Abstract
This meta-analysis was performed to assess sexual functions following adult male circumcision. We searched the Cochrane Central Register of Controlled Trials, PUBMED, EMBASE, the Cochrane Database of Systematic Review and Web of Science from their inception until January 2013 to identify all eligible studies that reported on men's sexual function after circumcision. The Cochrane Collaboration's RevMan 5.2 software was employed for data analysis, and the fixed or the random effect model was selected depending on the proportion of heterogeneity. We identified 10 studies, which described a total of 9317 circumcised and 9423 uncircumcised men who were evaluated for the association of circumcision with male sexual function. There were no significant differences in sexual desire (odds ratio (OR): 0.99; 95% confidence interval (CI): 0.92–1.06), dyspareunia (OR: 1.12; 95% CI: 0.52–2.44), premature ejaculation (OR: 1.13; 95% CI: 0.83–1.54), ejaculation latency time (OR: 1.33; 95% CI: 0.69–1.97), erectile dysfunctions (OR: 0.90; 95% CI: 0.65–1.25) and orgasm difficulties (OR: 0.97; 95% CI: 0.83–1.13). These findings suggest that circumcision is unlikely to adversely affect male sexual functions. However, these results should be evaluated in light of the low quality of the existing evidence and the significant heterogeneity across the various studies. Well-designed and prospective studies are required for a further understanding of this topic.
Keywords: complications, male circumcision, review, sexual function
Introduction
Male circumcision is one of the most commonly performed surgical procedures in the world. Globally, an estimated one-third of males are circumcised for religious, cultural, medical, personal preference and several other reasons.1 Circumcision is generally considered as a simple, rapid operation with efficacy for protection against HIV and other sexually transmitted infections, as confirmed in numerous, high-quality studies.2,3,4,5,6,7 Circumcision has been reported to adversely affect sexual function;8 however, the majority of studies, including high-quality ones9,10,11 and ones with data arising from randomized controlled trials (RCTs),12,13 show no difference or improvement in sexual function, sensitivity and satisfaction after circumcision. All of the data were considered by the American Academy of Pediatrics in formulating its 2012 policy, which concluded that there were no adverse effects on these parameters.14 Speculative assertions that the removal of fine-touch neuroreceptors of the foreskin, reorganization/atrophy of neural circuitry and keratinisation of the glans penis as a result of circumcision might lower sensitivity and lead to sexual dysfunction8,15,16,17 have been refuted by the American Academy of Pediatrics and through evaluations by experts of such reports.14,18,19,20,21,22
Across cultural, religious and health-related differences around the world, the pleasures of sexual intimacy and orgasm are ubiquitously considered as important for well-being and health, and sexual dysfunction may give rise to lowered self-esteem and dysfunctional relationships.23,24 In this context, we attempted to perform a systematic review and meta-analysis of the comparative effectiveness of circumcised and uncircumcised men on their sexual functions, including sexual desire, dyspareunia, premature ejaculation (PE), ejaculation latency time and erectile dysfunctions (EDs), by collecting all published relevant studies to provide a comprehensive survey that addresses this controversy.
Materials and methods
Data sources and search strategy
We searched the PUBMED, EMBASE, the Cochrane Database of Systematic Review and Web of Science from their inception until January 2013. The search terms used to identify potentially eligible studies from each data source were as follows: ‘circumcision, male' ‘circumcision' ‘sexual dysfunction' ‘ejaculation' ‘dyspareunia' ‘sexual desire' ‘orgasm' and ‘erection'. We also searched the reference lists of the relevant studies. Two of our authors independently screened all citations and abstracts identified by the search strategy used to screen eligible studies. Articles in other languages were also sought and evaluated.
Study outcomes
The primary outcomes in our work were PE and ED, and the secondary outcomes were low or lack of sexual desire, dyspareunia and orgasm difficulties. Because there is no agreement as to what constitutes PE, the quantifiable and objective outcome thrust times between penetration and ejaculation, namely, the intravaginal ejaculation latency time (IELT), were also analysed from the included studies.
