Abstract
Objective
To examine the effectiveness of a primary care-based obesity intervention over the first year (6 intervention contacts) of a planned 2 year study.
Design
Cluster-randomized controlled trial.
Setting
10 pediatric practices; 5 Intervention and 5 Usual Care.
Participants
475 children ages 2 – 6 years with body mass index (BMI) ≥ 95th percentile or 85th- < 95th percentile if at least one parent was overweight; 445 (93%) had 1 year outcomes.
Intervention
Intervention practices received primary care restructuring, and families received motivational interviewing by clinicians and educational modules targeting TV, fast food, and sugar sweetened beverages.
Outcome Measures
Change in BMI and obesity-related behaviors from baseline to 1 year.
Results
Compared with usual care, intervention participants had a smaller, non-significant increase in BMI (−0.21 kg/m2; 95% CI: −0.50, 0.07; p=0.15), greater decreases in TV viewing (−0.36 hours/day; 95% CI: −0.64, −0.09; p=0.01) and had slightly greater decreases in fast food (−0.16 servings/week; 95% CI: −0.33, 0.01; p=0.07) and sugar sweetened beverages (−0.22 servings/day; 95% CI: −0.52, 0.08; p=0.15). In post-hoc analyses, we observed significant effects on BMI among females (−0.38 kg/m2; 95% CI: −0.73, −0.03; p=0.03) but not males (0.04 kg/m2; 95% CI: −0.55, 0.63; p=0.89) and among participants in households with annual incomes $50,000 or less (−0.93 kg/m2; 95% CI: −1.60, −0.25; p=0.01) but not in higher income households (0.02 kg/m2; 95% CI: −0.30, 0.33; p=0.92).
Conclusions
After 1 year, the High Five for Kids intervention was effective in reducing TV viewing but did not significantly reduce BMI.
INTRODUCTION
In the U.S., approximately 21.2% of children ages 2 – 5 years are overweight (age- and sex-specific BMI 85th to 94th percentile) and 10.4% are obese (BMI ≥ 95th percentile).1 Preschool age children who are overweight, especially those with overweight parents, tend themselves to become obese as adults 2 and are at high risk of short- 3 and long-term adverse outcomes. 4–8 The pediatric primary care team is well positioned to provide effective interventions to promote healthful behaviors among families of young children. Well child visits occur at least annually from ages 2 through 6 years and additional problem-oriented visits provide other opportunities to develop a relationship with the child and family. The continuity of the relationship between pediatricians and families, embodied in the concept of the “medical home,”9 promotes receptivity to suggestions for changes in health related behaviors.10
Few interventions to prevent childhood obesity have been conducted in the primary care setting. 11–23 Only one primary care-based randomized controlled trial (RCT) 23 and two, non-randomized trials have focused on children < 6 years.19, 20 In the Live, Eat, and Play (LEAP) RCT of 2112 children ages 5 to 9 years in Australia,23 consultations with general practitioners on obesity-related behaviors did not result in significant BMI reduction at 9 or 15 months post enrollment. In a non-randomized study of 1128 children ages 3 to 6 years who attended primary care clinics in Singapore, Ray et al.19 found that nurse-led counseling sessions were effective in reducing obesity prevalence. In another non-randomized trial conducted within US-based primary care pediatric offices, motivational interviewing by pediatricians and dietitians was effective in reducing BMI percentile among 91 overweight children ages 3 to 7 years.20 Although each of these studies showed the feasibility and, in some, the effectiveness of primary care-based interventions for obesity management, none of these trials involved the entire primary health care team; two were further limited by their non-randomized design; and the one US-based study had a small sample size.
The purpose of this study was to assess the extent to which a primary care-based intervention, compared with the usual care control condition, resulted in a smaller increase in BMI and improvement in obesity-related behaviors among children age 2 through 6 years at elevated risk of obesity.
METHODS
Study Design, Setting, and Randomization
High Five for Kids is a cluster-randomized controlled trial in 10 primary care pediatric offices of Harvard Vanguard Medical Associates (HVMA), a multi-site group practice in Massachusetts. The intervention duration is 2 years and includes an intensive 1-year intervention period followed by a less intensive maintenance period. This paper reports the results after the first year of intervention. To pair practices in preparation for blocked, or stratified, randomization, we first divided the practices into the biggest 4 and smallest 6, then matched within those groups as closely as possible on racial/ethnic composition. Within each of five pairs, a computerized routine randomly allocated one practice to the intervention group and one to the usual care control group.
Participants
Participants comprised children ages 2.0 – 6.9 years whose BMI was ≥ 95th percentile or whose BMI was 85th–<95th percentile if at least one parent was overweight (BMI ≥ 25 kg/m2) and who received their pediatric care at HVMA between August 2006 and October 2008. We excluded 1) children whose parent or guardian could not respond to interviews in English or Spanish, 2) children whose families were planning to leave HVMA, 3) families for whom the primary care clinician thought the intervention was not appropriate, and 4) children with chronic medical conditions.
Using the electronic medical records, we identified 3253 children who had a BMI ≥ 85th percentile sometime within the year prior to their index well child care visit. After each pediatric provider offered medical clearance, and approximately 1 month prior to the child’s scheduled well child care visit, we mailed a letter to each parent introducing the study. The letter included an opt-out telephone number to call if the family did not want to participate. We telephoned those individuals who did not opt-out within 7 days after mailing the letter. During the telephone call, research staff conducted a baseline interview and mailed a written informed consent to parents. Research assistants assessed parental BMI by interview. Participants were enrolled once we confirmed their BMI at the scheduled well child care visit and we received written informed consent.
At 1 year, participants completed a telephone interview with research staff and had their heights and weights measured as part of their annual well child care visit. We offered all participants $20 for completing each telephone interview. We also reimbursed intervention participants for the co-pay incurred at each visit with the nurse practitioners. All study procedures were approved by the human subjects committee of Harvard Pilgrim Health Care.
