Abstract
Traditionally, mitochondria have been regarded solely as energy generators for cells; however, accumulating data have demonstrated that these complex organelles play a variety of roles within the cardiomyocyte that extend beyond this classic function. Mitochondrial dynamics involves mitochondrial movements and morphologic alterations by tethering, fusion, and fission, which depend on cellular energy requirements and metabolic status. Many studies have indicated that mitochondrial dynamics may be a fundamental component of the maintenance of normal cellular homeostasis and cardiac function. Mitochondrial dynamics is controlled by the protein machinery responsible for mitochondrial fusion and fission, but cardiomyocytes are densely packed as part of an intricate cytoarchitecture for efficient and imbalanced contraction; thus, mitochondrial dynamics in the adult heart are restricted and occur more slowly than in other organs. Cardiac mitochondrial dynamics is important for cardiac physiology in diseased conditions such as ischemia-reperfusion (IR) injury. Changes in mitochondrial morphology through modulation of the expression of proteins regulating mitochondrial dynamics demonstrates the beneficial effects on cardiac performance after IR injury. Thus, accurately defining the roles of mitochondrial dynamics in the adult heart can guide the identification and development of novel therapeutic targets for cardioprotection. Further studies should be performed to establish the exact mechanisms of mitochondrial dynamics.
Keywords: Mitochondrial dynamics; Myocardial reperfusion injury; Myocytes, cardiac
INTRODUCTION
Mitochondria are typically regarded as energy generators, but the latest data demonstrate other divergent functions such as oxygen free radical production, control of cell ion homeostasis, and regulation of cell apoptosis and necrosis.1 Clearly, ATP generation is the most important role of mitochondria, especially in the heart. Because the heart requires a continuous supply of energy throughout life, cardiomyocytic mitochondria are densely packed to form a complex structure accounting for -35% of cardiac muscle cell volume.2 The cardiomyocytic mitochondria maintain the largest relative density of any organ in the body and build a highly organized and solid cytoarchitecture with other organelles. Their regulatory pathway is not fully understood, but many studies have suggested that ADP/ATP/inorganic phosphorus and cytosolic calcium (Ca2+) are essential to regulate oxidative phosphorylation and energy generation.3-6 Most cytosolic Ca2+ is released from the sarcoplasmic reticulum (SR) and acts as a crucial element for contraction of myocytes. Thus, its harmonic import and export via the T-tubules are essential for normal excitation-contraction coupling.7
The term "mitochondrial dynamics" connotes the mitochondrial movements, morphologic and distributional alterations, mitophagy, and tethering/fusion/fission that depend on energy requirements and metabolic status.8-10 It is finely controlled by intricate protein machinery11 and exhibits high organ specificity. For example, mitochondria in neurons, fibroblasts, and other cells change their locations actively, whereas in adult cardiomyocytes, they are not able to move easily owing to the peculiar subcellular environment, i.e., rigid cytoskeleton and abundance of myofilaments.12 Accumulating data, however, suggest that the proteins involved in cardiac mitochondrial dynamics are important for cardiac physiology in normal and diseased conditions. Here, we review new concepts and evidence for cardiac mitochondrial dynamics.
MITOCHONDRIAL DYNAMICS IN THE HEART
Many early experimental studies investigating mitochondrial dynamics were carried out by use of noncardiac cells. In recent years, however, there have also been studies on mitochondrial dynamics in the heart. Because of their unfettered movement and the comparatively homogeneous reticular distribution pattern of mitochondria, the cells employed in the majority of studies were neonatal cardiomyocytes, immortal cardiac cell lines, or vascular cells.13-23 Adult cardiomyocytes are organized by a complex cytoarchitecture for efficient and finely controlled contraction so that mitochondrial movements are significantly restricted. But more recent studies have proposed that regulation of mitochondrial dynamics is also present in adult cardiomyocytes, indicating that adult cardiac mitochondria have preserved their fusion, fission, and mitophagy abilities.
1. Mitochondrial distribution and subpopulations in adult cardiomyocytes
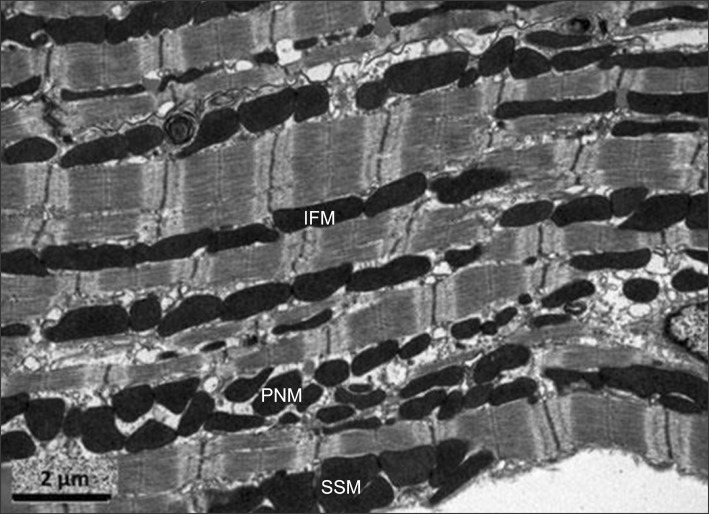
Mitochondria are an indispensable part of the cardiac cytoarchitecture and are arranged in three distinct subpopulations in the adult heart: intermyofibrillar mitochondria, subsarcolemmal mitochondria, and perinuclear mitochondria.24 Intermyofibrillar mitochondria are aligned along the myofibrils and function as a main producer of ATP. They are actively in contact with the surrounding SR and myofibrils.12,25 Subsarcolemmal mitochondria are arranged just beneath the sarcolemma and are possibly involved in ion homeostasis or signaling pathways.26,27 Last, perinuclear mitochondria are adjacent to the nucleus and probably participate in the nuclear transcription and translocation processes, but the exact mechanism has not yet been elucidated (Fig. 1).
