Abstract
Given that the there is little information about the current status of brucellosis and Q fever in most parts of Iran, the aim of this study was to assay the seroprevalence of these two diseases in high-risk populations of Kurdistan Province in western Iran. Two hundred fifty sera samples were collected from hunters and their families, butchers, health care workers, and those referred to medical diagnostic laboratories in the southwestern regions of Kurdistan Province. Sera were tested to detect specific immunoglobulin G (IgG) antibodies against brucellosis and Coxiella burnetii (phase I and II). The seroprevalence of brucellosis and Q fever (C. burnetii IgG phase I and II) was 6.4% and 27.83% (20% and 14.52%), respectively. The highest seroprevalence of Q fever (38%) and brucellosis (12%) was seen in butchers, who handled cattle, sheep, and goats during their work. Age had a significant positive association with Q fever seropositivity (p=0.04). The seroprevalence of Q fever was higher in those people who had been in employment for more than 10 years (21.88%) compared to others (7.79%) (p=0.02). The keeping of animals (p=0.03), hunting and eating the meat of wild animals (p=0.02), and not disinfecting hands and faces after working (for health care workers and butchers) (p=0.02) were risk factors for Q fever seropositivity. This study showed a relatively high seroprevalence of brucellosis and Q fever in high-risk populations of Kurdistan Province. It is suggested that complementary studies be carried out in other parts of western Iran to clarify the epidemiological aspects of these diseases.
Key Words: : Coxiella burnetii, Brucellosis, Seroprevalence–Kurdistan, Risk factor
Introduction
From among approximately 1400 known human pathogenic agents, nearly 85% of them are zoonotic (Jones et al. 2008). Monitoring, control, and prevention of zoonotic diseases are considered an important challenge for health systems worldwide.
Brucellosis is one of the most important bacterial zoonotic diseases that is a public health problem in most parts of the world (Seleem et al. 2010). Brucellosis causes a severely debilitating and disabling illness, with fever, sweating, fatigue, weight loss, headache, and joint pain persisting for weeks to months (Dean et al. 2012). Neurological complications, endocarditis, and testicular or bone abscess formation can also occur (Buzgan et al. 2010). This disease is usually transmitted to humans through consumption of unpasteurized dairy products or through direct contact with infected animals, placentas, or aborted fetuses and is considered to be an occupational disease (Dean et al. 2012). Farmers, butchers, slaughterhouse workers, shepherds, veterinarians, and dairy factories workers are at high risk of the disease (Agasthya et al. 2007).
Q fever is also a zoonotic disease, which is caused by Coxiella burnetii. Livestock and pets are the main reservoirs of this disease. In animals, Q fever usually causes disease with no clinical signs or subclinical symptoms (Woldehiwet 2004). Transmission of infection to humans occurs mainly through inhalation of contaminated aerosols, and the disease occurs without symptoms or as mild to lethal forms (Marrie 2009, Angelakis and Raoult 2010). In humans, Q fever may appear as an acute (usually a self-limited febrile disease, pneumonia, or hepatitis) or chronic form (usually endocarditis) (Angelakis and Raoult 2010). Livestock handlers, farmers, veterinarians, slaughterhouse workers, people in contact with raw milk and its products, and laboratory personnel are most at risk of infection (Madariaga et al. 2003).
Epidemiological studies on zoonotic diseases can present important information on the status of the diseases and their risk factors to enable researchers and health system employees to implement appropriate preventive programs for this disease. In this regard, several epidemiological studies have been carried out on brucellosis among high-risk groups such as butchers, slaughterhouse workers, farmers, and veterinarians in some parts of the Iran, and the seroprevalence of brucellosis and its risk factors has been demonstrated (Salari 2002, Karimi et al. 2003, Parizadeh et al. 2009, Beheshti et al. 2010, Nikokar et al. 2011). However, on the basis of our best knowledge, there is no published seroepidemiological study on Q fever in high-risk populations in Iran. Given that the there was insufficient information on the current status of brucellosis and Q fever in most western regions of Iran, the aim of this study was to assay the seroprevalence of these two diseases in high-risk populations of Kurdistan Province in western Iran.