Treatment Groups
Usual Care
Participants randomized to usual care received the current standard of care offered by their pediatric practice. This included well child care visits and follow up appointments for weight checks with their pediatrician or a subspecialist (e.g. nutritionist). Visits for families in the usual care group included the baseline and annual well child care visits.
Intervention
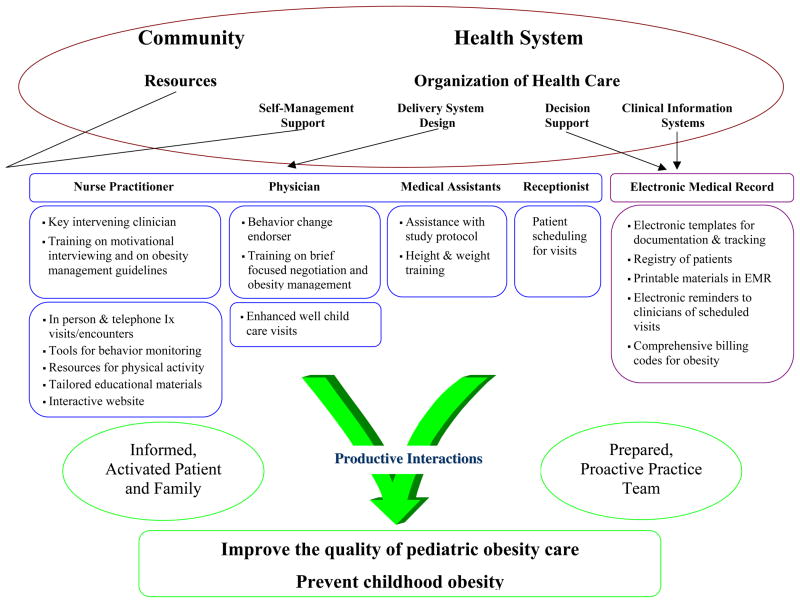
The overarching model for this intervention was the Chronic Care Model 24 which posits that changes in primary care to produce functional patient outcomes require changes for all members of the practice team (Figure 1). Major components of the intervention involved changes to the health care system. We trained all members of the practice team to play an active role in the intervention. We enhanced the electronic medical record system to assist clinicians with decision support, patient tracking, follow up, scheduling, and billing (Figure 1). After reorganization of the delivery of primary and acute care, the pediatric nurse practitioners conducted chronic disease management visits with intervention participants. Prior to the start of the intervention, we negotiated with the regional insurance companies to pay for up to four visits for both overweight and obese patients in the first year of the study.
Figure 1.
Conceptual framework, based on the Chronic Care Model, of the High Five for Kids Study
We trained the pediatric nurse practitioners to be the key intervening clinicians and to use motivational interviewing (MI) during four, 25 minute, in-person, chronic disease management visits and three, 15 minute telephone calls in the first year of the intervention. MI is a communication technique that enhances self-efficacy, increases recognition of inconsistencies between actual and desired behaviors, teaches skills for reduction of this dissonance, and enhances motivation for change.25–28 Components include de-emphasis on labeling, giving the parent responsibility for identifying which behaviors are problematic, encouraging parents to clarify and resolve ambivalence about behavior change, and setting goals to initiate the change process.25, 27, 28 We trained the primary care pediatricians in the intervention practices to use brief focused negotiation skills 29 at all routine well child care visits to endorse family behavior change. Brief focused negotiation is based on the concepts of MI but tailored for brief sessions such as the clinical encounter. To ensure accurate measurements of heights and weights, we trained all medical assistants in intervention and usual care practices on conducting research-standard anthropometric measurements. We also trained the medical receptionists to schedule initial and follow up visits with the nurse practitioners based on the study protocol.
We developed several resources to assist the physicians and nurse practitioners in supporting participants and their family in behavior change. For the patient waiting rooms, we created posters highlighting our targeted behaviors to encourage dialogue during well child care visits (Figure 2). For the chronic disease management visits with the nurse practitioners, we developed educational modules targeting TV, fast food, and sugar sweetened beverages that were matched to a family’s stage of readiness to change; 27 printed and electronic tools for self-management support, lists of local resources for physical activity; and an interactive website with educational materials, recipes, and other features. To further support behavior change, the nurse practitioners provided small incentives such as water bottles, books, and snack containers. In addition, the nurse practitioners offered interested families an electronic TV monitoring device to assist with the goal of reducing TV viewing.
Figure 2.
Participant flow for the High Five for Kids Study
Outcome Measures
Our primary outcome was change in BMI from baseline to 1 year. Medical assistants measured children’s weight, without shoes, using an electronic, calibrated Seca scale and height using a stadiometer. We calculated BMI and age- and sex-specific BMI z-scores and percentiles.30
The behavioral goals for children in the intervention were less than 1 hour/day of TV + video viewing, removing the TV from or avoiding putting a TV in the room where the child sleeps, less than or equal to 1 serving/week of fast food, and less than or equal to 1 serving/day of sugar sweetened beverages. To assess average daily TV + video viewing, we used previously validated questions. 31 We also asked if the child had a TV in the room where he or she sleeps. We measured daily sugar sweetened beverage intake using questions from a validated semi-quantitative child food frequency questionnaire 32 and we measured fast food intake using a single question shown to be associated with BMI in an adolescent cohort. 33 We also measured child’s daily fruit and vegetable intake,34 and outdoor physical activity time.35 During interviews with research staff, the parent who brought the child to their well child care visit reported their height and weight range from which we estimated their BMI. Research assistants asked the parent to report the height and weight of the child’s other parent. Parents also reported their educational attainment, marital status, annual household income, and their child’s race/ethnicity.
We culled data from the electronic medical record on completed visits and telephone calls. To assess parents’ acceptance of and satisfaction with the intervention components, we asked parents in the intervention group during the 1 year interview to rate how satisfied they were with the program. We also asked parents if they would recommend the program to their family or friends, and whether they had chosen to work on specific behaviors.