Data extraction and quality assessment
Only studies that compared sexual functions with male circumcision status were included. All relevant studies identified from the search strategy were used for detailed assessment. Studies with insufficient data were not included due to potential statistical analysis limitations. Additionally, studies among men who had sex with other men were excluded because the sexual function criteria were unclear for such evaluations. Data were independently extracted from the included studies by two investigators. Discrepancies for study inclusion between the investigators were resolved by discussions or further consultations with a third investigator. The extracted data included data sources, eligibility, methods, participant characteristics, interventions and results. The quality of these eligible citations was assessed using the Newcastle-Ottawa Scale, which was independently scored by two investigators.
Data synthesis and analysis
Primary and secondary outcomes were calculated from the estimates of each study to enumerate pooled odds ratios (ORs) and confidence intervals (CIs). The Review Manager 5.2 software (The Cochrane Collaboration, Oxford, UK) statistical package was used to analyse the ORs for dichotomous variables and the mean differences for continuous variables. Meta-analyses were performed using this software to determine the ORs and CIs of men for the following criteria: PE, ED, dyspareunia, orgasm difficulties, and low or lack of sexual desire. The Mantel–Haenszel-type method was used to estimate the pooled ORs for all strata. The proportion of heterogeneity across the studies was tested using the I2 index (range: 0%–100%). If I2≤50%, the variation of the studies was considered to be homogenous and the fixed-effect model was adopted. If I2>50%, the variation of studies was considered as significantly heterogeneous and the random-effect model was adopted. All P values were two-tailed, and α<0.05 was considered statistically significant (P<0.05).
Results
Data retrieval
A total of 183 studies met the inclusion criteria on the basis of our search strategy and relevant references. Upon the completion of primary screenings by scanning titles and abstracts, the full texts of 19 potentially relevant studies were obtained for the secondary screenings. We excluded nine studies because of insufficient or duplicated data, or because they described female ‘circumcision'. Thus, 10 studies were identified as eligible for this systematic review, including a total of 18 740 participants (including self-controlled studies), of whom 9317 (49.72%) were circumcised (Figure 1).
Figure 1.
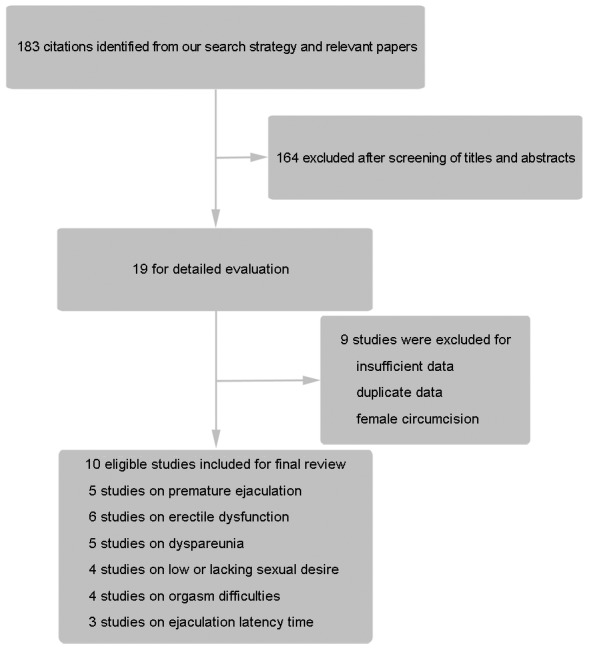
Flow diagram for selection of studies.
Study characteristics
Ten studies were included in our analysis (Table 1), which most relied on retrospective institutional data from case–control studies or on cross-sectional designs; however, two relatively well-designed studies were also eligible. Participants from these studies were relatively well represented, including Caucasian, Black African and Asian. The 10 studies selected for this meta-analysis described sexual-function criteria, including five with PE, six with ED, five with dyspareunia, four with orgasm difficulties, four with low or absent sexual desire and three with IELT. Nine of the eligible studies were published in English, and one was published in Chinese.
