Abstract
Background
Toll-like receptors (TLRs) are expressed by a variety of cells, including intestinal epithelia. However, the full spectrum of regulators modulating innate responses via TLRs has not been delineated. Tribbles (Trib) have been identified as a highly conserved family of kinase-like proteins. We sought to clarify the role of Trib2 in the TLR signaling pathway.
Materials and Methods
Trib2 mRNA and protein levels were analyzed by quantitative PCR and Western blot, respectively. Immunohistochemical staining was used to determine the expression of Trib2 in human tissue. Involvement of Trib2 in NF-κB pathways was assessed in epithelial cells by NF-κB reporter assay. Proteins that interacted with Trib2 were identified by mass spectrometry and confirmed by immunoprecipitation. The domain essential for Trib2 function was mapped using truncated constructs.
Results
Trib2 expression is decreased in active inflamed tissue from patients with inflammatory bowel disease. Trib2 is expressed in human and mouse colonic epithelium as well as immune cells, and its expression in epithelium is inducible in a ligand-dependent manner by TLR5 ligand stimulation. Trib2 inhibits TLR5-mediated activation of NF-κB downstream of TRAF6. Trib2 selectively modulates MAPK pathways p38 and JNK but not p44/p42 (ERK1/2). NF-κB2 (p100) was identified as a Trib2 binding partner in regulating the TLR5 signaling pathway that leads to inhibition of NF-κB activity. Residues 158–177 in the Trib 2 kinase-like domain are required for Trib2 function.
Conclusions
These observations indicate that Trib2 is a novel regulator in the TLR5 signaling pathway and altered expression of Trib2 may play a role in IBD.
Keywords: Tribbles 2, Toll-like receptor, IBD, nuclear factor kappa B, MAPK, mitogen activated protein kinase, NF-κB2
Introduction
Toll-like receptor (TLR) signaling pathways play key roles in both innate and adaptive immune responses to invasive microorganisms1. TLRs are expressed by a variety of cell populations including dendritic cells, macrophages, B cells, and specific subsets of T cells, as well as non-immune epithelial cells and fibroblasts2. TLRs initiate common NF-κB/AP-1 and distinct IRF3/7 pathways to coordinate innate immunity and to shape adaptive immunity against diverse pathogens3. The intestinal epithelium is one of the most active sites of immune reactivity, in constant communication with both microorganisms and nutritional byproducts in the lumen, as well as the underlying dense network of innate and adaptive immune cells. Epithelial cell-specific NF-κB activation or suppression appears to be a nodal point in the suppression and/or recruitment of immune responses in inflammatory bowel disease (IBD)4. In particular, NF-κB signaling in intestinal epithelium has been shown to be important in maintaining mucosal homeostasis and in mediating pathogen-specific responses5–6.
Although a defect in TLR signaling can render the host susceptible to various pathogens, overactivation or dysregulation of signaling can also be deleterious and has been found to contribute to sepsis, atherosclerosis, systemic lupus erythematosus, and IBD7–8. TLR signal-induced and/or TLR-associated negative regulators have evolved to help in preventing potentially harmful immune responses and in fine-tuning the immune responses. Extensive work has enabled the formulation of a map of the TLR signaling network9. However, relatively few negative regulators have been found, suggesting that there may be additional, as yet unrecognized negative regulators in TLR signaling pathways.
Tribbles (Trib) comprise a family of kinase-like proteins10 containing a single kinase-like domain. Mammals have three homologs of Trib: Trib1, Trib2, and Trib3. Although the kinase-like domain is highly conserved, it is uncertain whether the domain actually possesses catalytic activity11. Trib family members lack the protein-protein interaction domains typical of kinases and scaffold proteins. However, recent evidence indicates that at least some Trib family members modulate the activity and possibly the balance of activation between a number of key signaling pathways10. Trib1 and Trib3 play regulatory roles in the AP-1 pathway by binding to MAP kinase pathway intermediates in response to proinflammatory stimuli 12. Trib3 has been reported to be a regulator for ATF413, p65/rel A14, and Akt/PKB15. Trib1 has also been found to be a negative regulator of CCAAT/enhancer-binding protein β (C/EBPβ) expression and a modulator of C/EBPβ-dependent gene expression in TLR-mediated signaling16. In contrast, relatively little is known about the functional role of Trib2. First identified as a phosphoprotein in canine thyroid cells17, Trib2 has been shown to inactivate C/EBPα, cause acute myelogenous leukemia18, and suppress adipocyte differentiation by inhibiting AKT and C/EBPβ19. It also has been reported to act as a pro-apoptotic molecule that induces apoptosis in cells of hematopoietic origin20. We undertook this study to clarify the physiological role of human Trib2 by examining its role in modulating TLR signaling pathways.
Materials and Methods
Immunohistochemistry
Ileum and colon tissue samples were obtained from the Massachusetts General Hospital Tissue Repository and the tissue bank of the Center for the Study of Inflammatory Bowel Disease, following the guidelines set forth by the ethics committee of the Massachusetts General Hospital. Tissues were frozen into optimal cutting temperature (OCT) compound (Ames Company, Elkhart, IN) and kept at −80°C until use. Frozen sections (8μm thick) were stained using the avidin-biotin complex method. Rabbit anti-human Trib2 was used for human samples at 1:100, followed by 4plus™ HRP detection system (Biocare Medical, Concord, CA). Samples with no primary antibody served as negative control.
RNA extraction and real-time RT-PCR
Total RNA from cell lines was isolated using an RNA extraction kit (Qiagen, Valencia, CA) according to the manufacturer’s instructions. Total RNA from human IBD tissue and mouse colon (C57BL/6 at 6–8 weeks of age) was isolated using Trizol. Specific mouse primary immune cells were collected from spleen, thymus and lymph nodes of 6–8-week-old C57BL/6 mice and then separated using magnetic beads (Miltenyi Biotec, Auburn, CA). After confirming the specific immune cell subpopulation by FACS analysis, RNA was isolated by RNA extraction kit (Qiagen). For reverse transcription, 2μg of total RNA were transcribed using the iScript cDNA Synthesis Kit (Bio-Rad, Hercules, CA). Real-time RT-PCR was performed in a DNA Engine Opticon 2 (Bio-Rad) using iQ SYBR Green Supermix (Bio-Rad).
Cell Culture
HEK293 cells stably transfected with TLR2, TLR3 or TLR9 were gifts from Dr. Douglas Golenbock (University of Massachusetts Medical School, Worcester, MA). These cell lines were grown in DMEM supplemented with 10% fetal bovine serum (FBS), 10μg/ml ciprofloxacin (Sigma-Aldrich, St. Louis, MO) and 10μg/ml G418 (Invitrogen, Carlsbad, CA). HEK293 cells stably transfected with TLR5 were purchased from InvivoGen (San Diego, CA) and were grown in DMEM supplemented with 10% FBS, 100μg/ml Normocin (InvivoGen) and 10μg/ml blasticidin. Cell lines (SW480, HCT 116, HT-29, Caco-2, THP-1, Jurkat, Raji) were obtained from the American Type Culture Collection (ATCC, Manassas, VA). SW480, HCT 116 and HT-29 cells were cultured in DMEM with 10% FBS and 1% penicillin/streptomycin. Caco-2 cells were maintained in DMEM with 20% FBS and 1% penicillin/streptomycin. THP-1, Jurkat and Raji cells were grown in IMDM medium with 10% FBS and 1% penicillin/streptomycin. Cells were grown at 37°C (5% CO2) in a humidified incubator.