Data Analysis
We first examined baseline distributions of child and parent characteristics by intervention status. In intent-to-treat analyses, we used crude and adjusted multivariate regression models, corrected for clustering by practice, to examine differences from baseline to 1 year between the intervention and usual care groups. For continuous outcomes we used linear regression models and for dichotomous outcomes we used logistic regression models. For all models, to account for intraclass correlation, we performed generalized linear mixed models that accounted for clustering by practices (PROC GLIMMIX in SAS version 9.2; Cary, NC).
RESULTS
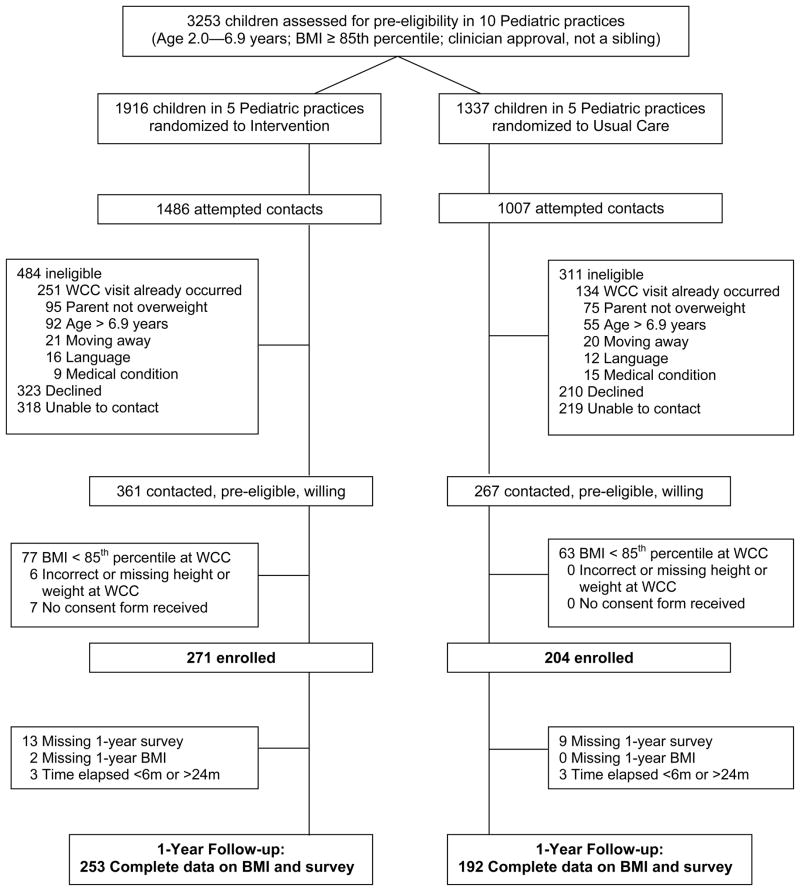
Figure 3 shows the participant flow in the High Five for Kids study. We enrolled 271 children in the intervention group and 204 in usual care. 253 participants in the intervention group (93% of those enrolled) and 192 participants in usual care (94% of those enrolled) completed a 1-year telephone interview and well child care visit for BMI measurement. Table 1 shows characteristics of our study sample, overall and by intervention assignment. At baseline, mean (SD) BMI was 19.2 (2.6) among intervention children and 19.1 (2.0) among usual care children and BMI z-scores were 1.88 (0.69) and 1.82 (0.56), respectively. 53% of intervention children had a BMI ≥ 95th percentile v. 60% of usual care children. Children randomized to the intervention group were more likely to be racial/ethnic minorities, have an obese parent, and live in lower income households (Table 1). There were no group differences at baseline in health behaviors (Table 1).
Figure 3.
High Five for Kids poster for pediatric primary care waiting rooms
Table 1.
Baseline Characteristics and Behaviors of Participants in the High Five for Kids Study, Overall and by Intervention Assignment
| Child Characteristics | Overall (N=445) | Intervention (N=253) | Usual Care (N=192) |
|---|---|---|---|
|
| |||
| Mean (SD) or N (%) | |||
| Age, years (SD) | 4.9 (1.2) | 4.8 (1.2) | 5.2 (1.1) |
| Gender | |||
| Female | 215 (48%) | 121 (48%) | 94 (49%) |
| Male | 230 (52%) | 132 (52%) | 98 (51%) |
| Race/Ethnicity | |||
| White | 252 (57%) | 118 (47%) | 134 (70%) |
| Black | 84 (19%) | 70 (28%) | 14 (7%) |
| Latino | 74 (17%) | 48 (19%) | 26 (14%) |
| Other | 35 (8%) | 17 (7%) | 18 (9%) |
| Body mass index, kg/m2 (SD) | 19.2 (2.4) | 19.2 (2.6) | 19.1 (2.0) |
| Body mass index, z-score (SD) | 1.85 (0.63) | 1.88 (0.69) | 1.82 (0.56) |
| Body mass index category | |||
| 85th to 94th percentile | 195 (44%) | 118 (47%) | 77 (40%) |
| ≥ 95th percentile | 250 (56%) | 135 (53%) | 115 (60%) |
| Time elapsed from baseline to follow up visit, months (SD) | 12.8 (2.2) | 12.9 (2.3) | 12.7 (2.0) |
| Child Health Behaviors | |||
| Sugar-sweetened beverage intake, svgs/day | 2.1 (1.7) | 2.3 (1.8) | 2.0 (1.5) |
| Fast food consumption, svgs/week | 1.1 (0.9) | 1.2 (0.9) | 1.1 (0.9) |
| Total TV + video viewing, hours/day | 2.6 (1.5) | 2.7 (1.6) | 2.4 (1.3) |
| TV in room where child sleeps | 158 (36%) | 100 (40%) | 58 (30%) |
| Other health behaviors | |||
| Fruit and vegetables intake, svgs/day | 2.4 (1.5) | 2.4 (1.5) | 2.4 (1.5) |
| Outdoor active playtime, hours/day | 2.0 (1.4) | 1.9 (1.5) | 2.1 (1.4) |
|
Parent and Household Characteristics
| |||
| Parent overweight/obesity status | |||
| Normal weight (BMI < 25 kg/m2) | 17 (4%) | 8 (3%) | 9 (5%) |
| Overweight (BMI 25 to < 30 kg/m2) | 189 (43%) | 90 (36%) | 99 (52%) |
| Obese (BMI ≥ 30 kg/m2) | 238 (54%) | 154 (61%) | 84 (44%) |
| Parent educational attainment | |||
| Some college or below | 171 (38%) | 106 (42%) | 65 (34%) |
| College graduate | 274 (62%) | 147 (58%) | 127 (66%) |