Table 1. Characteristics of the eligible studies.
| Study source | Country | Age (average (range)), year | Study design | Duration | Study size | NOS score (max: 9) |
|---|---|---|---|---|---|---|
| Frisch et al. (2011)17 | Denmark | — | Case–control study | — | 2345 | 6 |
| Waldinger et al. (2009)25 | Netherlands, Spain, United Kingdom and the United States | 38.5(/) | Case–control study | 4 weeks | 347 | 5 |
| Krieger et al. (2008)13 | Kenya | — | Randomized, controlled trial | 24 months | 2784 | — |
| Senol et al. (2008)26 | Turkey | 23.4 (18–27) | Self-controlled trial | 12 weeks | 43 | — |
| Kigozi et al. (2008)12 | Uganda | — (15–49) | Randomized, controlled trial | 24 months | 4456 | — |
| Richters et al. (2006)27 | Australia | — (16–59) | Case–control study | — | 7060 | 7 |
| Masood et al. (2005)28 | United Kingdom | — (18–60) | Self-controlled trial | ≥3 months | 84 | — |
| Senkul et al. (2004)29 | Turkey | 22.3 (19–28) | Self-controlled trial | ≥12 weeks | 42 | — |
| Shen et al. (2004)30 | China | 33.2 (22–51) | Self-controlled trial | 12 months | 95 | — |
| Laumann et al. (1997)9 | United States | — (18–59) | Case–control study | — | 1221 | 7 |
Abbreviation: NOS, Newcastle-Ottawa Scale.
PE and ejaculation latency time
PE data were available from five of the included studies, and three studies provided data on IELT. The difference in PE incidence between the circumcised and uncircumcised groups was not significant (OR: 1.13; 95% CI: 0.83–1.54) (Figure 2). In agreement with the PE data, the IELT between the circumcised and control groups demonstrated no significant difference (OR: 1.33; 95% CI: 0.69–1.97) (Figure 3).
Figure 2.
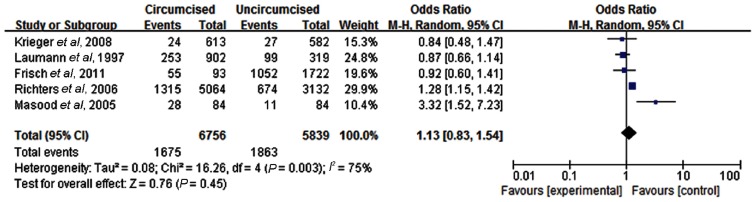
PE in circumcised and uncircumcised men. PE, premature ejaculation.
Figure 3.
Ejaculation latency time in circumcised and uncircumcised men.
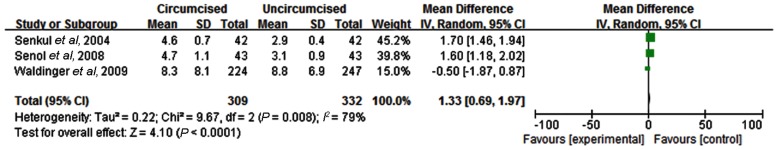
ED
Morbidities of ED or ‘trouble keeping an erection' in both the circumcised and uncircumcised group were presented in six of the included studies. Although the incidence of ED was variable between different studies, there was no significant difference in ED between the circumcised and uncircumcised groups (OR: 0.90; 95% CI: 0.65–1.25) (Figure 4).
Figure 4.
ED in circumcised and uncircumcised men. ED, erectile dysfunction.
Low or absent sexual desire
Three of the four studies that provided clear data were case–control studies. The prevalence of low or lack of sexual desire across the studies was generally low, and heterogeneity between the studies was minimal. There was no difference between the prevalence of low or reduced sexual desire (OR: 0.99; 95% CI: 0.92–1.06) (Figure 5).
Figure 5.
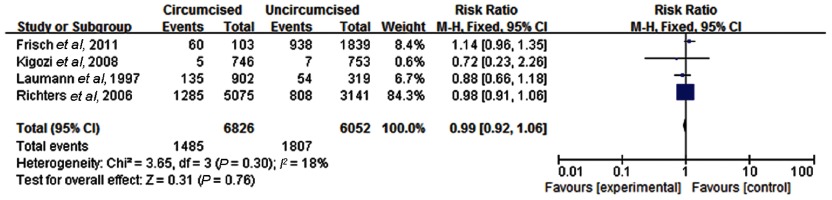
Low or lacking sexual desire in circumcised and uncircumcised men.