Reagents and antibodies
Toll-like receptor ligands, (Pam3CSK4, poly(I:C), flagellin (Salmonella Typhimurium) and CpG oligonucleotide) were purchased from InvivoGen. Polyclonal rabbit antibodies against phospho-JNK, phospho-ERK 1/2, phospho-p38, phospho-IKKα/β, phospho-p65, phospho-NF-κB2 and total JNK, ERK1/2, p38, IKKα/β and p65 were purchased from Cell Signaling Technology (Danvers, MA). Other antibodies used were mouse monoclonal antibodies to FLAG M2 (α-FLAG, Sigma), HA (Covance, Princeton, NJ), NF-κB2 (Abcam, Cambridge, UK), TRAF6 and rabbit polyclonal anti-MyD88 (Santa Cruz Biotechnology, Santa Cruz, CA). Rabbit polyclonal antibody against human Trib2 was raised against the N-terminal-68-EPLEGDHVFRAVHLH-82 peptide sequence of the molecule and affinity purified (Affinity Bioreagents, Deerfield, IL). Antibody specificity was confirmed by blocking antibody binding with the immunizing peptide (Affinity Bioreagents).
Plasmids, small interfering RNA, and transfection
HA-tagged human Trib2 expression vector pCMV-TAG-Trib2 (HA-Trib2) was generated by PCR amplification of Trib2 cDNA, digestion with Sal1 and Not1, and insertion into the multiple cloning sites of pCMV-TAG vector (Invitrogen). FLAG-tagged human Trib2 expression vector (FLAG-Trib2) was generated by a similar method and cloned into Sal1- and Not1-digested pCMV 3xFLAG vector (Clontech). MyD88 and TRAF6 plasmids were gifts from Dr. Son-Yong and FLAG-tagged NF-κB2 was kindly provided by Dr. Adrian Ting (Mount Sinai School of Medicine, New York, NY). The sequences of siRNA to Trib2 were as follows: sense 5′-UAGCGAGAUAUGGGAGAUCTT-3′, anti-sense 5′-GAUCUCCCAUAUCUCGCUATT-3′. Negative control siRNA and siTLR5 were purchased from Ambion (Austin, TX). Cells were transfected using cationic lipid (Lipofectamine 2000, Invitrogen) according to the manufacturer’s protocols.
NF-κB reporter luciferase assay
For NF-κB activity determination, cells were transfected with 20ng of pIV luciferase reporter plasmid and 0.05ng Renilla plasmid. Activity was measured using the Dual-Luciferase Reporter Assay System (Promega, Madison, WI) in a BD Monolight 3010 luminometer (BD Biosciences, San Diego, CA) in accordance with the manufacturer’s instructions and normalized to Renilla activity.
Immunoprecipitation and immunoblotting
For immunoprecipitation, cell lysates were incubated with appropriate specific antibodies for 3 hours at 4°C and subsequently mixed with antibody affinity gel (goat affinity-purified antibody to mouse IgG, ICN Pharmaceuticals) for an additional 90 min at 4°C; or cell lysates were incubated with anti-FLAG M2-agarose (Sigma, A2220) for 90 min at 4°C. Immunoprecipitates were washed 3 times with standard lysis buffer. Immunoprecipitated proteins and total cell lysates were resolved by SDS-PAGE, transferred to Immobilon-P membranes (Millipore, Bedford, MA) and immunoblotted with the indicated antibodies. Horseradish peroxidase-conjugated anti-mouse or anti-rabbit antibodies (DakoCytomation California, Carpinteria, CA) were used as secondary antibodies. Detection was performed by enhanced chemiluminescence with the Western Lightning Chemiluminescence Reagent (PerkinElmer Life Sciences, Boston, MA). Membranes were stripped and reprobed with anti-total MAPK (for MAP kinase antibodies) or anti-actin to confirm equal loading.
Generation of stable clones and mass spectrometry (MS) analysis
Trib2 was cloned into pcDNA4/TO-FLAG-Strep II. In this construct, the FLAG-Strep II TAP tag is in the N terminus and is derived from pcDNA™4/TO (Invitrogen, V1020-20). After transfecting the construct into HEK293T cells, stable clones were selected by culturing cells in the presence of Zeocin (200ng/ml). Clonal cell lines were grown to ~70 % confluence. Cells were washed with PBS and lysed at 4°C with 1 ml of ice-cold PLC lysis buffer (50 mM HEPES pH 7.5, 150 mM NaCl, 5% glycerol, 0.5% TX100, 1.5 mM MgCl2, 1 mM EGTA supplemented with 10 μg/ml leupeptin, 10 μg/ml aprotinin, 1 mM PMSF, 20 μg/ml RNase A, 1 mM DTT and 1 mM orthovanadate). Lysates were clarified by centrifugation at 100,000 × g and by passage through a 0.45 μm filter, then pre-cleared with 10% agarose beads (Sigma) for 30 minutes at 4°C. Supernatants were incubated with anti-M2 (Sigma) and 100 μl of 10% mouse agarose at 4°C for 2 hours. Agarose beads were washed three times with PLC lysis buffer and eluted by incubation with PBS containing 1 mg/ml FLAG peptide for 20 minutes at room temperature. Eluents were subjected to a second purification step using Strep II beads and eluted with elution buffer. Finally, eluents were separated by SDS-PAGE and visualized by colloidal Coomassie (Bio-Rad). Excised protein bands were sent to the Harvard Partners Center of Proteomics and Genomics (Cambridge, MA) for mass spectrometry analysis. Results from the MS/MS spectra were searched using the MASCOT program against the NCBI non-redundant database. Putative binding partners of Trib2 were further confirmed by immunoprecipitation.
Truncated Trib2 constructs
Truncated Trib2 constructs were created and designated ΔN (no N-terminal domain), ΔC (no C-terminal domain) and ΔNC (no N- and C-terminal domains; kinase-like domain only) Trib2 constructs. In addition, six constructs were made with truncations within the kinase-like domain: Mut#2 (stop at codon 145), Mut#3 (stop at codon 158), Mut#4 (stop at codon 177), Mut#5 (stop at codon 245), Mut#6 (stop at codon 270) and Mut#7 (stop at codon 300). All constructs were sequenced by Sanger sequencing and expression was confirmed by Western blot.
Statistical analysis
Statistical differences between groups were analyzed by Student’s t test. Data are expressed as mean ± standard error (SE). All experiments were repeated at least three times. A p value of 0.05 was considered to be statistically significant.