| Annual Household Income | |||
| $50,000 or less | 126 (29%) | 88 (36%) | 38 (20%) |
| ≥ $50,001 | 313 (71%) | 160 (64%) | 153 (80%) |
| Marital Status | |||
| Married | 338 (76%) | 187 (75%) | 151 (79%) |
| Not married | 107 (24%) | 66 (26%) | 41 (21%) |
Table 2 shows participants’ BMI at baseline and at 1 year by intervention assignment. At 1 year, BMI had increased by a mean of 0.31 kg/m2 in the intervention group and 0.49 kg/m2 in the usual care group, yielding a crude difference of −0.19. After multivariable adjustment, compared with usual care, intervention participants had a smaller, non-significant increase in mean BMI from baseline to 1 year than usual care participants (−0.21 kg/m2; 95% CI: −0.50, 0.07; p=0.15). We observed similar results using change in age- and sex-specific BMI z-score as the outcome (−0.05 units; 95% CI: −0.14, 0.04; p=0.28). In post-hoc stratified analyses, we observed statistically significant intervention effects on BMI among females (−0.38 kg/m2; 95% CI: −0.73, −0.03; p=0.03) but not males (0.04 kg/m2; 95% CI: −0.55, 0.63; p=0.89) and among participants in households with annual incomes $50,000 or less (−0.93 kg/m2; 95% CI: −1.60, −0.25; p=0.01) but not in higher income households (0.02 kg/m2; 95% CI: −0.30, 0.33; p=0.92).
Table 2.
Change in Body Mass Index from Baseline to 1 Year, by Intervention Assignment and within Subgroup.
| Outcome | Baseline | 1-Year | Change | Crude difference‡ | Adjusted difference* | P-value |
|---|---|---|---|---|---|---|
| N (%) or Mean (SE) | β (95% CI) | |||||
| BMI, kg/m2 | ||||||
| Intervention | 19.2 (0.2) | 19.5 (0.2) | 0.31 (0.09) | −0.19 (−0.50, 0.12) | −0.21 (−0.50, 0.07) | 0.15 |
| Usual Care | 19.1 (0.1) | 19.6 (0.2) | 0.49 (0.10) | |||
| BMI Outcome by Subgroup: | ||||||
| Child Age at baseline: | ||||||
| < 60 months | ||||||
| Intervention | 19.0 (0.2) | 19.0 (0.3) | 0.01 (0.13) | −0.20 (−0.64, 0.24) | −0.29 (−0.75, 0.17) | 0.22 |
| Usual Care | 18.9 (0.2) | 19.1 (0.3) | 0.22 (0.18) | |||
| ≥ 60 months | ||||||
| Intervention | 19.4 (0.2) | 20.0 (0.3) | 0.58 (0.12) | −0.05 (−0.38, 0.28) | −0.13 (−0.48, 0.22) | 0.46 |
| Usual Care | 19.3 (0.2) | 19.9 (0.2) | 0.63 (0.12) | |||
| Child Gender: | ||||||
| Female | ||||||
| Intervention | 19.2 (0.2) | 19.5 (0.3) | 0.30 (0.12) | −0.33 (−0.69, 0.03) | −0.38 (−0.73, −0.03) | 0.03 |
| Usual Care | 19.3 (0.2) | 19.9 (0.3) | 0.63 (0.14) | |||
| Male | ||||||
| Intervention | 19.2 (0.2) | 19.5 (0.3) | 0.33 (0.14) | −0.03 (−0.61, 0.55) | 0.04 (−0.55, 0.63) | 0.89 |
| Usual Care | 19.0 (0.2) | 19.4 (0.3) | 0.36 (0.14) | |||
| Child Race/Ethnicity: | ||||||
| White | ||||||
| Intervention | 19.0 (0.2) | 19.2 (0.3) | 0.18 (0.12) | −0.24 (−0.59, 0.10) | −0.19 (−0.54, 0.16) | 0.30 |
| Usual Care | 18.9 (0.2) | 19.3 (0.2) | 0.42 (0.11) | |||
| Black | ||||||
| Intervention | 19.6 (0.3) | 20.1 (0.4) | 0.50 (0.19) | −0.60 (−1.60, 0.40) | −0.64 (−1.61, 0.32) | 0.20 |
| Usual Care | 19.5 (0.5) | 20.6 (0.7) | 1.08 (0.43) | |||
| Latino | ||||||
| Intervention | 19.3 (0.4) | 19.8 (0.5) | 0.46 (0.21) | 0.01 (−0.71, 0.73) | 0.09 (−0.72, 0.90) | 0.82 |
| Usual Care | 19.8 (0.5) | 20.2 (0.7) | 0.45 (0.31) | |||
| Other | ||||||
| Intervention | 18.6 (0.3) | 18.6 (0.3) | 0.03 (0.36) | −0.61 (−1.53, 0.32) | −0.48 (−1.58, 0.63) | 0.41 |
| Usual Care | 19.5 (0.5) | 20.1 (0.6) | 0.64 (0.30) | |||
| Parent education: | ||||||
| < Some college or below | ||||||
| Intervention | 19.6 (0.3) | 20.1 (0.4) | 0.49 (0.16) | −0.42 (−0.93, 0.09) | −0.36 (−0.92, 0.19) | 0.20 |
| Usual Care | 19.1 (0.2) | 20.0 (0.3) | 0.91 (0.20) | |||
| ≥ College graduate | ||||||
| Intervention | 18.9 (0.2) | 19.1 (0.2) | 0.18 (0.11) | −0.09 (−0.38, 0.20) | −0.14 (−0.44, 0.16) | 0.37 |
