Introduction
HTLV-I infection is a worldwide health problem and approximately 15–20 million persons are estimated to be infected with this infection (1). High HTLV-I seroprevalence rates in the general population or specific groups such as blood donors, have been reported from southwest of Japan, Caribbean basin, South America, Sub-Saharan Africa, and northeastern Iran (1,2).
Although most infected people remain asymptomatic, the virus is associated with exceptionally severe diseases, such as adult T-cell leukemia/lymphoma (ATL), and HTLV-I-associated myelopathy/tropical spastic paraparesis (HAM/TSP) (3). HTLV-I infection could transmit from mother to child, predominantly through breastfeeding, via sexual intercourse, and parenteral transmission by transfusion of infected cellular blood products or sharing of needles and syringes (1,4).
Presence of HTLV-I infection was reported in 1990 among the Jews emigrated from Mashhad, northeast of Iran (5), and then some patients with ATL were indentified in Mashhad who were seropositive for HTLV-I (6). In later studies, the rate of HTLV-I infection in Mashhad was reported 3% in general population (7) and about 2% in blood donors (8) in 1996. There were some small to large scale epidemiological studies that have reported the prevalence of HTLV-I infection in blood donors from various regions of the country. The widest survey has been conducted by Rezvan et al. in 21 regional blood centres in 1996. This study reported a 0.29% rate for HTLV-I infection in total serum samples; 1.97% among Mashhadi blood donors, and zero to 0.5 percent in other centres (8). Moreover, later surveys in several regions of Iran reported different rates of the infection in blood donors. Nevertheless, there is no overall estimation of the infection in the country. This study conducted to accurately estimate the prevalence of HTLV-I infection in the Iranian blood donors through a comprehensive systematic review of literature and evidences.
Methods
Study Question
The interested outcome was the presence of HTLV-I antibody in blood samples of the Iranian blood donors, based on any blood tests or even if laboratory tests are not identified clearly, until August 2011.
Search Strategy
“HTLV” was used as a key word anywhere in the text for searching national electronic databases and websites. “HTLV” anywhere in the text (all fields), and “Iran”, “Iranian” or “Iranians” in the title, subject terms (keywords) or affiliation were also used for searching other databases.
Electronic Databases
Seventeen electronic bibliographic databases, and publishers of the health and biological sciences were searched. These included: BioMedCentral, BMJ Journals, Cochrane Library, Directory of Open Access Journals (DOAJ), Ebscohost, Emerald Journals, Google Scholar, MD Consult, OvidSP, Oxford Journals, ProQuest, PubMed, ScienceDirect, Scopus, SpringerLink Contemporary, Web of Knowledge (ISI), and Wiley InterScience Journals. Moreover, all seven Iranian databases of literatures including Iranian Research Institute for Information Science and Technology (IranDoc), Iranian Database of Medical Sciences Papers (IranMedex), Iranian Database of Publication (Magiran), Global Medical Articles Library (Medlib), National Management System for Science and Technology Information (ISNet), the Regional Information Centre for Science & Technology (RICeST), and Scientific Information Database (SID) were investigated.
Gray Literature Search
All of Iranian medical universities’ websites as well as Iranian databases such as IranDoc, ISNet, and RICeST were searched for reports of scientific congresses, research projects, and dissertations. Also libraries of faculties of medicine from Mashhad University of Medical Sciences (MUMS), and Islamic Azad University, Mashhad branch, were investigated for their thesis archives. National reports from Centre for Disease Control (CDC) of the Iranian Ministry of Health, and the Iranian Blood Transfusion Organization (IBTO) websites were also investigated. Finally, cited items of identified studies were screened.
Critical Appraisal and Selection of Studies
All titles and abstracts were screened, and relevant citations were reviewed thoroughly and checked for eligibility criteria to include the studies in the analysis. The inclusion criteria were all cross-sectional surveys that have employed appropriate sampling methods, had adequate sample size (more than 200 individuals), and provided estimation of prevalence of HTLV-I infection in blood donors using valid measurement methods in both English and Persian languages.
Data Extraction
The selected and included citations were reviewed, and the findings were extracted to a sheet. The extracted data was first author, year of the study, province/city of the study, sampling method, sample size, name of the kits and methods used for HTLV antibody detection, mean and standard deviation of subjects’ age, percentage of male subjects, and total and sex-related HTLV-I point prevalence.
