Abstract
Objectives
To investigate the bond strength and seal ability produced by AH Plus/gutta-percha, EndoREZ and RealSeal systems to root canal dentin.
Material and Methods
Sixty extracted single-root human teeth, instrumented manually to size 40, were divided into three groups (n=20) according to the sealer used; G1: AH Plus, G2: EndoREZ, and G3: RealSeal sealers. After filling using the lateral condensation technique, each sealer group was randomly divided into two subgroups according to the tests applied (n=10 for µPush-out test and n=10 for fluid filtration test). A fluid filtration method was used for quantitative evaluation of apical leakage. Four 1-mm-thick slices (cervical and medium level) were obtained from each root sample and a µPush-out test was performed. Failure modes were examined under microscopy at 40x, and a one-way ANOVA was applied to analyze the permeability. Non-parametrical statistics for related (Friedman's and Wilcoxon's rank tests) or unrelated samples (Kruskal-Wallis' and Mann-Whitney's tests) allowed for comparisons of µPush-out strength values among materials at the different levels. Statistical significance was accepted for p values <.05.
Results
There are no significant differences among fluid filtration of the three sealers. The sealer/core material does not significantly influence the µPush-out bond strength values (F=2.49; p=0.10), although statistically significant differences were detected with regard to root level (Chi2=23.93; p<0.001). AH Plus and RealSeal obtained higher bond strength to intraradicular dentin in the medium root slices.
Conclusions
There are no significant differences between the permeability and global µPush-out bond strength to root canal dentin achieved by AH Plus/gutta-percha, EndoREZ and RealSeal systems.
Keywords: Resin cements, Root canal filling material, Compressive strength, Leakage
INTRODUCTION
The fundamental goals of endodontic therapy are to achieve successful cleaning and shaping of root canals and a hermetic apical seal25. An ideal root canal sealer should adhere to both dentin and the core filling material. Methacrylate resin-based sealers, based on dentin adhesion technologies, have been developed in an attempt to seal the root canal system more effectively, improving bonding to radicular dentin26, but their utilization requires removal of the smear layer and collagen exposure, because retention is largely achieved by micromechanical interlocking between collagen matrix and resin29. Ethylenediaminetetraacetic acid (EDTA) has been widely used for this purpose as the final irrigant before applying methacrylate resin-based sealers5,13; however, the results were poor regarding its bond strength adhesion to root dentin, whereas the non-bonding AH Plus sealer presented greater adhesion7,10,17,18.
No correlation has been found between apical microleakage and sealer bond strengths to intraradicular dentin in vitro1,2. While we assume that preventing effective microleakage is perhaps more important for endodontic application than bond strength26, there is no universally accepted method for the evaluation of leakage33. Each has its limitations, being governed by electrical, filtration and/or diffusion laws24. Comparisons between different methods point to contradictory results, and, therefore, questionable clinical relevance12,24.
Push-out bond strength testing has become a common method for determining the effectiveness of adhesion between endodontic materials and intraradicular dentin. Zicari, et al.34 (2008) have correlated the push-out bond strength and sealing ability with the fluid filtration method of adhesive cements routinely used for fiber-post bonding, but to date there is no documented correlation using methacrylate resin-based sealers. We believe that this aspect is very important, because any filtration can hydrolytically degrade the adhesive interface. Hence, the purpose of this in vitro study was to quantitatively assess the bond strength to dentin root canal and the sealing properties of two methacrylate resin-based sealers and their corresponding core points (RealSeal and EndoREZ), then compare them with the gold standard conventional nonbonding AH Plus/gutta-percha. The µPush-out test and fluid filtration method were used to test the null hypothesis that there is no difference in the bond strength and sealing properties of RealSeal, EndoREZ systems and AH Plus/gutta-percha.
MATERIAL AND METHODS
We used 60 human anterior teeth, recently extracted for periodontal reasons from anonymous subjects under a protocol (nº 11/2011) approved by the Ethics Committee of the School of Dentistry, University of Granada. All teeth had single straight root canals and closed apices and none showed caries lesions or had received restorative or root canal treatment. After extraction, any calculus and soft tissue was removed and they were stored in 0.1% thymol diluted in distilled water at 4ºC for use in this study within 3 months following extraction.
