The patient
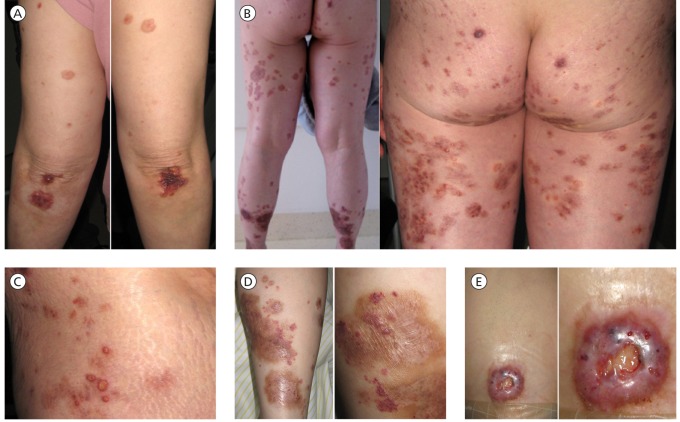
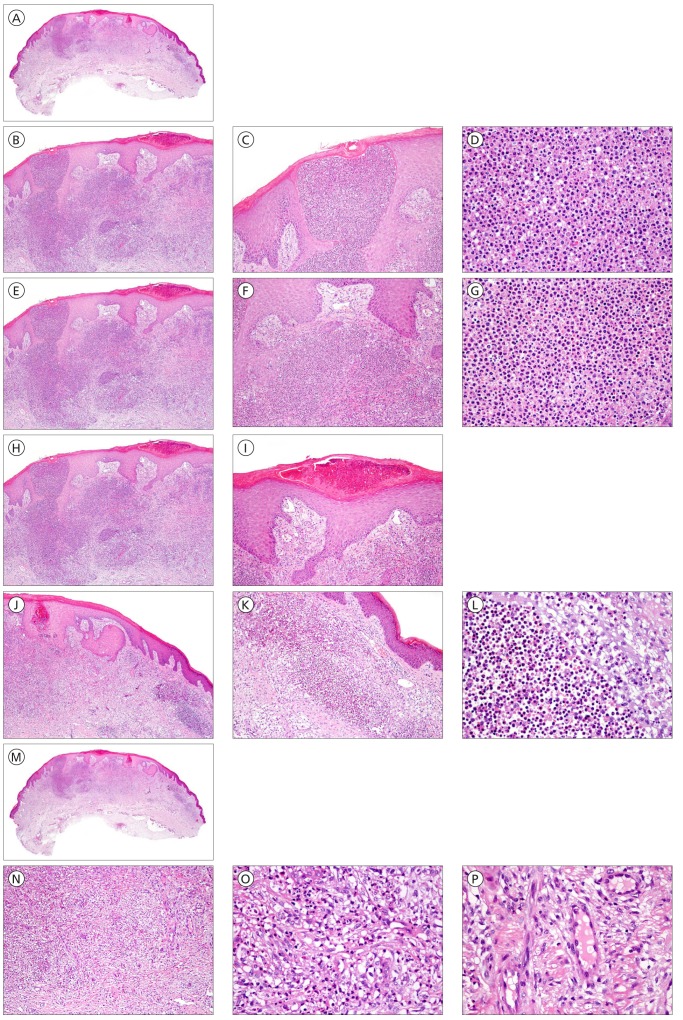
A 61-year-old woman presented herself with a chronic and widespread eruption of erythematous papules, pustules, ulcers, and hyperpigmented scars (Figures 1A–E). She had a history of rheumatoid arthritis. A biopsy specimen was taken from a plaque on the leg (Figures 2A–P). What is your diagnosis?
Figures 1A–E.
Clinical appearance of the widespread eruption of erythematous papules, pustules, ulcers, and hyperpigmented scars.
Figures 2A–P.
Histopathology.
Answer and explanation
Rheumatoid neutrophilic dermatitis
The section pictured in Figures 2A–P shows irregular epidermal and infundibular acanthosis and dilation of infundibula filled with neutrophils. Diffuse infiltrates are present in the dermis and are dominated by far by neutrophils. Some nuclear dust of neutrophils is present but there is no deposition of fibrin in the vessel walls. Fibrosis is seen in the deeper dermis. In the absence of clinical information, the best interpretation of the changes in this section is pyoderma gangrenosum.
The clinical pictures (Figures 1A–E), however, illustrate an extensive eruption that consists of erythematous papules, pustules, ulcers, and hyperpigmented scars. The clinical appearance taken together with the history of severe rheumatoid arthritis enables a diagnosis of rheumatoid neutrophilic dermatitis to be made based on clinicopathological correlation.