Statistical Analysis
The total and sex-related point prevalence of HTLV-I infection was recalculated according to the number of infected cases, and total observations reported in each study. Binomial 95% CI was computed using EPI 6.0 software (CDC, USA). Meta-analysis method using random effect model was used based on the results of heterogeneity test (Cochrane Q) with significance set at P< 0.05.
Results
Search Result
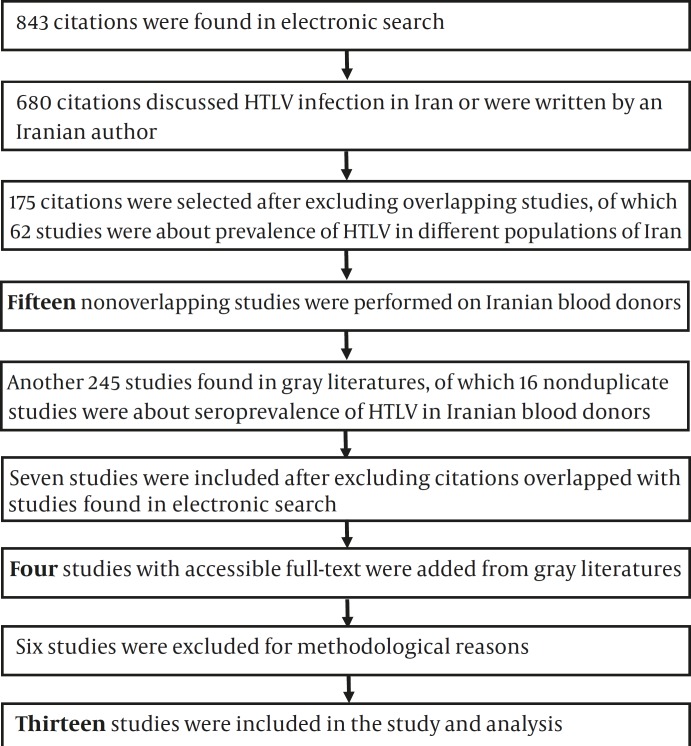
175 relevant nonduplicate citations of all 843 electronic searched citations were found, of which 17 studies discussed seroprevalence of HTLV-I in Iranian blood donors (8-24). Two studies were excluded due to overlapping samples (12,15).
In gray literature search another 245 surveys including 104 published in abstract books of congresses, 64 research reports, and 77 theses were found, of which seven nonoverlapping studies were with subjects in blood donors (25-31). Access to data of three studies was not possible in spite of requesting from related institutes (29-31). Moreover, one relevant study published in Persian found from backward citations (32) but had overlap with another English paper (8). On the other hand, no relevant data was found in searching organizations reports. After excluding studies with samples that were not representative of the target population (11,18, 24) or with inadequate samples size (13, 28) and/or studies which did not use confirmatory tests (13,16), finally 13 studies were selected. The detailed search process is demonstrated in Figure 1.
Figure 1.
Diagram of Searches and Systematic Review for Prevalence of HTLV-I Infection in Iranian Blood Donors
Studies
Thirteen relevant studies with a total of 1,091,361 subjects were found of satisfactory quality (8-10,14,17, 19-23, 25-27). All included surveys were cross sectional studies conducted on Iranian blood donors from 1996 to 2009 with sample size ranging from 960 to 243,856 (Table 1). One study had been conducted in the regional blood centres of 21cities in the country (8) and six were from Mashhad covering the years from 1997 to 2000 (9,14) and 2004 to 2009 (10,22,25,26).
Table 1.
