Abstract
Purpose
In certain cancers, MDM2 SNP309 has been associated with early tumor onset in women. In melanoma, incidence rates are higher in women than in men among individuals less than age 40; however, among those older than age 50, melanoma is more frequent in men than in women. To investigate this difference, we examined the association between MDM2 SNP309, age at diagnosis, and gender among melanoma patients.
Experimental Design
Prospectively enrolled melanoma patients (N=227) were evaluated for MDM2 SNP309 and the related polymorphism, p53 Arg72Pro. DNA was isolated from patient blood samples and genotypes were analyzed by PCR-RFLP. Associations between MDM2 SNP309, p53 Arg72Pro, age at diagnosis, and clinicopathologic features of melanoma were analyzed.
Results
The median age at diagnosis was 13 years earlier among women with a SNP309 GG genotype (46 years) compared to women with TG+TT genotypes (59 years; p=0.19). Analyses using age dichotomized at each decade indicated that women with a GG genotype had significantly higher risks of being diagnosed with melanoma at ages less than 50 compared to women 50 and older, but not 60 and older. At ages less than 50, women with a GG genotype had a 3.89 times greater chance of being diagnosed compared to women with TG+TT genotypes (p=0.01). Similar observations were not seen among men.
Conclusions
Our data suggest that MDM2 may play an important role in the development of melanoma in women. The MDM2 SNP309 genotype may help identify women at risk for developing melanoma at a young age.
Keywords: Melanoma, MDM2, SNP309, estrogen
Introduction
Melanoma incidence rates vary dramatically with gender and age. According to NCI SEER data (1), melanoma incidence rates are greater among women than men between the ages of 20 and 40, and among women in this age group melanoma incidence rates rise steeply. After the age of 40, melanoma incidence rates continue to rise in women, but at a slower pace. In men, the most rapid increase in incidence rates occurs between the ages of 50 and 80. As a result of these trends, the incidence rates of melanoma are greater among women than men at ages less than 40, equal in both sexes between the ages of 40 and 44, and greater among men than women at ages over 45. Interestingly, the natural incidence of menopause prior to age 40 is quite low; however, nearly 10% of postmenopausal women in the U.S. are between the ages of 40 and 50, with many others entering the menopause transition or perimenopause during this decade (2). The average age of menopause in the U.S. and other Western countries is 51 years (3). Given these observations, it is possible that the discordance in melanoma incidence rates between men and women, both above and below the age of 50, is related in part to estrogen signaling.
Recently, a single nucleotide polymorphism (SNP) at position 309 in the P2 promoter of MDM2 (rs2279744; T/G) has been associated with the onset of several different cancers among younger women. For example, women with an MDM2 SNP309 G allele display earlier-onset soft tissue sarcoma, diffuse large B-cell lymphoma, colorectal cancer, and non-small cell lung cancer compared to patients lacking the G allele (4–10). In these studies, the differences in tumor onset were observed when patients were divided into “premenopausal” and “postmenopausal” groups using the age of 51 as an approximation for menopausal status. Although these tumor types are not classically considered to be related to hormonal signaling, additional in-vitro studies demonstrated a mechanistic link to estrogen signaling. The estrogen receptor (ER) serves as a cotranscriptional activator of the transcription factor Sp1 by binding to its C-terminal domain (11). The presence of the G nucleotide at SNP309 increases the binding affinity of Sp1 for the promoter, and transcriptional activity of the MDM2 gene (12, 13). Studies of additional tumor types support the estrogen signaling hypothesis. For example, among ovarian cancers and invasive ductal carcinomas of the breast, the association between age of onset and SNP309 genotype was only observed among estrogen-receptor positive (versus estrogen-receptor negative) tumors (4, 14). More recently, endometrial cancer risk was found to be greater in women with a SNP309 GG genotype as compared to women with other genotypes, an important observation given that endometrial cancer risk increases with unopposed estrogen stimulation of the uterus (15).
MDM2 is a key negative regulator of the tumor suppressor, p53. Via its E3 ubiquitin ligase properties, MDM2 targets p53 for proteasomal degradation (16–18). In a subset of human tumors, overexpression of MDM2 is associated with accelerated cancer progression and lack of response to therapy (19). These observations suggest that MDM2 overexpression may substitute for p53 mutations in these tumors. Melanoma belongs to a group of tumors where p53 mutations are rare. Unexpectedly, our group found that MDM2 overexpression is an independent predictor of improved survival in melanoma (20), a finding that was later reproduced by another group of investigators (21). Similar observations have been made in other tumor types. MDM2 accumulation correlates with favorable clinical-pathological parameters in patients with esophageal, ovarian, colon, and non-small cell lung cancer (22–25), suggesting that MDM2 accumulation may not drive an aggressive, malignant phenotype in all tumors. A recent study in ovarian carcinoma found that the MDM2 SNP309 G allele correlated with increased overall survival despite an earlier age of onset (14).
Several studies in other tumors have examined the association between MDM2 SNP309 and a well-studied polymorphism in p53, Arg72Pro (rs1042522; R/P). The results have shown positive associations between the proline/proline (PP) genotype and disease risk for some tumor types (e.g. esophageal squamous cell carcinoma, lung cancer, renal cell carcinoma) but no association for other tumor types (e.g. colorectal cancer, breast cancer) (26–30). The association between the p53 Arg72Pro polymorphism itself and melanoma risk is controversial (31–34) with some studies showing associations between melanoma risk and the PP genotype (31–33), but others showing increased melanoma risk with the arginine/arginine (RR) genotype (34).
Our pilot study examines the relationship between MDM2 SNP309, p53 Arg72Pro, and patient and tumor clinicopathologic factors in a population of newly diagnosed melanoma patients.
Materials and Methods
Patient Population
The study cohort consisted of 227 newly diagnosed primary melanoma patients prospectively enrolled in the Interdisciplinary Melanoma Cooperative Group (IMCG) at the New York University (NYU) School of Medicine between August 2002 and November 2006. Clinicopathologic, demographic, and survival data were recorded prospectively for all patients. The NYU Institutional Review Board approved this study and informed consent was obtained from all patients at the time of enrollment.
Genotype Analysis
Genomic DNA was isolated from 227 peripheral blood leukocyte specimens collected at the time of patient enrollment (AutoGen, QuickGene Mini80, Holliston, MA). Twenty to 100 ng of genomic DNA from each sample was amplified by PCR using published primers and conditions for MDM2 SNP309 (12) and p53 Arg72Pro (34). Genotypes were determined by restriction fragment length polymorphism (RFLP) analysis using MspA1I (New England Biolabs, Ipswich, MA) for SNP309, and BstUI and BtgI (NEB) for Arg72Pro. Genotype assays contained negative and positive control DNAs. Eleven melanoma cell lines (SKMEL 19, 29, 85, 94, 100, 103, 147, 173, 187, 192, 197) were also analyzed for MDM2 SNP309 and p53 Arg72Pro genotypes.