Materials and Methods
Study area and sampling
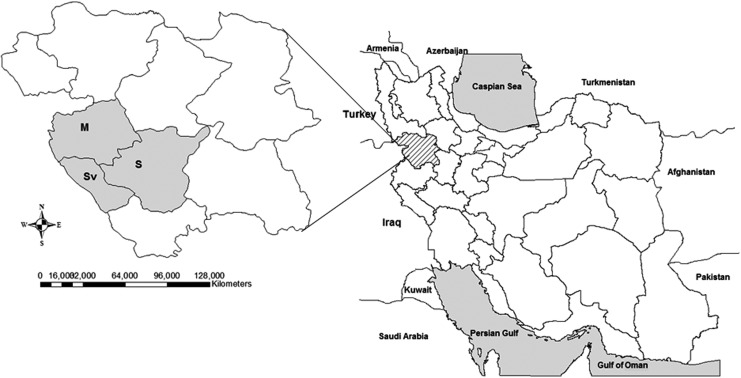
This study was carried out during 2011–2012 among high-risk populations in Kurdistan Province in western Iran. The sampling of this survey was from western regions of this province, with a focus on Sanandaj, Marivan, and Sarvabad counties (Fig. 1). Hunters and their families, butchers, and health care workers, as high-risk groups of people, as well as those referred to medical diagnostic laboratories for routine testing, as a control group, were recruited in the study. All individuals enrolled in this survey were over 18 years old. After obtaining informed consent for participation in the study, information on each participant's demographic characteristics, exposure to risks (keeping animals, hunting or eating the meat of wild animals), and use of personal protective equipment and disinfectants (for relevant occupations) was collected by means of a researcher-designed questionnaire. After completion of the questionnaire, an 8-mL blood sample was collected from each participant and immediately transferred to the laboratory for separation of sera. Sera were kept below −20°C and transferred to the Department of Epidemiology of the Pasteur Institute of Iran (Tehran, Iran).
FIG. 1.
Location of Kurdistan Province on a map of Iran (right). Sampling conducted from Marivan (M), Sarvabad (Sv), and Sanandaj (S) counties in 2012 (left).
Ethical considerations
The proposal of this study was accepted by the ethics committee of the Pasteur Institute of Iran.
Detection of brucellosis antibody (IgG)
A commercial enzyme-linked immunosorbent assay (ELISA) kit (IBL, Hamburg, Germany) was used for brucellosis antibody (immunoglobulin G [IgG]) detection. Positive and borderline sera in the ELISA method were confirmed by the standard tube agglutination test (STAT) (Pasteur Institute of Iran) as a gold standard test for brucellosis diagnosis, and serum titers greater than 1:80 were considered positive.
Detection of C. burnetii antibodies (IgG I and II)
IgG antibodies against C. burnetii were detected using a commercial ELISA kit (Virion/Serion Co., Germany) according to the manufacturer's instructions. Phase I and II antibodies were identified in separate assays.
Statistical analysis
The data were analyzed by SPSS software (version 16). Chi-squared, Fisher exact, and logistic regression tests were used to compare the variables. A p value less than 0.05 was considered statistically significant.
Results
In this study, 100 samples from referrals to medical diagnostic laboratories and 150 samples from high-risk individuals (including 50 samples from hunters and their families, 50 samples from health care workers, and 50 samples from butchers) were collected from the counties of Sarvabad (no.=204, 81.60%), Marivan (no.=23, 9.20%, and Sanandaj (no.=23, 9.20%). In all, 206 (82.40%) of the participants were male. The median age of participants and length of employment for health care workers and butchers was 39.5 and 10 years, respectively. High-risk occupational groups found themselves at higher risk of zoonotic diseases (42%) compared to the control group (3%) (p<0.001). Ninety percent of high-risk group participants stated that secretions (blood and body fluids) of patients or animals had been splashed on their faces and bodies during work; 74.74% of them did not disinfect their knives, and 78.79% of them had never applied chemical disinfectant to their hands and faces.
