Abstract
Objective
Investigate whether body mass index (BMI), comorbidity, gender and age predict patient-reported functional limitation 2- and 5-years after Primary Total Knee Arthroplasty (TKA).
Methods
Overall moderate-severe activity limitation was defined as ≥2 activities (walking, stairs, rising chair) with moderate-severe limitation. Complete dependence on walking-aids or inability to walk was assessed (reference, no dependence). Multivariable logistic regressions were adjusted additionally for income, diagnosis, distance from medical center, ASA score and implant type.
Results
Overall moderate-severe activity limitation was reported by 20.7% at 2-years and 27.1% at 5-years. Significantly predictors of overall moderate-severe activity limitation 2-years post-TKA (odds (95% confidence interval)) were: BMI 30–34.9, 1.5 (1.0,2.0), 35–39.9, 1.8 (1.3,2.7) and ≥40, 3.0 (2.0,4.5) versus BMI≤25; higher Deyo-Charlson index, 1.7 (1.4,2.2) per 5-point increase; female gender, 2.0 (1.7,2.5); age 71–80, 2.1 (1.5,2.8) and age>80, 4.1 (2.7,6.1) versus age≤60.
At 5-years post-TKA, significant predictors of overall moderate-severe activity limitation were: BMI 35–39.9, 2.1 (1.4,3.3) and ≥40, 3.9 (2.3,6.5); higher Deyo-Charlson index, 1.4 (1.0,1.8); female gender, 2.2 (1.7,2.7); age 71–80, 2.4 (1.7,3.5) and age>80, 4.7 (2.8,7.9). Complete dependence on walking-aids was significantly higher at 2- and 5-years, respectively, in patients with: higher comorbidity, 2.3 (1.5,3.3) and 2.1 (1.4,3.2); female gender 2.4 (1.5,3.9) and1.7 (1.1,2.6); ;age 71–80, 1.6(1.03,2.5) and 2.1(1.2,3.4); and age >80, 3.2 (1.6,6.7) and 5.1 (2.3,11.0).
Conclusions
Modifiable (BMI, comorbidity) and non-modifiable predictors (age, gender) increased the risk of functional limitation and walking-aid dependence after primary TKA. Interventions targeting comorbidity and BMI pre-operatively may positively impact function post-TKA.
Keywords: Predictors, Functional Limitation, Total Knee Arthroplasty, Body Mass Index, Comorbidity, Gender, Age
INTRODUCTION
The 2003 NIH consensus statement [1] and a recent systematic review of Total Knee Arthroplasty (TKA) outcomes [2] concluded that age, gender and Body Mass Index (BMI) do not seem to significantly impact short-term outcomes following TKA. However, most studies that examined these relationships consisted of small sample sizes. Since poor outcomes after knee arthroplasty occur in <10% patients, sample sizes of 500 patients or less provide only 50 patients with outcomes of interest, which may not allow adjustment for important covariates/confounders. Examination of associations of these modifiable (BMI and comorbidity) and unmodifiable (gender and age) factors with functional outcome after TKA should be done with well-designed studies of large cohorts that can control for important covariates. This is important, since: (a) TKA is a common procedure –half a million procedures were performed in 2005 in the U.S. [3]; (b) The increase in proportion of older adults [4] and those with obesity [5] in the U.S. will have a major impact on volume of knee arthroplasty, which is projected to grow by 673% to 3.48 million by 2030 [3]; and (c) Suboptimal TKA outcomes can have a significant impact on patient satisfaction, medical costs and health care utilization. Knowing whether these factors are associated with functional outcomes can inform patients, surgeons and policy makers alike.
Published literature in this area can be summed up being contradictory and consisting of small sized studies that did not adjust for important covariates and confounders. Higher BMI was significantly associated with worse function outcomes in some studies [6–12] while other studies found no association [13–21] or association with stairs, but not walking distance [22]. BMI is of special interest, since it is modifiable and is a significant risk factor for osteoarthritis [23, 24] and for undergoing TKA [14]. Higher medical comorbidity was associated with poorer function in some studies [9, 16, 25], but not in others [7, 15, 17, 26, 27]. Age was associated with function in one study [9], but not in others [7, 15–17, 20, 26, 27]. Women were reported to have significantly worse [15, 28], or similar function compared to men [7, 9, 16, 17, 20, 26, 27]. Possible reasons for variation include using different outcome measures (Knee Society Scale (KSS) versus Western Ontario McMaster Arthritis Index (WOMAC) versus other measures), follow-up duration, sample sizes and controlling for different confounders. Due to contradictory results of previous results, more research is needed to examine if these factors are associated with functional outcomes.
We recently reported that female gender and younger age are significantly associated with more knee pain 2-years after primary TKA in a large cohort of patients [29]. In this study, using the same prospectively collected function data during clinical follow-up, we aimed at assessing impact of patient factors on 2- and 5-year function outcomes after primary TKA. We hypothesized that: (1) Higher pre-operative BMI and comorbidity will be independently associated with poorer function outcomes 2- and 5-years after primary TKA; (2) female gender and older age will be independently associated with worse function outcomes in this population.