Dyspareunia and orgasm difficulties
Dyspareunia is defined as pain during or after sex and is more often observed in women than in men. In our meta-analysis, five included studies that focused on this issue. Like the other outcomes, no significant differences between the circumcised and control groups were observed (OR: 1.12; 95% CI: 0.52–2.44) (Figure 6). In the circumcised and uncircumcised groups, orgasm difficulties and the inability to ejaculate were examined in four studies. There were no statistically significant differences between the circumcised and the control groups (OR: 0.97; 95% CI: 0.83–1.13) (Figure 7).
Figure 6.
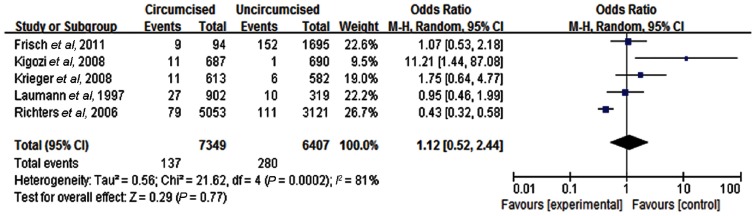
Dyspareunia in circumcised and uncircumcised men.
Figure 7.
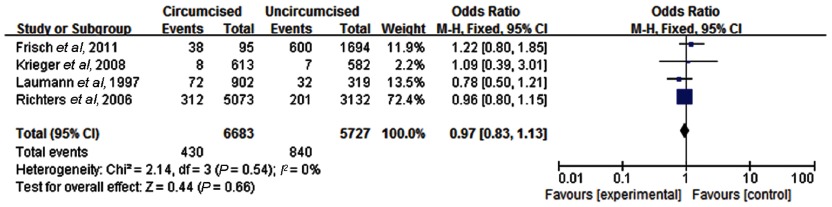
Orgasm difficulties in circumcised and uncircumcised men.
Discussion
Male circumcision has been performed for over 15 000 years and is practiced in almost all countries around the world. There is widespread belief that circumcision provides improved penile hygiene and protects against urinary tract infections, phimosis, paraphimosis, balanoposthitis, venereal diseases and cancer.5,14,18,22,31,32 It is claimed that the foreskin has important functions,32 but this has been disputed by lots of studies.14,18,19,20,21,22 The existing evidence from case–control, cross-sectional, cohort and RCT studies were analysed in our systematic review to ascertain pooled estimates of the sexual-function consequences of male circumcision. Overall, the results revealed no significant differences between circumcised and uncircumcised men regarding PE, IELT, ED, low or absent sexual desire, orgasm difficulties and dyspareunia.
Male sexual dysfunction has been considered as a neurobiological phenomenon or a psychological disturbance. The prepuce is a simple fold of skin composed of an outer keratinized (skin) and inner (mucosal) layers that are rich in nerves. Theoretically, partial or total surgical removal of the prepuce leaves the somatic penis sensory fibres exposed to direct stimulation and in theory could benefit sexual function. A cross-sectional study of Korean men reported decreased masturbatory pleasure after undergoing adult circumcision,33 although numerous flaws in this study have been identified.34
Although there is no universally accepted definition, PE is regarded as the most common sexual dysfunction in most countries.35 No significant difference was obtained based on the conflicting studies regarding the effect of male circumcision on PE and ejaculation latency time. This result is in agreement with a report by Hosseini et al.36 that described the post-circumcision, mucosal cuff length as not being a PE risk factor. Additionally, a recent study of Senel et al.37 that examined the long-term effects of circumcision on sexual function concluded that circumcision did not adversely affect sexual functions, but it caused a significant improvement in erectile function and overall sexual satisfaction. Similarly, in our work, we found that male circumcision did not adversely affect ED. Although the international index of erectile function is the most commonly used method for evaluating ED, the participant's self-reported erection status was mainly used to measure the outcome in most studies. The ability to achieve an orgasm is a major determinant of sexual and marital satisfaction. We obtained no evidence that this differed between the circumcised and uncircumcised groups. Nonetheless, decision-making should be made in accordance with the differences of PE evaluation and significant heterogeneity across the included studies.