The seroprevalence of Q fever antibodies of phases I and II (IgG) was 20% and 14.52%, respectively; 3.91% and 8.30% of participants had a borderline titer for IgG phase I and II, respectively. The overall seroprevalence of Q fever (having antibodies of phase I and or phase II) was 27.83%.
From all 250 sera, 12 (4.8%) and 5 (2%) of samples were positive and borderline respectively for Brucella IgG antibodies by ELISA. The seroprevalence of brucellosis antibodies among participants was 6.4% (16 sera) by STAT.
Among the counties, the highest seroprevalence of Q fever and brucellosis was observed in Sanandaj (52.17%) and Marivan (13%), respectively. The highest and the lowest Q fever seroprevalences were observed in butchers (38%) and health care workers (6%), respectively. Butchers (12%) and hunters (2%) had the highest and lowest seroprevalences, respectively, for brucellosis (Table 1). Q fever seropositivity in health care workers (6%) was significantly lower in comparison with the control group (30%) (p=0.003). Q fever seroprevalence was much higher in older people (older than the median age of the participants=39.5 years old) (p=0.04). In addition, the length of employment for hunters, butchers, and health care workers was a risk factor for Q fever seropositivity, so that the seroprevalence of Q fever was higher in people having been employed for more than 10 years (21.88%) compared with others (7.79%) (p=0.02).
Table 1.
The Relationship Between Demographic Characteristics of Participants and the Seroprevalence of Q Fever and Brucellosis
| |
|
Q fever |
Brucellosis |
||||
|---|---|---|---|---|---|---|---|
| Variable | No. tested (%inf) | OR (95% CI) | p value | No. tested (%inf) | OR (95% CI) | p value | |
| Occupation |
Control |
80 (30.00) |
Reference |
— |
100 (5.00) |
Reference |
— |
| |
Hunters |
50 (36.00) |
1.31 (0.62,2.78) |
0.48 |
50 (2.00) |
0.39 (0.44,3.41) |
0.39 |
| |
Health care worker |
50 (6.00) |
0.15 (0.04,0.53) |
0.003 |
50 (8.00) |
1.65 (0.42,6.44) |
0.47 |
| |
Butchers |
50 (38.00) |
1.43 (0.68,3.01) |
0.35 |
50 (12.00) |
2.59 (0.75,8.95) |
0.13 |
| County |
Marivan |
23 (17.39) |
Reference |
— |
23 (13.04) |
Reference |
— |
| |
Sanandaj |
23 (52.17) |
5.18 (1.34, 20.09) |
0.02 |
23 (7.70) |
0.64 (0.10, 4.21) |
0.63 |
| |
Sarvabad |
184 (26.09) |
1.57 (0.58. 4.87) |
0.43 |
204 (5.39) |
0.38 (0.10, 1.78) |
0.16 |
| Age |
Age ≤39.5 |
122 (22.13) |
1.83 (1.02,3.29) |
0.04 |
130 (4.61) |
1.88 (0.66, 5.34) |
0.30 |
| |
Age >39.5 |
108 (34.26) |
|
|
120 (8.33) |
|
|
| Length of employment |
≤10 |
77 (7.79) |
3.31 (1.92,9.21) |
0.02 |
77 (6.49) |
1.49 (0.43,5.13) |
0.52 |
| |
>10 |
64 (21.88) |
|
|
64 (9.37) |
|
|
| Location |
Urban |
45 (20.00) |
1.69 (0.76,3.75) |
0.19 |
51 (11.76) |
0.39 (0.14,1.15) |
0.10 |
| |
Rural |
185 (29.73) |
|
|
199 (5.02) |
|
|
| Gender |
Female |
37 (18.92) |
1.80 (0.75,4.33) |
0.19 |
44 (2.27) |
3.38 (0.43,26.2) |
0.32 |
| Male | 193 (29.53) | 206 (7.28) | |||||
OR, odds ratio; CI, confidence interval.