Results
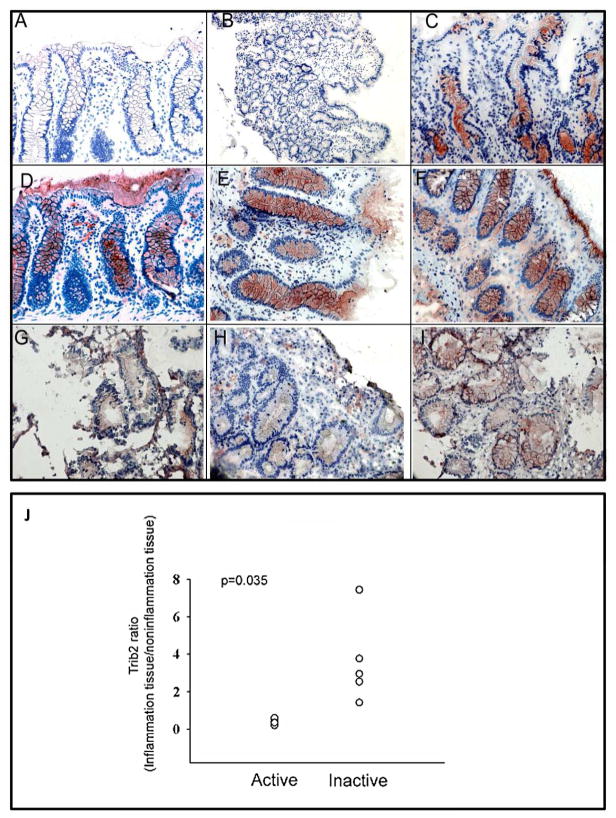
Trib2 expression is decreased in active inflammatory tissue from IBD patients
As Trib2 has been shown to be a regulator in inflammatory activation21, we first investigated the expression level of Trib2 in human chronic inflammatory bowel disease (IBD). Immunohistochemical staining was performed on colonic tissue biopsies taken from inflamed areas of colonic mucosa of IBD patients and colonic tissue from normal controls. Compared to normal tissue, Trib2 staining was less intense in the inflamed tissue from IBD patients, especially in the epithelium (Figure 1A–1I). The specificity of immunohistochemical staining by Trib2 antibody was verified by staining murine ileum with the rabbit isotype control (data not shown). The ratio of Trib2 mRNA expression in inflamed tissue compared to non-inflamed tissue decreased significantly in active IBD patients (0.41 ± 0.16, n=5; Crohn’s disease:3; Ulcerative colitis: 2) compared to inactive IBD patients (3.62 ± 2.3, n=5; Crohn’s disease:3; Ulcerative colitis: 2) (p=0.035) (Figure 1J). These observations suggest that Trib2 is expressed in human colon/intestinal epithelium and decreases during active inflammation.
Figure 1. Trib2 expression is decreased in active inflammatory bowel disease tissue.
(A–I) Immunohistochemical staining of human ileum and colon tissue for Trib2. A, negative control for staining of colon; B, negative control for staining of ileum; C, normal ileum; D–F, independent normal colons; G–I, colon biopsy specimens from active inflammatory sites of three different IBD patients. (J) Quantitative real-time PCR using paired RNA from inflammatory and non-inflammatory tissues of active (n=5) and inactive (n=5) IBD patients.
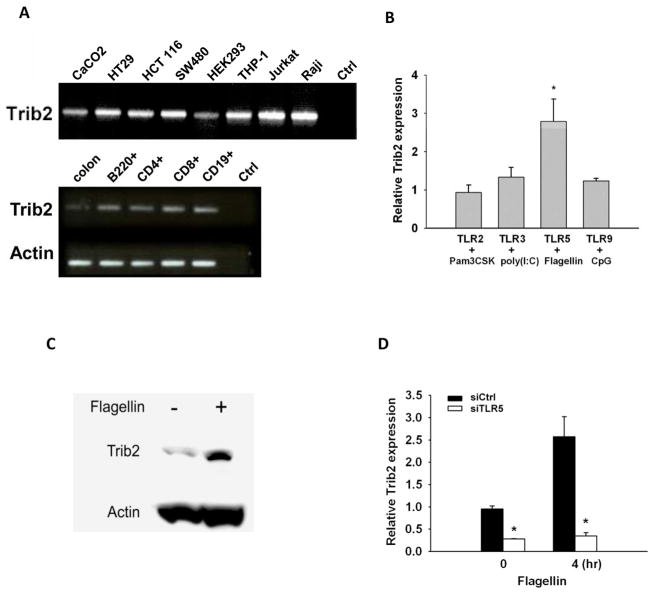
Trib2 is expressed in human and mouse colonic epithelium and immune cells
We examined the basal expression of Trib2 mRNA expression (Figure 2A, upper panel) in human colonic epithelial cell lines (Caco-2, HT29, HCT 116, and SW480), immune cell lines (THP-1, Jurkat and Raji) and HEK293 cells by RT-PCR. All cell lines examined expressed Trib2. Trib2 mRNA was also was expressed in mouse colon and immune cells (B220+, CD4+, CD8+ and CD19+ cells) (Figure 2A, lower panel).
Figure 2. Trib2 is expressed in human and mouse colorectal epithelial and immune cells and the expression is inducible by TLR5 ligand.
(A) Upper panel: RT-PCR with Trib2-specific primers using template cDNA prepared from human colonic epithelial cell lines (Caco-2, HT29, HCT 116 and SW480), HEK293, and immune cells (THP-1, Jurkat and Raji). Water (no cDNA) in the PCR reaction was used as the negative control; Lower panel: RT-PCR with Trib2-specific primers using template cDNA prepared from full thickness mouse colon, B220, CD4+, CD8+ and CD19+ cells. (B) Quantitative RT-PCR with Trib2-specific primers using template cDNA prepared from HEK293 cells stably transfected with TLR2, TLR3, TLR5 or TLR9 after Pam3CSK4 (1μg/ml), poly(I:C) (2.5μg/ml), flagellin (100ng/ml) or CpG oligonucleotide (10μg/ml) treatment for 4 hours (n≥3). Results were normalized to untreated cells (n≥3). (C) Western blots of total cell lysates from SW480 cells with and without flagellin stimulation (100ng/ml) for 6 hours. The same membranes were probed for Trib2 and actin. (D) Quantitative RT-PCR of Trib2 using RNA from HEK293 cells stably transfected with TLR5, transiently transfected with 30nM siTLR5 or control siRNA for 24 hours, then treated with flagellin (100ng/ml) for 0 or 4 hours (n≥3). * p<0.05 for all panels.