Statistical Methods
Characteristics of melanoma patients were summarized using medians with interquartile ranges for continuous variables and percentages for categorical variables. Wilcoxon rank sum tests (for continuous variables) and chi-square statistics and Fisher’s exact tests (for categorical variables) were used to identify differences between men and women.
The associations between SNP309 and Arg72Pro genotypes were evaluated using Fisher’s exact tests. Histopathologic features of melanoma were compared by genotype separately for men and women using Kruskal-Wallis tests for continuous variables and chi-square statistics for categorical variables. The distributions of age of diagnosis by SNP309 genotype and Arg72Pro genotype are presented graphically for men and women using boxplots. The odds of being diagnosed with melanoma by a specified age for patients with the SNP309 GG genotype were compared to the odds of diagnosis by this age for patients with SNP309 TG or TT genotypes. This was done using odds ratios with 95% confidence intervals. These odds ratios were estimated for selected cutpoints of the age distribution.
Statistical analyses were performed at a significance level of 0.05 (2-sided). No adjustments were made for multiple comparisons. SAS 9.1 and SPSS 14.0 were used for statistical analyses.
Results
Patient characteristics
Table 1 presents a summary of patient and tumor characteristics. A total of 227 primary melanoma patients were studied. Ninety-eight percent of patients were Caucasian. The gender distribution of these patients, 59% men and 41% women, is nearly identical to the gender distribution of melanoma patients in the U.S. (1). The median age at melanoma diagnosis was 58 years, similar to the national median of 59 years. The distribution of melanomas by stage was 75.3% Stage I, 16.7% Stage II, 7.9% Stage III, and 0% Stage IV. No differences were found between men and women with respect to personal or family history of melanoma, histologic type, median tumor thickness, ulceration, or recurrence. However, the anatomic site of melanoma did differ significantly between men and women (p<0.001, Fisher’s exact test). This observation is in accordance with published epidemiologic data (35). In addition, 98% of patients in the study were Caucasian, as is typical for the incidence of melanoma in the U.S. population.
Table 1.
Characteristics of Study Population
| A. Patient Characteristics | Total N (%) |
Women N (%) |
Men N (%) |
|---|---|---|---|
| All Melanoma Patients | 227 (100) | 93 (41.0) | 134 (59.0) |
| Median age at diagnosis | 58 | 57 | 58.5 |
| History of multiple melanoma | 29 (12.8) | 12 (12.9) | 17 (12.7) |
| Family history of melanoma | 23 (10.1) | 11 (11.8) | 12 (9.0) |
| Stage of disease at recruitment | |||
| I | 171 (75.3) | 74 (79.6) | 97 (72.4) |
| II | 38 (16.7) | 14 (15.1) | 24 (17.9) |
| III | 18 (7.9) | 5 (5.4) | 13 (9.7) |
|
| |||
| B. Tumor Characteristics |
Total N (%) |
Women N (%) |
Men N (%) |
|
| |||
| Histologic Type | |||
| Superficial Spreading | 111 (48.9) | 46 (49.5) | 65 (48.5) |
| Nodular | 49 (21.6) | 16 (17.2) | 33 (24.6) |
| Other* | 32 (14.1) | 16 (17.2) | 16 (11.9) |
| Unclassified | 35 (15.4) | 15 (16.1) | 20 (14.9) |
| Median thickness, mm | 0.85 | 0.72 | 0.9 |
| Anatomic site | |||
| Axial | 132 (58.1) | 38 (40.9) | 94 (70.1) |
| Extremity | 95 (41.9) | 55 (59.1) | 40 (29.9) |
| Ulceration | 34 (15.0) | 12 (12.9) | 22 (16.4) |
| Recurrence | 14 (6.2) | 5 (5.4) | 9 (6.7) |
Unknown values are not included in the table.
“Other” is comprised of desmoplastic, lentigo maligna, and acral lentiginous, as well as those melanomas that did not fit into one histologic category.
MDM2 SNP309 and p53 Arg72Pro genotypes in patient germline DNA
As an initial analysis, we compared the PCR-RFLP genotyping methodology with routine sequencing of DNA extracted from 11 melanoma cell lines available in the lab. We found complete concordance between these methods, and used the PCR-RFLP method for the patient samples. An example of the genotyping results is shown in Figure 1. Among the cell lines, the distribution of MDM2 SNP309 genotypes was TT 18.2%, TG 54.5%, and GG 27.3%. The distribution of p53 Arg72Pro genotypes was RR 72.7%, RP 0%, and PP 27.3%. Supplemental Table 1 shows the SNP309 and Arg72Pro genotypes for each melanoma cell line. We subsequently examined MDM2 SNP309 and p53 Arg72Pro genotypes in the cohort of melanoma patients described above. We successfully amplified DNA from 216/227 (95.2%) patients for MDM2 SNP309, and from 213/227 (93.8%) patients for p53 Arg72Pro. MDM2 SNP309 genotype frequencies were TT 31.5%, TG 44.4%, and GG 24.1%; p53 Arg72Pro genotype frequencies were RR 57.7%, RP 35.2%, and PP 7.0%.
Figure 1. PCR-RFLP analysis of SNP309 and Arg72Pro genotypes.
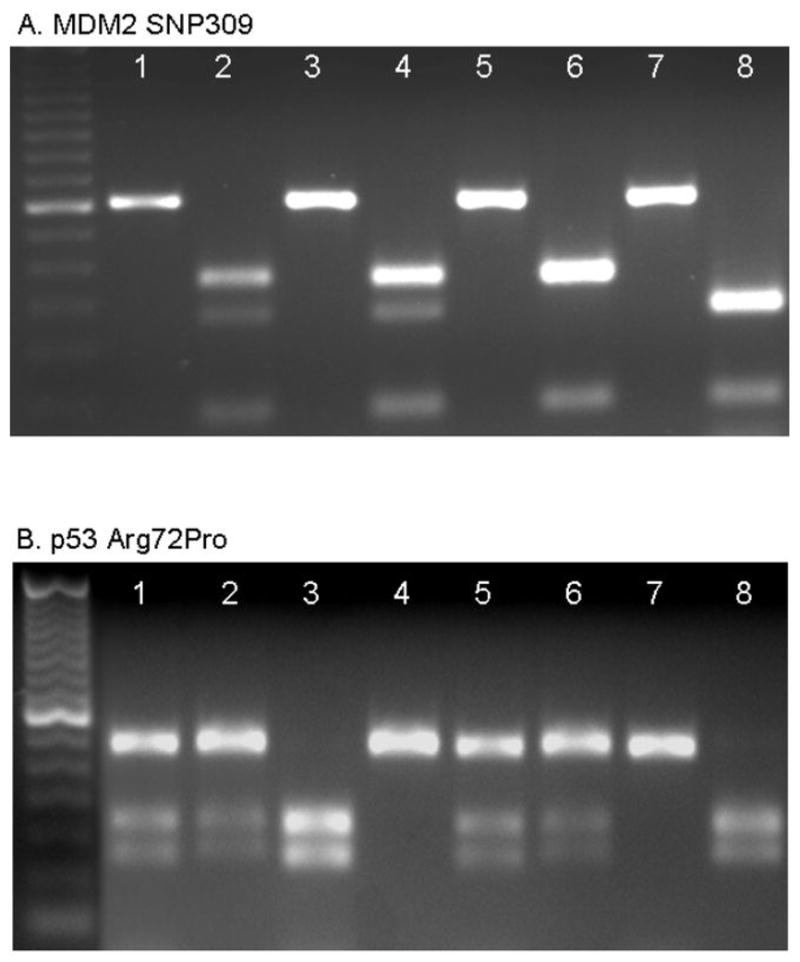
Each pair of lanes (e.g., 1+2, 3+4, etc.) represents the analysis from a single patient. A 50 bp ladder (left-most lane) was used to distinguish band size. A. MDM2 SNP309. Odd lanes were loaded with PCR products, and even lanes with the products of an MspA1I digest. One upper band (233 bp) represents the TT genotype (lane 6), two bands (233 and 187 bp) represent the TG genotype (lanes 2 and 4), and one lower band (187 bp) represents the GG genotype (lane 8). B. p53 Arg72Pro. Odd lanes were loaded with the products of the BstUI digest; even lanes with the products of the BtgI digest. In odd lanes, one upper band (296 bp) represents the PP genotype (lane 7), three bands (296, 169, and 127 bp) represent the RP genotype (lanes 1 and 5), and two lower bands (169, 127 bp) represent the RR genotype (lane 3). In even lanes, one upper band (296 bp) represents the RR genotype (lane 4), three bands (296, 169, and 127 bp) represent the RP genotype (lanes 2 and 6), and two lower bands (169, 127 bp) represent the PP genotype (lane 8).