FIG. 1.
The three subpopulations of mitochondria: interfibrillar mitochondria (IFM), perinuclear mitochondria (PNM), and subsarcolemmal mitochondria (SSM). Reprinted with permission from Ong et al.84
2. Mitochondrial fusion
Mitochondria have a double-membrane structure including the outer mitochondrial membrane (OMM) and inner mitochondrial membrane (IMM). The OMM encloses the entire organelle, isolating the contents from the cytoplasm, and contains numerous porins for passive and active transport of molecules. The IMM divides the internal substance into a matrix core and an intermembranous space, which is compartmentalized into an abundance of cristae. This double-membrane structure is an essential part of distinguishing between the enzymes required for ATP generation, but hinders mitochondrial tethering and fusion.
Mitochondrial fusion of the OMM and IMM occurs individually and sequentially and is mediated by distinct proteins containing GTPase and coiled-coil domains (heptad-repeat domains, HR1 and HR2). Fusion of the OMM is regulated by mitofusins (Mfn1, Mfn2) located in the outer membrane,28,29 whereas fusion of the IMM is arbitrated by optic atrophy 1 (Opa1) present in the inner membrane.30 Structurally, the proteins share an extracellular amino terminal GTPase domain mediating GTP hydrolysis, a transmembrane (TM) domain allowing the anchorage of the proteins to the membranes, and HR domains involved in homotypic (e.g., Mfn1-Mfn1, Mfn2-Mfn2, and Opa1-Opa1) and heterotypic (e.g., Mfn1-Mfn2) interactions.23,31
Human mitofusins were first discovered by the Santel group in 2001.28 Mitofusins reside in the OMM and act as a starter for the mitochondrial fusion process. The HR2 domains of mitofusins on one mitochondrion are assumed to develop complexes with mitofusins on other mitochondria, and these complexes initiate tethering and fusion between neighboring mitochondria.32 Mfn1 has higher GTPase activity than does Mfn2, so it is reported that Mfn1 tethers mitochondria more efficiently than does Mfn2.33 As mentioned, mitofusins can interact both homotypically and heterotypically; thus, the fusion process has adaptability. Mfn1 or Mfn2 single knockout cells or tissues do not prevent fusion, but Mfn1 and Mfn2 double knockout cells or tissues demonstrate marked mitochondrial fragmentation.34-36
Opa1 is expressed throughout the body, and it mediates the IMM fusion process and modulates apoptotic cristae remodeling.37 Mutations in the Opa1 gene are related to autosomal dominant optic atrophy.38 Opa1 has 8 human isoforms and is cleaved by mitochondrial protease. As a result, short forms of Opa1 (S-Opa1) and long forms of Opa1 (L-Opa1) are generated. The former is water-soluble and is located in the intermembranous space, whereas the latter has a TM domain and is anchored in the IMM.11 Genetic ablation of Opa1 also prevents mitochondrial fusion and produces mitochondrial fragmentation.39,40
3. Mitochondrial fission
Mitochondrial fusion mechanisms are thought to be relatively well established, but mitochondrial fission processes have not been fully clarified. Fission processes are probably divided into several stages: mitochondrial constriction, dynamin-related peptide 1 (Drp1) recruitment, fission complex assembly on the OMM, de facto mitochondrial fission, and fission complex dismantling.11
Drp1, also called dynamin-like protein 1 (Dlp-1), is a cytosolic protein that has a GTPase domain and a GTPase effector (assembly) domain.41 Drp1 translocates to the fission site on the OMM of the mitochondria via cytosolic dynein or the actin network.42,43 After proper translocation, Drp1 oligomerizes to form a ring and constricts the mitochondrial fission site in a GTP-dependent manner. Drp1 has no TM domain for anchoring to the mitochondrial membrane, so it requires a docking receptor on the OMM. Human mitochondrial fission protein 1 (Fis1) was the first protein regarded as a mitochondrial receptor for Drp1.44 It is a small protein (17 kDa) anchoring to the OMM, and its amino-terminus contains five α-helices that allow interaction with Drp1.45 Fis1 is thought to conduct suborganelle localization of activated Drp1 oligomer to the constrictive site of mitochondria and facilitates the mitochondrial fission process.46
Some studies have suggested that Fis1 deficiency does not influence the recruitment of Drp1.47,48 Some investigators found three other proteins involved in mitochondrial fission located on the OMM: mitochondrial fission factor (Mff) and mitochondrial dynamics proteins of 49 kDA or 51 kDA (MiD49 and MiD51). However, the exact mechanisms underlying the fission process remain unclear.
4. Mitochondrial trafficking
Mitochondrial trafficking is controlled by specific proteins such as mitochondrial Miro1 and Miro2 and cytosolic Grif-1 and OIP106 in a calcium-dependent manner. Miro proteins are located on the OMM and comprise two Ras-GTPase domains, a TM domain, and calcium-sensitive EF motifs.49 Cytosolic Grif-1 and OIP106 bind Miro proteins and motor molecules (dynein, kinesin), inducing mitochondrial trafficking along microtubules.50 Miro proteins are reported to influence mitochondrial morphology in immortalized cardiac cells (H9c2 cells). Their overexpression leads to mitochondrial elongation; on the other hand, genetic ablation of Miro genes induces mitochondrial fragmentation.13 However, the roles of mitochondrial motility proteins are restricted in adult cardiomyocytes owing to the complex and dense cytoarchitecture.