The crowns of the teeth were cut perpendicular to the long axis of the root at the cement-enamel junction with a diamond coated disk at slow speed with constant water-cooling. Root canals were instrumented using the step back technique to obtain a flared preparation. In all teeth, the working length was determined visually by subtracting 1mm from the length of a #10 K-file (Dentsply Maillefer, Ballaigues, Switzerland) at the apical foramen. Biomechanical preparation was performed manually with K-files until size #40. After each step in the flare preparation, the canal was irrigated with 2.5% sodium hypochlorite during 1 min. Then, 17% EDTA was used as a final irrigant for 1 min, after a rinse of distilled water (1 min) to remove any remnants of the irrigating solutions. The canals were dried using paper points.
The roots were randomly divided into three equal groups (n=20) according to the root canal sealer used; G1: AH Plus (Dentsply Maillefer, Ballaigues, Switzerland), G2: EndoREZ (Ultradent Products, Inc., South Jordan, Utah, USA) and G3: RealSeal (Sybron Endo, Glendora, CA, USA).
For the group filled with AH Plus, the sealer was mixed using AH Plus jet mixing system, and then introduced into the root canal orifices with the intraoral tip. A 40.02 taper master gutta-percha cone was placed into the canal and then the canal was filled up using the cold lateral condensation technique and accessory gutta-percha points size #25 and #20 dipped in a small amount of sealer.
EndoREZ was mixed in an ultra-mixer and dispensed using a narrow diameter syringe (Skini Syringe) (Ultradent Products Inc., South Jordan, Utah, USA) with a fine-tipped cannula Navi Tip (Ultradent Products, Inc., South Jordan, Utah, USA). Roots were filled totally with EndoREZ sealer. Then a 40.02 resin coated gutta-percha cone (EndoREZ point) (Ultradent Products, Inc., South Jordan, Utah, USA) was placed inside the canal, and additional EndoREZ points size #25 and #20 were placed into the canal using the cold lateral condensation technique.
For the group filled with RealSeal, RealSeal Primer (SybronEndo, Glendora, CA, USA) was introduced into the root canal with a paper point (Roeko, Langenau, Germany) soaked with the primer for the apical region. The primer was placed into the middle and coronal part using a micro brush (Microbrush International, Grafton, WI, USA). After 30 seconds, excess primer was removed with paper points. The sealer was dispensed directly from the tip of its auto mix dual-chamber syringe, according to the manufacturer's instructions. A 40.02 taper RealSeal master point was placed into the canal and then additional RealSeal accessory points size #25 and #20 were placed into the canal using the cold lateral condensation technique.
In all specimens, the excess of points was removed with a hot instrument and the remainder was condensed vertically. They were resected at the apex perpendicular to the long axis of the tooth until 10 mm of root length was obtained. Each root was transferred to a test tube (Eppendorf Ibérica, Madrid, Spain) and stored in a humidifier at 37ºC for 24 hours to complete sealer setting. All preparation and obturation procedures were done by one operator.
Finally, each sealer group (n=20) was randomly divided into two subgroups according to tests applied (n=10 for µPush-out test and n=10 for fluid filtration test).
Leakage evaluation
The external root surfaces of subgroups for the fluid filtration test were covered with a layer of nail varnish leaving the coronal and apical orifices open. The specimens were attached to a device to measure the permeability by fluid transport described by Pashley, et al.22 (1988). The roots were inserted into a silicon tube (2 mm internal diameter), and attached with cyanoacrylate glue on the outer surface of the tube. A pressure tank of 250 ml of distilled water was placed 100 cm higher than the root to create a pressure of 100 cm H2O. A 10 ml micropipette was inserted and attached with cyanoacrylate glue to measure movement of the air bubble introduced into the system with a micro syringe. Fluid pressure was applied from the coronal area in apical direction. The volume of fluid transport was measured by observing the movement of air bubbles within a 10 ml micropipette at 24 hours.
Previously, the system was sealed and checked for 10 min to ensure there was no leakage. The root was covered with water and then covered with a plastic dish to prevent evaporation. Each specimen was attached to the device, and then the system was bled by opening the joint between the water reservoir and the specimen. The air bubble was then aligned with the zero point of the 10 ml scale. Permeability was measured as the distance that the bubble had moved by the end of 24 hours. This measurement showed the amount of fluid which had permeated through the root filling in µl. A test was done with two additional roots, covering the apex with two layers of nail varnish, to ensure that there was no leakage or fluid movement anywhere within the device.