HTLV-I Infection Prevalence Rate in Iranian Blood Donors
| Country region | Province | Time of study | Sample Size | Total prevalence; % (95% CI) | Prevalence in men; % (95% CI) | Prevalence in women; % (95% CI) |
|---|---|---|---|---|---|---|
| Total | 21 provinces from the country (8) |
1996 | 15,866 | 0.296 (0.218-0.394) |
ND | ND |
| East | South Khorasan (23)* | 2006-9 | 42,652 | 0.042 (0.025-0.067) |
ND | ND |
| Northeast | Razavi Khorasan (9) | 1999 | 28,487 | 0.769 (0.671-0.877) |
ND | ND |
| Razavi Khorasan (14) | 1997-2000 | 184,496 | 1.161 (1.113-1.211) |
ND | ND | |
| Razavi Khorasan (10) | 2004-6 | 232,648 | 0.453 (0.426-0.481) |
0.422 (0.395-0.450) |
0.762 (0.650-0.888) |
|
| Razavi Khorasan (25) | 2006-8 | 243,856 | 0.406 (0.381-0.432 0 |
0.362 (0.338-0.388) |
0.980 (0.839-1.138) |
|
| Razavi Khorasan (26) | 2006-8 | 201,719 | 0.421 (0.394-0.451) |
ND | ND | |
| Razavi Khorasan (22)* | 2008-9 | 79,687 | 0.378 (0.336-0.423) |
ND | ND | |
| Centre | Alborz (27)* | 2009 | 32,958 | 0.112 (0.79-0.155) |
0.103 (0.071-0.146) |
0.257 (0.084-0.599) |
| Northwest | West Azarbaijan (19)* | 2005-6 | 2046 | 0.342 (0.138-0.704) |
0.262 (0.085-0.610) |
1.471 (0.179-5.211) |
| West | Ilam (20)* | 2006-7 | 960 | 0.208 (0.025-0.751) |
0.122 (0-0.676) |
0.725 (0.018-3.971) |
| Southwest | Bushehr (17)* | 2002-3 | 22,740 | 0.013 (0-0.039) |
0.017 (0-0.049) |
0 (0-0.078) |
| South | Hormozgan (21)* | 2007-8 | 1100 | 0.182 (0.022-0.655) |
ND | ND |
* Included studies into meta-analysis
ND: Not Determined
The age of the subjects was only determined in five studies (9,10,19,20,27) which was between 17 and 65. Sex distribution of subjects was reported in nine studies (9,10, 17,19,20,22,23,25,27), 79 to 94 percent of the subjects were males. All studies had used ELISA tests by several HTLV detection kits (such as Biomeriux, Diapro, Genlab, MP Diagnostics, Organon, Ortho, and ZeptoMetrix) for primary screening, and western blot by some HTLV-blot kits, mainly Genlab, with or without PCR as confirmatory tests.
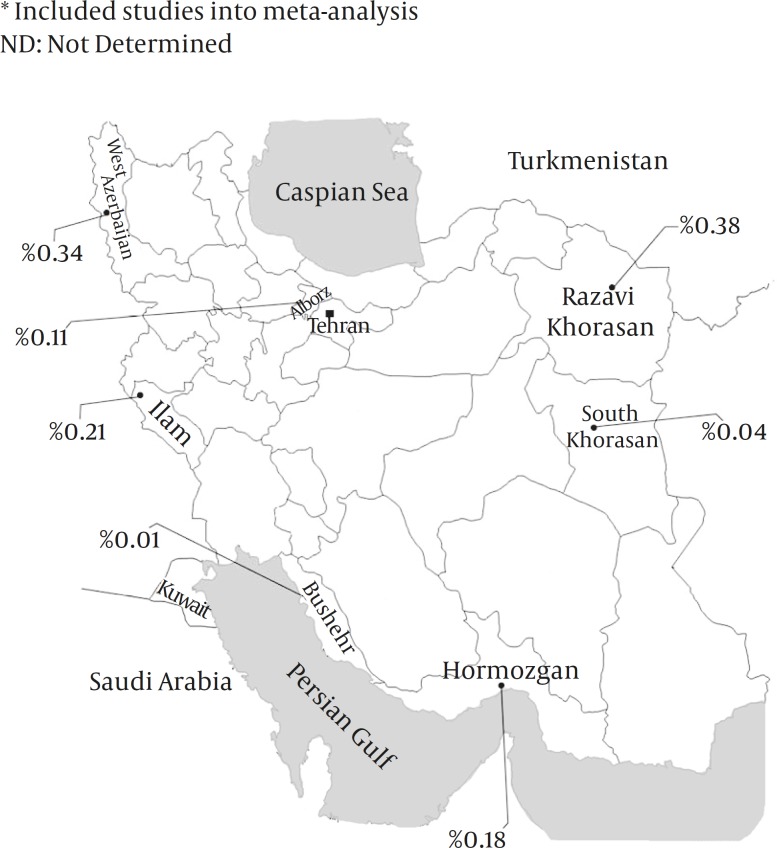
HTLV-I Infection Prevalence
Mashhad, the capital city of Razavi Khorasan province, has still remained as the most prevalent area for HTLV-I infection; however, the infection rate has fallen from 1.16% in 1997-2000 (14) to 0.38% in 2008-2009 (22).Urmia, the capital city of West Azerbaijan province, has the second place, and HTLV-I infection prevalence has reported as high as 0.34% (19). Prevalence of the infection among blood donation volunteers in Karaj, the capital city of Alborz province, and Hormozgan and Ilam provinces ranges from 0.11 to 0.21 percent (20,21,27). The lowest prevalence rates were seen in south Khorasan (0.042%) (23) and Bushehr (0.013%) (17). Prevalence of the infection according to the sex was verified or calculable only in six surveys. Except for one study (17), the infection rate in female blood donors was 2 to 6 times higher than males (Table 1).