ALTERED MITOCHONDRIAL DYNAMICS IN HEART DISEASE
Mitochondria modulate cardiomyocyte contractility by supplying ATP and participating in calcium homeostasis. Some studies have suggested that altered mitochondrial morphology is directly involved in the detriment to cardiac function under stress.51,52 However, the precise mechanisms by which mitochondria interact with cardiac myofibrils are not fully understood.
1. Mitochondrial permeability transition pore (MPTP)
The mitochondrial permeability transition pore (MPTP) is a nonselective channel located on the IMM. It is permeable to solutes up to 1.5 kDa and mediates the degree of mitochondrial permeability by alteration of mitochondrial membrane potential. Excessive production of reactive oxygen species (ROS) and calcium overload in the mitochondrial matrix dissipate the proton electrochemical gradient (ΔΨm) and open the MPTP. This leads to uncoupling of oxidative phosphorylation and further production of ROS, resulting in ATP depletion and mitochondrial rupture.53,54 This in turn releases proapoptotic proteins such as cytochrome c, Smac/DIABLO, and endonuclease-G (endoG), which activate the caspase protease system and ultimately induce apoptosis or necrosis of the cell.1,54-56
Numerous heart diseases are related to increases in MPTP activators such as calcium and oxidative stress and reductions in MPTP inhibitors such as ATP/ADP. Several studies have demonstrated that inhibition of the MPTP pore lessens the cardiomyocyte loss that underlies some cardiac pathologies including myocardial ischemia/reperfusion (IR) injury,57,58 calcium-induced cardiomyopathy,59 diabetic cardiomyopathy,60 and the cardiotoxicity of anti-cancer drugs.61
There have been a few studies of the relationships between mitochondrial fusion proteins and the MPTP opening. In accordance with these studies, lack of Opa1 and Mfns was associated with delayed MPTP opening,18,51,52 which suggested that mitochondrial fusion proteins expedite MPTP opening under normal conditions. However, Neuspiel et al.62 demonstrated that the overexpression of Mfn2 protects against MPTP opening. Further investigations are required to elucidate the exact mechanisms involved in these phenomena.
2. Mitochondrial dynamics and apoptosis in cardiac cells
Studies on the relationships between mitochondrial dynamics and apoptosis are at an early stage even now. Mfn2 is being highlighted as a regulator of the apoptotic process, but its primary actions remain controversial. Guo et al.63 and Shen et al.64 suggested that Mfn2 may function as a pro-apoptotic modulator by suppressing the phosophoinositide 3-kinase (PI3K)-Akt pathway under oxidative stress in vascular smooth muscle cells and H9c2 cells, respectively. On the other hand, Parra et al. reported that ablation of Mfn2 exacerbated the ceramide-induced pro-apoptotic processes such as mitochondrial fragmentation, Drp1 localization, and release of cytochrome c in neonatal cardiomyocytes.21
3. Mitochondrial dynamics and myocardial ischemia-reperfusion injury
In coronary artery disease, the most effective therapeutic option for reducing ischemic myocardial injury and infarct size is prompt and efficient myocardial reperfusion, but the myocardial reperfusion process can induce further myocardial cell death. This phenomenon is called myocardial IR injury.65,66 The outcomes of IR injury are reversible (arrhythmia, myocardial stunning) or irreversible (microvascular obstruction, cardiomyocytic death). Oxidative stress, intracellular calcium overload, MTPT opening, and hypercontracture of myofibrils are important contributory factors in lethal myocardial IR injury.66
Mitochondrial fission and fragmentation are commonly observed in cells with IR injury. Chen et al.67 found that the deficiency of OPA1 is closely associated with IR-induced mitochondrial fragmentation in H9c2 cells. Additionally, Ong et al.68 elucidated that mitochondrial fragmentation during myocardial ischemia turns on the actions of Drp1 in HL-1 cell lines. The exact activation process of Drp1 under ischemic conditions is not fully understood, but calcineurin-induced dephosphorylation of Drp1 by mitochondrial calcium overload has been observed in some studies.69,70
4. Mitochondrial dynamics and other heart diseases
Until recently, mitochondrial fusion proteins were relatively disregarded in studies on human heart disease, and in fact, Charcot-Marie-Tooth syndrome and autosomal dominant optic atrophy caused by functional loss of Mfn2 and Opa1, respectively, show no cardiac manifestations.71 However, there has been some evidence that cardiomyopathies are the result of an imbalance in mitochondrial dynamics, and that heart failure is related to altered cardiac mitochondrial morphology.
The integrity of the mitochondrial network is compromised and the mitochondrial membrane is disrupted in chronically failed hearts. Additionally, reductions in the total mitochondrial number and size have also been observed.72,73 Sabba et al.74 and Di Lisa et al.75 suggested that these phenomena are positively correlated with the heart failure severity index and are capable of determining the destiny of cardiac cells. Furthermore, recent studies have suggested that Opa1 deficiency decreases the expression of nuclear antioxidant genes, induces fragmentation of cardiac mitochondria, and results in late-onset heart failure.67,76
Changes in mitochondrial dynamics have also been observed in dilated cardiomyopathy. A heterozygous Drp1 gene mutation (C452F) gave rise to severe dilated cardiomyopathy after 11 weeks in mice.77 Selective ablation of Mfn1 and Mfn2 also resulted in severe dilated cardiomyopathy in a mouse model, whereas combined Mfn1/Mfn2 ablation was lethal.36 Both studies demonstrated defects in mitochondrial respiration and mitochondrial fragmentation.