Analysis of SNP309 and p53 Arg72Pro genotypes and clinicopathologic variables
We analyzed histopathologic features of each patient’s tumor specimen for association with the MDM2 and p53 genotypes. There were no associations between the polymorphisms and histopathologic subtype, tumor thickness, anatomic site and tumor ulceration (Tables 2A & 2B). In addition we did not find any association between these genetic polymorphisms and patient recurrence or overall survival (data not shown).
Table 2A.
Histopathologic features of melanoma by MDM2 SNP309 genotype
| Women (N=89) | Men (N=127) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Patient and Tumor Characteristics | TT N (%) |
TG N (%) |
GG N (%) |
P value | TT N (%) |
TG N (%) |
GG N (%) |
P value |
| All Melanoma Patients | 33 (37.1) | 35 (39.3) | 21 (23.6) | -- | 35 (27.6) | 61 (48.0) | 31 (24.4) | -- |
| History of multiple melanoma | 4 (12.5) | 5 (14.7) | 1 (5.0) | 0.63 | 4 (11.8) | 9 (15.8) | 3 (10.0) | 0.78 |
| Family history of melanoma | 6 (20.7) | 3 (9.1) | 2 (10.5) | 0.42 | 3 (8.8) | 5 (9.3) | 4 (14.8) | 0.73 |
| Stage of disease | ||||||||
| I | 26 (78.8) | 28 (80.0) | 18 (85.7) | 0.81 | 28 (80.0) | 40 (65.6) | 23 (74.2) | 0.56 |
| II | 4 (12.1) | 5 (14.3) | 3 (14.3) | 5 (14.3) | 14 (23.0) | 4 (12.9) | ||
| III | 3 (9.1) | 2 (5.7) | 0 (0) | 2 (5.7) | 7 (11.5) | 4 (12.9) | ||
| Histologic Type | ||||||||
| SS | 15 (45.5) | 17 (48.6) | 12 (57.1) | 0.72 | 17 (48.6) | 26 (42.6) | 15 (48.4) | 0.8 |
| Nodular | 4 (12.1) | 8 (22.9) | 4 (19.0) | 7 (20.0) | 20 (32.8) | 6 (19.4) | ||
| Other | 6 (18.2) | 6 (17.1) | 3 (14.3) | 5 (14.3) | 7 (11.5) | 4 (12.9) | ||
| Unclassified | 8 (24.2) | 4 (11.4) | 2 (9.5) | 6 (17.1) | 8 (13.1) | 6 (19.4) | ||
| Tumor thickness, mm (median, IQR) | 0.53 (1.05) | 0.85 (1.05) | 0.8 (0.92) | 0.41* | 0.78 (0.87) | 1.12 (2.0) | 0.90 (1.15) | 0.35* |
| Anatomic site | ||||||||
| Axial | 13 (39.4) | 13 (37.1) | 10 (47.6) | 0.62 | 24 (68.6) | 45 (73.8) | 22 (71.0) | 0.87 |
| Extremity | 20 (60.6) | 22 (62.9) | 11 (52.4) | 11 (31.4) | 16 (26.2) | 9 (29.0) | ||
| Ulceration | 2 (6.1) | 8 (22.9) | 2 (9.5) | 0.12 | 4 (11.4) | 14 (23.0) | 3 (9.7) | 0.2 |
| Recurrence | 3 (9.1) | 2 (5.7) | 0 (0) | 0.36 | 1 (2.9) | 6 (9.8) | 2 (6.5) | 0.5 |
Table 2B.
Histopathologic features of melanoma by p53 Arg72Pro genotype
| Women (N=87) | Men (N=126) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Patient and Tumor Characteristics | RR N (%) |
RP N (%) |
PP N (%) |
P value | RR N (%) |
RP N (%) |
PP N (%) |
P value |
| All Melanoma Patients | 52 (59.8) | 29 (33.3) | 6 (6.9) | -- | 71 (56.3) | 46 (36.5) | 9 (7.1) | -- |
| History of multiple melanoma | 7 (13.5) | 3 (10.3) | 0 (0.0) | 1 | 6(9.0) | 9 (20.0) | 1 (11.1) | 0.27 |
| Family history of melanoma | 8 (17.0) | 1 (3.4) | 1 (20.0) | 0.18 | 6 (8.5) | 5 (10.9) | 1 (11.1) | 1 |
| Stage of disease | ||||||||
| I | 43 (82.7) | 22 (75.9) | 4 (66.7) | 0.53 | 54 (76.1) | 31 (67.4) | 5 (55.6) | 0.47 |
| II | 7 (13.5) | 5 (17.2) | 1 (16.7) | 11 (15.5) | 10 (21.7) | 2 (22.2) | ||
| III | 2 (3.8) | 2 (6.9) | 1 (16.7) | 6 (8.5) | 5 (10.9) | 2 (22.2) | ||
| Histologic Type | ||||||||
| SS | 28 (53.8) | 14 (48.3) | 2 (33.3) | 0.81 | 32 (45.1) | 21 (45.7) | 4 (44.4) | 0.89 |
| Nodular | 7 (13.5) | 6 (20.7) | 2 (33.3) | 16 (22.5) | 14 (30.4) | 3 (33.3) | ||
| Other | 9 (17.3) | 6 (20.7) | 1 (16.7) | 9 (12.7) | 6 (13.0) | 1 (11.1) | ||
| Unclassified | 8 (15.4) | 3 (10.3) | 1 (16.7) | 14 (19.7) | 5 (10.9) | 1 (11.1) | ||
| Tumor thickness, mm (median, IQR) | 0.70 (0.91) | 0.77 (1.05) | 0.88 (8.04) | 0.83* | 0.76 (1.15) | 0.90 (1.48) | 1.70 (2.33) | 0.07* |
| Anatomic site | ||||||||
| Axial | 20 (38.5) | 13 (44.8) | 2 (33.3) | 0.78 | 52 (73.2) | 33 (71.7) | 6 (66.7) | 0.86 |
| Extremity | 32 (61.5) | 16 (55.2) | 4 (66.7) | 19 (26.8) | 13 (28.3) | 3 (33.3) | ||
| Ulceration | 6 (11.5) | 4 (13.8) | 2 (33.3) | 0.26 | 9 (12.7) | 9 (19.6) | 3 (33.3) | 0.2 |
| Recurrence | 2 (3.8) | 2 (6.9) | 1 (16.7) | 0.31 | 4 (5.6) | 4 (8.7) | 1 (11.1) | 0.63 |
P value calculated by Fisher’s Exact Test unless otherwise specified.
