Abstract
[Purpose] The aim of the present study was to analyze the effect of an ankle-foot orthosis on gait variables (velocity and cadence) of stroke patients. To do this, a systematic review was conducted of four databases. [Subjects and Methods] The papers identified were evaluated based on the following inclusion criteria: 1) design: controlled, clinical trial; 2) population: stroke patients; 3) intervention: analysis of spatiotemporal variables of gait with an ankle-foot orthosis; 4) control group with different intervention or no intervention; and 5) outcome: improvement in gait velocity or cadence. [Results] Thirteen controlled trials addressing the effect of an ankle-foot orthosis on gait variables of stroke patients were found. They exhibited methodological quality of 3 or more points on the PEDro scale. [Conclusion] While the findings suggest the benefits of an AFO regarding gait velocity, the impact of this type of orthosis on cadence remains inconclusive. Thus, there is a need for further well-designed randomized, controlled, clinical trials to establish better scientific evidence for the effects of AFO usage on gait variables of stroke patients.
Key words: Stroke, Orthosis, Gait
INTRODUCTION
Cerebrovascular accident (stroke) is one of the main causes of disability and mortality in the developed world1, 2). Stroke victims experience a number of neurological deficits and disabilities, such as hemiparesis, communication disorder, cognitive impairment and visual-spatial perception disorder3). Moreover, approximately 50 to 60% of stroke victims experience some degree of motor impairment even after completing the standard rehabilitation protocol, and approximately 50% are at least partially dependent on others with regard to activities of daily living3, 4).
According to Wit et al.5), the ability to walk following a stroke is often impaired due to muscle weakness, spasticity, compromised sensory-motor control and/or the loss of cognitive functions. Most hemiparetic patients exhibit motor dysfunction, which affects their ability to walk, leading to an abnormal gait pattern. Stroke victims exhibit coordination deficits that persist beyond the rehabilitation process, including altered trunk, pelvis, knee and ankle coordination in the standing position and during gait, leading to a reduction in walking endurance and velocity6).
A number of therapeutic methods are described in the literature for the motor recovery of limbs affected by spasticity, allowing improvements in strength, range of motion and function of patients with hemiparesis7,8,9,10). Equino-varus foot, which is common in these patients, shifts the weight support of the heel to the lateral-plantar surface of the foot, and may cause a loss of balance and a reduction in stride security. Ankle-foot orthoses (AFO) are prescribed to facilitate ankle control in cases of equinus and/or varus foot11), and they reduce energy expenditure while walking12).
Kinematic analysis has been employed for the evaluation of normal and pathological human gait and allows the analysis of spatiotemporal characteristics, such as step length, cadence (number of steps per minute), stride duration and velocity. The spatiotemporal characteristics of gait describe the quantitative aspects of the movement pattern13). According to Leung and Moseley14), changes in step length, duration in the stance and swing phases, and double support time are related to reductions in gait symmetry and gait velocity, leading to the specific gait pattern exhibited by patients with hemiparesis: a relatively shorter step length, a longer stance phase and a shorter swing phase of the affected side.
Recovering the ability to walk is an important goal of the rehabilitation process for stroke patients. According to Gok et al.15), gait velocity, cadence and step length are diminished in hemiparetic gait and devices, such as an AFO, can improve these aspects. An AFO is generally prescribed to provide mediolateral stability of the ankle in the stance phase, facilitate gait in the swing phase and support the ankle. However, some researchers hold the view that an AFO can prolong dependence on a mechanical device, leading to an increase in muscle disuse, especially the dorsiflexors of the ankle, with a consequent delay in functional recovery14).
The aim of the present study was to conduct a systematic review of the literature to determine the effect of an AFO on spatiotemporal gait variables (cadence and velocity) of stroke patients.
SUBJECTS AND METHODS
For the development of a systematic review, searches were performed for randomized controlled clinical trials that analyzed the effect of an AFO on stroke patients (acute/chronic; ischemic/hemorrhagic). Studies involving a combination of AFO use and co-intervention were avoided.
We searched for studies involving three-dimensional movement analysis of spatiotemporal gait variables (cadence and velocity) as well as measures of independent gait over short distances (6 and 10 meters).