MITOCHONDRIAL DYNAMICS AS A NOVEL THERAPEUTIC TARGET
Modification of mitochondrial dynamics has emerged as a novel pharmacological strategy for cardioprotection, especially in IR injury. Previous studies reported that trimetazidine reduced infarct size in animal ischemic heart models.78,79 The exact mechanism is not fully understood, but there has been some evidence that trimetazidine decreases ROS production and delays calcium-mediated MPTP opening via re-coupling of the mitochondrial respiratory chain.80-82 Ranolazine also demonstrated similar effects on mitochondria and reduced additional IR injury.83 The proteins modulating mitochondrial dynamics are regarded as an essential component of appropriate mitochondrial and cell survival, and ultimately, normal cardiac function, but their pharmacological use is still not realized.
1. Mitochondrial dynamics as a therapeutic target for cardioprotection
Altering mitochondrial morphology by regulating the expression of the proteins involved in mitochondrial dynamics has demonstrated beneficial effects on cardiac performance after IR injury in some studies. Mdiv-1, a Drp1-specific inhibitor, impeded mitochondrial fragmentation, as determined by electron microscopy; delayed the opening of MPTP; and reduced myocardial infarct size significantly in in vivo murine hearts as well as in HL-1 cells.68 Wang et al.70 reported that microRNA-499 (miR-499), which inhibits the calcineurin-dependent activation of Drp-1, as mentioned above, could protect against IR injury. Thus, short-term inhibition of Drp1 during IR injury may be advantageous for effective cardioprotection. However, the adult hearts of Mfn2 knockout mice exhibit an enlargement of the subsarcolemmal mitochondria, depolarization of the mitochondrial membrane, delayed MPTP opening, and also improvement of cardiac function following ex vivo IR injury compared with mice from the control group.51 These findings contrast with the results of other studies that demonstrated a beneficial role of Mfn2 in terms of MPTP opening in neurons62 and HL-1 cells.68 These findings suggest that the effects of Mfn2 are cell-specific and may change with mitochondrial cell development but have not yet been fully elucidated.84
SUMMARY
Numerous studies have described how mitochondrial dynamics may be essential in the maintenance of normal mitochondrial and cellular homeostasis and cardiac function. Mitochondrial dynamics is modulated by complex protein machinery regulating the fusion and fission of mitochondria. In adult heart, cardiomyocytes are organized by an intricate cytoarchitecture for efficient and well-modulated contraction, and thus, mitochondrial movements are markedly restricted and morphological changes of the mitochondria are more slowly controlled than in other organs.
Mitochondrial dynamics is a crucial component for the adaptation of cardiomyocytes under stresses such as IR injury. Rats with genetically manipulated mitochondrial dynamics genes are especially vulnerable to ischemia, and the proteins encoded by these genes act as key determinants of cellular fates in such environments.
Accordingly, identifying the various roles of mitochondrial dynamics in the adult heart could result in the development of novel therapeutic targets for cardioprotection. Further animal- and human-based studies should be performed to establish the exact mechanisms underlying mitochondrial dynamics.
Footnotes
None declared.
References
- 1.Crow MT, Mani K, Nam YJ, Kitsis RN. The mitochondrial death pathway and cardiac myocyte apoptosis. Circ Res. 2004;95:957–970. doi: 10.1161/01.RES.0000148632.35500.d9. [DOI] [PubMed] [Google Scholar]
- 2.Page E, McCallister LP. Quantitative electron microscopic description of heart muscle cells. Application to normal, hypertrophied and thyroxin-stimulated hearts. Am J Cardiol. 1973;31:172–181. doi: 10.1016/0002-9149(73)91030-8. [DOI] [PubMed] [Google Scholar]
- 3.Balaban RS, Kantor HL, Katz LA, Briggs RW. Relation between work and phosphate metabolite in the in vivo paced mammalian heart. Science. 1986;232:1121–1123. doi: 10.1126/science.3704638. [DOI] [PubMed] [Google Scholar]
- 4.Cortassa S, Aon MA, Marbán E, Winslow RL, O'Rourke B. An integrated model of cardiac mitochondrial energy metabolism and calcium dynamics. Biophys J. 2003;84:2734–2755. doi: 10.1016/S0006-3495(03)75079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz LA, Swain JA, Portman MA, Balaban RS. Relation between phosphate metabolites and oxygen consumption of heart in vivo. Am J Physiol. 1989;256:H265–H274. doi: 10.1152/ajpheart.1989.256.1.H265. [DOI] [PubMed] [Google Scholar]