Kruskal-Wallis test
Unknown values are not included in the table. Stage of disease was at time of recruitment. SS=Superficial spreading. “Other” is comprised of desmoplastic, lentigo maligna, and acral lentiginous, as well as those melanomas that did not fit into one histologic category.
Association between SNP309 genotype, patient gender, and age at melanoma diagnosis
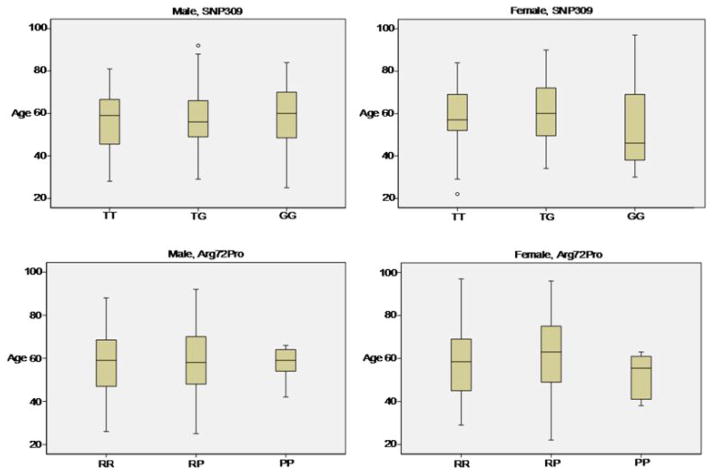
Figure 2 presents boxplots that summarize the distribution of age at diagnosis for MDM2 SNP309 and p53 Arg72Pro genotypes by gender. Overall, the median age at diagnosis in men was 58.5 years compared to 57 years in women. Among women, age at diagnosis ranged from 19 to 97 years of age, and was 13 years earlier among women with an MDM2 SNP309 GG genotype (median 46 years, IQR 31) as compared to women with TG+TT genotypes (median 59 years, IQR 19) (p=0.19, Mann-Whitney). Among men, age at diagnosis ranged from 25 to 92 years of age, and was approximately equal between men with an MDM2 SNP309 GG genotype (median 60 years, IQR 21.5) and men with TG+TT genotypes (median 58 years, IQR 19.5) (p=0.48, Mann-Whitney).
Figure 2. Age at melanoma diagnosis by SNP309 and Arg72Pro genotypes for men and women.
These boxplots display the distributions of age at diagnosis for patients categorized by gender and genotype. Each box marks off the lower and upper quartile of an age distribution; the line within the box represents the median age. The vertical lines outside the box terminate at the largest and smallest values beyond the box that are within 1.5 times the interquartile range (IQR) from the box; any point beyond 1.5 IQRs from the box is considered an outlier, as is indicated by the circles in Figures 2A and 2B. The relatively low age at diagnosis for women with the SNP309 GG genotype is evident in Figure 2B.
The distributions of MDM2 SNP309 genotypes among patients in 10-year age-at-diagnosis groups are shown in Table 3. Comparing women with the GG genotype to women with either TT or TG phenotypes, we observed that by the age of 50, 11/21 (52.4%) of women with a GG genotype were diagnosed with melanoma, compared to 15/68 (22.1%) of women with either a TT or TG genotype (p=0.0126, Fisher’s exact test). Among women with the GG genotype, the highest proportion 8/21 (38.1%) were diagnosed between the ages of 30–39 years. Among women with TG and TT genotypes, only 6/68 (8.8%) were diagnosed in the 30–39 year old age group (p=0.0034, Fisher’s exact test). These differences were not observed in men.
Table 3.
MDM2 SNP309 genotype distribution in 10-year age-at-diagnosis groups
| Women
| |||
|---|---|---|---|
| Age at diagnosis | TT+TG N (%) |
GG N (%) |
Total N (%) |
| 19–29 | 2 (2.9) | 0 (0) | 2 (2.2) |
| 30–39 | 6 (8.8) | 8 (38.1) | 14 (15.7) |
| 40–49 | 7 (10.3) | 3 (14.3) | 10 (11.2) |
| 50–59 | 19 (27.9) | 1 (4.8) | 20 (22.5) |
| 60–69 | 16 (23.5) | 4 (19.0) | 20 (22.5) |
| 70–79 | 11 (16.2) | 3 (14.3) | 14 (15.7) |
| 80–89 | 6 (8.8) | 0 (0) | 6 (6.7) |
| 90–99 | 1 (1.5) | 2 (9.5) | 3 (3.4) |
| Total | 68 (100) | 21 (100) | 89 (100) |
| Men
| |||
|---|---|---|---|
| Age at diagnosis | TT+TG N (%) |
GG N (%) |
Total N (%) |
| 19–29 | 2 (2.1) | 4 (12.9) | 6 (4.7) |
| 30–39 | 6 (6.3) | 2 (6.5) | 8 (6.3) |
| 40–49 | 19 (19.8) | 2 (6.5) | 21 (16.5) |
| 50–59 | 26 (27.1) | 7 (22.6) | 33 (26.0) |
| 60–69 | 26 (27.1) | 7 (22.6) | 33 (26.0) |
| 70–79 | 14 (14.6) | 7 (22.6) | 21 (16.5) |
| 80–89 | 2 (2.1) | 2 (6.5) | 4 (3.1) |
| 90–99 | 1 (1.0) | 0 (0) | 1 (0.8) |
| Total | 96 (100) | 31 (100) | 127 (100) |
p=0.0098 (Chi-square)
p=0.12 (Chi-square)
Percentages displayed are column percentages, representing percents within genotypes.