Trib2 expression in epithelium is ligand-dependent and inducible by TLR5 ligand stimulation
As shown by immunohistochemical staining, cells expressing decreased levels of Trib2 in active IBD patients were mostly epithelial. In order to further characterize the regulation of Trib2 expression in epithelial cells by TLR ligands, HEK293 cells stably transfected with TLR2, TLR3, TLR5 or TLR9 were stimulated with their respective ligands. mRNA expression of Trib2 was upregulated 3.27-fold within four hours of stimulation by the TLR5 ligand flagellin, compared to 1.12-fold by TLR2 ligand Pam3CSK4, 1.1-fold by TLR3 ligand poly(I: C), and 1.07-fold by TLR9 ligand CpG oligonucleotide (Figure 2B). Consistent with these findings, Trib2 protein expression was induced by flagellin stimulation in SW480 cells (Figure 2C).
To confirm that the TLR5-mediated Trib2 expression was ligand-dependent, a functional siRNA approach was employed. Trib2 was found to be upregulated by flagellin only when TLR5 was expressed (Figure 2D). This result suggested that the expression of Trib2 is TLR5 ligand-dependent. Accordingly, we next pursued studies of pathways regulating Trib2 following stimulation of TLR5.
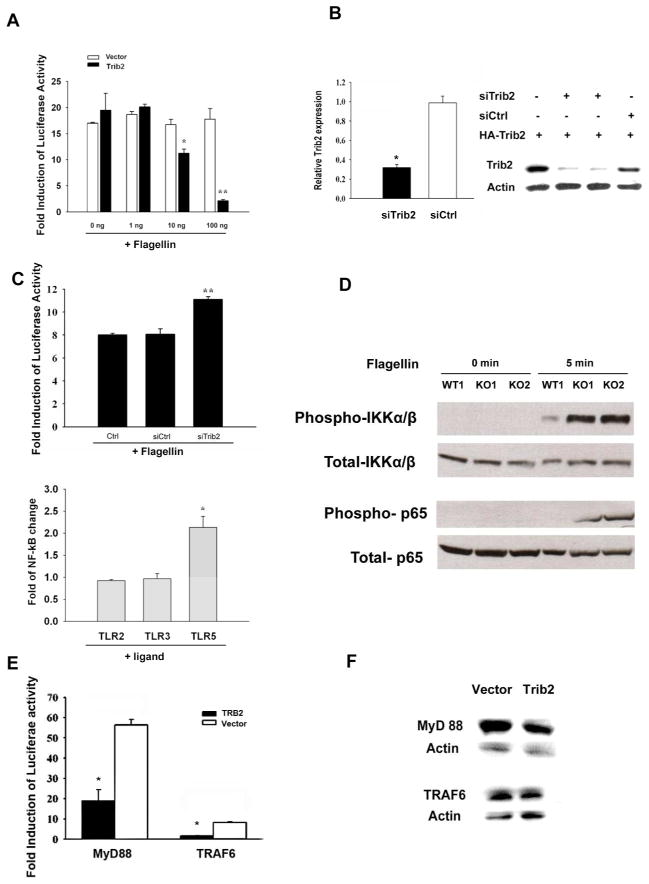
Trib2 inhibits TLR5-mediated activation of NF-κB downstream of TRAF6
After observing that Trib2 mRNA and protein levels were upregulated in response to TLR5 ligand, we next examined the effect of Trib2 on NF-κB activation. Using a NF-κB luciferase reporter assay in HEK293 cells stably transfected with TLR5, we found that overexpression of Trib2 inhibited TLR5-mediated activation of NF-κB in a concentration-dependent manner (Figure 3A). We next examined this result using a siRNA approach. The specificity of Trib2 siRNA was validated by examining both mRNA and protein levels (Figure 3B). Consistent with the results from overexpression of Trib2, NF-κB activity increased in the presence of Trib2 siRNA (Figure 3C, upper panel). To exclude off-target effects of siRNA on type I interferon expression, HEK293/TLR5 cells were transfected with siRNA for 24 hours, stimulated with flagellin, and RNA was isolated. Quantitative PCR was performed to assess the relative expression of interferon α and β. No difference was observed between control and Trib2 siRNA groups (data not shown). To confirm that the inhibition of NF-κB activity was TLR5 ligand-specific, we examined NF-κB reporter activity using HEK293 cells stably expressing TLR2, TLR3 and TLR5. These cells were transfected with siRNA and stimulated with their respective ligands. An increase of NF-κB activity was seen in the presence of Trib2 siRNA only in TLR5 cells stimulated with TLR5 ligand flagellin (Figure 3C, lower panel).
Figure 3. Trib2 inhibits TLR5-mediated activation of NF-κB downstream of the TRAF6 complex.
(A) HEK293/TLR5 cells were transfected with increasing amounts of Trib2 or empty vector and NF-κB reporter with Renilla. Cells were stimulated with flagellin (100ng/ml, 6 hours) 24 hours post-transfection and luciferase assay was performed. Results are normalized to cells transfected with NF-κB in the absence of ligand stimulation (n=4. (B) Left panel: Quantitative RT-PCR of Trib2 was performed using RNA from HEK293/TLR5 cells after transfection with 20nM of Trib2 siRNA or control siRNA for 24 hours. Results are normalized to HEK293/TLR5 without siRNA (n=3). Right panel: HA-Trib2 (100ng/ml) was co-transfected with Trib2-specific or control siRNA (100nM) in HEK293/TLR5 cells. Lysates were collected 24 hours post-transfection and assessed by Western blot. (C) Upper panel: HEK293/TLR5 cells were transfected with Trib2 siRNA or control siRNA (20nM) or transfected with NF-κB reporter and Renilla only (Ctrl). Cells were stimulated with flagellin (100ng/ml, 6 hours) 24 hours post-transfection and luciferase assay was performed (n≥4). Results were normalized to cells transfected with NF-κB in absence of ligand stimulation. Lower panel: HEK293/TLR2, HEK293/TLR3 or HEK293/TLR5 cells were transfected with Trib2 siRNA or control siRNA (20nM). Cells were treated with Pam3CSK4 (1μg/ml, 6 hours), poly(I:C) (2.5μg/ml, 6 hours) or flagellin (100ng/ml, 6 hours) 24 hours post-transfection and luciferase reporter assay was performed (n≥3). Results were normalized to cells transfected with control siRNA. (D) Macrophages from Trib2 KO and WT mice were stimulated with flagellin (100ng/ml, 0 or 5 min) and cell lysates were collected. Membranes were first hybridized with phospho-IKKα/β or phospho-p65 antibodies, then stripped and rehybridized with anti- IKKα/β or anti-p65 antibodies. (E) MyD88 (200ng/ml) or TRAF6 (200ng/ml) were co-transfected with Trib2 (100ng/ml) or empty vector (100ng/ml) and NF-κB reporter with Renilla. Luciferase assay was performed 24 hours post-transfection. Results were normalized to cells transfected with NF-κB without MyD88 or TRAF6 (n≥4). (F) Western blots of the same cell lysates used for the luciferase assay were hybridized with MyD88 and TRAF6 antibodies. Membranes were stripped and rehybridized with anti-actin as the loading control. * p<0.05; ** p<0.01 for all panels.