- 6.Maack C, Cortassa S, Aon MA, Ganesan AN, Liu T, O'Rourke B. Elevated cytosolic Na+ decreases mitochondrial Ca2+ uptake during excitation-contraction coupling and impairs energetic adaptation in cardiac myocytes. Circ Res. 2006;99:172–182. doi: 10.1161/01.RES.0000232546.92777.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bers DM. Calcium cycling and signaling in cardiac myocytes. Annu Rev Physiol. 2008;70:23–49. doi: 10.1146/annurev.physiol.70.113006.100455. [DOI] [PubMed] [Google Scholar]
- 8.Bereiter-Hahn J. Behavior of mitochondria in the living cell. Int Rev Cytol. 1990;122:1–63. doi: 10.1016/s0074-7696(08)61205-x. [DOI] [PubMed] [Google Scholar]
- 9.Rossignol R, Gilkerson R, Aggeler R, Yamagata K, Remington SJ, Capaldi RA. Energy substrate modulates mitochondrial structure and oxidative capacity in cancer cells. Cancer Res. 2004;64:985–993. doi: 10.1158/0008-5472.can-03-1101. [DOI] [PubMed] [Google Scholar]
- 10.Soubannier V, McBride HM. Positioning mitochondrial plasticity within cellular signaling cascades. Biochim Biophys Acta. 2009;1793:154–170. doi: 10.1016/j.bbamcr.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Liesa M, Palacín M, Zorzano A. Mitochondrial dynamics in mammalian health and disease. Physiol Rev. 2009;89:799–845. doi: 10.1152/physrev.00030.2008. [DOI] [PubMed] [Google Scholar]
- 12.Vendelin M, Béraud N, Guerrero K, Andrienko T, Kuznetsov AV, Olivares J, et al. Mitochondrial regular arrangement in muscle cells: a "crystal-like" pattern. Am J Physiol Cell Physiol. 2005;288:C757–C767. doi: 10.1152/ajpcell.00281.2004. [DOI] [PubMed] [Google Scholar]
- 13.Saotome M, Safiulina D, Szabadkai G, Das S, Fransson A, Aspenstrom P, et al. Bidirectional Ca2+-dependent control of mitochondrial dynamics by the Miro GTPase. Proc Natl Acad Sci U S A. 2008;105:20728–20733. doi: 10.1073/pnas.0808953105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O-Uchi J, Jhun BS, Hurst S, Bisetto S, Gross P, Chen M, et al. Overexpression of ryanodine receptor type 1 enhances mitochondrial fragmentation and Ca2+-induced ATP production in cardiac H9c2 myoblasts. Am J Physiol Heart Circ Physiol. 2013 doi: 10.1152/ajpheart.00094.2013. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beraud N, Pelloux S, Usson Y, Kuznetsov AV, Ronot X, Tourneur Y, et al. Mitochondrial dynamics in heart cells: very low amplitude high frequency fluctuations in adult cardiomyocytes and flow motion in non beating Hl-1 cells. J Bioenerg Biomembr. 2009;41:195–214. doi: 10.1007/s10863-009-9214-x. [DOI] [PubMed] [Google Scholar]
- 16.Chalmers S, Saunter C, Wilson C, Coats P, Girkin JM, McCarron JG. Mitochondrial motility and vascular smooth muscle proliferation. Arterioscler Thromb Vasc Biol. 2012;32:3000–3011. doi: 10.1161/ATVBAHA.112.255174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poburko D, Liao CH, van Breemen C, Demaurex N. Mitochondrial regulation of sarcoplasmic reticulum Ca2+ content in vascular smooth muscle cells. Circ Res. 2009;104:104–112. doi: 10.1161/CIRCRESAHA.108.180612. [DOI] [PubMed] [Google Scholar]
- 18.Papanicolaou KN, Kikuchi R, Ngoh GA, Coughlan KA, Dominguez I, Stanley WC, et al. Mitofusins 1 and 2 are essential for postnatal metabolic remodeling in heart. Circ Res. 2012;111:1012–1026. doi: 10.1161/CIRCRESAHA.112.274142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Makino A, Suarez J, Gawlowski T, Han W, Wang H, Scott BT, et al. Regulation of mitochondrial morphology and function by O-GlcNAcylation in neonatal cardiac myocytes. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1296–R1302. doi: 10.1152/ajpregu.00437.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Din S, Mason M, Völkers M, Johnson B, Cottage CT, Wang Z, et al. Pim-1 preserves mitochondrial morphology by inhibiting dynamin-related protein 1 translocation. Proc Natl Acad Sci U S A. 2013;110:5969–5974. doi: 10.1073/pnas.1213294110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parra V, Eisner V, Chiong M, Criollo A, Moraga F, Garcia A, et al. Changes in mitochondrial dynamics during ceramide-induced cardiomyocyte early apoptosis. Cardiovasc Res. 2008;77:387–397. doi: 10.1093/cvr/cvm029. [DOI] [PubMed] [Google Scholar]
- 22.Liao XD, Wang XH, Jin HJ, Chen LY, Chen Q. Mechanical stretch induces mitochondria-dependent apoptosis in neonatal rat cardiomyocytes and G2/M accumulation in cardiac fibroblasts. Cell Res. 2004;14:16–26. doi: 10.1038/sj.cr.7290198. [DOI] [PubMed] [Google Scholar]
- 23.Chen H, Detmer SA, Ewald AJ, Griffin EE, Fraser SE, Chan DC. MitofusinsMfn1 and Mfn2 coordinately regulate mitochondrial fusion and are essential for embryonic development. J Cell Biol. 2003;160:189–200. doi: 10.1083/jcb.200211046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoppel CL, Tandler B, Fujioka H, Riva A. Dynamic organization of mitochondria in human heart and in myocardial disease. Int J Biochem Cell Biol. 2009;41:1949–1956. doi: 10.1016/j.biocel.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuznetsov AV, Hermann M, Saks V, Hengster P, Margreiter R. The cell-type specificity of mitochondrial dynamics. Int J Biochem Cell Biol. 2009;41:1928–1939. doi: 10.1016/j.biocel.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Palmer JW, Tandler B, Hoppel CL. Heterogeneous response of subsarcolemmal heart mitochondria to calcium. Am J Physiol. 1986;250:H741–H748. doi: 10.1152/ajpheart.1986.250.5.H741. [DOI] [PubMed] [Google Scholar]