Rheumatoid neutrophilic dermatitis (RND) was first described by Ackerman in 1978 [1]. It appears in adults of both sexes with severe rheumatoid arthritis. Lesions are typically distributed symmetrically over joints of the elbows and knees. Individual lesions are papules, plaques and nodules, pustules, ulcerations, and scars. Urticarial lesions also have been observed in some patients [1–3]. Lesions come and go slowly over months or years [1].
RND is associated invariably with severe rheumatoid arthritis. Even though first described only in patients with high titers of rheumatoid factor, it was then shown to appear also in patients who are negative for a circulating rheumatoid factor [4].
Histopathologic changes have been described as a heavy dermal infiltrate of neutrophils with variable degrees of leukocytoclasis but no vasculitis [1, 4]. Fibrinoid degeneration of collagen, resembling the collagen changes present in rheumatoid nodules in a miniaturized form also has been reported [5].
The pattern of rheumatoid neutrophilic dermatitis bears many attributes in common with Sweet’s syndrome, on one hand, and pyoderma gangrenosum, on the other. Ackerman suggested that rheumatoid neutrophilic dermatitis could be a synonym for Sweet’s syndrome in a patient with severe rheumatoid arthritis because one of the conditions known to be responsible for Sweet’s syndrome is rheumatoid arthritis [6]. In contrast, association of rheumatoid neutrophilic dermatitis with pyoderma gangrenosum has been described [7]. In the patient presented here, some lesions were indistinguishable clinically from pyoderma gangrenosum, while typical lesions of Sweet syndrome were lacking. In clinicopathological correlation, RND seems to be distinct and different from both Sweet’s syndrome and pyoderma gangrenosum.
Rheumatoid arthritis is a chronic inflammatory arthritis that relatively commonly shows extra-articular manifestations, especially in the skin. Rheumatoid nodules, rheumatoid vasculitis, pyoderma gangrenosum, interstitial granulomatous dermatitis with arthritis, palisaded neutrophilic and granulomatous dermatitis, and rheumatoid neutrophilic dermatitis have been reported to be associated with the condition [8]. In comparison with other cutaneous manifestations of the disease, however, rheumatoid neutrophilic dermatitis is a very rare skin manifestation in patients with rheumatoid arthritis. In a relatively recent study of 215 patients with rheumatoid arthritis, only two were diagnosed with rheumatoid neutrophilic dermatitis [9].
Treatment of rheumatoid neutrophilic dermatitis is often difficult. Skin lesions do not respond necessarily to systemic treatment of the arthritis. Usually, dramatic response to systemic corticosteroids is seen. However, lesions quickly reappear on withdrawal of that medication.
References
- 1.Ackerman AB. A Method by Pattern Analysis. Philadelphia: Lea & Febiger; 1978. Histologic Diagnosis of Inflammatory Skin Diseases; p. 437. [Google Scholar]
- 2.Brown TS, Fearneyhough PK, Burruss JB, et al. Rheumatoid neutrophilic dermatitis in a woman with seronegative rheumatoid arthritis. J Am Acad Dermatol. 2001;45(4):596–600. doi: 10.1067/mjd.2001.119031. [DOI] [PubMed] [Google Scholar]
- 3.Ichikawa MM, Murata Y, Higaki Y, et al. Rheumatoid neutrophilic dermatitis. Eur J Dermatol. 1998;8(5):347–9. [PubMed] [Google Scholar]
- 4.Bevin AA, Steger J, Mannino S. Rheumatoid neutrophilic dermatitis. Cutis. 2006;78(2):133–6. [PubMed] [Google Scholar]
- 5.Lazarov A, Mor A, Cordoba M, et al. Rheumatoid neutrophilic dermatitis: an initial dermatological manifestation of seronegative rheumatoid arthritis. J Eur Acad Dermatol Venereol. 2002;16(1):74–6. doi: 10.1046/j.1468-3083.2002.00401.x. [DOI] [PubMed] [Google Scholar]
- 6.Ackerman AB, Böer A, Benin B, et al. An Algorithmic Method Based on Pattern Analysis. 3rd Edition. New York City: Ardor Scribendi, Ltd.; 2005. Histologic Diagnosis of Inflammatory Skin Diseases. [Google Scholar]
- 7.MacAya A, Servitje O, Jucglà A, et al. Rheumatoid neutrophilic dermatitis associated with pyoderma gangrenosum. Br J Dermatol. 2000;142(6):1246–8. doi: 10.1046/j.1365-2133.2000.03565.x. [DOI] [PubMed] [Google Scholar]
- 8.Sayah A, English JC., 3rd Rheumatoid arthritis: a review of the cutaneous manifestations. J Am Acad Dermatol. 2005;53(2):191–209. doi: 10.1016/j.jaad.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Ergun T, Inanc N, Tuney D, et al. Skin manifestations of rheumatoid arthritis: a study of 215 Turkish patients. Int J Dermatol. 2008;47(9):894–902. doi: 10.1111/j.1365-4632.2008.03708.x. [DOI] [PubMed] [Google Scholar]