Searches were carried out of the PubMed (Medline), LILACS, Scielo and Physiotherapy Evidence Database (PEDro) databases using the following descriptors: 1) Stroke; 2) Gait; 3) Stroke AND Gait; 4) Ankle Foot Orthosis; 5) Stroke AND Ankle Foot Orthosis; and 6) Spatiotemporal parameters.
The papers identified in the initial search were evaluated based on the following inclusion criteria: 1) design: controlled, clinical trial; 2) population: stroke patients; 3) intervention: analysis of spatiotemporal variables of gait with an ankle-foot orthosis; 4) control group with different intervention or no intervention; and 5) outcome: improvements in gait velocity or cadence.
The randomized controlled clinical trials selected were analyzed for methodological quality using the PEDro scale, which has 11 items for the evaluation of internal validity and statistical information of randomized controlled trials. Each adequately fulfilled item (with the exception of Item 1, which addresses external validity) receives 1 point and contributes to the score wich has a maximum of 10 points. The official scores described at the electronic addresses of the databases were used. If a paper analyzed was not found in one of the databases, the score was determined by two independent, blinded researchers.
The full texts of the selected papers served as the reference and benchmark for the discussion and broadening of the concepts of the issue addressed. Meta-analysis was not possible due to the lack of certain data necessary for statistical analysis as well as the use of different outcome measures. What follows is, therefore, a descriptive and comparative analysis of the findings.
RESULTS
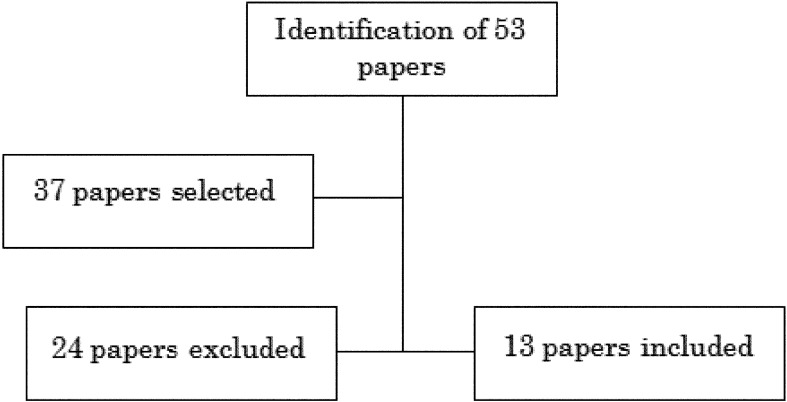
The initial search of the databases yielded 37 papers, 24 of which did not meet the inclusion criteria. Thus, 13 papers were found addressing the use of an AFO on hemiparetic gait, specifically improvements in the spatiotemporal variables of gait velocity or cadence (Fig. 1). The studies involved a total of 315 participants (216 men and 99 women), With a mean age of 56.8 years. The etiology of stroke was ischemic in 47 cases and hemorrhagic in 36 cases. A total of 114 patients had left-side hemiparesis and 126 had right-side hemiparesis. It is noteworthy that not all studies reported the type of stroke and prevalence of the affected side.
Fig. 1.
Flowchart of studies included in review
The initial search of the databases yielded 53 titles addressing the use of an AFO on hemiparetic gait. However, some papers did not meet the inclusion criteria and some did not achieve the necessary score on the PEDro scale merit inclusion in the present review. Other papers addressed alterations in other functional aspects, such as balance or muscle activity, and were therefore not selected. The final sample was made up of 13 papers that achieved a minimum of 3 points on the PEDro scale and were therefore considered methodologically adequate (Table 1 and 2
Table 2. Scores of papers included in review.
| PEDro | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
| Eligibility | N | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Randomized allocation | Y | N | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Concealed allocation | N | N | Y | N | N | N | N | N | N | Y | N | Y | Y |
| Similar prognosis | N | Y | Y | N | Y | Y | Y | Y | Y | N | N | Y | Y |
| Blinded subjects | N | N | N | N | N | N | N | N | N | N | N | N | N |
| Blinded therapists | N | N | N | N | N | N | N | N | N | Y | N | N | N |
| Blinded raters | N | Y | N | N | N | N | N | N | N | N | N | N | N |
| Key outcomes | N | N | Y | N | N | Y | N | N | N | N | N | Y | Y |
| Intention to treat | N | N | Y | N | N | N | N | N | N | N | N | N | N |
| Comparison between groups | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y |
| Precision and variability | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 3/10 | 4/10 | 6/10 | 3/10 | 3/10 | 4/10 | 3/10 | 4/10 | 3/10 | 5/10 | 3/10 | 6/10 | 6/10 |
Y = yes; N = no
).