- 27.Riva A, Tandler B, Loffredo F, Vazquez E, Hoppel C. Structural differences in two biochemically defined populations of cardiac mitochondria. Am J Physiol Heart Circ Physiol. 2005;289:H868–H872. doi: 10.1152/ajpheart.00866.2004. [DOI] [PubMed] [Google Scholar]
- 28.Santel A, Fuller MT. Control of mitochondrial morphology by a human mitofusin. J Cell Sci. 2001;114:867–874. doi: 10.1242/jcs.114.5.867. [DOI] [PubMed] [Google Scholar]
- 29.Legros F, Lombès A, Frachon P, Rojo M. Mitochondrial fusion in human cells is efficient, requires the inner membrane potential, and is mediated by mitofusins. Mol Biol Cell. 2002;13:4343–4354. doi: 10.1091/mbc.E02-06-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alexander C, Votruba M, Pesch UE, Thiselton DL, Mayer S, Moore A, et al. OPA1, encoding a dynamin-related GTPase, is mutated in autosomal dominant optic atrophy linked to chromosome 3q28. Nat Genet. 2000;26:211–215. doi: 10.1038/79944. [DOI] [PubMed] [Google Scholar]
- 31.Santel A, Frank S, Gaume B, Herrler M, Youle RJ, Fuller MT. Mitofusin-1 protein is a generally expressed mediator of mitochondrial fusion in mammalian cells. J Cell Sci. 2003;116:2763–2774. doi: 10.1242/jcs.00479. [DOI] [PubMed] [Google Scholar]
- 32.Koshiba T, Detmer SA, Kaiser JT, Chen H, McCaffery JM, Chan DC. Structural basis of mitochondrial tethering by mitofusin complexes. Science. 2004;305:858–862. doi: 10.1126/science.1099793. [DOI] [PubMed] [Google Scholar]
- 33.Ishihara N, Eura Y, Mihara K. Mitofusin 1 and 2 play distinct roles in mitochondrial fusion reactions via GTPase activity. J Cell Sci. 2004;117:6535–6546. doi: 10.1242/jcs.01565. [DOI] [PubMed] [Google Scholar]
- 34.Chen H, Chomyn A, Chan DC. Disruption of fusion results in mitochondrial heterogeneity and dysfunction. J Biol Chem. 2005;280:26185–26192. doi: 10.1074/jbc.M503062200. [DOI] [PubMed] [Google Scholar]
- 35.Chen H, McCaffery JM, Chan DC. Mitochondrial fusion protects against neurodegeneration in the cerebellum. Cell. 2007;130:548–562. doi: 10.1016/j.cell.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 36.Chen Y, Liu Y, Dorn GW., 2nd Mitochondrial fusion is essential for organelle function and cardiac homeostasis. Circ Res. 2011;109:1327–1331. doi: 10.1161/CIRCRESAHA.111.258723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frezza C, Cipolat S, Martins de Brito O, Micaroni M, Beznoussenko GV, Rudka T, et al. OPA1 controls apoptotic cristae remodeling independently from mitochondrial fusion. Cell. 2006;126:177–189. doi: 10.1016/j.cell.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 38.Delettre C, Lenaers G, Griffoin JM, Gigarel N, Lorenzo C, Belenguer P, et al. Nuclear gene OPA1, encoding a mitochondrial dynamin-related protein, is mutated in dominant optic atrophy. Nat Genet. 2000;26:207–210. doi: 10.1038/79936. [DOI] [PubMed] [Google Scholar]
- 39.Dorn GW, 2nd, Clark CF, Eschenbacher WH, Kang MY, Engelhard JT, Warner SJ, et al. MARF and Opa1 control mitochondrial and cardiac function in Drosophila. Circ Res. 2011;108:12–17. doi: 10.1161/CIRCRESAHA.110.236745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song Z, Ghochani M, McCaffery JM, Frey TG, Chan DC. Mitofusins and OPA1 mediate sequential steps in mitochondrial membrane fusion. Mol Biol Cell. 2009;20:3525–3532. doi: 10.1091/mbc.E09-03-0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smirnova E, Shurland DL, Ryazantsev SN, van der Bliek AM. A human dynamin-related protein controls the distribution of mitochondria. J Cell Biol. 1998;143:351–358. doi: 10.1083/jcb.143.2.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Varadi A, Johnson-Cadwell LI, Cirulli V, Yoon Y, Allan VJ, Rutter GA. Cytoplasmic dynein regulates the subcellular distribution of mitochondria by controlling the recruitment of the fission factor dynamin-related protein-1. J Cell Sci. 2004;117:4389–4400. doi: 10.1242/jcs.01299. [DOI] [PubMed] [Google Scholar]
- 43.De Vos KJ, Allan VJ, Grierson AJ, Sheetz MP. Mitochondrial function and actin regulate dynamin-related protein 1-dependent mitochondrial fission. Curr Biol. 2005;15:678–683. doi: 10.1016/j.cub.2005.02.064. [DOI] [PubMed] [Google Scholar]
- 44.Yoon Y, Krueger EW, Oswald BJ, McNiven MA. The mitochondrial protein hFis1 regulates mitochondrial fission in mammalian cells through an interaction with the dynamin-like protein DLP1. Mol Cell Biol. 2003;23:5409–5420. doi: 10.1128/MCB.23.15.5409-5420.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jofuku A, Ishihara N, Mihara K. Analysis of functional domains of rat mitochondrialFis1, the mitochondrial fission-stimulating protein. Biochem Biophys Res Commun. 2005;333:650–659. doi: 10.1016/j.bbrc.2005.05.154. [DOI] [PubMed] [Google Scholar]