Of the 10 studies included, only two involved data arising from large, well-designed RCTs and provided high-quality, epidemiological evidence. Most of the studies included in this meta-analysis are less rigorous in design and not very homogeneous, as they differ in their study populations. The recent manuscript by Frisch et al.17 focused on the association of circumcision status with subjective criteria, such as sexual experiences and difficulties with sexual desire, needs fulfilment and functioning, rather than objective parameters, such as PE, ejaculation latency time and ED. The authors concluded that circumcision was associated with frequent orgasm difficulties in Danish men. Waldinger et al.25 sought to investigate the intravaginal ejaculation latency time distribution in the general male population from different countries. This study included a ‘non-selected' sample of 474 men from The Netherlands, Spain, the United Kingdom, Turkey, and the United States. Senol et al.26 used a different study design that was based on the assessment of the participant's pudendal-evoked potential rather than utilizing a questionnaire.
The study of Richters et al.27 examined the effects of circumcision on the sexual health of 10 173 enrolled men but provided no evidence regarding the effects on sexual sensitivity. Conversely, Masood et al.28 reported a 38% improvement in penile sensation after circumcision. An overall 61% satisfaction rate was considered as a poor outcome of circumcision. In the study by Senkul et al.,29 the study group consisted of 42 male patients with a median age of 22.3 years, whose sexual performance was evaluated using the Brief Male Sexual Function Inventory and the ejaculatory latency time before and after circumcision. This report claimed an increase in the ejaculatory latency time after circumcision. The study by Shen et al.30 reported mild or moderate erectile dysfunction after circumcision, while Laumann et al.9 suggested that circumcised men engaged in more elaborate sets of sexual practices. However, this pattern differed across ethnic groups and suggests the influence of social factors.
Increased participant losses during follow-ups in several studies may adversely affect the findings as a result of non-response bias.12,13,28 The relatively short, post-circumcision follow-up period may not accurately reflect sexual function at a later time, resulting in risk of bias for this meta-analysis.26,28,29 Furthermore, the study validity may be affected by several factors, including subjective self-reporting, lack of physiological or laboratory indicators of sexual dysfunction or consensus on what constitutes sexual dysfunction for individuals with different education levels, cultures and religions. Moreover, operative methods, participants' ages and any coexisting medical conditions were not analysed by subgroup, and these could also contribute to study bias. Furthermore, well-designed trials seeking to minimize bias should be performed. Nevertheless, the data provided here affirm that the majority of published research arises from good to excellent studies on sexual function and sensitivity following circumcision. Because policy-makers have emphasized that infancy is the optimum time for circumcision for a variety of reasons,14,18,22 our findings should provide reassurance to parents when considering this procedure for their newborn sons.
Conclusion
In summary, male circumcision does not appear to adversely affect penile sexual function or sensitivity when compared with uncircumcised men. Although the literature contains a wide range of evidence for and against circumcision, the better quality studies affirm the recommendations of reputable experts who have evaluated the benefits and risks of circumcision as a desirable intervention early in life.14,18,22
Regardless of the present study outcome that shows an absence of adverse circumcision effects on a range of parameters related to sexual function and penile sensitivity, there is scope for further research, especially additional large, well-designed RCTs in diverse settings and over much longer time periods.
Author contributions
YT and KJW conceived the review. YT, WL and XY carried out the search, study selection and data extraction. YT, RW and JZW drafted the manuscript. KJW, WL and JZW participated in critical revision of the manuscript. All authors read and approved the final manuscript.
None of the authors have any conflicts of interests related to this study.