Micro Push-out test
Ten roots for each group were cut into four slices 1 mm thick, from cervical to apical direction (Cervical1 [C1], Cervical2 [C2], Middle1 [M1], Middle2 [M2]), using a 300 µm thick sintered diamond wafering blade perpendicular to the long axis of the root canal at low speed with constant water cooling. The thickness of each root slice was assessed by means of a digital caliper. Each slice was subjected to compressive loading via a universal testing machine (Instron 3345, Instron Ltd, High Wycombe, UK) equipped with a 0.5 mm-diameter cylindrical plunger. The plunger was positioned so that it only touched the root filling on loading, without touching the canal wall or introducing shear stress along the interfaces. Thus, the side with the smaller diameter of the root canal faced upwards and was aligned with the shaft that would exert pressure load on the filling (apical-coronally) until the filling was displaced. The machine was calibrated at a constant speed of 0.5 mm/min, and the maximum failure load was recorded in Newton (N). Failure was shown by the extrusion of the intact cone of root filling from the root slice and affirmed by the appearance of a sharp drop along the load/time curve recorded by the testing machine. The computer and software attached to the universal testing machine calculated the µPush-out bond strength value for each specimen, and converted them into MPa by dividing the applied load by the bonded area.
The slices were examined under a stereomicroscope at 40x magnification to determine modes of failure: adhesive at filling material with dentin interface, cohesive within filling material, or mixed failure.
Statistical analysis
The normality of the data distribution in all the study groups was verified by applying the Shapiro-Wilk test, and Levene's test was used to explore the homogeneity of variance among groups.
Fluid movement values at 24 hours were compared among the three different sealers and filling materials by means of one-way ANOVA and Tukey's tests.
To analyze µPush-out bond strength values, an ANOVA for repeated measures was first applied to explore the influence of the root level (within-subject factor) and sealers/filling material (between-subjects factor) on the µPush-out bond strength to root walls. As the sample groups did not fulfill homoscedasticity requirements, non-parametrical tests were used to compare µPush-out bond strength values among materials (Kruskal-Wallis' and Mann-Whitney's U test) and root levels (Friedman's tests for multiple comparisons and Wilcoxon's rank tests, for pairwise comparison).
The Chi2 test was used to analyze the mode of failure distribution among groups. Differences were considered significant for p<0.05.
RESULTS
Permeability test
Mean fluid filtration values (SD) are recorded in Table 1. The AH Plus/gutta-percha group showed the highest value and the RealSeal group the lowest value, though there were no significant differences among the three sealer/core materials. This study makes manifest that all the materials used allowed fluid to flow along the root canal twenty four hours after filling.
Table 1.
Mean values and standard deviation of permeability (µL/24 h)
| Groups | Sealer | n | Mean permeability (sd) |
| I | AH Plus | 10 | 10.34(6.45) |
| II | EndoREZ | 10 | 8.49(5.92) |
| III | RealSeal | 10 | 6.20(3.82) |
Micro Push-out bond strength
Descriptive statistics of the µPush-out bond strength are given in Table 2.
Table 2.
Means and standard (MPa) deviations of µPush-out bond strength test. Different letters indicate significant differences in µPush-out strength values among root levels, for each material and for the whole sample
| Groups | Cervical1 | Cervical2 | Medium1 | Medium2 | Mean(sd) |
| AH Plus | 1.69(1.18)ª | 2.05(1.00)a,b | 2.48(1.32)a,b | 3.30(2.22)b1 | 2.38(1.14) |
| EndoREZ | 0.95(1.08) | 2.06(1.77) | 1.59(0.98) | 1.44(1.11) | 1.51(0.94) |
| RealSeal | 0.77(0.46)ª | 0.94(0.68)a,b | 3.41(1.88)b,c | 4.59(2.34)c | 2.43(1.01) |
| Mean (sd) | 1.14(1.01)ª | 1.69(1.31)b | 2.49(1.58)c | 3.11(2.31)c |
Different letters indicate significant differences in µPush-out strength values among root levels, for each material and for the whole sample
ANOVA for repeated measures demonstrated that root level (F=27.148, p<0.001), and the interaction between the root level and sealer/core material (F=8.66, p=0.001), significantly affect the µPush-out bond strength to the walls of the root canal. The sealer/core material in itself does not significantly influence the µPush-out bond strength values (F=2.492; p=0.102).