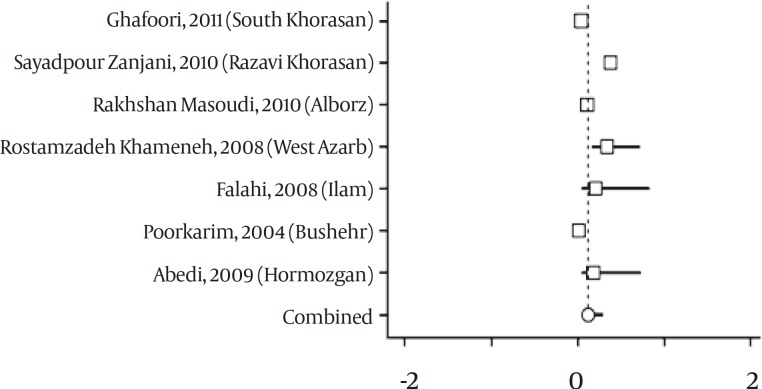
From six studies conducted in Mashhad, the latest survey included in meta-analysis (17) and a study performed in 21 provinces was excluded (8). According to data from seven studies, point estimation for HTLV prevalence in Iranian blood donors was 0.119% (95% CI: 0.050-0.287 percent). (Figures 2 & 3). By using heterogeneity test, a significant variation was found between the studies (Q= 151.13, df=6, P<0.001, I-squared= 96.03%).
Figure 2.
Forest Plot of Surveys on Prevalence of HTLV-I Infection in Iranian Blood Donors
Figure 3.
Prevalence of HTLV-I Infection Among Blood Donors in Different Provinces of Iran
Discussion
This review for estimating the overall prevalence of HTLV-I infection in Iranian blood donors indicated that distribution of HTLV-I infection in our country is not uniform, and there were significant discrepancies in different provinces regarding the infection rates. Mashhad in northeast of Iran, as previously reported (7, 8, 11), has the highest frequency of the infection. Our recent study showed that Mashhad has still remained an endemic area for HTLV-I infection with 2.12% prevalence in the general population (33). Also high prevalence of the infection in other cities of Razavi Khorasan province such as Neyshabour, and Sabzevar has been demonstrated (34, 35). Nevertheless, a declining trend in the infection prevalence among blood donors in Mashhad has been occurred. This decline could be attributed to an important strategy for donor screening. Since 1995, all donated blood samples in the blood transfusion centre of North, Razavi, and South Khorasan provinces, are routinely screened for HTLV-I (36). Similarly, a significant decline of the carrier rate among younger blood donors has been reported in Japan, due to screening blood donors for HTLV-I, and refraining from breastfeeding (37).
Dissimilar distribution of HTLV-I infection in different parts of Iran might be due to variant demographic characteristics of studied population or different applied laboratory kits. However, most blood donors (92%) in Iran are men, and according to the Iranian Blood Transfusion Organization (IBTO) criteria the age range of donors must be between 18 and 65 years (38). On the other hand, geographical clustering of the virus among neighbours has to be considered as important issue (1,3). In Turkmenistan, in proximity of Northeastern Iran, 0.2% of blood donors were HTLV-I infected (39). In contrast, the infection is probably rare in other neighboring countries of Iran. In Kuwait and Saudi Arabia, in proximity of Southwestern Iran, 0.016% and 0.046% of national blood donors showed antibodies against HTLV-I, respectively (40,41).
Also this review showed that HTLV-I infection is not probably limited to the northeast of Iran. It seems that strict screening of donated bloods should be considered in other provinces such as West Azarbaijan where evidences suggest relatively considerable rate of the infection.