- 46.Lackner LL, Horner JS, Nunnari J. Mechanistic analysis of a dynamin effector. Science. 2009;325:874–877. doi: 10.1126/science.1176921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee YJ, Jeong SY, Karbowski M, Smith CL, Youle RJ. Roles of the mammalian mitochondrial fission and fusion mediators Fis1, Drp1, and Opa1 in apoptosis. Mol Biol Cell. 2004;15:5001–5011. doi: 10.1091/mbc.E04-04-0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wasiak S, Zunino R, McBride HM. Bax/Bak promote sumoylation of DRP1 and its stable association with mitochondria during apoptotic cell death. J Cell Biol. 2007;177:439–450. doi: 10.1083/jcb.200610042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fransson S, Ruusala A, Aspenström P. The atypical Rho GTPases Miro-1 and Miro-2 have essential roles in mitochondrial trafficking. Biochem Biophys Res Commun. 2006;344:500–510. doi: 10.1016/j.bbrc.2006.03.163. [DOI] [PubMed] [Google Scholar]
- 50.Rice SE, Gelfand VI. Paradigm lost: milton connects kinesin heavy chain to miro on mitochondria. J Cell Biol. 2006;173:459–461. doi: 10.1083/jcb.200604071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Papanicolaou KN, Khairallah RJ, Ngoh GA, Chikando A, Luptak I, O'Shea KM, et al. Mitofusin-2 maintains mitochondrial structure and contributes to stress-induced permeability transition in cardiac myocytes. Mol Cell Biol. 2011;31:1309–1328. doi: 10.1128/MCB.00911-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Piquereau J, Caffin F, Novotova M, Prola A, Garnier A, Mateo P, et al. Down-regulation of OPA1 alters mouse mitochondrial morphology, PTP function, and cardiac adaptation to pressure overload. Cardiovasc Res. 2012;94:408–417. doi: 10.1093/cvr/cvs117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hausenloy DJ, Yellon DM. The mitochondrial permeability transition pore: its fundamental role in mediating cell death during ischaemia and reperfusion. J Mol Cell Cardiol. 2003;35:339–341. doi: 10.1016/s0022-2828(03)00043-9. [DOI] [PubMed] [Google Scholar]
- 54.Baines CP. The molecular composition of the mitochondrial permeability transition pore. J Mol Cell Cardiol. 2009;46:850–857. doi: 10.1016/j.yjmcc.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Murphy E, Steenbergen C. Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol Rev. 2008;88:581–609. doi: 10.1152/physrev.00024.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kroemer G, Galluzzi L, Brenner C. Mitochondrial membrane permeabilization in cell death. Physiol Rev. 2007;87:99–163. doi: 10.1152/physrev.00013.2006. [DOI] [PubMed] [Google Scholar]
- 57.Hausenloy DJ, Duchen MR, Yellon DM. Inhibiting mitochondrial permeability transition pore opening at reperfusion protects against ischaemia-reperfusion injury. Cardiovasc Res. 2003;60:617–625. doi: 10.1016/j.cardiores.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 58.Piot C, Croisille P, Staat P, Thibault H, Rioufol G, Mewton N, et al. Effect of cyclosporine on reperfusion injury in acute myocardial infarction. N Engl J Med. 2008;359:473–481. doi: 10.1056/NEJMoa071142. [DOI] [PubMed] [Google Scholar]
- 59.Nakayama H, Chen X, Baines CP, Klevitsky R, Zhang X, Zhang H, et al. Ca2+- and mitochondrial-dependent cardiomyocyte necrosis asa primary mediator of heart failure. J Clin Invest. 2007;117:2431–2444. doi: 10.1172/JCI31060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Oliveira PJ, Seiça R, Coxito PM, Rolo AP, Palmeira CM, Santos MS, et al. Enhanced permeability transition explains the reduced calcium uptake in cardiac mitochondria from streptozotocin-induced diabetic rats. FEBS Lett. 2003;554:511–514. doi: 10.1016/s0014-5793(03)01233-x. [DOI] [PubMed] [Google Scholar]
- 61.Kerkelä R, Grazette L, Yacobi R, Iliescu C, Patten R, Beahm C, et al. Cardiotoxicity of the cancer therapeutic agent imatinib mesylate. Nat Med. 2006;12:908–916. doi: 10.1038/nm1446. [DOI] [PubMed] [Google Scholar]
- 62.Neuspiel M, Zunino R, Gangaraju S, Rippstein P, McBride H. Activated mitofusin 2 signals mitochondrial fusion, interferes with Bax activation, and reduces susceptibility to radical induced depolarization. J Biol Chem. 2005;280:25060–25070. doi: 10.1074/jbc.M501599200. [DOI] [PubMed] [Google Scholar]
- 63.Guo X, Chen KH, Guo Y, Liao H, Tang J, Xiao RP. Mitofusin 2 triggers vascular smooth muscle cell apoptosis via mitochondrial death pathway. Circ Res. 2007;101:1113–1122. doi: 10.1161/CIRCRESAHA.107.157644. [DOI] [PubMed] [Google Scholar]
- 64.Shen T, Zheng M, Cao C, Chen C, Tang J, Zhang W, et al. Mitofusin-2 is a major determinant of oxidative stress-mediated heart muscle cell apoptosis. J Biol Chem. 2007;282:23354–23361. doi: 10.1074/jbc.M702657200. [DOI] [PubMed] [Google Scholar]