METHODS
Data Sources and Study Cohort
The Mayo Clinic Total Joint registry, that has prospectively captured pain and function data from every patient who underwent a primary TKA at the Mayo Clinic since 1993, was used for this study. A validated knee questionnaire that included knee function questions [30] is mailed to the patients, administered during the clinic visit or by telephone at 2- and 5-year time-points after the TKA. The questions are similar to those in the Knee Society Score, the most widely used outcome instrument used in studies of TKA follow-up. For this study, a patient was included in the analyses if they had undergone a primary TKA between 1993 and 2005 (to allow for the 2-year questionnaire response) and had responded to at least one of the questionnaires at 2- or 5-year follow-up. We obtained additional variables of interest such as zip code and comorbidity using other institutional research databases.
Predictor Variables of Interest
BMI, comorbidity, gender and age were the four variables of interest. BMI was categorized as <25, 25–29.9, 30–34.9, 35–39.9, ≥40 [31]; categories <18.5 and 18.5–24.9 were collapsed into single category due to small numbers in <18.5 category. Comorbidity was assessed using validated Deyo-Charlson index [32], and treated as a continuous variable. The Deyo-Charlson index is the most commonly used comorbidity measure consisting of a weighted scale of 17 comorbidities (including cardiac, pulmonary, renal, hepatic disease, diabetes, cancer, HIV etc.), expressed as a summative score [33, 34]. Age was categorized as ≤60, 61–70, 71–80, >80, based on an a priori clinical decision by an experienced orthopedic surgeon (D.L.), similar to previous studies [14, 29]. The reference categories were, BMI <25, male gender and age ≤60, respectively. To test the robustness of our estimates, we also considered BMI and age as continuous variables in separate multivariable regression models.
Functional Outcomes
The outcomes of interest were function outcomes in patients with primary TKA at 2- and 5-years. We assessed this by:
- limitations of three key activities of daily living, including, distance walked, using stairs and rising from chair classified as follows:
- Distance walked: 'Unlimited’ or '> 10 blocks' = None; '5–10 blocks ' = Mild; '< 5 blocks '=Moderate; 'Housebound', 'Indoors only' or 'Unable' = Severe;
- Stairs: 'Normal Up and Down’=None; ‘'Normal Up, Down with Rail' = Mild; 'Up and Down with Rail' = Moderate; 'Up with Rail, Down Unable' OR 'Unable ' = Severe; and
- Rise from Chair: 'Able, no arms’ = None; 'Able, with Arms' = Mild; 'Able with difficulty' = Moderate; ' Unable ' = Severe.
overall limitation of activities: Overall limitation was defined as moderate/severe, if a patient had ≥2 activities (walking, stairs, rising chair) with moderate or severe limitation (reference, <2 limitations).
use of walking aids: The use of walking aids was categorized clinically as follows: ‘no aid’, ‘cane occasionally’ = no dependence; ‘cane full time’ = some dependence; ‘crutch’ ‘2 canes’, ‘2 crutches’, ‘walker’ or ‘unable to walk’ = complete dependence/unable.
We examined the association of predictors of interest with presence of moderate-severe limitation in overall activity (reference, <2 activities with limitation), walking, climbing stairs and rising from chair. For use of walking aids, the outcomes were some dependence (reference, no dependence) or complete dependence/unable (reference, no dependence). It is important to realize that medical comorbidity can impact these measures of function far more than TKA, which was one of the reasons to simultaneously adjust all models for comorbidity.
Covariates/confounders
The following variables were included in the multivariable regression analyses: (1) demographic: median annual household income (≤$35K, >$35K–$45K or >$45 K (reference category)) determined based on zip code and the median household income for geographical area using the census data for the respective year of survey; (2) American Society of Anesthesiologists Physical Status (ASA) score, a validated measure of peri- and post-operative outcomes, categorized as class I-II vs. III-IV [35, 36]; (3) Operative diagnosis: osteoarthritis, rheumatoid/inflammatory arthritis, or other (avascular necrosis, fracture etc.) for primary TKA; (4) distance from medical center (0–100 miles, >100–500 miles, >500 miles); and (5) implant type: cemented or uncemented/hybrid; and (6) pre-operative limitation in walking, climbing stairs and rising from a chair.
Statistical Analyses
Summary statistics (mean, standard deviation and percents) are presented for demographic and clinical characteristics of primary TKA cohorts at 2- and 5-years. The prevalence of moderate-severe overall functional limitation was compared between primary TKA at 2- and 5-years using chi-square tests.