For the whole sample, statistically significant differences were detected with respect to the root level (Friedman's test, Chi2=23.93; p<0.001). Pairwise comparisons gave differences among all levels, with increased µPush-out values from cervical to apical except between M1 and M2 levels.
When each material was considered separately, AH Plus/gutta-percha also demonstrated significant differences according to root level, obtaining the lowest values in slice C1. For RealSeal system, the µPush-out bond strength increases apically, with C1≤C2≤M1=M2. EndoREZ system showed a similar behavior at all root levels (Chi2=3.54; p=0.315).
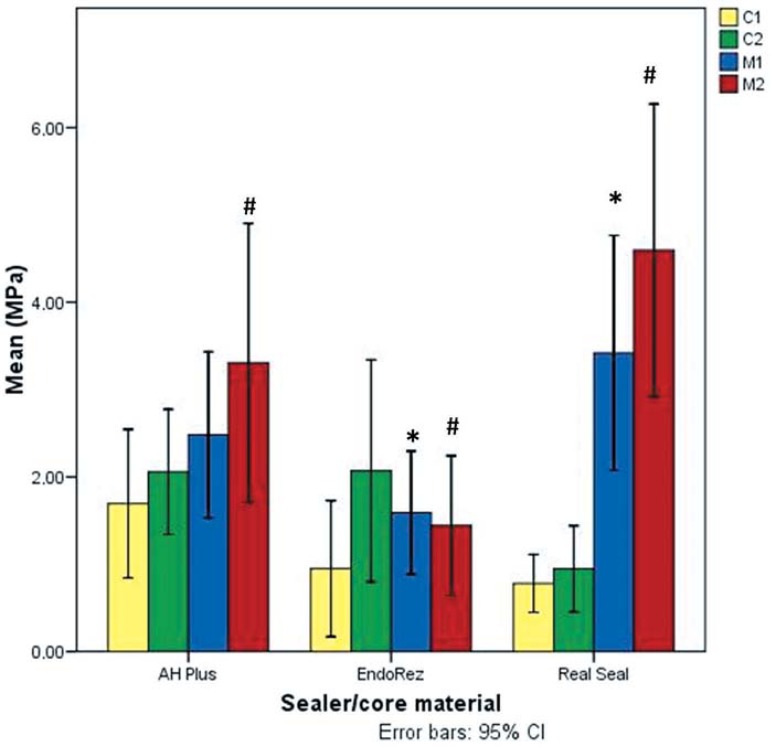
µPush-out values of the three sealing systems were also compared in each level. Levels C1 and C2 showed no differences in terms of sealer/core materials, but there were differences between sealers at deeper levels: M1 and M2. RealSeal demonstrated greater bond strength than EndoREZ at M1 level (U=21.00; p=0.028). At M2 level, EndoREZ showed a significantly lesser bond strength than AH Plus (U=22.00; p=0.034) and RealSeal (U=13.00; p=0.005) (Figure 1).
Figure 1.
Bar chart showing µPush-out bond strength values and comparisons among sealer/core materials in each root level (Mann-Whitney's U test)
*Significant differences among EndoREZ and Real Seal at M1 level
#Siginificant differences at M2 level: EndoREZ µPush-out was significantly lesser than the rest of sealer/core materials
Mode of failure
The predominating type of failure for all three sealer/core materials tested was adhesive failure, followed by mixed type failures. For the whole sample, this distribution was similar among the three sealers used (Chi2=2.45, p=0.65), and the four root levels (Chi2=4.66, p=0.58) (Table 3).
Table 3.