Table 4 shows the odds ratios for initial diagnosis of melanoma below a specified age (with age dichotomized at 10 year intervals) for patients with the SNP309 GG genotype as compared to patients with SNP309 TG+TT genotypes. This is shown separately for men and women. At age cutpoints below 50 years of age, women with the SNP309 GG genotype are more likely to be diagnosed with melanoma in the younger age category as compared to women with TG+TT genotypes; at age cutpoints of 60 and greater, the association is weak. Women with an MDM2 SNP309 GG genotype had a 3.89 times greater chance of being diagnosed at ages less than 50 years as compared to women with TG+TT genotypes (95% CI: 1.22, 12.31; p=0.01). Note that the odds ratio was 4.62 (95% CI: 1.23, 16.86; p=0.02) when an age of less than 40 was used as a cut point, though there was considerable overlap between the confidence intervals for the odds ratios when age was cut at 40 and at 50. These associations were not seen among men. p53 Arg72Pro genotypes were not associated with melanoma risk in women or men.
Table 4.
Odds ratios and exact 95% confidence intervals for initial diagnosis of melanoma at ages less than the age shown below, for the MDM2 SNP309 GG genotype compared to other MDM2 SNP309 genotypes
| Women (N=89) | Men (N=127) | |||
|---|---|---|---|---|
|
| ||||
| Age cutpoint | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval |
| 40 | 4.62 | (1.23, 16.86) | 2.64 | (0.68, 9.55) |
| 50 | 3.89 | (1.22, 12.31) | 0.89 | (0.31, 2.39) |
| 60 | 1.33 | (0.44, 4.08) | 0.76 | (0.31, 1.86) |
| 70 | 1.15 | (0.34, 4.60) | 0.53 | (0.19, 1.54) |
| 80 | 1.09 | (0.19, 11.61) | 0.47 | (0.05, 5.89) |
Discussion
Our study identified an important association between age at melanoma diagnosis, female gender, and the GG genotype for MDM2 SNP309. Although overall MDM2 SNP309 genotype frequencies did not differ between genders, women diagnosed at younger ages were more likely to have an MDM2 SNP309 GG genotype as compared to older women. The greatest odds ratio for the diagnosis of melanoma among women with a SNP309 GG genotype was for those under the age of 40 and the association remained significant as age increased to 50. The association was weak for ages of 50 and greater. The decrease in the odds ratio from 4.62 to 3.89 as the age cutpoint increased from age 40 to age 50 may reflect the fact that it is not uncommon for women to undergo menopause prior to the age of 50, but it is rare for this to occur prior to the age of 40 (2, 3). These findings, combined with the SEER epidemiologic observation that prior to the age of 40 melanoma is more common among women than men (but not after the age of 50), support the hypothesis that active estrogen signaling in combination with the GG genotype may contribute to melanoma onset in women. Nevertheless, this pilot study was limited by not having information regarding the menopausal status of our patients at the time of their melanoma diagnosis. A follow-up replication study will include these data to more precisely characterize the association between the SNP309 genotype and menopausal status at the time of melanoma diagnosis.
The role of estrogen in the development of melanoma remains controversial. The debate began in the 1970s when two initial observations were made: 1) young women taking oral contraceptives appeared to be at increased risk for melanoma (36), and 2) pregnancy-related skin pigmentation changes were linked to the accelerated synthesis of melanin by estrogen (37). While some follow-up studies found associations between oral contraceptives, hormonal replacement, pregnancy, and melanoma (38–41), others did not (42–46). In addition, immunohistochemical studies in melanoma showed little or no staining for what is now recognized as ERα (47–50); however, type-II, low affinity estrogen binding sites were detected in melanoma (51). Interestingly, ERβ, a subsequently discovered isoform of ER (52), was recently found to be expressed in 100% of 94 melanocytic lesions, while only 7.5% of these lesions expressed ERα (53). A meta-analysis of clinical trials using tamoxifen, a selective estrogen receptor modulator, in patients with metastatic melanoma showed that tamoxifen did not improve response or survival when administered with combined chemotherapy regimens (54); however, recent breast cancer studies have shown that ERβ may affect tumor resistance to tamoxifen (55–57), so it is conceivable that the failure of tamoxifen to improve outcomes in melanoma patients is related to the greater expression of ERβ versus ERα in melanoma.
Limitations of the current study include the lack of a group of patients unaffected by melanoma, and lack of patient ancestry data. Regarding non-melanoma controls, MDM2 SNP309 genotypes have been analyzed in over 2,000 control subjects worldwide (4, 6–8, 12, 26, 28, 58–63). The GG genotype frequency in these control individuals ranged from 10–34%, with no substantial variation between men and women. Variation in allele frequencies have been observed between ethnic populations and could potentially bias our results if the patients from one ethnic group were over-represented in a particular grouping of patients being analyzed. For example, Caucasians of Ashkenazi Jewish descent have been noted to harbor a higher frequency of GG genotypes (64); however, analysis of a subset of our patients (n=45) for whom self-reported ancestry data were available did not reveal an enrichment of Ashkenazi female patients below age 50, suggesting that it is unlikely that our results are biased by enrichment of patients from that ethnic group.
Recently, an analysis of MDM2 SNP309, p53 Arg72Pro, and skin cancer risk was published using patients from the Nurses Health Study. Among the 219 melanoma patients studied, no significant associations were observed between either of these polymorphisms and the risk of melanoma. There were also no statistically significant associations between these polymorphisms and the risk of basal cell carcinoma or squamous cell carcinoma (65). As they did not present an estimate of the risk of melanoma by age group, it is difficult to directly compare their results with ours. However, an important difference between these cohorts was the frequency of the GG genotype. Among their patients, the frequency of the GG genotype was 13% versus 24% in our cohort. Thus, they may have been unable to detect the association that we describe due to a lack of sufficient numbers of patients with the GG genotype. This difference in the frequencies of the GG genotype between the two cohorts may be related to differences in ancestry among the patients enrolled. Alternatively, it may be related to patient age at diagnosis. We found a high GG frequency (42%) in women diagnosed at ages less than 50 years, and a much lower frequency (14%) in women diagnosed at 50 years of age and older. The mean age of melanoma diagnoses in their cohort was 63.4 years versus 57 years for both the mean and median of women in our cohort. Therefore, it is possible that the lower GG genotype frequency in their cohort is related to the higher mean age of their patients compared to our patients.
Studies in other cancers have reported a combined effect of both MDM2 and p53 polymorphisms on cancer risk and survival (26–28). The effect of p53 Arg72Pro on melanoma remains controversial with some studies reporting associations between melanoma and the PP genotype (31–33), and others reporting associations between melanoma and the RR genotype (34). In our study, the distribution of p53 Arg72Pro genotypes did not vary by age or gender, and there was no evidence suggesting a strong association between the p53 Arg72Pro genotypes and melanoma risk, including a possible combined effect of both MDM2 SNP309 and p53 Arg72Pro genotypes on melanoma risk.