| Usual Care | 19.1 (0.2) | 19.4 (0.2) | 0.27 (0.10) | |||
| Household income: | ||||||
| $50,000 or less | ||||||
| Intervention | 19.6 (0.3) | 20.0 (0.4) | 0.40 (0.17) | −1.02 (−1.65, −0.38) | −0.93 (−1.60, −0.25) | 0.01 |
| Usual Care | 19.9 (0.4) | 21.3 (0.5) | 1.42 (0.29) | |||
| ≥ $50,001 | ||||||
| Intervention | 19.0 (0.2) | 19.3 (0.2) | 0.27 (0.11) | −0.01 (−0.35, 0.33) | 0.02 (−0.30, 0.33) | 0.92 |
| Usual Care | 19.0 (0.2) | 19.2 (0.2) | 0.26 (0.09) | |||
| Parental overweight/obesity status at baseline: | ||||||
| BMI 25 to < 30 kg/m2 | ||||||
| Intervention | 18.9 (0.2) | 19.5 (0.4) | 0.58 (0.19) | 0.10 (−0.45, 0.65) | −0.04 (−0.66, 0.58) | 0.89 |
| Usual Care | 18.8 (0.2) | 19.3 (0.3) | 0.48 (0.18) | |||
| BMI ≥ 30 kg/m2 | ||||||
| Intervention | 19.9 (0.3) | 20.2 (0.4) | 0.27 (0.17) | −0.57 (−1.13, 0.00) | −0.29 (−0.90, 0.31) | 0.34 |
| Usual Care | 19.9 (0.4) | 20.1 (0.5) | 0.84 (0.19) | |||
Corrected for clustering within practice.
Adjusted for child age, gender, and race/ethnicity; parent education and overweight/obesity status at baseline; household income; and time elapsed from baseline to follow up visit.
Table 3 shows baseline and 1 year levels of our behavioral outcomes. In adjusted models, intervention participants decreased their TV + video viewing more than usual care participants (−0.36 hrs/day; 95% CI: −0.64, −0.09; p=0.01). We also observed greater decreases in fast food intake (−0.16 servings/week; 95% CI: −0.33, 0.01; p=0.07) and sugar sweetened beverage intake (−0.22 servings/day; 95% CI: −0.52, 0.08; p=0.15), though the confidence intervals for these effects did not exclude a null effect. For the dichotomous outcome of TV in the room where the child sleeps, we did not observe an intervention effect (Table 3).
Table 3.
Change in Health Behaviors from Baseline to 1 Year, by Intervention Assignment.
| Behavioral Outcomes | Baseline | 1-Year | Change | Crude difference‡ | Adjusted difference* | P-value |
|---|---|---|---|---|---|---|
| N (%) or Mean (SE) | β (95% CI) | |||||
| Sugar-sweetened beverages, svgs/d | ||||||
| Intervention | 2.25 (0.11) | 1.66 (0.08) | −0.59 (0.10) | −0.26 (−0.54, 0.01) | −0.22 (−0.52, 0.08) | 0.15 |
| Usual Care | 1.95 (0.11) | 1.63 (0.09) | −0.33 (0.06) | |||
| Fast food consumption, svgs/week | ||||||
| Intervention | 1.16 (0.06) | 0.94 (0.05) | −0.22 (0.05) | −0.20 (−0.37, −0.02) | −0.16 (−0.33, 0.01) | 0.07 |
| Usual Care | 1.13 (0.06) | 1.11 (0.06) | −0.02 (0.06) | |||
| Total TV + video viewing, hrs/d | ||||||
| Intervention | 2.67 (0.10) | 2.13 (0.07) | −0.53 (0.09) | −0.45 (−0.71, −0.20) | −0.36 (−0.64, −0.09) | 0.01 |
| Usual Care | 2.44 (0.10) | 2.36 (0.09) | −0.07 (0.09) | |||
| TV in bedroom, %† | N (%) or Mean (SE) | OR (95% CI) | ||||
| Intervention | 100 (40%) | 75 (30%) | −25 (10%) | 0.71 (0.37, 1.33) | 0.65 (0.32, 1.32) | 0.23 |
| Usual Care | 58 (30%) | 49 (26%) | −9 (5%) | |||
| Other Behavioral Outcomes | N (%) or Mean (SE) | β (95% CI) | ||||
| Fruit and vegetable intake, svgs/d | ||||||
| Intervention | 2.43 (0.09) | 2.65 (0.10) | 0.22 (0.09) | 0.06 (−0.21, 0.33) | 0.12 (−0.17, 0.42) | 0.41 |
| Usual Care | 2.39 (0.11) | 2.55 (0.11) | 0.16 (0.11) | |||
| Outdoor active playtime, hours/d | ||||||
| Intervention | 1.88 (0.09) | 1.94 (0.09) | 0.06 (0.10) | −0.13 (−0.44, 0.18) | −0.24 (−0.57, 0.09) | 0.16 |
| Usual Care | 2.08 (0.10) | 2.28 (0.12) | 0.20 (0.13) | |||
Corrected for clustering within practice.
Adjusted for child age, gender, and race/ethnicity; parent education and overweight/obesity status at baseline; household income; and exact time elapsed from baseline to follow up visit.
Additionally adjusted for having a TV in the bedroom at baseline.