To further characterize Trib2 as a negative regulator in the NF-κB pathway, we next used peritoneal macrophages from Trib2 knockout mice, which were kindly provided by Dr. JY Yen from the Sinica Academica (Taipei, Taiwan). Following flagellin stimulation, we found that levels of phosphorylated IKKα/β (Figure 3D, upper panel) and p65 (Figure 3D, lower panel) were increased in macrophages from Trib2 knockout mice compared to wild-type control cells.
We next sought to determine at which point in the NF-κB pathway Trib2 was interfering with TLR5-dependent NF-κB activation. To address this question, MyD88 and TRAF6 were co-transfected with Trib2 into HEK293/TLR5 cells and NF-κB activation was assessed. The inhibitory effects of Trib2 on NF-κB could not be rescued by overexpression of MyD88 or TRAF6 (Figure 3E), indicating that Trib2 affects NF-κB signaling downstream of the TRAF6 complex. The transfection efficiency of MyD88 and TRAF6 in the Trib2- and vector-transfected groups was validated by Western blot (Figure 3F). Overexpression of Trib2 was also validated by Western blot (data not shown).
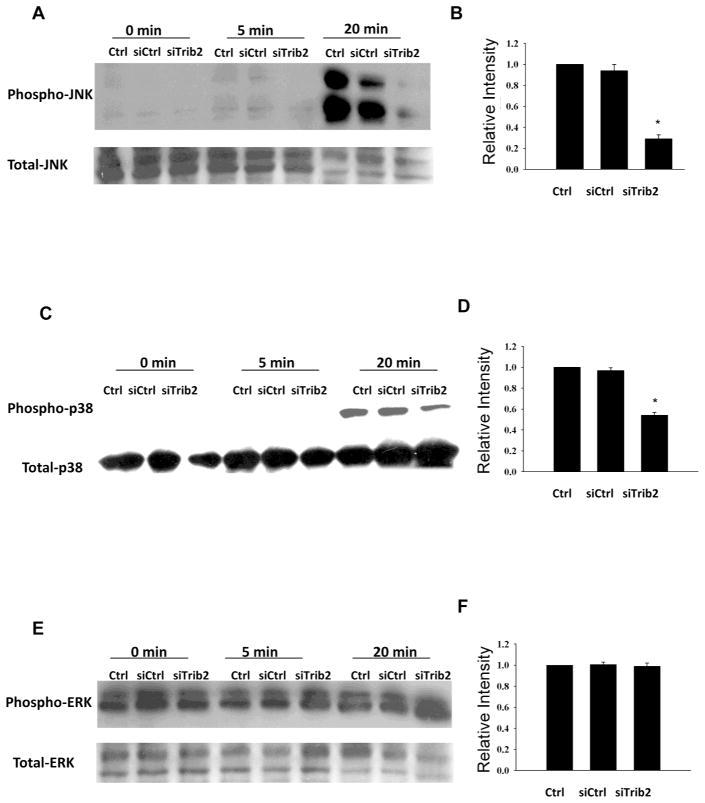
Trib2 selectively modulates p38 and JNK MAPK pathways but not p44/p42 (ERK1/2)
In addition to the NF-κB pathway, the MAP kinase pathway plays an important role in TLR signaling. To determine whether Trib2 exerts a regulatory effect on the MAP kinase pathways, we evaluated the impact of Trib2-specific siRNA on p38, p44/p42 (ERK 1/2), and JNK pathways in HEK293/TLR5 cells. Knockdown of Trib2 significantly and selectively decreased the TLR5 ligand-induced phosphorylation of JNK and p38, but had no effect on the ERK pathway (Figure 4).
Figure 4. siRNA knockdown of Trib2 expression decreases phosphorylation of p38 and JNK but not p44/p42 (ERK1/2).
HEK293/TLR5 cells were transfected with Trib2 siRNA or control siRNA, or left untransfected (Ctrl) for 24 hours. Cells were treated with flagellin (100ng/ml) for 0, 5 or 20 min. Membranes were hybridized with indicated phospho-antibodies, then stripped and rehybridized with anti-MAPK antibodies. Bands from the 20-minute flagellin treatment were quantified by densitometry. (A, B: JNK; C, D: p38; E, F: ERK). * p<0.05 for all panels.
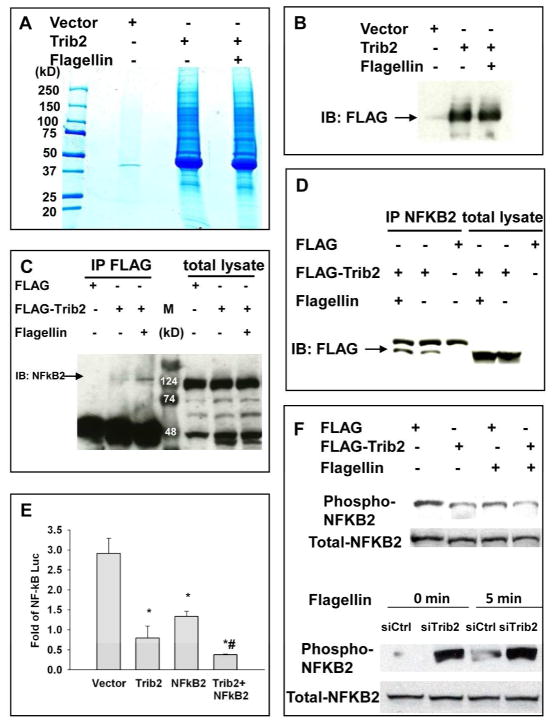
NF-κB2 (p100) interacts with Trib2
We next used a proteomics approach to identify proteins in the NF-κB pathway that physically interact with Trib2 in response to flagellin stimulation. HEK293 cells stably transfected with FLAG- and Strep II-tagged Trib2 were stimulated with flagellin. Following sequential purification with FLAG and Strep II beads, eluted proteins were separated by SDS-PAGE and visualized by colloidal Coomassie (Figure 5A) and immunoblotted with FLAG antibody (Figure 5B). Excised protein bands were sent to the Harvard Partners Center of Proteomics and Genomics for mass spectrometry (MS) analysis. Results from the MS/MS spectra were searched using MASCOT against the NCBI non-redundant database. A total of 368 proteins were found. After verifying biological information from the NCBI database, we identified NF-κB2 (p100/p52), which plays a role in NF-κB pathway, as a Trib2-interacting protein.
Figure 5. NF-κB2 (p100) is a binding partner of Trib2 in regulating the TLR5 signaling pathway that inhibits NF-κB activity.