Failure mode. n (%). Different letters indicate significant differences in µPush-out strength values among root levels, for each material and for the whole sample
| Groups | Failure | Cervical1 | Cervical2 | Medium1 | Medium2 | Total |
| AH Plus | Adhesive Mixed Cohesive | 4 (13.30%) 5 (16.7%) 1 (3.3%) | 5 (16.5%) 3 (10.0%) 2 (6.7%) | 5 (16.7%) 3 (10.0%) 2 (6.7%) | 7 (23.3%) 3 (10.0%) 0 (0.0%) | 21 (52.5%) 14 (35%) 5 (12.5%) |
| EndoRez | Adhesive Mixed Cohesive | 6 (20.0%) 3 (10.0%) 1 (3.3%) | 4 (13.3%) 3 (10.0%) 3 (10.0%) | 8 (26.7%) 2 (6.7%) 0 (0.0%) | 9 (30.0%) 1 (3.3%) 0 (0.0%) | 27 (67.5%) 9 (22.5%) 4 (10.0%) |
| RealSeal | Adhesive Mixed Cohesive | 7 (23.3%) 3 (10.0%) 0 (0.0%) | 7 (23.3%) 3 (10.0%) 0 (0.0%) | 6 (20.0%) 3 (10.0%) 1 (3.3%) | 6 (20.0%) 2 (6.7%) 2 (6.7%) | 26 (65.0%) 11 (27.5%) 3 (7.5%) |
| Total | Adhesive Mixed Cohesive | 17 (56.7%) 11 (36.7%) 2 (6.7%) | 16 (53.3%) 9 (30.0%) 5 (16,7%) | 19 (63.3%) 8 (26.7%) 3 (10%) | 22 (73.3%) 6 (20.0%) 2 (6.7%) |
DISCUSSION
In this study, permeability and µPush-out bond strength were compared among roots treated endodontically with AH Plus, EndoREZ and RealSeal sealers and root canals filled using lateral condensation technique at 24 hours. The results showed that the permeability and global µPush-out bond strength is not affected by the kind of sealer/core material.
Microleakage studies are most commonly used to measure the ex vivo sealing ability of a root canal filling, though various methods have been proposed or recommended for evaluation of leakage33. In this study, an endodontic fluid transport model was chosen to evaluate the sealing ability of three different root canal sealers, in view of its advantages: the samples are not destroyed, it provides quantitative measurement, and the results are precise, as small volumes can be recorded15,19,24. We used different samples for fluid filtration and µPush-out bond strength, to be performed at exactly 24 hours' time, thus avoiding different degrees of conversion for the sealers. We did not light-cure the coronal portion of the RealSeal sealer as recommend by manufacturer's instruction, because fast-setting light-cured resin sealers produce restriction in the flow and consequent defects or weakening of bond strength9. Moreover, the slow chemical reaction of methacrylate-based self-etching sealers may reduce shrinkage stress by means of prolonged plastic flow during the setting time of the material14. We held that such behavior would allow for complete resin infiltration into the demineralized dentin.
Our results showed that there were no statistically significant differences in the values of fluid filtration among the three sealers used in the study. It is noteworthy, however, that none of the investigated sealers/core materials achieved a tight seal at the filling-cement-root interface, a point also brought out by Vasconcelos, et al.32 (2011), allowing fluid to flow along the filled root canal twenty-four hours after filling, whereas the control showed no filtration. Currently, the clinical relevance of leakage tests in vitro has been questioned12, because it is difficult to interpret results when, in our opinion, only zero filtration can be considered a good result. Moreover, there is no correlation among various methods to evaluate microleakage, and the outcome of the tests depends on the evaluation method12,24. In the absence of correlation between the ex vivo sealing ability of root filled teeth and "clinical success"20, we believe there is a threshold for microleakage values that would prove clinically relevant21.
The adhesion tests of methacrylate bond sealer to dentin have not yet been standardized. The µPush-out test seems to be more reliable because it allows for adequate standardization of the specimens, the absence of premature failures and the variability of data distribution, while supplying a better estimation of the actual bonding effectiveness11. In all of the studies reviewed, biomechanical preparation is done with mechanical instrumentation because it is easier to perform and provides a more appropriate standardization of root canals. We used the step back technique and lateral condensation because it is still widely used throughout the world; moreover, there is no study of endodontic sealer adhesion and µPush-out, because the small final diameter of the canal makes the µPush-out test more difficult to perform.