Keeping animals (p=0.03), hunting and eating the meat of wild animals (p=0.02), and failing to disinfect hands and faces after working (for health care workers and butchers) (p=0.02) were risk factors for Q fever seropositivity. There was no significant relationship between demographic characteristics and possible risk factors of participants and brucellosis seropositivity (Table 2).
Table 2.
The Relationship Between the Potential Risk Factors and Seropositivity of Q Fever and Brucellosis in Western Iran
| |
|
|
Q fever |
Brucellosis |
||
|---|---|---|---|---|---|---|
| Variable | Category | No tested (% inf) | p value | No. tested (% inf) | p value | |
| Splashing animal fluids on face/body |
Yes |
135 (26.67) |
0.99 |
135 (8.15) |
0.60 |
|
| |
|
No |
15 (26.67) |
|
15 (0.00) |
|
| Attitudea |
Yes |
162 (33.33) |
0.01 |
184 (5.98) |
0.77 |
|
| |
|
No |
65 (15.38) |
|
66 (7.58) |
|
| Hunting/Consumption wild animal meat |
Yes |
136 (33.82) |
0.02 |
149 (5.37) |
0.42 |
|
| |
|
No |
91 (19.78) |
|
101 (7.92) |
|
| Keeping animals |
Yes |
98 (35.71) |
0.03 |
105 (7.62) |
0.50 |
|
| |
|
No |
129 (22.48) |
|
145 (5.52) |
|
| Kind of kept animal |
Cattle |
Yes |
83 (35.8) |
0.76 |
90 (7.78) |
0.99 |
| |
|
No |
14 (28.57) |
|
14 (7.14) |
|
| |
Goats/sheep |
Yes |
56 (42.86) |
0.06 |
62 (6.45) |
0.71 |
| |
|
No |
39 (23.08) |
|
42 (9.52) |
|
| |
Dogs and cats |
Yes |
4 (50.00) |
0.61 |
4 (0.00) |
0.99 |
| |
|
No |
91 (34.06) |
|
100 (8.00) |
|
| Cutting hand/year |
>5 time |
93 (24.73) |
0.71 |
93 (7.53) |
0.99 |
|
| |
|
<5 time |
47 (27.66) |
|
47 (8.51) |
|
| Disinfection tools |
Yes |
25 (12.00) |
0.16 |
25 (8.00) |
0.99 |
|
| |
|
No |
74 (25.68) |
|
74 (10.81) |
|
| Disinfection hands/face |
Yes |
21 (4.76) |
0.03 |
21 (9.52) |
0.99 |
|
| No | 78 (26.92) | 78 (10.26) | ||||
See themselves at risk of zoonosis.
Discussion and Conclusion
This study showed a relatively high prevalence of brucellosis and Q fever in Kurdistan Province, with the seroprevalence of C. burnetii IgG phase I and II and brucellosis IgG at 20%, 14.5% and 6.4%, respectively.
The last human case of Q fever in Iran was reported several decades ago (Mostafavi et al. 2012b), but recent reports of the disease in livestock in different parts of Iran (Sakhaee and Khalili 2010, Mostafavi et al. 2012a) show a wide distribution of the disease all over the country (Mostafavi et al. 2012b). In the present study, which is the first study on Q fever in the human population of western Iran, the seroprevalence rate of Q fever IgG phases I and II was 20% and 14.5%, respectively. In the only study conducted in recent years (2010), the prevalence of IgG phases I and II of C. burnetii was reported at 24% and 36%, respectively, in febrile patients of Kerman Province (southeast Iran) (Khalili et al. 2010).
In the present study, age and length of employment were correlated parameters and had a positive significant association with the seroprevalence of Q fever, and these findings are consistent with other similar studies (McCaughey et al. 2008, Anderson et al. 2009). Studies conducted around the world have shown that livestock is the main reservoir for Q fever in humans (Angelakis and Raoult 2010). Therefore, exposure to livestock can be an important risk factor for this disease and in increasing the risk of Q fever seropositivity in people who keep livestock. A history of hunting and eating the meat of wild animals also had a statistically significant influence on Q fever seropositivity in our study, with Q fever seroprevalence in these persons being double that of others. As expected, in the present study, disinfecting hands and faces with disinfectants (for health care workers and butchers) was a protective factor against Q fever seropositivity. Given the above facts, the importance of disinfecting and using personal protection equipment during work in high-risk occupations is identified.