Acknowledgments
This work was performed with support of the Deputy of Research, ACECR-Mashhad Branch, Mashhad, Iran. Author appreciates Dr. Ramin Sadeghi from MUMS, for his valuable consultation in meta-analysis of the findings. Also I would like to thank the personnel of libraries of faculties of medicine from MUMS as well as Islamic Azad University-Mashhad branch, for granting permission to investigate their dissertations.
References
- 1.Proietti FA, Carneiro-Proietti AB, Catalan-Soares BC, Murphy EL. Global epidemiology of HTLV-I infection and associated diseases. Oncogene. 2005;24(39):6058–68. doi: 10.1038/sj.onc.1208968. [DOI] [PubMed] [Google Scholar]
- 2.Matsuoka M, Jeang KT. Human T-cell leukemia virus type I at age 25: a progress report. Cancer Res. 2005;65(11):4467–70. doi: 10.1158/0008-5472.CAN-05-0559. [DOI] [PubMed] [Google Scholar]
- 3.Verdonck K, González E, Van Dooren S, Vandamme AM, Vanham G, Gotuzzo E. Human T-lymphotropic virus 1: recent knowledge about an ancient infection. Lancet Infect Dis. 2007;7(4):266–81. doi: 10.1016/S1473-3099(07)70081-6. [DOI] [PubMed] [Google Scholar]
- 4.Vrielink H, Reesink HW. HTLV-I/II prevalence in different geographic locations. Transfus Med Rev. 2004;18(1):46–57. doi: 10.1016/j.tmrv.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Meytes D, Schochat B, Lee H, Nadel G, Sidi Y, Cerney M, et al. Serological and molecular survey for HTLV-I infection in a high-risk Middle Eastern group. Lancet. 1990;336(8730):1533–5. doi: 10.1016/0140-6736(90)93308-c. [DOI] [PubMed] [Google Scholar]
- 6.Farid R, Shirdel A, Tabei SZ. Clinical manifestation of adult T cell lymphoma/ leukemia associated with HTLV-I in north-eastern Iran. Iranian J Med Sci. 1992;17(3):105–108. [Google Scholar]
- 7.Safai B, Huang JL, Boeri E, Farid R, Raffat J, Schutzer P, et al. Prevalence of HTLV type I infection in iran: a serological and genetic study. AIDS Res Hum Retroviruses. 1996;12(12):1185–90. doi: 10.1089/aid.1996.12.1185. [DOI] [PubMed] [Google Scholar]
- 8.Rezvan H, Ahmadi J, Farhadi M. A cluster of HTLV-I infection in northeastern of Iran. Transfusion Today. 1996;7:8–9. [Google Scholar]
- 9.Abbaszadegan MR, Gholamin M, Tabatabaee A, Farid R, Houshmand M, Abbaszadegan M. Prevalence of human T-lymphotropic virus type 1 among blood donors from Mashhad, Iran. J Clin Microbiol. 2003;41(6):2593–5. doi: 10.1128/JCM.41.6.2593-2595.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tarhini M, Kchour G, Sayadpour Zanjani D, Rafatpanah H, Otrock ZK, Bazarbachi A, Farid R. Declining tendency of human T-cell leukaemia virus type I carrier rates among blood donors in Mashhad, Iran. Pathology. 2009;41(5):498–9. doi: 10.1080/00313020903041010. [DOI] [PubMed] [Google Scholar]
- 11.11 Farid R, Etemadi M, Baradaran H, Nikbin B. Seroepidemiology and virology of HTLV-I in the city of Mashhad, northeastern Iran. Serodiagnosis and immunotherapy in infectious disease 1993. 5(4):251–2. [Google Scholar]
- 12.Farid Hosseini R, Etemadi MM, Baradaran H, Malek Nejad A, Amina H, Shahriari Z. Seroepidemiology of HTLV-I in the city of Mashhad. J Med Counc Islam Repub Iran. 1996;4(13):318–21. (Persian) [Google Scholar]
- 13.Ajami A, Hosseini RF, Tabarestani N. Seroepidemiological survey of HTLV-I/II in blood donors of Mazandaran in 1999. J Mazandaran Univ Med Sci . 2000;10(26):45–48 . (Persian) [Google Scholar]