In this study, we used three totally different kinds of sealers: a conventional nonbonding epoxy resin-based sealer, AH Plus; a first generation non-acidic diurethane dimethacrylate and triethyleneglycol dimethacrylate, EndoREZ; and a second generation sealer, RealSeal, based on adhesive technology with a self-etching primer and in association with a thermoplastic synthetic polyester polymer-based root canal filling material. It should be noted that the conventional nonbonding AH Plus/gutta-percha root filling was equal to RealSeal and EndoREZ. These discouraging results are in line with those of Ungor, et al.31 (2006), who found that the Epiphany/Resilon combination was not superior to the AH Plus/gutta-percha combination. Still, most studies report that AH Plus sealer presents greater adhesion to dentin than RealSeal, regardless of root canal wall treatment3,7,18. Clinicians need to be aware that methacrylate resin-based sealers did not meet expectations regarding adhesion to root dentin, and, at this point in their development, there are no clear benefits in their use26.
The µPush-out bond strength results were significantly influenced by dentin location. AH Plus and RealSeal obtained higher values in the deeper slices, while EndoREZ showed the lowest values, regardless of location. All sealers exhibited their low µPush-out bond strength values in two superficial slices. This can be explained by the presence of oxygen, inhibiting sealer setting and producing a layer with low polymerization.
Because we adopted a clinical approach, we were not able to ascertain whether an increase of the adhesive strength to the apex will remain in the most apical sections. Manual instrumentation until 40 ISO width produce very limited widening of the canal in the apical section, making it impossible to perform µPush-out tests without values having a frictional component with the canal walls. Previous authors have tested apices, but no realistic enlargements were made regarding canal preparation with drills for a post2 or using a tapered diamond bur18.
The values of the µPush-out test are very low, consistent with results of other studies using the same methodology, indicating that the bonding of two methacrylate resin-based sealers and root dentin is much weaker than with resin-dentin bonds, 25-30 MPa30. Furthermore, the adhesive failures between sealer/dentin interface clearly suggest an inadequate level of adhesion between sealer and dentin in terms of bond strength2,17,27. This may be due to the difficulties in testing materials with great plasticity, such as gutta-percha, RealSeal and EndoREZ points; in contrast, when the test was done with sealer and no core material, values were higher1,2, suggesting failure may be traced to the sealer/material interface. In a root canal there is a highly unfavorable configuration factor (ratio of bonded to unbounded resin surfaces)6 that contributes to maximizing the polymerization stress of resin-based materials along the root canal walls; this may even exceed the bond strength of dentin adhesives to dentin, resulting in gap formation along the surfaces4,6,8. Along these lines, Souza, et al.28 (2012) report that there is a correspondence between the presence of gaps and microleakage.
Despite the material's relatively low bond strength to root dentin, it may be effective in preventing microleakage16. The main problem is that this low µPush-out bond strength is accompanied by fluid filtration. The adhesion of resin sealer to gutta-percha or core seems to play an important role in microleakage prevention, since it does not have to be at the sealer-dentin interface. Microleakage can affect the bonding of sealers to dentin by plasticization (fluids are absorbed by resins)8 and hydrolysis due to water entry in the interface. In addition, collagen degradation may occur due to host-derived matrix metalloproteinases (MMPs) in dentin that are slowly released over time when self-etching adhesives are used23. RealSeal may therefore adversely affect the longevity of bonded root canal fillings by accelerating degradation of the bond through the movement of fluid between the hybrid layer and unaffected dentin8,23.
This study reveals that global µPush-out bond strength and permeability were not affected by different sealer/core materials: this leads us to partially accept the null hypothesis, because in the two deeper slices, RealSeal and AH Plus achieved higher µPush-out bond strength than EndoREZ. We cannot confirm any clear relationship between permeability and µPush-out bond strength.
CONCLUSIONS
This study makes manifest that AH Plus/gutta-percha, EndoREZ and RealSeal systems allowed fluid to flow along the filled root canal in the twenty-four hours after filling. No significant differences were found among global µPush-out bond strengths of the three sealers/filling materials; but there does exist a regional influence, by which the µPush-out strength achieved with RealSeal and AH Plus to intraradicular dentin was found to be greater in the medium root slices.
Acknowledgments
ACKNOWLEDGEMENT
This investigation was supported by Research Grant no. CGL2011-25906.