Brucellosis is an important endemic zoonotic disease in Iran and has been reported from different parts of the country (Mostafavi and Asmand 2012). Kurdistan Province is one of the provinces with reports of high levels of brucellosis (Moradi et al. 2006), with 10,260 cases of brucellosis being reported in this province between 1999 and 2008 (Mostafavi and Asmand 2012). In our study, the seroprevalence of brucellosis was 6.4%, which is lower than that obtained from similar studies in other areas of the country, with brucellosis seroprevalence reported at 8.5% in butchers, slaughterhouse workers, and veterinarians of Kazeroon (southern Iran) in 2010 (Beheshti et al. 2010); 30.3% in butchers, slaughterhouse workers, veterinarians, farmers, milk collectors, and shepherds of Khorasan Razavi Province (northeast Iran) in 2005–2006 (Parizadeh et al. 2009); 7.1% in slaughterhouse workers and rural inhabitants of Gilan Province (northern Iran) in 2009 (Nikokar et al. 2011); and 11.7% in butchers and slaughterhouse workers of Shiraz (southern Iran) in 1999–2000 (Karimi et al. 2003). On the other hand, brucellosis seroprevalence was reported to be 3.2% in Yazd Province (central Iran) in 2007–2009 (Salari 2002), which was lower than brucellosis seroprevalence in the present study.
One of the limitations of this study was the lack of a proper occupation to represent the general population. Although patients referred to medical diagnostic laboratories were selected as a control group and as representative of the general population in this study, because of easy access to their blood, it would appear that this group of people was not a good representative group because there was no significant difference in the seropositivity rate of brucellosis in this group in comparison to other high-risk groups. Q fever seroprevalence in this group (30%) was surprisingly significantly higher than that of health care workers (6%), and there was no significant statistical difference in the seropositivity of this group and other high-risk groups. One possible justification for this finding is that the people in the health care workers group may have different origins and have lived a shorter time in this region than the other groups in this region.
Even though an acceptable sample size was enrolled in this study, the number of samples in each group (hunters, health care workers, butchers, and referrals to medical diagnostic laboratories) was not good enough to provide a judgment of the situation of these diseases in these groups. Although the ELISA test is a test with high sensitivity and specificity for diagnosis of C. burnetii antibodies, this test is used for the seroepidemiological studies and primary screening of patients. Other methods, such as indirect immunofluorescence, are recommended to confirm the positive cases. It is suggested that in the future complementary studies should be carried out in other regions of Kurdistan Province and neighboring provinces to clarify the epidemiological aspects of these diseases in western Iran.
Acknowledgments
We appreciate the financial support of the Pasteur Institute of Iran and the Centre for Disease Control of the Iranian Ministry of Health and Medical education (grant no. 582). We would like to express our gratitude to Dr. Bidarpour, Mr. Karimi, Mr. Banafshi, Mr. Bahmani, and Mr. Faraji of Kurdistan University of Medical Sciences for their support in sampling and Dr. Behzad Esfandiari and Ms. Manijeh Yousefi Behzadi for their support in data entry of the questionnaire.
Author Disclosure Statement
The authors declare that they have no competing financial interests.