Table 1. Data on papers included in review.
| Number of papers | Author and year of publication | PEDro | Type of study |
| 1 | Gok et al., 200315) | 3/10 | Clinical trial |
| 2 | Iwata et al., 200316) | 4/10 | Clinical trial |
| 3 | De Wit et al., 20045) | 6/10 | Clinical trial |
| 4 | Wang et al., 200517) | 3/10 | Clinical trial |
| 5 | Thijssen et al., 200618) | 3/10 | Clinical trial |
| 6 | Bleyenheuft et al., 200819) | 4/10 | Clinical trial |
| 7 | Simons et al., 200920) | 3/10 | Clinical trial |
| 8 | Fatone et al., 200921) | 4/10 | Clinical trial |
| 9 | Hiroaki et al., 200922) | 3/10 | Clinical trial |
| 10 | Lewallen et al., 201023) | 5/10 | Clinical trial |
| 11 | Chen et al., 201011) | 3/10 | Clinical trial |
| 12 | Erel et al., 201124) | 6/10 | Clinical trial |
| 13 | De Sèse et al., 201125) | 6/10 | Clinical trial |
In the present review, only outcomes regarding gait velocity and cadence (number of steps per minute) were considered. No analysis was performed regarding changes in stride or the step cycle or other aspects related to the benefits of the use of an AFO, which have been widely discussed in the literature. The papers included in the present review report significant differences in gait velocity with the use of an AFO, but divergent results regarding cadence (Table 3).
Table 3. Summary of outcomes.
| Author / Year | Sample | Outcome measures | Main outcomes |
| Gök et al., 200315) | n=12 stroke patients | Analysis of spatiotemporal gait variables, kinetic and kinematics using the 370 Vicon system under 3 conditions: without AFO, with plastic AFO and with metal AFO | - No significant difference in cadence under any condition; - Significant difference in gait velocity with both AFOs (0.32 m/s without AFO vs. 0.37 m/s with plastic AFO − p<0.05; 0.32 m/s without AFO vs. 0.41 m/s with metal AFO − p<0.05) |
| Iwata et al., 200316) | n=9 stroke patients (AFO group + tone inhibitory bar attached to AFO) and n=8 control group (AFO alone) | Cadence and gait velocity (10-m walk) | - Gait velocity increased by 13.8% (p=0.0045) in comparison to control group; - Cadence increased by 6.1% (p=0.0056) in comparison to control group |
| De Wit et al., 20045) | n=20 chronic stroke patients wearing AFO for at least six months | 10-meter walk test, Timed Up-and-Go (TUG) test and Stairs test performed with and without AFO | Statistically significant mean difference of 4.8 cm/s in gait velocity (95% CI: 0.85/8.7: p=0.02), 3.6 s on TUG (95% CI: 2.4/4.8: p=0.000) and 8.6 s on Stairs test (95% CI: 3.1/14.1: p=0.004) favoring AFO |
| Wang et al., 200517) | n=42 subjects with short-term hemiparesis (≤6 months) and 61 subjects with long-term hemiparesis (≥ 12 months) | Balance and gait with and without AFO; Static and dynamic balance activities evaluated using Balance System; functional balance evaluated using Berg scale; gait velocity and cadence measured during 10-m walk | - Significant improvement in gait velocity (0.58 m/s without AFO vs. 0.69 m/s with AFO − p=0.028) and cadence (75.06 steps/min without AFO vs. 87.26 steps/min with AFO − p=0.021) in group with short-term hemiparesis - No significant effects in group with long-term hemiparesis |
| Thijssen et al., 200618) | n=27 chronic stroke patients | Energy expenditure, gait velocity and step length under 3 conditions: without AFO, immediately after fitting of AFO and after 3 weeks of AFO usage | - Significant reduction in energy expenditure and increase in gait velocity immediately after fitting of AFO; - No significant difference in cadence; - No significant changes in gait pattern after 3 weeks of familiarization. |