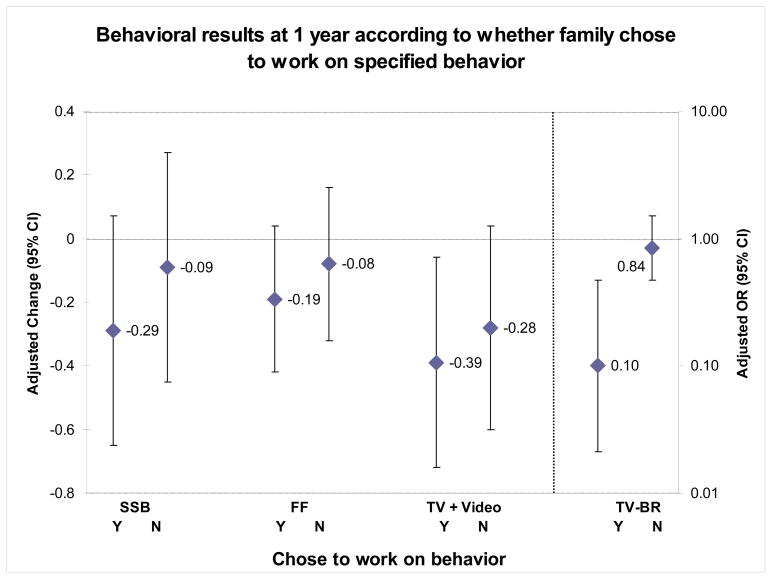
Over their multiple visits and phone calls, participating families could choose to work on one or more behavioral targets. Of the 253 participants in the intervention group, 68% chose to work on decreasing their child’s sugar sweetened beverage intake, 62% chose to work on decreasing their child’s fast food intake, 63% chose to work on decreasing their child’s TV + video viewing, but only 9% chose to work on removing the TV from or avoiding putting a TV in the room where their child sleeps. We stratified models by whether the family chose to work on the behavior or not, and used usual care as the comparison for each model. In these stratified analyses, we observed greater intervention effects among participants who chose to work on specified behaviors (Figure 4).
Figure 4.
Change in health behaviors from baseline to 1-year according to whether the family chose to work on the behavior
We aimed for intervention participants to complete 6 intervention activities with the nurse practitioner by 1-year. Among the 253 intervention participants, 141 (56%) had completed at least two of 6 activities. Compared to usual care, intervention participants who completed ≥ 2 activities by 1-year had greater decreases in TV + video viewing (−0.58 hours/day; 95% CI: −0.92, −0.24; p=0.001) and sugar sweetened beverage intake (−0.31 servings/day; 95% CI: −0.74, 0.12; p=0.15). Intervention participants with < 2 activities by 1 year had only minimal decreases in their TV + video viewing (−0.04 hours/day) and sugar sweetened beverage intake (−0.02 servings/day). There was no difference in BMI or fast food intake change based on adherence to the intervention protocol.
Based on follow up questions of the 253 intervention participants, 97% reported being “somewhat” or “very satisfied” with the High Five for Kids program and 91% reported they would recommend the program to their family and friends.
DISCUSSION
In this 1-year follow up of a primary care-based, cluster-randomized controlled trial we found that a multi-component obesity intervention based on the Chronic Care Model improved TV + video viewing particularly among families who chose to work on reducing TV time and removing or avoiding a TV in the room where the child sleeps. Children in the High Five for Kids intervention group had a smaller, but non-significant, increase in BMI overall. In addition, in post-hoc analyses, the intervention significantly improved BMI among females and those living in lower income households.
To our knowledge, the High Five for Kids study is the first randomized controlled trial in a primary care setting aimed at reducing obesity among preschool age children. A recent review of primary care based interventions for treating overweight and obese children and adolescents 22 identified no moderate to high intensity interventions for children < 6 years of age and only the LEAP trial 23, a low intensity intervention that involved consultations with general practitioners on nutrition, physical activity, and sedentary behavior, included children ages 5 and over. Our intervention was also innovative in that we attempted to effect sustainable changes in the health care system to prevent and manage childhood obesity. We recognized that the complexity of childhood obesity as a chronic medical problem required a new paradigm to improve obesity-related outcomes. Thus, based on the Chronic Care Model, the High Five for Kids intervention involved changes in the roles and responsibilities for the entire practice team, retraining of clinicians to support family behavior change, as well as updating clinical information systems and providing families’ links to their community for physical activity. We designed intervention components to be sustainable in a “real-world” primary care setting by training existing clinical staff to deliver the intervention. The intervention was also designed to be of moderate to high intensity requiring 6 intervention activities over a 1-year period.
In our intervention, the overall adjusted mean difference (intervention v. usual care) in BMI was −0.21 kg/m2 at 1 year. This magnitude of effect is very similar to that of the LEAP study 23 in which the adjusted mean difference in BMI was −0.20 kg/m2 (95% CI: −0.6, 0.1) at 9 months. Several factors could have contributed to the lack of a statistically significant intervention effect on BMI. First, our intervention involved only the primary care setting and not children’s communities or environment. It is possible that primary care-based interventions alone will not effect change in BMI but could complement and potentially enhance more comprehensive efforts in multiple settings. Second, adherence to intervention activities was relatively low; just over half of the participants completed at least two of the six visits/phone calls. It is possible that the intervention “dose” delivered was not sufficient in effecting changes in BMI. Third, we taught the nurse practitioners to use motivational interviewing to structure their visits and telephone calls. Parents were provided a choice of behaviors to work on in a non-prescriptive style and this could have led to parents choosing behaviors that could have had a lower impact on BMI, e.g. fruit and vegetable intake. Fourth, it is possible that BMI changes might lag behind the behavioral changes we observed in our intervention. Thus, we will evaluate the effect of the intervention after the planned 2-year intervention period.