REFERENCES
- 1.Babb BR, Loushine RJ, Bryan TE, Ames JM, Causey MS, Kim J, et al. Bonding of self-adhesive (self-etching) root canal sealers to radicular dentin. J Endod. 2009;35:578–582. doi: 10.1016/j.joen.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Barbizam JV, Trope M, Tanomaru-Filho M, Teixeira EC, Teixeira FB. Bond strength of different endodontic sealers to dentin: pushout test. J Appl Oral Sci. 2011;19:644–647. doi: 10.1590/S1678-77572011000600017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braga RR, Ferracane JL. Alternatives in polymerization contraction stress management. Crit Rev Oral Biol Med. 2004;15:176–184. doi: 10.1177/154411130401500306. [DOI] [PubMed] [Google Scholar]
- 4.Braga RR, Ferracane JL, Condon JR. Polymerization contraction stress in dual-cure cements and its effect on interfacial integrity of bonded inlays. J Dent. 2002;30:333–340. doi: 10.1016/s0300-5712(02)00047-7. [DOI] [PubMed] [Google Scholar]
- 5.Carvalho AS, Camargo CH, Valera MC, Camargo SE, Mancini MN. Smear layer removal by auxiliary chemical substances in biomechanical preparation: a scanning electron microscope study. J Endod. 2008;34:1396–1400. doi: 10.1016/j.joen.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 6.Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996;21:17–24. [PubMed] [Google Scholar]
- 7.De-Deus G, Di Giorgi K, Fidel S, Fidel RA, Paciornik S. Push-out bond strength of Resilon/Epiphany and Resilon/Epiphany self-etch to root dentin. J Endod. 2009;35:1048–1050. doi: 10.1016/j.joen.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 8.De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84:118–132. doi: 10.1177/154405910508400204. [DOI] [PubMed] [Google Scholar]
- 9.Feilzer AJ, de Gee AJ, Davidson CL. Setting stresses in composites for two different curing modes. Dent Mater. 1993;9:2–5. doi: 10.1016/0109-5641(93)90095-8. [DOI] [PubMed] [Google Scholar]
- 10.Fisher MA, Berzins DW, Bahcall JK. An in vitro comparison of bond strength of various obturation materials to root canal dentin using a push-out test design. J Endod. 2007;33:856–858. doi: 10.1016/j.joen.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 11.Goracci C, Tavares AU, Fabianelli A, Cardoso PC, Tay FR, Ferrari M. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004;112:353–361. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 12.Karagenç B, Gençoglu N, Ersoy M, Cansever G, Külekçi G. A comparison of four different microleakage tests for assessment of leakage of root canal fillings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:110–113. doi: 10.1016/j.tripleo.2005.10.044. [DOI] [PubMed] [Google Scholar]
- 13.Khedmat S, Shokouhinejad N. Comparison of the efficacy of three chelating agents in smear layer removal. J Endod. 2008;34:599–602. doi: 10.1016/j.joen.2008.02.023. [DOI] [PubMed] [Google Scholar]
- 14.Lawson MS, Loushine B, Mai S, Weller RN, Pashley DH, Tay FR, et al. Resistance of a 4-META-containing, methacrylate-based sealer to dislocation in root canals. J Endod. 2008;34:833–837. doi: 10.1016/j.joen.2008.03.028. [DOI] [PubMed] [Google Scholar]
- 15.Miletic I, Anic I, Pezelj-Ribaric S, Jukic S. Leakage of five root canal sealers. Int Endod J. 1999;32:415–418. doi: 10.1046/j.1365-2591.1999.00254.x. [DOI] [PubMed] [Google Scholar]
- 16.Nagas E, Altundasar E, Serper A. The effect of master point taper on bond strength and apical sealing ability of different root canal sealers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e61–e64. doi: 10.1016/j.tripleo.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 17.Nagas E, Uyanik MO, Eymirli A, Cehreli ZC, Vallittu PK, Lassila LV, et al. Dentin moisture conditions affect the adhesion of root canal sealers. J Endod. 2012;38:240–244. doi: 10.1016/j.joen.2011.09.027. [DOI] [PubMed] [Google Scholar]