| Bleyenheuft et al., 200819) | n=10 patients with chronic hemiparesis | 10-meter walk test, followed by instrumented gait test on treadmill under three conditions: without AFO, with rigid AFO and with dynamic Chignon orthosis | Mechanical work improved equally with both orthoses. Chignon orthosis led to significant improvement in gait velocity in comparison to no orthosis (0.81 m/s vs. 0.64 m/s − p<0.001) and segment kinematics of the ankle; No significant differences in cadence (p=0.79) |
| Simons et al., 200920) | n=20 stroke patients | Berg balance scale, Timed Up-and-Go test, Timed Balance test, 10-m walk test and Functional Ambulation Categories with and without AFO | Significant improvements in majority of functional tests with AFO; - Significant difference in 10-m walk test (0.58 ± 0.24 m/s with AFO vs. 0.46 ± 0.21 m/s without AFO − p=0.000) |
| Fatone et al., 200921) | n=16 stroke patients (mean age: 53.2 years) wearing AFO; n=12 healthy individuals (mean age: 57.1 years) | Gait analysis: kinetics, kinematics and gait variables | - No significant difference in gait velocity between groups (p=0.095) |
| Hiroaki et al., 200922) | n=16 stroke patients with hemparesis | Spatiotemporal gait analysis with and without use of plastic AFO walking on paper catwalk | - Significant increases in gait velocity, cadence, step length and stride length on affected and non-affected sides with use of AFO in comparison to non-use; - gait velocity: 18.1 m/s without AFO vs. 22.9 m/s with AFO (p=0.0032); - cadence: 66.8 steps/min without AFO vs. 73.3 steps/min with AFO (p=0.015) |
| Lewallen et al., 201023) | n=13 chronic stroke patients | Spatiotemporal gait analysis evaluated with rigid AFO, articulated AFO and without AFO (shoes alone) | No significant differences among groups |
| Chen et al., 201011) | n=14 stroke patients; n=11 healthy individuals | Gait analysis: kinetics, kinematics and gait variables under three conditions (without AFO, with anterior AFO and with posterior AFO) | - No significant differences in gait velocity, step length or duration of cycle in comparison to control group |
| Erel et al., 201124) | n=28 stroke patients with chronic hemiparesis allocated to an experimental group (EG) or a control group (CG) | Both groups initially evaluated in shoes alone; Experimental group evaluated after three months of dynamic AFO usage; Functional tests: Functional Reach, Timed Up-and-Go test, Timed Up Stairs, Timed Down Stairs, gait velocity and Physiological Cost Index | - No significant differences between groups regarding variables analyzed; - After 3 months, significant differences in Timed Up Stairs (12 s in EG vs. 15 s in CG − p=0.040) and gait velocity (0.99 m/s in EG vs. 0.72 m/s in CG − p=0.001); - No significant differences regarding Functional Reach, Timed Up-and-Go or Timed Down Stairs (p>0.05) |
| De Sèse et al., 201125) | n=28 stroke patients, 13 wearing Chignon AFO and 15 wearing standard AFO (control) | 10-meter walk test (gait velocity) and kinematic gait variables | - Significant increase in gait velocity in Chignon group over control group immediately (27.2 ± 36% vs. −0.8 ± 17% − p=0.006), after 30 days (39.9 ± 19% vs. 7.5 ± 17% − p=0.0004) and after 90 days (44.6 ± 27% vs. 17.1 ± 0.3% − p=0.04) |
DISCUSSION
According to Verma et al.26), impaired gait following a stroke is one of the most widely investigated aspects of neurological disorders, and the recovery of gait is one of the main goals of the rehabilitation process. A number of treatment methods have been developed to restore the walking ability of stroke patients. They include the use of an ankle-foot orthosis (AFO), which restricts the movement of the ankle, especially excessive plantar flexion, thereby enhancing stability in the stance phase and allowing greater freedom in the swing phase of the gait cycle14, 27,28,29).