Cross-sectional,36–38 longitudinal,39, 40 and experimental 41–43 evidence suggest that TV viewing and TVs in bedrooms are associated with obesity risk in children. Although several interventions have attempted to reduce TV viewing only 3 published studies have included children less than 6 years of age, 41, 42, 44 only two of which successfully decreased TV viewing. 41, 42 Using intervention strategies similar to Dennison et al.41 and by Epstein et al.42 we found that children in the intervention group decreased their TV + video viewing by 0.36 hours/day. The magnitude of effect was higher (−0.58 hours/day) if parents chose to work on reducing their child’s TV + video viewing. This magnitude of effect was similar to the two published interventions that included preschool age children. Our results lend support to multi-modal interventions to reduce TV viewing among young children.
We observed greater intervention effects among female participants and among those living in lower income households. It is possible that the gender differences we observed could be due to parents of girls being more attuned to issues of weight, diet, and activity and could have been more responsive to the intervention. A similar gender difference in intervention effect has been shown in other childhood obesity intervention studies. 45 Participating children living in lower income households had higher BMIs at baseline. It is possible the intervention was more effective among these children because they had more “room to move”. These findings deserve further investigation.
This intervention had several limitations. First, although we attempted to match the pediatric sites to obtain similar participant characteristics in intervention and usual care, unbalanced participant characteristics at baseline occurred. This imbalance may have also affected differences in parent obesity and household income. However, adjusted and unadjusted results were similar, suggesting that any imbalance in observed (or unobserved) characteristics did not affect inferences. Second, electronic medical records, which we used for decision support and recruiting and tracking of intervention participants, are not available in all pediatric practices. Thus, our intervention may not generalize to all pediatric settings. Third, although we used validated measures to assess our behavioral outcomes, we used parental report of behaviors rather than objective measures. Thus, it is possible that parents could exaggerate self-reported improvements in behaviors. For this reason, our primary outcome was BMI, a more objective measure. Fourth, because our intervention was not a factorial design, we are not able to specifically say which components were more effective. However, our results indicate that participants with more fidelity to protocol had greater improvement in their behaviors possibly indicating that with greater fidelity to protocol, we could have had greater magnitudes of effects.
In summary, after 1 year we found that the High Five for Kids study improved TV-viewing behaviors among preschool age children but did not have significant effects on BMI or diet-related behaviors. We plan further follow up to evaluate the intervention effects over a longer period and to examine the components of such an intervention that are maximally effective, scalable, and cost effective.
Acknowledgments
This study was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD 050966).
Footnotes
The abstract of this manuscript was published as part of the proceedings of the 2010 Pediatric Academic Societies Meeting.
Author Contributions: Elsie M. Taveras, MD, MPH, Steven L. Gortmaker, PhD, Katherine H. Hohman, MPH, Christine M. Horan, MPH, Ken P. Kleinman, ScD, Kathleen Mitchell, MD, Sarah Price, MPH, Lisa A. Prosser, PhD, Sheryl L. Rifas-Shiman, MPH, Matthew W. Gillman, MD, SM. Dr. Taveras had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Taveras EM, Gillman MW, Gortmaker SL, Prosser, LA, Kleinman K.
Acquisition of data: Taveras EM, Gillman MW, Hohman KH, Horan CM.
Analysis and interpretation of data: Taveras EM, Rifas-Shiman SL, Gillman MW, Kleinman K, Gortmaker SL, Prosser, LA, Kleinman K, Price S, Hohman KH, Horan CM.
Drafting of manuscript: Taveras EM
Critical revision of the manuscript for important intellectual content: Rifas-Shiman SL, Gillman MW, Kleinman K, Gortmaker SL, Prosser, LA, Kleinman K, Price S, Hohman KH, Horan CM.
Statistical analysis: Kleinman K, Rifas-Shiman SL.
Obtained funding: Gillman MW, Taveras EM.
Administrative, technical, or material support: Price S, Hohman KH, Horan CM.
Study supervision: Gillman MW, Taveras EM, Gortmaker SL, Prosser, LA, Kleinman K.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH., Jr Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 3.Skinner AC, Steiner MJ, Henderson FW, Perrin EM. Multiple markers of inflammation and weight status: cross-sectional analyses throughout childhood. Pediatrics. 2010;125(4):e801–809. doi: 10.1542/peds.2009-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 Pt 2):518–525. [PubMed] [Google Scholar]
- 5.Dietz WH, Jr, Gross WL, Kirkpatrick JA., Jr Blount disease (tibia vara): another skeletal disorder associated with childhood obesity. J Pediatr. 1982;101(5):735–737. doi: 10.1016/s0022-3476(82)80305-3. [DOI] [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 7.Castro-Rodriguez JA, Holberg CJ, Morgan WJ, Wright AL, Martinez FD. Increased incidence of asthmalike symptoms in girls who become overweight or obese during the school years. Am J Respir Crit Care Med. 2001;163(6):1344–1349. doi: 10.1164/ajrccm.163.6.2006140. [DOI] [PubMed] [Google Scholar]
- 8.Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136(5):664–672. doi: 10.1067/mpd.2000.105141. [DOI] [PubMed] [Google Scholar]
- 9.Medical Home Initiatives for Children with Special Needs Project Advisory Committee. The Medical Home. Pediatrics. 2002;110(1 Pt 1):184–186. [Google Scholar]
- 10.Taveras EM, Capra AM, Braveman PA, Jensvold NG, Escobar GJ, Lieu TA. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112(1 Pt 1):108–115. doi: 10.1542/peds.112.1.108. [DOI] [PubMed] [Google Scholar]