References
- Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO) Male circumcision: global trends and determinants of prevalence, safety and acceptability. Geneva; UNAIDS/WHO; 2007; [Google Scholar]
- Wawer MJ, Tobian AA, Kigozi G, Kong X, Gravitt PE, et al. Effect of circumcision of HIV-negative men on transmission of human papillomavirus to HIV-negative women: a randomised trial in Rakai, Uganda. Lancet. 2011;377:209–18. doi: 10.1016/S0140-6736(10)61967-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey RC, Moses S, Parker CB, Agot K, Maclean I, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- Morris BJ, Mindel A, Tobian AA, Hankins CA, Gray RH, et al. Should male circumcision be advocated for genital cancer prevention. Asian Pac J Cancer Prev. 2012;13:4839–42. doi: 10.7314/apjcp.2012.13.9.4839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellsague X, Bosch FX, Munoz N, Meijer CJ, Shah KV, et al. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. N Engl J Med. 2002;346:1105–12. doi: 10.1056/NEJMoa011688. [DOI] [PubMed] [Google Scholar]
- Morris BJ, Wiswell TE.Circumcision and lifetime risk of urinary tract infection: a systematic review and meta-analysis. J Urol 2012piiS0022-5347(12)05623-6. [DOI] [PubMed] [Google Scholar]
- Taylor JR, Lockwood AP, Taylor AJ. The prepuce: specialized mucosa of the penis and its loss to circumcision. Br J Urol. 1996;77:291–5. doi: 10.1046/j.1464-410x.1996.85023.x. [DOI] [PubMed] [Google Scholar]
- Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States. Prevalence, prophylactic effects, and sexual practice. JAMA. 1997;277:1052–7. [PubMed] [Google Scholar]
- Fink KS, Carson CC, DeVellis RF. Adult circumcision outcomes study: effect on erectile function, penile sensitivity, sexual activity and satisfaction. J Urol. 2002;167:2113–6. [PubMed] [Google Scholar]
- Payne K, Thaler L, Kukkonen T, Carrier S, Binik Y. Sensation and sexual arousal in circumcised and uncircumcised men. J Sex Med. 2007;4:667–74. doi: 10.1111/j.1743-6109.2007.00471.x. [DOI] [PubMed] [Google Scholar]
- Kigozi G, Watya S, Polis CB, Buwembo D, Kiggundu V, et al. The effect of male circumcision on sexual satisfaction and function, results from a randomized trial of male circumcision for human immunodeficiency virus prevention, Rakai, Uganda. BJU Int. 2008;101:65–70. doi: 10.1111/j.1464-410X.2007.07369.x. [DOI] [PubMed] [Google Scholar]
- Krieger JN, Mehta SD, Bailey RC, Agot K, Ndinya-Achola JO, et al. Adult male circumcision: effects on sexual function and sexual satisfaction in Kisumu, Kenya. J Sex Med. 2008;5:2610–22. doi: 10.1111/j.1743-6109.2008.00979.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics Task Force on Circumcision Circumcision policy statement Pediatrics 2012130585–6.22926180 [Google Scholar]
- Immerman RS, Mackey WC. A proposed relationship between circumcision and neural reorganization. J Genet Psychol. 1998;159:367–78. doi: 10.1080/00221329809596158. [DOI] [PubMed] [Google Scholar]
- Sorrells ML, Snyder JL, Reiss MD, Eden C, Milos MF, et al. Fine-touch pressure thresholds in the adult penis. BJU Int. 2007;99:864–9. doi: 10.1111/j.1464-410X.2006.06685.x. [DOI] [PubMed] [Google Scholar]
- Frisch M, Lindholm M, Gronbaek M. Male circumcision and sexual function in men and women: a survey-based, cross-sectional study in Denmark. Int J Epidemiol. 2011;40:1367–81. doi: 10.1093/ije/dyr104. [DOI] [PubMed] [Google Scholar]
- Morris BJ, Wodak AD, Mindel A, Schrieber L, Duggan KA, et al. Infant male circumcision: An evidence-based policy statement. Open J Prev Med. 2012;2:79–92. doi: 10.1111/j.1445-5994.2012.02823.x. [DOI] [PubMed] [Google Scholar]
- Waskett JH, Morris BJ. Fine-touch pressure thresholds in the adult penis. BJU Int. 2007;99:1551–2. doi: 10.1111/j.1464-410X.2007.06970_6.x. [DOI] [PubMed] [Google Scholar]