- 65.Piper HM, García-Dorado D, Ovize M. A fresh look at reperfusion injury. Cardiovasc Res. 1998;38:291–300. doi: 10.1016/s0008-6363(98)00033-9. [DOI] [PubMed] [Google Scholar]
- 66.Yellon DM, Hausenloy DJ. Myocardial reperfusion injury. N Engl J Med. 2007;357:1121–1135. doi: 10.1056/NEJMra071667. [DOI] [PubMed] [Google Scholar]
- 67.Chen L, Gong Q, Stice JP, Knowlton AA. Mitochondrial OPA1, apoptosis, and heart failure. Cardiovasc Res. 2009;84:91–99. doi: 10.1093/cvr/cvp181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ong SB, Subrayan S, Lim SY, Yellon DM, Davidson SM, Hausenloy DJ. Inhibiting mitochondrial fission protects the heart against ischemia/reperfusion injury. Circulation. 2010;121:2012–2022. doi: 10.1161/CIRCULATIONAHA.109.906610. [DOI] [PubMed] [Google Scholar]
- 69.Cereghetti GM, Stangherlin A, Martins de, Chang CR, Blackstone C, Bernardi P, et al. Dephosphorylation by calcineurin regulates translocation of Drp1 to mitochondria. Proc Natl Acad Sci U S A. 2008;105:15803–15808. doi: 10.1073/pnas.0808249105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang JX, Jiao JQ, Li Q, Long B, Wang K, Liu JP, et al. miR-499 regulates mitochondrial dynamics by targeting calcineurin and dynamin-related protein-1. Nat Med. 2011;17:71–78. doi: 10.1038/nm.2282. [DOI] [PubMed] [Google Scholar]
- 71.Dorn GW., 2nd Mitochondrial dynamics in heart disease. Biochim Biophys Acta. 2013;1833:233–241. doi: 10.1016/j.bbamcr.2012.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schaper J, Froede R, Hein S, Buck A, Hashizume H, Speiser B, et al. Impairment of the myocardial ultrastructure and changes of the cytoskeleton in dilated cardiomyopathy. Circulation. 1991;83:504–514. doi: 10.1161/01.cir.83.2.504. [DOI] [PubMed] [Google Scholar]
- 73.Beutner G, Sharma VK, Giovannucci DR, Yule DI, Sheu SS. Identification of a ryanodine receptor in rat heart mitochondria. J Biol Chem. 2001;276:21482–21488. doi: 10.1074/jbc.M101486200. [DOI] [PubMed] [Google Scholar]
- 74.Sabbah HN, Sharov V, Riddle JM, Kono T, Lesch M, Goldstein S. Mitochondrial abnormalities in myocardium of dogs with chronic heart failure. J Mol Cell Cardiol. 1992;24:1333–1347. doi: 10.1016/0022-2828(92)93098-5. [DOI] [PubMed] [Google Scholar]
- 75.Di Lisa F, Bernardi P. Mitochondrial function as a determinant of recovery or death in cell response to injury. Mol Cell Biochem. 1998;184:379–391. [PubMed] [Google Scholar]
- 76.Chen L, Liu T, Tran A, Lu X, Tomilov AA, Davies V, et al. OPA1 mutation and late-onset cardiomyopathy: mitochondrial dysfunction and mtDNA instability. J Am Heart Assoc. 2012;1:e003012. doi: 10.1161/JAHA.112.003012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ashrafian H, Docherty L, Leo V, Towlson C, Neilan M, Steeples V, et al. A mutation in the mitochondrial fission gene Dnm1l leads to cardiomyopathy. PLoS Genet. 2010;6:e1001000. doi: 10.1371/journal.pgen.1001000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Noble MI, Belcher PR, Drake-Holland AJ. Limitation of infarct size by trimetazidine in the rabbit. Am J Cardiol. 1995;76:41B–44B. [PubMed] [Google Scholar]
- 79.Kara AF, Demiryürek S, Celik A, Tarakçioğlu M, Demiryürek AT. Effects of trimetazidine on myocardial preconditioning in anesthetized rats. Eur J Pharmacol. 2004;503:135–145. doi: 10.1016/j.ejphar.2004.09.037. [DOI] [PubMed] [Google Scholar]
- 80.Monteiro P, Duarte AI, Gonçalves LM, Moreno A, Providência LA. Protective effect of trimetazidine on myocardial mitochondrial function in an ex-vivo model of global myocardial ischemia. Eur J Pharmacol. 2004;503:123–128. doi: 10.1016/j.ejphar.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 81.Argaud L, Gomez L, Gateau-Roesch O, Couture-Lepetit E, Loufouat J, Robert D, et al. Trimetazidine inhibits mitochondrial permeability transition pore opening and prevents lethal ischemia-reperfusion injury. J Mol Cell Cardiol. 2005;39:893–899. doi: 10.1016/j.yjmcc.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 82.Dedkova EN, Seidlmayer LK, Blatter LA. Mitochondria-mediated cardioprotection by trimetazidine in rabbit heart failure. J Mol Cell Cardiol. 2013;59:41–54. doi: 10.1016/j.yjmcc.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Aldakkak M, Camara AK, Heisner JS, Yang M, Stowe DF. Ranolazine reduces Ca2+ overload and oxidative stress and improves mitochondrial integrity to protect against ischemia reperfusion injury in isolated hearts. Pharmacol Res. 2011;64:381–392. doi: 10.1016/j.phrs.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ong SB, Hall AR, Hausenloy DJ. Mitochondrial dynamics in cardiovascular health and disease. Antioxid Redox Signal. 2013;19:400–414. doi: 10.1089/ars.2012.4777. [DOI] [PMC free article] [PubMed] [Google Scholar]