Several studies have examined the effect of MDM2 SNP309 on cancer survival. Studies in gastric and renal cell carcinomas have shown that MDM2 SNP309 associates with decreased survival (28, 60); however, a recent study in ovarian cancer has shown that MDM2 SNP309 associates with improved survival (14). Data from our group and others have shown that accumulation of MDM2 protein in primary melanoma is an independent predictor of improved survival (20, 21). It is possible that the increased expression of MDM2 in these patients was due to the presence of a SNP309 GG genotype. Unfortunately, germline DNA from the patients in our previous study is not available for analysis. In the current study, mean follow-up time was not sufficient to analyze the effects of MDM2 SNP309 on survival. Future studies will be conducted to address this question.
In conclusion, our pilot study suggests that MDM2 may play an important role in the development of melanoma in women. The MDM2 SNP309 genotype may help identify women at risk for developing melanoma at a young age. Also, these data suggest that it may be worthwhile to revisit the effects of estrogen on melanoma in the context of the appropriate MDM2 SNP309 genotype.
Supplementary Material
Statement of Translational Relevance.
One of the principles of cancer medicine is early detection of localized disease to prevent metastatic disease. Ideally, early detection efforts are best applied to those patients at highest risk for a given cancer. This manuscript describes a statistically significant relationship between age-related melanoma risk in women and an inherited genetic polymorphism. Although these results need to be replicated, the risk estimate is substantial for women under the age of 50, but not for older women, suggesting a role of female hormones in melanoma pathogenesis. On the clinical side, these findings may lead to a genetic test to identify women less than 50 who are at increased risk for melanoma. These patients may benefit from more careful early detection screening. In the laboratory, these results may stimulate research into the role of female hormones in melanoma.
Acknowledgments
Grant Support
Partial support provided by NYU Cancer Center Support Grant NCI P30 CA16087 (JDG, LR) Marc Jacobs Foundation
The authors would like to acknowledge Weiming Gai and Adam Litterman for assistance with laboratory methods, and Jessie Yu for help with collecting clinicopathologic data.
Footnotes
Conflict of Interest
The authors have no conflict of interest to declare.
References
- 1.Ries L, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2005. National Cancer Institute; Bethesda, MD: 2008. Based on November 2007 SEER data submission, posted to the SEER web site. [Google Scholar]
- 2.NAMS. Menopause Practice: A Clinician’s Guide. 3. Cleveland: The North American Menopause Society Professional Education Committee; 2007. Overview of Menopause and Aging; pp. 9–17. [Google Scholar]
- 3.Nelson HD. Menopause. Lancet. 2008;371:760–70. doi: 10.1016/S0140-6736(08)60346-3. [DOI] [PubMed] [Google Scholar]
- 4.Bond GL, Hirshfield KM, Kirchhoff T, et al. MDM2 SNP309 accelerates tumor formation in a gender-specific and hormone-dependent manner. Cancer research. 2006;66:5104–10. doi: 10.1158/0008-5472.CAN-06-0180. [DOI] [PubMed] [Google Scholar]
- 5.Bond GL, Menin C, Bertorelle R, Alhopuro P, Aaltonen LA, Levine AJ. MDM2 SNP309 accelerates colorectal tumour formation in women. J Med Genet. 2006;43:950–2. doi: 10.1136/jmg.2006.043539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lind H, Zienolddiny S, Ekstrom PO, Skaug V, Haugen A. Association of a functional polymorphism in the promoter of the MDM2 gene with risk of nonsmall cell lung cancer. Int J Cancer. 2006;119:718–21. doi: 10.1002/ijc.21872. [DOI] [PubMed] [Google Scholar]
- 7.Menin C, Scaini MC, De Salvo GL, et al. Association between MDM2-SNP309 and age at colorectal cancer diagnosis according to p53 mutation status. J Natl Cancer Inst. 2006;98:285–8. doi: 10.1093/jnci/djj054. [DOI] [PubMed] [Google Scholar]
- 8.Alhopuro P, Ylisaukko-Oja SK, Koskinen WJ, et al. The MDM2 promoter polymorphism SNP309T-->G and the risk of uterine leiomyosarcoma, colorectal cancer, and squamous cell carcinoma of the head and neck. J Med Genet. 2005;42:694–8. doi: 10.1136/jmg.2005.031260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yarden RI, Friedman E, Metsuyanim S, Olender T, Ben-Asher E, Papa MZ. MDM2 SNP309 accelerates breast and ovarian carcinogenesis in BRCA1 and BRCA2 carriers of Jewish-Ashkenazi descent. Breast Cancer Res Treat. 2007 doi: 10.1007/s10549-007-9797-z. [DOI] [PubMed] [Google Scholar]
- 10.Atwal GS, Rabadan R, Lozano G, et al. An information-theoretic analysis of genetics, gender and age in cancer patients. PLoS ONE. 2008;3:e1951. doi: 10.1371/journal.pone.0001951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saville B, Wormke M, Wang F, et al. Ligand-, cell-, and estrogen receptor subtype (alpha/beta)-dependent activation at GC-rich (Sp1) promoter elements. J Biol Chem. 2000;275:5379–87. doi: 10.1074/jbc.275.8.5379. [DOI] [PubMed] [Google Scholar]
- 12.Bond GL, Hu W, Bond EE, et al. A single nucleotide polymorphism in the MDM2 promoter attenuates the p53 tumor suppressor pathway and accelerates tumor formation in humans. Cell. 2004;119:591–602. doi: 10.1016/j.cell.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 13.Hu W, Feng Z, Ma L, et al. A single nucleotide polymorphism in the MDM2 gene disrupts the oscillation of p53 and MDM2 levels in cells. Cancer research. 2007;67:2757–65. doi: 10.1158/0008-5472.CAN-06-2656. [DOI] [PubMed] [Google Scholar]
- 14.Bartel F, Jung J, Bohnke A, et al. Both Germ Line and Somatic Genetics of the p53 Pathway Affect Ovarian Cancer Incidence and Survival. Clin Cancer Res. 2008;14:89–96. doi: 10.1158/1078-0432.CCR-07-1192. [DOI] [PubMed] [Google Scholar]