- Morris BJ, Waskett JH, Gray RH. Does sexual function survey in Denmark offer any support for male circumcision having an adverse effect. Int J Epidemiol. 2012;41:310–2–312–4. doi: 10.1093/ije/dyr180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris BJ, Waskett JH, Bollinger D, van Howe R. Claims that circumcision increases alexithymia and erectile dysfunction are unfounded: a critique of Bollinger and Van Howe's Alexthymia and circumcision trauma: a preliminary investigation. Int J Mens Health. 2012;11:177–84. [Google Scholar]
- Morris BJ, Waskett JH, Banerjee J, Wamai RG, Tobian AA, et al. A ‘snip' in time: what is the best age to circumcise. BMC Pediatr. 2012;12:20. doi: 10.1186/1471-2431-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symonds T, Roblin D, Hart K, Althof S. How does premature ejaculation impact a man s life. J Sex Marital Ther. 2003;29:361–70. doi: 10.1080/00926230390224738. [DOI] [PubMed] [Google Scholar]
- Althof SE. Psychological treatment strategies for rapid ejaculation: rationale, practical aspects, and outcome. World J Urol. 2005;23:89–92. doi: 10.1007/s00345-004-0489-6. [DOI] [PubMed] [Google Scholar]
- Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med. 2009;6:2888–95. doi: 10.1111/j.1743-6109.2009.01392.x. [DOI] [PubMed] [Google Scholar]
- Senol MG, Sen B, Karademir K, Sen H, Saracoglu M. The effect of male circumcision on pudendal evoked potentials and sexual satisfaction. Acta Neurol Belg. 2008;108:90–3. [PubMed] [Google Scholar]
- Richters J, Smith AM, de Visser RO, Grulich AE, Rissel CE. Circumcision in Australia: prevalence and effects on sexual health. Int J STD AIDS. 2006;17:547–54. doi: 10.1258/095646206778145730. [DOI] [PubMed] [Google Scholar]
- Masood S, Patel HR, Himpson RC, Palmer JH, Mufti GR, et al. Penile sensitivity and sexual satisfaction after circumcision: are we informing men correctly. Urol Int. 2005;75:62–6. doi: 10.1159/000085930. [DOI] [PubMed] [Google Scholar]
- Senkul T, IserI C, Sen B, KarademIr K, Saracoglu F, et al. Circumcision in adults: effect on sexual function. Urology. 2004;63:155–8. doi: 10.1016/j.urology.2003.08.035. [DOI] [PubMed] [Google Scholar]
- Shen Z, Chen S, Zhu C, Wan Q, Chen Z.Erectile function evaluation after adult circumcision. Zhonghua Nan Ke Xue 20041018–9.Chineses. [PubMed] [Google Scholar]
- Siegfried N, Muller M, Deeks JJ, Volmink J. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane Database Syst Rev. 2009. p. CD003362. [DOI] [PMC free article] [PubMed]
- Morris BJ, Gray RH, Castellsague X, Bosch FX, Halperin DT, et al. The strong protective effect of circumcision against cancer of the penis. Adv Urol. 2011;2011:812368. doi: 10.1155/2011/812368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Pang MG. The effect of male circumcision on sexuality. BJU Int. 2007;99:619–22. doi: 10.1111/j.1464-410X.2006.06646.x. [DOI] [PubMed] [Google Scholar]
- Willcourt R. The effect of male circumcision on sexuality. BJU Int. 2007;99:1169–70. doi: 10.1111/j.1464-410X.2007.06895_3.x. [DOI] [PubMed] [Google Scholar]
- Wylie KR, Ralph D. Premature ejaculation: the current literature. Curr Opin Urol. 2005;15:393–8. doi: 10.1097/01.mou.0000186844.40506.98. [DOI] [PubMed] [Google Scholar]
- Hosseini SR, Khazaeli MH, Atharikia D. Role of postcircumcision mucosal cuff length in lifelong premature ejaculation: a pilot study. J Sex Med. 2008;5:206–9. doi: 10.1111/j.1743-6109.2007.00477.x. [DOI] [PubMed] [Google Scholar]
- Senel FM, Demirelli M, Misirlioglu F, Sezgin T. Adult male circumcision performed with plastic clamp technique in Turkey: results and long-term effects on sexual function. Urol J. 2012;9:700–5. [PubMed] [Google Scholar]