A reduction in gait velocity is common among stroke victims. Mean gait velocity of healthy individuals is around 1.3 m/s, but ranges from 0.23 to 0.73 m/s among individuals with hemiparesis26). In the majority of studies analyzed, the use of a rigid or articulated AFO offered important benefits with regard to gait velocity of stroke patients, regardless of the material with which the device was made.
An AFO seems to exert a positive influence on the joint alignment of the affected lower limb, with improvements in cadence and gait velocity. While these variables alone do not represent improved gait stability, the analysis of such aspects allows a better practical understanding of the effects of physical therapy and improvements in the motor skills of stroke patients30).
The findings of the present review revealed divergence in the results of different studies regarding changes in cadence with the use of an AFO. While Iwata et al.16), Wang et al.17) and Hiroaki et al.22) report improvements in cadence, Chen et al.11), Gok et al.15), Thijssen et al.18) and Bleyenheuft et al.19) found no significant change in this variable. However, the same was true of gait velocity, as the majority of studies report significant improvements in gait velocity with the use of an AFO5, 15,16,17,18,19,20, 22, 24, 25). The exception was the study by Lewallen et al.23), but the authors compared gait velocity between use of rigid and articulated orthoses.
Gök et al.15) compared plastic and metal AFOs and found a significant increase in gait velocity in individuals with hemiparesis with both types of orthosis, but no significant changes in cadence. Iwata et al.16) analyzed the use of an inhibitory bar attached to an AFO worn by patients with hemiparesis and found an increase in gait velocity of approximately 13% as well as a significant increase in cadence (6%) in comparison to a control group. Bleyenheuft et al.19) compared gait velocity and cadence in the 10-meter walk test between a group wearing a rigid AFO and another group wearing a Chignon AFO, and found significant differences in gait velocity, but no changes in cadence. In a similar study, De Sèse et al.25) compared the Chignon AFO to a standard polypropylene AFO and found significant differences favoring the former immediately following fitting of the orthosis as well as after 30 and 90 days of usage.
In contrast to the above-mentioned findings, Chen et al.11) found no significant differences in spatiotemporal gait variables of stroke patients under three different conditions: 1) barefoot; 2) wearing an anterior AFO; and 3) wearing a posterior AFO. Likewise, Lewallen et al.23) found no significant differences in spatiotemporal gait variables of stroke patients wearing a rigid AFO and those wearing an articulated AFO.
Regarding the duration of use and adaptation to orthoses, a tendency toward an improvement in gait velocity and cadence was found with increased usage in the studies carried out by Erel et al.24) and De Sèse et al25). However, Thijssen et al.18) only found an immediate increase in gait velocity with the use of an AFO, there being no changes in either gait velocity or cadence after three weeks of familiarization with the orthosis.
In the comparisons of with and without the use of an AFO, or between an AFO group and a control group (without use of AFO), significant improvements in gait velocity were found15, 17, 20, 22, 24), and significant improvements in cadence were found in the studies by Wang et al.17) and Hiroaki et al22). In a retrospective study by Esquinazi et al.31) in a three-dimensional gait lab, Moss Rehabilitation Engineering Center, in the spatiotemporal aspects of gait of 42 patients were evaluated and a significant improvement in both the speed and cadence of gait of the patients using AFO orthoses: (0.31 m/s) × speed with AFO (0.41 m/s), p<0.001; and cadence without AFO (63.3 steps/min) × cadence with AFO (68.8 steps/min), p<0.001.
All studies11, 21) comparing stroke patients wearing an AFO with healthy individuals found no statistically significant differences between the groups in spatiotemporal gait variables, kinetics or kinematics. These findings demonstrate the benefits of an AFO with respect to functional improvements in gait, with the values approaching those found in healthy individuals.
Based on the findings, all types of AFO resulted in a significant improvement in gait velocity compared to a control group without the use of an AFO. However, divergent results were reported for cadence with and without the use of an AFO, as some studies report an improvement in this variable and others report no significant improvement. Since cadence is the number of steps take in a certain time, these patients showed significant improvements in gait speed without changing the number of steps per minute.