- 14.Tavanai Sani A. Serologic Prevalence of HTLV among Blood Donors in Mashhad (Northeastern Iran) Arch Iranian Med. 2001;4(1):25–6. [Google Scholar]
- 15.Arjmandi F. HTLV-I prevalence in patients with leukemia/lymphoma and normal population. J Res Med Sci (JRMS) 2001;6(2):147–8 8 . (Persian) [Google Scholar]
- 16.Arjmandi F, Shahriari M, Sadeghi Hasanabadi A. A Comparative study of the prevalence of HTLV – I infection in Leukemia / non-Hodgkins lymphoma patients, thalassemic patients and blood donors. J Sahid Sadoughi Univ Med Sci. 2003;10(4):25–8. (Persian) [Google Scholar]
- 17.PourKarim MR, Khamisi Pour Gh, R, Zandi K, Roustaei MH. Prevalence of anti-HTLV-I & anti- HTLV-II antibodies in blood donors in Bushehr province. Iranian South Med J. 2004;6(2):161–4 . (Persian) [Google Scholar]
- 18.Karimi A, Nafici MR, Imani R. Comparison of Human T- cell Leukemia Virus Type-1 (HTLV-I) Seroprevalence in High Risk Patients (Thalassemia and Hemodialysis) and Healthy Individuals from Charmahal-Bakhtiari. Province Kuwait Med J. 2007;39(3):259–61. [Google Scholar]
- 19.Rostamzadeh Khameneh Z, Baradaran M, Sepehrvand N. Survey of the seroprovalence of HTLV I/II in hemodialysis patients and blood donors in Urmia. Saudi J Kidney Dis Transpl. 2008;19(5):838–41. [PubMed] [Google Scholar]
- 20.Falahi S, Sabahi F, Zeynali M, Kiani J, Ranjbari J. Incidince of human T-lymphotropic virus type 1 (HTLV-I) among blood donors from Ilam. Iran. Ir J Virol. 2008;1(3):11–4. [Google Scholar]
- 21.Abedi F, yavaian M, Shakibzadeh A, Khalvati B, Asadi AH. A pilot Seroepidemiologic study of HTLV in thalassemia, hemophilia, and hemodialysed patients in Hormozgan. Med J Hormozgan Univ. 2009;13(2):75–80 . (Persian) [Google Scholar]
- 22.Sayadpour Zanjani D, Shahabi M, Talaei N, Afzalaghaee M, Tehranian F, Bazargani R. Molecular analysis of human T cell lymphotropic virus type 1 and 2 (HTLV-I/2) seroindeterminate blood donors from Northeast Iran: evidence of proviral tax, env, and gag sequences. AIDS Res Hum Retroviruses. 2010;26(12):1–5. doi: 10.1089/aid.2010.0017. [DOI] [PubMed] [Google Scholar]
- 23.Ghafouri M, Ameli MR. Transfusion transmitted viral infections in blood donors of South Khorasan. Blood Quart (Sci J Iranian Blood Transfus Org) 2011;7(4):242–8 . (Persian) [Google Scholar]
- 24.Kazemi Arababadi M, Mohammadzadeh A, Pourfathollah AA, Kennedy D. Polymorphisms within Fas gene are not associated with occult hepatitis B virus infection. Hepat Mon. 2011;11(1):23–26. [PMC free article] [PubMed] [Google Scholar]
- 25.Haghighi S, Jalalian M, Bazargani R, Motamedi R. Co-infection between HTLV-I,2 and other transfusion transmissible viral infections in Mashhadi blood donors. 1st international congress on HTLV-I and associated diseases in Iran; Feb 18-20; Mashhad, Iran. 2010 . P-12. [Google Scholar]
- 26.Shahabi M, Sayadpour Zanjani D, Tehranian F. Seroindeterminate HTLV-I/II prevalence and characteristics in blood donors of Northeast of Iran. 1st international congress on HTLV-I and associated diseases in Iran; Feb 18-20; Mashhad, Iran. 2010 . p. O-26. [Google Scholar]
- 27.Rakhshan Masoudi Z, Yazdanparast E, Omidkhoda A, Zarei N, Firoozbakhat S, Zarei M. Frequency of human T-lymphotropic virus type 1,2 among Blood Donors from Karaj transfusion centre. 1st international congress on HTLV-I and associated diseases in Iran; Feb 18-20; Mashhad,Iran,. 2010. p. P-30. [Google Scholar]