(A–B) HEK293 cells stably transfected with Trib2 were stimulated with flagellin. Eluents from FLAG and Strep II beads were separated by SDS-PAGE and visualized by (A) colloidal Coomassie and (B) immunoblotting with FLAG antibody. (C) HEK293/TLR5 cells were transfected with FLAG-Trib2 or FLAG vector for 24 hours followed by stimulation with flagellin for 0 or 20 minutes. Lysates were immunoprecipitated with FLAG antibody and blotted for NF-κB2. (D) Same lysate as (C), immunoprecipitated with NF-κB2 antibody and blotted for FLAG. (E) MyD88 (200ng/ml) was co-transfected in HEK293/TLR5 cells with Trib2 (100ng/ml), NF-κB2 (500ng/ml) or empty vector and NF-κB reporter with Renilla. Luciferase assay was performed 24 hours post-transfection. Results were normalized to cells transfected with NF-κB but no MyD88 (n≥4). #, difference between Trib2 alone and Trib2 with NK-κB2, p<0.05. (F) Upper panel: HEK293/TLR5 cells were transfected with FLAG-Trib2 or FLAG vector for 24 hours followed by stimulation with flagellin for 0 or 5 minutes. Lower panel: HEK293/TLR5 cells were transfected with siCtrl or siTrib2 for 24 hours, followed by stimulation with flagellin for 0 or 5 minutes. Membranes were first hybridized with phospho-NF-κB2, then stripped and rehybridized with anti-NF-κB2 antibody. * p<0.05 for all panels.
We next confirmed the Trib2-NFκB2 (p100/p52) interaction using immunoprecipitation (Figure 5C–D). Using the NF-κB reporter assay, we found that co-transfection of Trib2 and NF-κB2 decreased the activity of NF-κB to a greater extent than transfection of either protein alone (Figure 5E). Phosphorylation of NF-κB2 decreased when Trib2 was overexpressed and increased when Trib2 was knocked down by siRNA (Figure 5F).
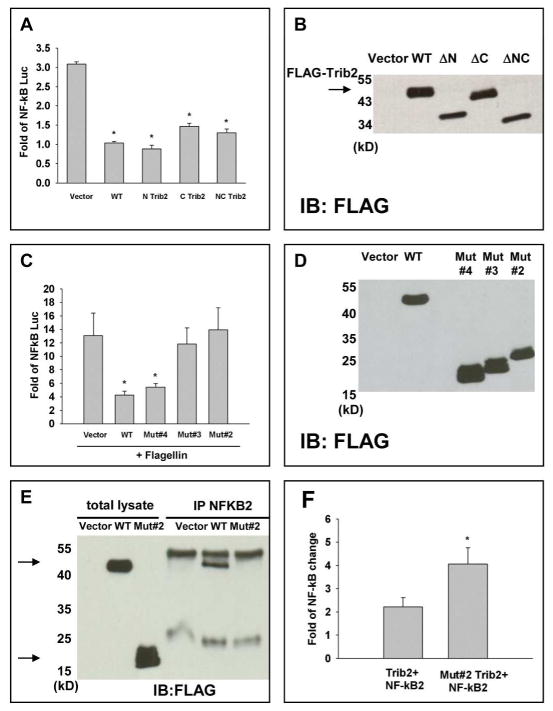
Residues 158–177 in the Trib2 kinase-like domain are essential for Trib2 function
We next sought to determine which domain of the Trib2 protein is essential to its function in the NF-κB pathway. Trib2 has three structural domains: an N-terminal domain, a C-terminal domain, and a kinase-like domain in the center. In order to identify the area essential for its function, we constructed truncated Trib2 proteins. Using the NF-κB reporter assay, we saw no significant change in the inhibition of NF-κB activity between full-length Trib2 and Trib 2 constructs ΔN (no N-terminal), ΔC (no C-terminal) or ΔNC (no N- and C-terminal domains, equivalent to the kinase-like domain only) (Figure 6A). This observation implied that the kinase-like domain was essential for Trib2 function. Protein expression of the ΔN, ΔC and ΔNC Trib2 constructs were validated by Western blot (Figure 6B).
Figure 6. The kinase-like domain of Trib2, especially residues 158–177, is the essential area for Trib2 function.
(A) HEK293/TLR5 cells were transfected with equal amounts of FLAG-Trib2, ΔN, ΔC and ΔNC truncated Trib2 constructs or empty vector along with NF-κB reporter with Renilla. Cells were stimulated with flagellin (100ng/ml, 6 hours) 24 hours post-transfection and luciferase assay was performed. Results were normalized to cells transfected with NF-κB in the absence of ligand stimulation. (B) Lysates from (A) were used for immunobloting with FLAG antibody. (C) HEK293/TLR5 cells were co-transfected with MyD88 and equal amounts of FLAG-tagged Trib2, truncated Trib2 constructs (Mut#2, Mut#3, Mut#4) or empty vector and NF-κB reporter with Renilla. NF-κB activity was assessed 24 hours post-transfection. Results were normalized to cells transfected with NF-κB in the absence of MyD88. (D) Lysates from (C) were used for immunoblotting with FLAG antibody. (E) HEK293/TLR5 cells were transfected with FLAG-Trib2, Trib 2 Mut#2, or FLAG vector. Lysates were immunoprecipitated 24 hours post-transfection using NF-κB2 antibody and immunoblotted with anti-FLAG. (F) HEK293/TLR5 cells were co-transfected with MyD88, NF-κB2 and equal amounts of FLAG-Trib2, Trib 2 Mut#2 or FLAG vector along with NF-κB reporter with Renilla. NF-κB luciferase reporter assay was performed 24 hours post-transfection. * p<0.05 for all panels.
To further define the region required for Trib2 function, we used truncated mutations of Trib2 within the kinase-like domain. When compared to full-length Trib2, the inhibition of NF-κB activity decreased in Mut#2 (stop at codon 145) and Mut#3 (stop at codon 158), but not in Mut#4 (stop at codon 177) (Figure 6C), Mut#5, Mut#6 or Mut#7 (data not shown). Expression levels of these constructs were validated by Western blot (Figure 6D). The binding of Trib2 and NF-κB2 was lost in Mut#2 (Figure 6E), and the increased inhibition of NF-κB activity in the presence of both Trib2 and NF-κB2 also lost in Mut#2 (Figure 6F). Taken together, these results suggest that the kinase-like domain, especially residues 158–177, forms the essential interaction domain for Trib2 function in regulating NF-κB activity in epithelial cells.
Discussion
Our data demonstrate that Trib2 is a negative regulator of the TLR5 ligand-dependent NF-κB activation pathway and interferes with NF-κB downstream of TRAF6. Trib2 binds to NF-κB2 to further decrease the activity of NF-κB by regulating the phosphorylation of NF-κB2, and the kinase-like domain (residues 174–180) is essential for its function. The expression of Trib2 is inducible by TLR5 ligand stimulation, a finding that is consistent with Trib2 serving a role in negative feedback regulation of TLR-dependent innate immune responses22. In addition, the expression of Trib2 in inflamed, active human IBD tissue is significantly decreased, especially in epithelial cells. This result correlates with excessively or inappropriately activated NF-κB in IBD. NF-κB activity has been observed in lamina propria mononuclear cells and in epithelial cells of the inflamed gut23–25, consistent with the notion that Trib2 is a negative regulator of NF-κB signaling.