The main limitations encountered in this study were related to the nature of the data. Most studies used ratings for immediate use, or AFO types of with and without the same short-term, with neither a long-term analysis nor a convenience sample, without the sample calculation of sample size. This review notes only data related to speed and cadence of gait patients with stroke. Although this study is relevant in some aspects, there are still questions of a primarily clinical character that need to be answered, such as the best type of AFO to prescribe, the correct time to prescribe, and how long it should be used, among others.
REFERENCES
- 1.Ferrarello F, Baccini M, Rinaldi LA, et al. : Efficacy of physiotherapy interventions late after stroke: a meta-analysis. J Neurol Neurosurg Psychiatry, 2011, 82: 136–143 [DOI] [PubMed] [Google Scholar]
- 2.Meilink A, Hemmen B, Seelen HA, et al. : Impact of EMG-triggered neuromuscular stimulation of the wrist and finger extensors of the paretic hand after stroke: a systematic review of the literature. Clin Rehabil, 2008, 22: 291–305 [DOI] [PubMed] [Google Scholar]
- 3.Belda-Lois JM, Mena-del Horno S, Bermejo-Bosch I, et al. : Rehabilitation of gait after stroke: a review towards a top-down approach. J Neuroeng Rehabil, 2011, 8: 66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thaut MH, Kenyon GP, Hurt CP, et al. : Kinematic optimization of spatiotemporal patterns in paretic arm training with stroke patients. Neuropsychologia, 2002, 40: 1073–1081 [DOI] [PubMed] [Google Scholar]
- 5.de Wit DC, Buurke JH, Nijlant JM, et al. : The effect of an ankle-foot orthosis on walking ability in chronic stroke patients: a randomized controlled trial. Clin Rehabil, 2004, 18: 550–557 [DOI] [PubMed] [Google Scholar]
- 6.Hollands KL, Pelton TA, Tyson SF, et al. : Interventions for coordination of walking following stroke: systematic Review. Gait Posture, 2012, 35: 349–359 [DOI] [PubMed] [Google Scholar]
- 7.Rezende FB, Borges HC, Monteiro VC, et al. : Effectiveness of functional electrical stimulation on upper limb of chronic hemiparesis. Neurociencias, 2009, 17: 72–78 [Google Scholar]
- 8.Díez EG: Physiotherapy for spasticity: techniques and methods. Fisioterapia, 2004, 26: 25–35 [Google Scholar]
- 9.Spaich EG, Tabernig CB: Electrical stimulation and spasticity: a review. Rehabilitacion Madr, 2002, 36: 162–166 [Google Scholar]
- 10.Lima MO, Lima FS, Freitas ST, et al. : Effect of neuromuscular electrical stimulation and isotonic exercises in the flexors and extensors muscles knee in hemiplegic patients. Rev Neurol, 2008, 48: 135–138 [PubMed] [Google Scholar]
- 11.Chen CC, Hong WH, Wang CM, et al. : Kinematic Features of Rear-foot motion using anterior and posterior ankle-foot orthoses in stroke patients with hemiplegic gait. Arch Phys Med Rehabil, 2010, 91: 1862–1868 [DOI] [PubMed] [Google Scholar]
- 12.Bregman DJ, Harlaar J, Meskers CG, et al. : Spring-like ankle foot orthoses reduce the energy cost of walking by taking over ankle work. Gait Posture, 2012, 35: 148–153 [DOI] [PubMed] [Google Scholar]
- 13.Iwabe C, Diz MA, Barudy DP: Kinematic analysis of gait in individuals with cerebrovascular accident. Rev Neuroscienc, 2008, 16: 292–296 [Google Scholar]
- 14.Leung J, Moseley A: Impact of ankle-foot orthoses on gait and leg muscle activity in adults with hemiplegia: systematic literature review. Physiotherapy, 2003, 89: 39–55 [Google Scholar]
