, educational materials, and counseling. Continued research in this area of family caregiver health is vital to ensure high-quality care is provided to the patient with PMBT while safeguarding caregivers’ health and emotional well-being.
Conclusion
Despite the study limitations, the results provide a glimpse of the transition family members go through when assuming the role of family caregiver as well as more detailed information regarding how distress appears and the changes that occur as family members assume the caregiver role. This study underscores the importance of continuing research in this area to provide the necessary interventions that will assist caregivers and provide support throughout their loved one’s disease trajectory.
Footnotes
This material is protected by U.S. copyright law. Unauthorized reproduction is prohibited. To purchase quantity reprints, please e-mail reprints@ons.org or to request permission to reproduce multiple copies, please e-mail pubpermissions@ons.org.
No financial relationships to disclose.
Sherwood can be reached at prs11@pitt.edu, with copy to editor at ONFEditor@ons.org.
References
- Brummett BH, Babyak MA, Siegler IC, Vitaliano PP, Ballard EL, Gwyther LP, Williams RB. Associations among perceptions of social support, negative affect, and quality of sleep in caregivers and noncaregivers. Health Psychology. 2006;25:220–225. doi: 10.1037/0278-6133.25.2.220. [DOI] [PubMed] [Google Scholar]
- Carter PA. A brief behavioral sleep intervention for family caregivers of persons with cancer. Cancer Nursing. 2006;29(2):95–103. doi: 10.1097/00002820-200603000-00003. [DOI] [PubMed] [Google Scholar]
- Chandana SR, Movva S, Arora M, Singh T. Primary brain tumors in adults. American Academy of Family Physicians. 2008;77:1423–1430. [PubMed] [Google Scholar]
- Creswell JW. Research design: Qualitative and quantitative approaches. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Fox SW, Mitchell SA, Booth-Jones M. Cognitive impairment in patients with brain tumors: Assessment and intervention in the clinic setting. Clinical Journal of Oncology Nursing. 2006;10:169–176. doi: 10.1188/06.CJON.169-176. [DOI] [PubMed] [Google Scholar]
- Happ MB, DeVito-Dabbs A, Tate J, Hricik A, Erlen J. Exemplars of mixed methods data combination and analysis. Nursing Research. 2006;55(2, Suppl):S43–S49. doi: 10.1097/00006199-200603001-00008. [DOI] [PubMed] [Google Scholar]
- Ishihara H, Kubota H, Lindberg RL, Leppert D, Gloor SM, Errede M, Frei K. Endothelial cell barrier impairment induced by glioblastomas and transforming grown factor β2 involves matrix metalloproteinases and tight junction proteins. Journal of Neuropathology and Experimental Neurology. 2008;67:435–448. doi: 10.1097/NEN.0b013e31816fd622. [DOI] [PubMed] [Google Scholar]
- Janda M, Eakin EG, Bailey L, Walker D, Troy K. Supportive care needs of people with brain tumours and their carers. Supportive Care in Cancer. 2006;14:1094–1103. doi: 10.1007/s00520-006-0074-1. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. 3. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Reblin M, Uchino BN. Social and emotional support and its implication for health. Current Opinion in Psychiatry. 2008;21:201–205. doi: 10.1097/YCO.0b013e3282f3ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmer C, Ward-Smith P, Latham S, Salacz M. When a family member has a malignant brain tumor: The caregiver perspective. Journal of Neuroscience Nursing. 2008;40(2):78–84. doi: 10.1097/01376517-200804000-00006. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Beidler SM, Beeber AS, Gambino P. A transactional model of cancer family caregiving skill. Advances in Nursing Science. 2006;29:271–286. doi: 10.1097/00012272-200607000-00009. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Stewart BJ, Archbold PG, Caparro M, Mutale F, Agrawal S. Effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncology Nursing Forum. 2008;35:49–56. doi: 10.1188/08.ONF.49-56. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Given BA, Donovan H, Baum A, Given CW, Bender CM, Schulz R. Guiding research in family care: A new approach to oncology caregiving. Psycho-Oncology. 2008;17:986–996. doi: 10.1002/pon.1314. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Given BA, Given CW, Schiffman RF, Murman DL, Lovely M, Remer S. Predictors of distress in caregivers of persons with a primary malignant brain tumor. Research in Nursing and Health. 2006;29:105–120. doi: 10.1002/nur.20116. [DOI] [PubMed] [Google Scholar]
- Stajduhar K, Martin WL, Barwich D, Fyles G. Factors influencing family caregivers’ ability to cope with providing end-of-life cancer care at home. Cancer Nursing. 2008;31:77–85. doi: 10.1097/01.NCC.0000305686.36637.b5. [DOI] [PubMed] [Google Scholar]
- Tait MJ, Petrik V, Loosemore A, Bell BA, Papadopoulos MC. Survival of patients with glioblastoma multiforme has not improved between 1993 and 2004: Analysis of 625 cases. British Journal of Neurosurgery. 2007;21:496–500. doi: 10.1080/02688690701449251. [DOI] [PubMed] [Google Scholar]
- Ziegler DS, Wright RD, Kesari S, Lemieux ME, Tran MA, Jain M, Kung AL. Resistance of human glioblastoma multiforme cells to growth factor inhibitors is overcome by blockade of inhibitor apoptosis proteins. Journal of Clinical Investigation. 2008;118:3109–3122. doi: 10.1172/JCI34120. [DOI] [PMC free article] [PubMed] [Google Scholar]