Intestinal epithelial cells, while playing important protective and absorptive functions, also actively participate in mucosal immunity by the elaboration of cytokines and chemokines. In the present study, Trib2 was found to be more inducible by the TLR5 ligand flagellin than by the ligands for TLR2, TLR3, or TLR9. Studies of circulating antibodies in the serum of Crohn’s disease patients and in murine colitis models have identified flagellin as a dominant antigen, suggesting a role for this bacterial protein in the immunopathogenesis of IBD26. In addition, studies of flagellin/TLR5 responses in epithelia have revealed intertwined activation of inflammatory and apoptotic pathways27.
When cells are stimulated by flagellin, both NF-κB and MAPK pathways are activated. Trib1 and Trib3 have been demonstrated to play regulatory roles in the AP-1 pathway by binding to mitogen-activated protein kinase kinase (MAPKK)12. Recently, Trib2 has been shown to negatively regulate IL-8 activity by binding to MEK1 and MKK7 in monocytes21. Our results indicate that in epithelial cells, Trib2 plays a regulatory role in the JNK and p38 pathways, but not in the ERK pathway. The concentration of a specific MAPK module, along with its duration of activation, can profoundly affect the biological response of MAPK signaling activation28. Transient activation of JNK or p38 might have a protective effect on cellular responses to a stress stimulus, whereas prolonged activation of the same MAPK might lead to a commitment to apoptosis. Cheung et al. have reported that TAB1 participates in SAPK2a/p38α-mediated feedback control of TAK1, which not only limits the activation of SAPK2a/p38α but synchronizes its activity with other signaling pathways that lie downstream of TAK1 (JNK and IKK)29. Trib2 might be predicted to be a regulator at this level to fine-tune the inflammatory and cell fate responses to TLR ligand stimulation.
The tribbles family of genes encodes pseudokinase proteins that are highly conserved. Instead of direct phosphorylation of target proteins, tribbles act as adaptors in signaling pathways for important cellular function and neoplastic transformation30. In addition to the known proteins interacting with Trib2 (COP131, C/EBPα18, C/EBPβ19, MEK121, MKK712, AKT1/215), we found that Trib2 interacts with NF-κB2/p100 and plays a regulatory role for NF-κB activity in the TLR5 signaling pathway.
The mammalian NF-κB signaling system consists of five NF-κB subunits (p65 (RelA), c-Rel, RelB, p50, and p52) and five proteins with inhibitory activity (IκBα, IκBβ, IκBε, p105 (NF-κB1), and p100 (NF-κB2)). In unstimulated cells, NF-κBs are bound by inhibitor proteins (IκBs) and are rendered inactive. Many stimuli, including TLR ligands, induce phosphorylation and proteasomal degradation of IκBs, leading to the activation of NF-κB-responsive gene expression. p105 and p100 have been reported to assemble into high molecular weight complexes that contribute to the regulation of all NF-κB isoforms. These complexes trap at least 50% of cytoplasmic p50 and p52 in macrophages following lipopolysaccharide stimulation, thus participating in terminating NF-κB signaling32. NF-κB2/p100 has a role in the negative regulation of RelB-induced dendritic cell maturation, with critical consequences for the regulation of adaptive immune responses33. NF-κB2/p100 also limits nuclear translocation of NF-κB1-RelA and thereby functions as a regulatory brake for the activation of naïve T cells34. Exacerbated activation of the NF-κB2 pathway is potentially associated with a wide range of disorders such as rheumatic arthritis, ulcerative colitis, and B cell lymphomas. Therefore, inhibitors of this pathway could be valuable tools for the treatment of inflammatory disorders and cancers35–36.
Studies of Trib2 domains responsible for protein binding or functional/oncogenic activity by Keeshan et al. showed that the N terminus of Trib2 is not essential for hematopoietic cell differentiation or myeloid cell transformation. In contrast, the integrity of the kinase-like domain is required for both of these activities31. Our results also support the notion that the kinase-like domain of Trib2 is required for regulation of NF-κB activity in epithelial cells. We localized the essential area for this regulatory role within the kinase-like domain as residues 158–177. This essential area is close to and overlaps the catalytic loop (RDLKLRK, residues 174–180) in structure. Truncated Trib2 proteins lacking this sequence lost the ability to bind to NF-κB2 and lost their inhibitory effect on NF-κB activity in epithelial cells.
Taken together, we found that Trib2 is a negative regulator of the TLR5 ligand-dependent NF-κB activation pathway, acting via binding to NF-κB2 and regulating the phosphorylation of NF-κB2, with the kinase-like domain essential for this function. The expression of Trib2 in active inflamed human IBD tissue is significantly decreased especially in epithelial cells, supporting the notion that Trib2 is a negative regulator of NF-κB signaling.
Acknowledgments
Grant Support: This work was supported by NIH funds DK060049 and DK043351 (R.J.X.), the Ministry of Education of Taiwan (Taiwan Study abroad Scholarship), the National Science Council of Taiwan (NSC-095-SAF-I-564-604-TMS, NSC-98-2314-B-002-094-MY2), the National Taiwan University Hospital (NTUH-97-N1038, NTUH-98-N1197) and by the Liver Disease Prevention & Treatment Research Foundation.
We thank Dr. Emiko Mizoguchi for help with immunohistochemical staining.
Footnotes
Author contributions:
RJX and DKP conceived and designed the experiments. SCW, IMR, ZC and ASH performed the experiments. SCW, IMR and RJX analyzed the data. SCW, IMR, RJX and DKP wrote the paper.