- 15.Gök H, Küçükdeveci A, Altinkaynak H, et al. : Effects of ankle-foot orthoses on hemiparetic gait. Clin Rehabil, 2003, 17: 137–139 [DOI] [PubMed] [Google Scholar]
- 16.Iwata M, Kondo I, Sato Y, et al. : An ankle-foot orthosis with inhibitor bar: effect on hemiplegic gait. Arch Phys Med Rehabil, 2003, 84: 924–927 [DOI] [PubMed] [Google Scholar]
- 17.Wang RY, Yen L, Lee CC, et al. : Effect of an ankle-foot orthosis on balance performance in patients with hemiparesis of different durations. Clin Rehabil, 2005, 19: 37–44 [DOI] [PubMed] [Google Scholar]
- 18.Thijssen DH, Paulus R, Van Uder CJ, et al. : Decreased energy cost and improved gait pattern using a new orthosis in persons with long-term stroke. Arch Phys Med Rehabil, 2007, 88: 181–186 [DOI] [PubMed] [Google Scholar]
- 19.Bleyenheuft C, Caty G, Lejeune T, et al. : Assessment of the Chignon dynamic ankle-foot orthosis using instrumented gait analysis in hemiparetic adults. Ann Readapt Med Phys, 2008, 51: 154–160 [DOI] [PubMed] [Google Scholar]
- 20.Simons CD, Van Asseldonk EH, Van der Kooij H, et al. : Ankle-foot orthosis in stroke: effects on functional balance, weight-bearing asymmetry and the contribution of each lower limb to balance control. Clin Biomech (Bristol, Avon), 2009, 24: 769–775 [DOI] [PubMed] [Google Scholar]
- 21.Fatone S, Gard SA, Malas BS: Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil, 2009, 90: 810–818 [DOI] [PubMed] [Google Scholar]
- 22.Hiroaki A, Michimata A, Sugawara K, et al. : Improving gait stability in stroke hemiplegic patients with a plastic ankle-foot orthosis. J Exp Med, 2009, 218: 193–199 [DOI] [PubMed] [Google Scholar]
- 23.Lewallen J, Miedaner J, Amyx S, et al. : Effect of three styles of custom ankle foot orthoses on the gait of stroke patients while walking on level and inclined surfaces. J Prosthet Orthot, 2010, 22: 78–83 [Google Scholar]
- 24.Erel S, Uygur F, Engin Simsek I, et al. : The effects of dynamic ankle-foot orthoses in chronic stroke patients at three-month follow-up: a randomized controlled trial. Clin Rehabil, 2011, 25: 515–523 [DOI] [PubMed] [Google Scholar]
- 25.de Sèze MP, Bonhomme C, Daviet JC, et al. : Effect of early compensation of distal motor deficiency by the Chignon ankle-foot orthosis on gait in hemiplegic patients: a randomized pilot study. Clin Rehabil, 2011, 25: 989–998 [DOI] [PubMed] [Google Scholar]
- 26.Verma R, Arya KN, Sharma P, et al. : Understanding gait control in post-stroke: implications for management. J Bodyw Mov Ther, 2012, 16: 14–21 [DOI] [PubMed] [Google Scholar]
- 27.Radtka SA, Oliveira GB, Lindstrom KE, et al. : The kinematic and kinetic affects of solid, hinged, and no ankle-foot orthosis on stair locomotion in healthy adults. Gait Posture, 2006, 24: 211–218 [DOI] [PubMed] [Google Scholar]
- 28.Cruz TH, Dhaher YY: Impact of ankle-foot-orthosis on frontal plane behaviors post stroke. Gait Posture, 2009, 30: 312–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kobayashi T, Leung AK, Akazawa Y, et al. : Design of a stiffness-adjustable ankle-foot orthosis and its effect on ankle joint kinematics in patients with stroke. Gait Posture, 2011, 33: 721–723 [DOI] [PubMed] [Google Scholar]
- 30.Padilha MG, Rueda FM, Diego AIM: Effect of ankle-foot orthosis in postural control after stroke: a systematic review. Neurologia, 2011. (in press). [DOI] [PubMed] [Google Scholar]
- 31.Esquenazi A, Ofluoglu D, Hirai B, et al. : The effect of an ankle-foot-orthosis on temporal spatial parameters and asymmetry of gait in hemiparetic patients. PM R, 2009, 1: 1014–1018 [DOI] [PubMed] [Google Scholar]