- 28.Mortezaee Z. Serologic frequency of HTLV-I and HTLV-II among blood donors and its relation with blood cells changes. University of Esfahan, Faculty of Sciences: 2007. [Google Scholar]
- 29.Talebian A, Amini kafiabad S. Prevalence of Anti-HTLV-I/II among blood donors in blood transfusion centres of 27 provinces of Iran. Research project. Iranian Blood Transfusion Organization; 2006. [Google Scholar]
- 30.Morshedi B. Investigation of HTLV-I among blood donors in Isfahan Blood Transfusion Organization. Research project. Isfahan University of Medical Sciences; 1996-1997. [Google Scholar]
- 31.Prevalence of HTLV-I/2 infections among blood donors in Ahvaz Blood Transfusion Organization, 1998. Research project. Ahvaz University of Medical Sciences; [Google Scholar]
- 32.Rezvan H, Farhadi M, Ahmadi J, Tarvian S. Preliminary survey of frequency of HTLV-I/II among blood donors in Iran. Blood J (Sci J Iranian Blood Transfus Org) 1995;2(1):23–8. (Persian) [Google Scholar]
- 33.Rafatpanah R, Hedayati-Moghaddam MR, Fathimoghadam F, Bidkhori HR, Shamsian SKh, Ahmadi S, et al. High prevalence of HTLV-I infection in Mashhad, Northeast Iran: A population-based seroepidemiology survey. J Clin Virol. 2011;52(3):172–6. doi: 10.1016/j.jcv.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Hedayati-Moghaddam MR, Fathimoghadam F, Eftekharzadeh Mashhadi I, Soghandi L, Bidkhori HR. Epidemiology of HTLV-I in Neyshabour, Northeast of Iran. Iran Red Cresc Med J. 2011;13(6):424–7. [PMC free article] [PubMed] [Google Scholar]
- 35.Azarpazhooh MR, Hasanpour K, Ghanbari M, Rezaee SAR, Mashkani B, Hedayati-Moghaddam MR, et al. Human t-lymphotropic virus type 1 prevalence in northeastern iran, sabzevar: An epidemiologic-based study and phylogenetic analysis. AIDS Res Hum Retroviruses. 2012;28(9):895–901. doi: 10.1089/AID.2011.0248. [DOI] [PubMed] [Google Scholar]
- 36.Rezvan H, Abolghassemi H, Kafiabad SA. Transfusion-transmitted infections among multitransfused patients in Iran: a review. Transfus Med. 2007;17(6):425–33. doi: 10.1111/j.1365-3148.2007.00794.x. [DOI] [PubMed] [Google Scholar]
- 37.Oguma S, Imamura Y, Kusumoto Y, Nishimura Y, Yamaguchi K, Takatsuki K, et al. Accelerated declining tendency of human T-cell leukemia virus type I carrier rates among younger blood donors in Kumamoto, Japan. Cancer Res. 1992;52:2620–3. [PubMed] [Google Scholar]
- 38.Abolghasemi H, Maghsudlu M, Amini Kafi-Abad S, Cheraghali A. Introduction to Iranian Blood Transfusion Organization and Blood Safety in Iran. Iranian J Publ Health. 2009;38(Suppl 1):82–7. [Google Scholar]
- 39.Senyuta N, Syrtsev A, Yamashita M, Stepina V, Susova O, Scherbak L, et al. Sero-epidemiologic and phylogenetic studies of HTLV-I infection in 2 countries of the Caspian Sea region. Int J Cancer. 1998;77:488–93. doi: 10.1002/(sici)1097-0215(19980812)77:4<488::aid-ijc2>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 40.Al-Mufti S, Voevodin A, Ahmed S, Al Hamdan S, Al-Basheer AA. Seroprevalence of Human T-Cell Leukemia/Lymphoma Virus Type I and Type II (HTLV-I/HTLV-II) Infection among Volunteer Blood Donors in Kuwait. Med Principles Pract. 1999;8:45–50. [Google Scholar]
- 41.Fawaz NA, Tamim H, Almawi WY. Low prevalence of antibodies to human T-lymphotropic virus-I/II among blood donors in eastern Saudi Arabia. Am J Infect Control. 2005;33(3):189–91. doi: 10.1016/j.ajic.2004.08.006. [DOI] [PubMed] [Google Scholar]