References
- 1.Iwasaki A, Medzhitov R. Toll-like receptor control of the adaptive immune responses. Nat Immunol. 2004;5:987–95. doi: 10.1038/ni1112. [DOI] [PubMed] [Google Scholar]
- 2.Carmody RJ, Chen YH. Nuclear factor-kappaB: activation and regulation during toll-like receptor signaling. Cell Mol Immunol. 2007;4:31–41. [PubMed] [Google Scholar]
- 3.Lee MS, Kim YJ. Pattern-recognition receptor signaling initiated from extracellular, membrane, and cytoplasmic space. Mol Cells. 2007;23:1–10. [PubMed] [Google Scholar]
- 4.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–34. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 5.Nenci A, Becker C, Wullaert A, et al. Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature. 2007;446:557–61. doi: 10.1038/nature05698. [DOI] [PubMed] [Google Scholar]
- 6.Zaph C, Troy AE, Taylor BC, et al. Epithelial-cell-intrinsic IKK-beta expression regulates intestinal immune homeostasis. Nature. 2007;446:552–6. doi: 10.1038/nature05590. [DOI] [PubMed] [Google Scholar]
- 7.Liew FY, Xu D, Brint EK, et al. Negative regulation of toll-like receptor-mediated immune responses. Nat Rev Immunol. 2005;5:446–58. doi: 10.1038/nri1630. [DOI] [PubMed] [Google Scholar]
- 8.Cario E. Bacterial interactions with cells of the intestinal mucosa: Toll-like receptors and NOD2. Gut. 2005;54:1182–93. doi: 10.1136/gut.2004.062794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oda K, Kitano H. A comprehensive map of the toll-like receptor signaling network. Mol Syst Biol. 2006;2:0015. doi: 10.1038/msb4100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hegedus Z, Czibula A, Kiss-Toth E. Tribbles: a family of kinase-like proteins with potent signalling regulatory function. Cell Signal. 2007;19:238–50. doi: 10.1016/j.cellsig.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Hegedus Z, Czibula A, Kiss-Toth E. Tribbles: novel regulators of cell function; evolutionary aspects. Cell Mol Life Sci. 2006;63:1632–41. doi: 10.1007/s00018-006-6007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiss-Toth E, Bagstaff SM, Sung HY, et al. Human tribbles, a protein family controlling mitogen-activated protein kinase cascades. J Biol Chem. 2004;279:42703–8. doi: 10.1074/jbc.M407732200. [DOI] [PubMed] [Google Scholar]
- 13.Ord D, Ord T. Mouse NIPK interacts with ATF4 and affects its transcriptional activity. Exp Cell Res. 2003;286:308–20. doi: 10.1016/s0014-4827(03)00070-3. [DOI] [PubMed] [Google Scholar]
- 14.Wu M, Xu LG, Zhai Z, et al. SINK is a p65-interacting negative regulator of NF-kappaB-dependent transcription. J Biol Chem. 2003;278:27072–9. doi: 10.1074/jbc.M209814200. [DOI] [PubMed] [Google Scholar]
- 15.Du K, Herzig S, Kulkarni RN, et al. TRB3: a tribbles homolog that inhibits Akt/PKB activation by insulin in liver. Science. 2003;300:1574–7. doi: 10.1126/science.1079817. [DOI] [PubMed] [Google Scholar]
- 16.Yamamoto M, Uematsu S, Okamoto T, et al. Enhanced TLR-mediated NF-IL6 dependent gene expression by Trib1 deficiency. J Exp Med. 2007;204:2233–9. doi: 10.1084/jem.20070183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilkin F, Suarez-Huerta N, Robaye B, et al. Characterization of a phosphoprotein whose mRNA is regulated by the mitogenic pathways in dog thyroid cells. Eur J Biochem. 1997;248:660–8. doi: 10.1111/j.1432-1033.1997.t01-1-00660.x. [DOI] [PubMed] [Google Scholar]
- 18.Keeshan K, He Y, Wouters BJ, et al. Tribbles homolog 2 inactivates C/EBPalpha and causes acute myelogenous leukemia. Cancer Cell. 2006;10:401–11. doi: 10.1016/j.ccr.2006.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naiki T, Saijou E, Miyaoka Y, et al. TRB2, a mouse Tribbles ortholog, suppresses adipocyte differentiation by inhibiting AKT and C/EBPbeta. J Biol Chem. 2007;282:24075–82. doi: 10.1074/jbc.M701409200. [DOI] [PubMed] [Google Scholar]
- 20.Lin KR, Lee SF, Hung CM, et al. Survival factor withdrawal-induced apoptosis of TF-1 cells involves a TRB2-Mcl-1 axis-dependent pathway. J Biol Chem. 2007;282:21962–72. doi: 10.1074/jbc.M701663200. [DOI] [PubMed] [Google Scholar]
- 21.Eder K, Guan H, Sung HY, et al. Tribbles-2 is a novel regulator of inflammatory activation of monocytes. Int Immunol. 2008;20:1543–50. doi: 10.1093/intimm/dxn116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawai T, Akira S. TLR signaling. Semin Immunol. 2007;19:24–32. doi: 10.1016/j.smim.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Rogler G, Brand K, Vogl D, et al. Nuclear factor kappaB is activated in macrophages and epithelial cells of inflamed intestinal mucosa. Gastroenterology. 1998;115:357–69. doi: 10.1016/s0016-5085(98)70202-1. [DOI] [PubMed] [Google Scholar]
- 24.Schreiber S, Nikolaus S, Hampe J. Activation of nuclear factor kappa B inflammatory bowel disease. Gut. 1998;42:477–84. doi: 10.1136/gut.42.4.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egan LJ, Toruner M. NF-kappaB signaling: pros and cons of altering NF-kappaB as a therapeutic approach. Ann N Y Acad Sci. 2006;1072:114–22. doi: 10.1196/annals.1326.009. [DOI] [PubMed] [Google Scholar]
- 26.Lodes MJ, Cong Y, Elson CO, et al. Bacterial flagellin is a dominant antigen in Crohn disease. J Clin Invest. 2004;113:1296–306. doi: 10.1172/JCI20295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeng H, Wu H, Sloane V, et al. Flagellin/TLR5 responses in epithelia reveal intertwined activation of inflammatory and apoptotic pathways. Am J Physiol Gastrointest Liver Physiol. 2006;290:G96–G108. doi: 10.1152/ajpgi.00273.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Winter-Vann AM, Johnson GL. Integrated activation of MAP3Ks balances cell fate in response to stress. J Cell Biochem. 2007;102:848–858. doi: 10.1002/jcb.21522. [DOI] [PubMed] [Google Scholar]
- 29.Cheung PC, Campbell DG, Nebreda AR, et al. Feedback control of the protein kinase TAK1 by SAPK2a/p38alpha. Embo J. 2003;22:5793–805. doi: 10.1093/emboj/cdg552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yokoyama T, Nakamura T. Tribbles in disease: Signaling pathways important for cellular function and neoplastic transformation. Cancer Sci. 2011;102:1115–22. doi: 10.1111/j.1349-7006.2011.01914.x. [DOI] [PubMed] [Google Scholar]
- 31.Keeshan K, Bailis W, Dedhia PH, et al. Transformation by Tribbles homolog 2 (Trib2) requires both the Trib2 kinase domain and COP1 binding. Blood. 2010;116:4948–57. doi: 10.1182/blood-2009-10-247361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Savinova OV, Hoffmann A, Ghosh G. The Nfkb1 and Nfkb2 proteins p105 and p100 function as the core of high-molecular-weight heterogeneous complexes. Mol Cell. 2009;34:591–602. doi: 10.1016/j.molcel.2009.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Speirs K, Lieberman L, Caamano J, et al. Cutting edge: NF-kappa B2 is a negative regulator of dendritic cell function. J Immunol. 2004;172:752–6. doi: 10.4049/jimmunol.172.2.752. [DOI] [PubMed] [Google Scholar]
- 34.Ishimaru N, Kishimoto H, Hayashi Y, et al. Regulation of naive T cell function by the NF-kappaB2 pathway. Nat Immunol. 2006;7:763–72. doi: 10.1038/ni1351. [DOI] [PubMed] [Google Scholar]
- 35.Dejardin E. The alternative NF-kappaB pathway from biochemistry to biology: pitfalls and promises for future drug development. Biochem Pharmacol. 2006;72:1161–79. doi: 10.1016/j.bcp.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 36.Xiao G, Rabson AB, Young W, et al. Alternative pathways of NF-kappaB activation: a double-edged sword in health and disease. Cytokine Growth Factor Rev. 2006;17:281–93. doi: 10.1016/j.cytogfr.2006.04.005. [DOI] [PubMed] [Google Scholar]