References
- Agasthya A, Isloor S, Prabhudas K. Brucellosis in high risk group individuals. Indian J Med Microbiol 2007; 25:28–31 [DOI] [PubMed] [Google Scholar]
- Anderson AD, Kruszon-Moran D, Loftis AD, McQuillan G, et al. . Seroprevalence of Q fever in the United States, 2003–2004. Am J Trop Med Hyg 2009; 81:691–694 [DOI] [PubMed] [Google Scholar]
- Angelakis E, Raoult D. Q fever. Vet Microbiol 2010; 140:297–309 [DOI] [PubMed] [Google Scholar]
- Beheshti S, Rezaian G, Azad F, Faghiri Z, et al. . Seroprevalence of brucellosis and risk factors related to high risk occupational groups in Kazeroon, south of Iran. Int J Occup Environ Med 2010; 1:62–68 [PubMed] [Google Scholar]
- Buzgan T, Karahocagil MK, Irmak H, Baran AI, et al. . Clinical manifestations and complications in 1028 cases of brucellosis: A retrospective evaluation and review of the literature. Int J Infect Dis 2010; 14:e469–e478 [DOI] [PubMed] [Google Scholar]
- Dean AS, Crump L, Greter H, Schelling E, et al. . Global burden of human brucellosis: A systematic review of disease frequency. PLoS Negl Trop Dis 2012; 6:e1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KE, Patel NG, Levy MA, Storeygard A, et al. . Global trends in emerging infectious diseases. Nature 2008; 451:990–993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karimi A, Alborzi A, Rasooli M, Kadivar M, et al. . Prevalence of antibody to Brucella species in butchers, slaughterers and others. East Mediterr Health J 2003; 9:178–184 [PubMed] [Google Scholar]
- Khalili M, Shahabi-Nejad N, Golchin M. Q fever serology in febrile patients in southeast Iran. Trans R Soc Trop Med Hyg 2010; 104:623–624 [DOI] [PubMed] [Google Scholar]
- Madariaga MG, Rezai K, Trenholme GM, Weinstein RA. Q fever: A biological weapon in your backyard. Lancet Infect Dis 2003; 3:709–721 [DOI] [PubMed] [Google Scholar]
- Marrie TJ. Q fever Bacterial Infections of Humans: Epidemiology and Control. Abrutyn E, Brachman PS. (eds). Springer: Philadelphia, PA: 2009:643–660 [Google Scholar]
- McCaughey C, McKenna J, McKenna C, Coyle P, et al. . Human seroprevalence to Coxiella burnetii (Q fever) in Northern Ireland. Zoonoses Public Health 2008; 55:189–194 [DOI] [PubMed] [Google Scholar]
- Moradi G, Kanani S, Sofimajidpur M, Ghaderi A. Epidemiologic survey of 3880 patients with brucellosis Kurdistan. Iran Infect Trop Dis J 2006; 11:28–32 [Google Scholar]
- Mostafavi E, Asmand M. Trends of brucellosis (malta fever) in Iran during the period 1991–2008. Iranian J Epidemiol 2012; 8:94–101 [Google Scholar]
- Mostafavi E, Esmaeili S, Shahdordizadeh M, Mahmoudi H, et al. . Seroepidemiological feature of Q fever among sheep in Northern Iran. Retrovirology 2012a; 9:P40. [PubMed] [Google Scholar]
- Mostafavi E, Rastad H, Khalili M. Q Fever: An emerging public health concern in Iran. Asian J Epidemiol 2012b; 5:66–74 [Google Scholar]
- Nikokar I, Hosseinpour M, Asmar M. Seroprevalence of brucellosis among high risk individuals in Guilan, Iran. J Res Med Sci 2011; 16:1366–1371 [PMC free article] [PubMed] [Google Scholar]
- Parizadeh SMJ, Seyednozadi M, Erfanian MR, Nezhad MA. A survey on antibody levels among individuals at risk of brucellosis in Khorasan Razavi Province, Iran. Pakistan J Nutr 2009; 8:139–144 [Google Scholar]
- Sakhaee E, Khalili M. The first serologic study of Q fever in sheep in Iran. Trop Animal Health Product 2010; 42:1561–1564 [DOI] [PubMed] [Google Scholar]
- Salari M. Seroepidemiological survey of brucellosis among animal farmers of Yazd province. Iranian J Publ Health 2002; 31:29–32 [Google Scholar]
- Seleem MN, Boyle SM, Sriranganathan N. Brucellosis: A re-emerging zoonosis. Vet Microbiol 2010; 140:392–398 [DOI] [PubMed] [Google Scholar]
- Woldehiwet Z. Q fever (coxiellosis): Epidemiology and pathogenesis. Res Vet Sci 2004; 77:93–100 [DOI] [PubMed] [Google Scholar]