- 15.Grady D, Gebretsadik T, Kerlikowske K, Ernster V, Petitti D. Hormone replacement therapy and endometrial cancer risk: a meta-analysis. Obstetrics and gynecology. 1995;85:304–13. doi: 10.1016/0029-7844(94)00383-O. [DOI] [PubMed] [Google Scholar]
- 16.Haupt Y, Maya R, Kazaz A, Oren M. Mdm2 promotes the rapid degradation of p53. Nature. 1997;387:296–9. doi: 10.1038/387296a0. [DOI] [PubMed] [Google Scholar]
- 17.Kubbutat MH, Jones SN, Vousden KH. Regulation of p53 stability by Mdm2. Nature. 1997;387:299–303. doi: 10.1038/387299a0. [DOI] [PubMed] [Google Scholar]
- 18.Bond GL, Hu W, Levine AJ. MDM2 is a central node in the p53 pathway: 12 years and counting. Curr Cancer Drug Targets. 2005;5:3–8. doi: 10.2174/1568009053332627. [DOI] [PubMed] [Google Scholar]
- 19.Freedman DA, Levine AJ. Regulation of the p53 protein by the MDM2 oncoprotein--thirty-eighth G.H.A. Clowes Memorial Award Lecture Cancer research. 1999;59:1–7. [PubMed] [Google Scholar]
- 20.Polsky D, Melzer K, Hazan C, et al. HDM2 protein overexpression and prognosis in primary malignant melanoma. J Natl Cancer Inst. 2002;94:1803–6. doi: 10.1093/jnci/94.23.1803. [DOI] [PubMed] [Google Scholar]
- 21.Berger AJ, Camp RL, Divito KA, Kluger HM, Halaban R, Rimm DL. Automated quantitative analysis of HDM2 expression in malignant melanoma shows association with early-stage disease and improved outcome. Cancer research. 2004;64:8767–72. doi: 10.1158/0008-5472.CAN-04-1384. [DOI] [PubMed] [Google Scholar]
- 22.Abdel-Fattah G, Yoffe B, Krishnan B, Khaoustov V, Itani K. MDM2/p53 protein expression in the development of colorectal adenocarcinoma. J Gastrointest Surg. 2000;4:109–14. doi: 10.1016/s1091-255x(00)80041-4. [DOI] [PubMed] [Google Scholar]
- 23.Baekelandt M, Kristensen GB, Nesland JM, Trope CG, Holm R. Clinical significance of apoptosis-related factors p53, Mdm2, and Bcl-2 in advanced ovarian cancer. J Clin Oncol. 1999;17:2061. doi: 10.1200/JCO.1999.17.7.2061. [DOI] [PubMed] [Google Scholar]
- 24.Higashiyama M, Doi O, Kodama K, et al. MDM2 gene amplification and expression in non-small-cell lung cancer: immunohistochemical expression of its protein is a favourable prognostic marker in patients without p53 protein accumulation. British journal of cancer. 1997;75:1302–8. doi: 10.1038/bjc.1997.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saito H, Tsujitani S, Oka S, Ikeguchi M, Maeta M, Kaibara N. The expression of murine double minute 2 is a favorable prognostic marker in esophageal squamous cell carcinoma without p53 protein accumulation. Annals of surgical oncology. 2002;9:450–6. doi: 10.1007/BF02557267. [DOI] [PubMed] [Google Scholar]
- 26.Hong Y, Miao X, Zhang X, et al. The role of P53 and MDM2 polymorphisms in the risk of esophageal squamous cell carcinoma. Cancer research. 2005;65:9582–7. doi: 10.1158/0008-5472.CAN-05-1460. [DOI] [PubMed] [Google Scholar]
- 27.Zhang X, Miao X, Guo Y, et al. Genetic polymorphisms in cell cycle regulatory genes MDM2 and TP53 are associated with susceptibility to lung cancer. Hum Mutat. 2006;27:110–7. doi: 10.1002/humu.20277. [DOI] [PubMed] [Google Scholar]
- 28.Hirata H, Hinoda Y, Kikuno N, et al. MDM2 SNP309 Polymorphism as Risk Factor for Susceptibility and Poor Prognosis in Renal Cell Carcinoma. Clin Cancer Res. 2007;13:4123–9. doi: 10.1158/1078-0432.CCR-07-0609. [DOI] [PubMed] [Google Scholar]
- 29.Talseth BA, Meldrum C, Suchy J, Kurzawski G, Lubinski J, Scott RJ. MDM2 SNP309 T>G alone or in combination with the TP53 R72P polymorphism does not appear to influence disease expression and age of diagnosis of colorectal cancer in HNPCC patients. Int J Cancer. 2007;120:563–5. doi: 10.1002/ijc.22339. [DOI] [PubMed] [Google Scholar]
- 30.Schmidt MK, Reincke S, Broeks A, et al. Do MDM2 SNP309 and TP53 R72P interact in breast cancer susceptibility? A large pooled series from the breast cancer association consortium. Cancer research. 2007;67:9584–90. doi: 10.1158/0008-5472.CAN-07-0738. [DOI] [PubMed] [Google Scholar]
- 31.Stefanaki I, Stratigos AJ, Dimisianos G, et al. p53 codon 72 Pro homozygosity increases the risk of cutaneous melanoma in individuals with dark skin complexion and among noncarriers of melanocortin 1 receptor red hair variants. Br J Dermatol. 2007;156:357–62. doi: 10.1111/j.1365-2133.2006.07645.x. [DOI] [PubMed] [Google Scholar]
- 32.Han J, Cox DG, Colditz GA, Hunter DJ. The p53 codon 72 polymorphism, sunburns, and risk of skin cancer in US Caucasian women. Mol Carcinog. 2006;45:694–700. doi: 10.1002/mc.20190. [DOI] [PubMed] [Google Scholar]
- 33.Gwosdz C, Scheckenbach K, Lieven O, et al. Comprehensive analysis of the p53 status in mucosal and cutaneous melanomas. Int J Cancer. 2006;118:577–82. doi: 10.1002/ijc.21366. [DOI] [PubMed] [Google Scholar]
- 34.Shen H, Liu Z, Strom SS, et al. p53 codon 72 Arg homozygotes are associated with an increased risk of cutaneous melanoma. J Invest Dermatol. 2003;121:1510–4. doi: 10.1046/j.1523-1747.2003.12648.x. [DOI] [PubMed] [Google Scholar]
- 35.Kopf AW, Welkovich B, Frankel RE, et al. Thickness of malignant melanoma: global analysis of related factors. The Journal of dermatologic surgery and oncology. 1987;13:345–90. 401–20. doi: 10.1111/j.1524-4725.1987.tb03726.x. [DOI] [PubMed] [Google Scholar]
- 36.Beral V, Ramcharan S, Faris R. Malignant melanoma and oral contraceptive use among women in California. Br J Cancer. 1977;36:804–9. doi: 10.1038/bjc.1977.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hall PF. The influence of hormones on melanogenesis. Australas J Dermatol. 1969;10:125–39. [PubMed] [Google Scholar]
- 38.Ellis DL, Wheeland RG. Increased nevus estrogen and progesterone ligand binding related to oral contraceptives or pregnancy. J Am Acad Dermatol. 1986;14:25–31. doi: 10.1016/s0190-9622(86)70002-9. [DOI] [PubMed] [Google Scholar]
- 39.Holly EA, Cress RD, Ahn DK. Cutaneous melanoma in women: ovulatory life, menopause, and use of exogenous estrogens. Cancer Epidemiol Biomarkers Prev. 1994;3:661–8. [PubMed] [Google Scholar]