- 11.Diaz RG, Esparza-Romero J, Moya-Camarena SY, Robles-Sardin AE, Valencia ME. Lifestyle intervention in primary care settings improves obesity parameters among Mexican youth. J Am Diet Assoc. Feb;110(2):285–290. doi: 10.1016/j.jada.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 12.Siegel RM, Rich W, Joseph EC, et al. A 6-month, office-based, low-carbohydrate diet intervention in obese teens. Clin Pediatr (Phila) 2009 Sep;48(7):745–749. doi: 10.1177/0009922809332585. [DOI] [PubMed] [Google Scholar]
- 13.Ewing LJ, Cluss P, Goldstrohm S, et al. Translating an evidence-based intervention for pediatric overweight to a primary care setting. Clin Pediatr (Phila) 2009 May;48(4):397–403. doi: 10.1177/0009922808330109. [DOI] [PubMed] [Google Scholar]
- 14.Rattay KT, Ramakrishnan M, Atkinson A, Gilson M, Drayton V. Use of an Electronic Medical Record System to Support Primary Care Recommendations to Prevent, Identify and Manage Childhood Obesity. Pediatrics. 2009;123:S100–S107. doi: 10.1542/peds.2008-1755J. [DOI] [PubMed] [Google Scholar]
- 15.Kubik MY, Story M, Davey C, Dudovitz B, Zuehlke EU. Providing obesity prevention counseling to children during a primary care clinic visit: results from a pilot study. J Am Diet Assoc. 2008 Nov;108(11):1902–1906. doi: 10.1016/j.jada.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Wake M, Gold L, McCallum Z, Gerner B, Waters E. Economic evaluation of a primary care trial to reduce weight gain in overweight/obese children: the LEAP trial. Ambul Pediatr. 2008 Sep-Oct;8(5):336–341. doi: 10.1016/j.ambp.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Patrick K, Calfas KJ, Norman GJ, et al. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2006;160(2):128–136. doi: 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- 18.Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obes Res. 2002;10:22–32. doi: 10.1038/oby.2002.4. [DOI] [PubMed] [Google Scholar]
- 19.Ray R, Lim LH, Ling SL. Obesity in preschool children: an intervention programme in primary health care in Singapore. Ann Acad Med Singapore. 1994 May;23(3):335–341. [PubMed] [Google Scholar]
- 20.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch Pediatr Adolesc Med. 2007 May;161(5):495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 21.Polacsek M, Orr J, Letourneau L, et al. Impact of a Primary Care Intervention on Physician Practice and Patient and Family Behavior: Keep ME Healthy--The Maine Youth Overweight Collaborative. Pediatrics. 2009 Jun 1;123(Supplement_5):S258–266. doi: 10.1542/peds.2008-2780C. [DOI] [PubMed] [Google Scholar]
- 22.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of Weight Management Interventions in Children: A Targeted Systematic Review for the USPSTF. Pediatrics. 2010;125(2):e396–418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 23.McCallum Z, Wake M, Gerner B, et al. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int J Obes (Lond) 2007 Apr;31(4):630–636. doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- 24.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]
- 25.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001 Jan;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 26.Miller W, Rollnick S. Motivational Interviewing. 2. New York, New York: Guilford Press; 2002. [Google Scholar]
- 27.Rollnick S, Butler C. Health Behavior Change: a guide for practitioners. Edinburgh; Scottland: 1999. [Google Scholar]
- 28.Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York: 2008. [Google Scholar]
- 29.Tyler DO, Horner SD. Family-centered collaborative negotiation: a model for facilitating behavior change in primary care. J Am Acad Nurse Pract. 2008 Apr;20(4):194–203. doi: 10.1111/j.1745-7599.2007.00298.x. [DOI] [PubMed] [Google Scholar]
- 30.Tamura T, Goldenberg RL, Freeberg LE, Cliver SP, Cutter GR, Hoffman HJ. Maternal serum folate and zinc concentrations and their relationships to pregnancy outcome. Am J Clin Nutr. 1992;56:365–370. doi: 10.1093/ajcn/56.2.365. [DOI] [PubMed] [Google Scholar]
- 31.Baker PC, Keck CK, Mott FL, Quinlan SV. NLSY Child Handbook, revised edition: A guide to the 1986–90 National Longitudinal Survey of Youth Child Data. Columbus, Ohio: 1993. [Google Scholar]
- 32.Blum RE, Wei EK, Rockett HR, et al. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J. 1999;3:167–172. doi: 10.1023/a:1022350023163. [DOI] [PubMed] [Google Scholar]
- 33.Taveras EM, Berkey CS, Rifas-Shiman SL, et al. Association of Consumption of Fried Food Away From Home With Body Mass Index and Diet Quality in Older Children and Adolescents. Pediatrics. 2005 Oct 1;116(4):e518–524. doi: 10.1542/peds.2004-2732. [DOI] [PubMed] [Google Scholar]
- 34.Rifas-Shiman SL, Willett WC, Lobb R, Kotch J, Dart C, Gillman MW. PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr. 2001;2001(4):249–254. doi: 10.1079/phn200061. in press. [DOI] [PubMed] [Google Scholar]
- 35.Burdette HL, Whitaker RC, Daniels SR. Parental report of outdoor playtime as a measure of physical activity in preschool-aged children. Arch Pediatr Adolesc Med. 2004 Apr;158(4):353–357. doi: 10.1001/archpedi.158.4.353. [DOI] [PubMed] [Google Scholar]
- 36.Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the Third National Health and Nutrition Examination Survey. JAMA. 1998;279(12):938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 37.Crespo CJ, Smit E, Troiano RP, Bartlett SJ, Macera CA, Andersen RE. Television watching, energy intake, and obesity in US children: results from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med. 2001;155(3):360–365. doi: 10.1001/archpedi.155.3.360. [DOI] [PubMed] [Google Scholar]
- 38.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109(6):1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 39.Dietz WH, Jr, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985;75(5):807–812. [PubMed] [Google Scholar]
- 40.Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986–1990. Arch Pediatr Adolesc Med. 1996;150(4):356–362. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 41.Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med. 2004 Feb;158(2):170–176. doi: 10.1001/archpedi.158.2.170. [DOI] [PubMed] [Google Scholar]
- 42.Epstein LH, Roemmich JN, Robinson JL, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008 Mar;162(3):239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999 Oct 27;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 44.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005 May;146(5):618–625. doi: 10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 45.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]