- 18.Nunes VH, Silva RG, Alfredo E, Sousa-Neto MD, Silva-Sousa YT. Adhesion of Epiphany and AH Plus sealers to human root dentin treated with different solutions. Braz Dent J. 2008;19:46–50. doi: 10.1590/s0103-64402008000100008. [DOI] [PubMed] [Google Scholar]
- 19.Oliver CM, Abbott PV. An in vitro study of apical and coronal microleakage of laterally condensed gutta-percha with Ketac-Endo and AH-26. Aust Dent J. 1998;43:262–268. doi: 10.1111/j.1834-7819.1998.tb00175.x. [DOI] [PubMed] [Google Scholar]
- 20.Oliver CM, Abbott PV. Correlation between clinical success and apical dye penetration. Int Endod J. 2001;34:637–644. doi: 10.1046/j.1365-2591.2001.00442.x. [DOI] [PubMed] [Google Scholar]
- 21.Özok AR, Verhaagen B, Wesselink PR. Improving the accuracy of a fluid transport method. Int Endod J. 2013;46:348–354. doi: 10.1111/j.1365-2591.2012.02123.x. [DOI] [PubMed] [Google Scholar]
- 22.Pashley DH, Derkson GD, Tao L, Derkson M, Kalathoor S. The effects of a multi-step dentin bonding system on dentin permeability. Dent Mater. 1988;4:60–63. doi: 10.1016/s0109-5641(88)80091-5. [DOI] [PubMed] [Google Scholar]
- 23.Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, et al. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83:216–221. doi: 10.1177/154405910408300306. [DOI] [PubMed] [Google Scholar]
- 24.Pommel L, Jacquot B, Camps J. Lack of correlation among three methods for evaluation of apical leakage. J Endod. 2001;27:347–350. doi: 10.1097/00004770-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Santos JN, Carrilho MR, De Goes MF, Zaia AA, Gomes BP, Souza-Filho FJ, et al. Effect of chemical irrigants on the bond strength of a self-etching adhesive to pulp chamber dentin. J Endod. 2006;32:1088–1090. doi: 10.1016/j.joen.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Schwartz RS. Adhesive dentistry and endodontics. Part 2: bonding in the root canal system-the promise and the problems: a review. J Endod. 2006;32:1125–1134. doi: 10.1016/j.joen.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 27.Shokouhinejad N, Sharifian MR, Jafari M, Sabeti MA. Push-out bond strength of Resilon/Epiphany self-etch and gutta-percha/AH26 after different irrigation protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e88–e92. doi: 10.1016/j.tripleo.2010.05.069. [DOI] [PubMed] [Google Scholar]
- 28.Souza SF, Francci C, Bombana AC, Kenshima S, Barroso LP, D'Agostino LZ, et al. Qualitative SEM/EDS analysis of microleakage and apical gap formation of adhesive root-filling materials. J Appl Oral Sci. 2012;20:329–334. doi: 10.1590/S1678-77572012000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tagami J, Tao L, Pashley DH. Correlation among dentin depth, permeability, and bond strength of adhesive resins. Dent Mater. 1990;6:45–50. doi: 10.1016/0109-5641(90)90044-f. [DOI] [PubMed] [Google Scholar]
- 30.Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod. 2007;33:391–398. doi: 10.1016/j.joen.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ungor M, Onay EO, Orucoglu H. Push-out bond strengths: the Epiphany-Resilon endodontic obturation system compared with different pairings of Epiphany, Resilon, AH Plus and gutta-percha. Int Endod J. 2006;39:643–647. doi: 10.1111/j.1365-2591.2006.01132.x. [DOI] [PubMed] [Google Scholar]
- 32.Vasconcelos BC, Bernardes RA, Duarte MA, Bramante CM, Moraes IG. Apical sealing of root canal fillings performed with five different endodontic sealers: analysis by fluid filtration. J Appl Oral Sci. 2011;19:324–328. doi: 10.1590/S1678-77572011005000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu MK, Wesselink PR. Endodontic leakage studies reconsidered. Part I. Methodology, application and relevance. Int Endod J. 1993;26:37–43. doi: 10.1111/j.1365-2591.1993.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 34.Zicari F, Couthino E, De Munck J, Poitevin A, Scotti R, NaertI, et al. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater. 2008;24:967–977. doi: 10.1016/j.dental.2007.11.011. [DOI] [PubMed] [Google Scholar]