- 40.Holly EA, Weiss NS, Liff JM. Cutaneous melanoma in relation to exogenous hormones and reproductive factors. J Natl Cancer Inst. 1983;70:827–31. [PubMed] [Google Scholar]
- 41.Feskanich D, Hunter DJ, Willett WC, et al. Oral contraceptive use and risk of melanoma in premenopausal women. Br J Cancer. 1999;81:918–23. doi: 10.1038/sj.bjc.6690787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lederman JS, Lew RA, Koh HK, Sober AJ. Influence of estrogen administration on tumor characteristics and survival in women with cutaneous melanoma. J Natl Cancer Inst. 1985;74:981–5. [PubMed] [Google Scholar]
- 43.Lea CS, Holly EA, Hartge P, et al. Reproductive risk factors for cutaneous melanoma in women: a case-control study. Am J Epidemiol. 2007;165:505–13. doi: 10.1093/aje/kwk040. [DOI] [PubMed] [Google Scholar]
- 44.Osterlind A, Tucker MA, Stone BJ, Jensen OM. The Danish case-control study of cutaneous malignant melanoma. III. Hormonal and reproductive factors in women. Int J Cancer. 1988;42:821–4. doi: 10.1002/ijc.2910420603. [DOI] [PubMed] [Google Scholar]
- 45.Silipo V, De Simone P, Mariani G, Buccini P, Ferrari A, Catricala C. Malignant melanoma and pregnancy. Melanoma Res. 2006;16:497–500. doi: 10.1097/01.cmr.0000232295.91536.09. [DOI] [PubMed] [Google Scholar]
- 46.Lens MB, Rosdahl I, Ahlbom A, et al. Effect of pregnancy on survival in women with cutaneous malignant melanoma. J Clin Oncol. 2004;22:4369–75. doi: 10.1200/JCO.2004.02.096. [DOI] [PubMed] [Google Scholar]
- 47.Flowers JL, Seigler HF, McCarty KS, Sr, Konrath J, McCarty KS., Jr Absence of estrogen receptor in human melanoma as evaluated by a monoclonal antiestrogen receptor antibody. Arch Dermatol. 1987;123:764–5. [PubMed] [Google Scholar]
- 48.Cohen C, DeRose PB, Campbell WG, Schlosnagle DC, Sgoutas D. Estrogen receptor status in malignant melanoma. Am J Dermatopathol. 1990;12:562–4. doi: 10.1097/00000372-199012000-00005. [DOI] [PubMed] [Google Scholar]
- 49.Duncan LM, Travers RL, Koerner FC, Mihm MC, Jr, Sober AJ. Estrogen and progesterone receptor analysis in pregnancy-associated melanoma: absence of immunohistochemically detectable hormone receptors. Hum Pathol. 1994;25:36–41. doi: 10.1016/0046-8177(94)90168-6. [DOI] [PubMed] [Google Scholar]
- 50.Lecavalier MA, From L, Gaid N. Absence of estrogen receptors in dysplastic nevi and malignant melanoma. J Am Acad Dermatol. 1990;23:242–6. doi: 10.1016/0190-9622(90)70205-v. [DOI] [PubMed] [Google Scholar]
- 51.Piantelli M, Maggiano N, Ricci R, et al. Tamoxifen and quercetin interact with type II estrogen binding sites and inhibit the growth of human melanoma cells. J Invest Dermatol. 1995;105:248–53. doi: 10.1111/1523-1747.ep12317599. [DOI] [PubMed] [Google Scholar]
- 52.Mosselman S, Polman J, Dijkema R. ER beta: identification and characterization of a novel human estrogen receptor. FEBS Lett. 1996;392:49–53. doi: 10.1016/0014-5793(96)00782-x. [DOI] [PubMed] [Google Scholar]
- 53.Schmidt AN, Nanney LB, Boyd AS, King LE, Jr, Ellis DL. Oestrogen receptor-beta expression in melanocytic lesions. Exp Dermatol. 2006;15:971–80. doi: 10.1111/j.1600-0625.2006.00502.x. [DOI] [PubMed] [Google Scholar]
- 54.Lens MB, Reiman T, Husain AF. Use of tamoxifen in the treatment of malignant melanoma. Cancer. 2003;98:1355–61. doi: 10.1002/cncr.11644. [DOI] [PubMed] [Google Scholar]
- 55.Duong BN, Elliott S, Frigo DE, et al. AKT regulation of estrogen receptor beta transcriptional activity in breast cancer. Cancer research. 2006;66:8373–81. doi: 10.1158/0008-5472.CAN-05-3845. [DOI] [PubMed] [Google Scholar]
- 56.Esslimani-Sahla M, Simony-Lafontaine J, Kramar A, et al. Estrogen receptor beta (ER beta) level but not its ER beta cx variant helps to predict tamoxifen resistance in breast cancer. Clin Cancer Res. 2004;10:5769–76. doi: 10.1158/1078-0432.CCR-04-0389. [DOI] [PubMed] [Google Scholar]
- 57.Speirs V, Malone C, Walton DS, Kerin MJ, Atkin SL. Increased expression of estrogen receptor beta mRNA in tamoxifen-resistant breast cancer patients. Cancer research. 1999;59:5421–4. [PubMed] [Google Scholar]
- 58.Boersma BJ, Howe TM, Goodman JE, et al. Association of breast cancer outcome with status of p53 and MDM2 SNP309. J Natl Cancer Inst. 2006;98:911–9. doi: 10.1093/jnci/djj245. [DOI] [PubMed] [Google Scholar]
- 59.Copson ER, White HE, Blaydes JP, Robinson DO, Johnson PW, Eccles DM. Influence of the MDM2 single nucleotide polymorphism SNP309 on tumour development in BRCA1 mutation carriers. BMC Cancer. 2006;6:80. doi: 10.1186/1471-2407-6-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ohmiya N, Taguchi A, Mabuchi N, et al. MDM2 promoter polymorphism is associated with both an increased susceptibility to gastric carcinoma and poor prognosis. J Clin Oncol. 2006;24:4434–40. doi: 10.1200/JCO.2005.04.1459. [DOI] [PubMed] [Google Scholar]
- 61.Walsh CS, Miller CW, Karlan BY, Koeffler HP. Association between a functional single nucleotide polymorphism in the MDM2 gene and sporadic endometrial cancer risk. Gynecol Oncol. 2007;104:660–4. doi: 10.1016/j.ygyno.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 62.Alazzouzi H, Suriano G, Guerra A, et al. Tumour selection advantage of non-dominant negative P53 mutations in homozygotic MDM2-SNP309 colorectal cancer cells. J Med Genet. 2007;44:75–80. doi: 10.1136/jmg.2006.042572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilkening S, Hemminki K, Rudnai P, et al. No association between MDM2 SNP309 promoter polymorphism and basal cell carcinoma of the skin. Br J Dermatol. 2007;157:375–7. doi: 10.1111/j.1365-2133.2007.07994.x. [DOI] [PubMed] [Google Scholar]
- 64.Atwal GS, Bond GL, Metsuyanim S, et al. Haplotype structure and selection of the MDM2 oncogene in humans. Proc Natl Acad Sci U S A. 2007;104:4524–9. doi: 10.1073/pnas.0610998104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nan H, Qureshi AA, Hunter DJ, Han J. A functional SNP in the MDM2 promoter, pigmentary phenotypes, and risk of skin cancer. Cancer Causes Control. 2008 doi: 10.1007/s10552-008-9231-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.