All univariate and multivariable analyses were performed with logistic regression using a generalized estimating equations (GEE) approach to adjust the standard errors for the correlation between observations on the same subject due to replacement of both knees and/or multiple operations on the same knee. The primary variables of interest (BMI, comorbidity, gender and age) were assessed for association with moderate-severe limitation in the three activities (walking, climbing, and rising from a chair), moderate-severe overall limitation (defined as having a moderate-severe limitation in at least two of the three activities).
Univariate and multivariable associations with these same variables of interest with the outcome of use of aids (categorized as some dependence, complete dependence, and no dependence) were assessed using polychotomous logistic regression. Separate regression analyses were performed for primary TKA cohorts at 2- and 5-years. Each multivariable regression included BMI, comorbidity, gender, age, operative diagnosis, distance from medical center, income category, implant design (cemented versus uncemented/hybrid), pre-operative functional limitation and ASA score; Odds ratios with 95% confidence intervals are presented. A p≤0.05 was considered significant. Detailed univariate and multivariable-adjusted associations are presented in a tabular form in appendix 1 and 2 for the interested readers.
Since the outcomes may have changed over a 12-year period, due to changes in prostheses, peri-operative management and rehabilitation regimens, we performed sensitivity analyses by adjusting the main models for the year of surgery. Responder bias was examined with logistic regression, assessing the associations of demographic and clinical characteristics with completion of a follow-up questionnaire at 2- and 5-years post-TKA.
RESULTS
Cohort Characteristics
The baseline demographic and clinical characteristics of the cohort are described in Table 1. 7,139 primary TKA patients responded to the function survey at 2-years and 4,234 primary TKA patients at 5-years. The main analytic cohort consisted of patients who provided both pre- and 2-year data (n= 4,701) and pre- and 5-year data (n=2,935). There were no clinically meaningful differences in characteristics of responders at follow-up (2 or 5-years) and those that had both pre-operative and follow-up data (Table 1). The cohorts had a mean age of 68 years and consisted of nearly equal proportions of men and women; osteoarthritis was the commonest diagnosis for primary TKAs. The majority of patients (>85%) were overweight or obese, i.e., had BMI >25.
Table 1.
Demographic and clinical characteristics of study cohort
| Entire Cohort | Study cohort with both pre- and post- operative data |
|||
|---|---|---|---|---|
| 2-year (n=7,139) |
5-year (n=4,234) |
2-year (n=4,701) |
5-year (n=2,935) |
|
| Mean Age (±SD) | 68±10 | 68±10 | 68±10 | 68±10 |
| Men/Women (% | 44%/56% | 45%/55% | 44%/56% | 45%/55% |
| Age groups n (% | ||||
| ≤60 yrs | 18% | 18% | 18% | 17% |
| 61–70 yrs | 36% | 37% | 36% | 39% |
| 71–80 yrs | 38% | 38% | 38% | 38% |
| >80 yrs | 8% | 7% | 7% | 6% |
| Body Mass index (in kg/m2) | ||||
| ≤24.9 | 13% | 13% | 13% | 13% |
| 25–29.9 | 35% | 36% | 35% | 36% |
| 30–34.9 | 29% | 30% | 30% | 30% |
| 35–39.9 | 14% | 14% | 14% | 14% |
| ≥40 | 9% | 7% | 8% | 7% |
| ASA Score | ||||
| Class I–II | 58% | 59% | 59% | 60% |
| Class III–IV | 42% | 41% | 41% | 40% |
| Cemented | ||||
| Yes | 98% | 99.7% | 98% | 99.7% |
| Hybrid | 2% | 0.3% | 2% | 0.2% |
| Underlying Diagnoses | ||||
| Rheumatoid Arthritis/Other Inflammatory arthritis conditions | 4% | 4% | 3% | 4% |
| Osteoarthritis | 94% | 93% | 95% | 94% |
| Other | 2% | 3% | 2% | 2% |
Other category includes: avascular necrosis, fracture, neoplasms, Paget’s disease, septic arthritis etc.
Numbers rounded to the nearest digit and therefore may not add up to 100% precisely in all cases
Survey Responders and Non-responders
Of the 11,294 primary TKAs, 10,957 were eligible for 2-year follow-up, i.e. they were alive at 2 years post-surgery. Of these, 7137 (65%) had completed a 2-year questionnaire, with 4,701 (66%) of these having completed both preoperative and 2-year questionnaires. 7,404 were eligible for 5-year follow-up, with 4211 (57%) having completed 5-year questionnaires, with 2,935 (70%) having both preoperative and 5-year questionnaires.
Non-responders were slightly more likely to be younger, have higher ASA class, higher Charlson index, live more than 500 miles away from the medical center or have diagnoses other than osteoarthritis for primary TKA.
Prevalence of Moderate-Severe Overall Functional Limitation
The prevalence of overall moderate-severe limitations in walking, climbing stairs, rising from a chair and overall functional limitation (≥2 activities) decreased significantly from pre-operative to the 2-year and 5-year follow-up post-primary TKA (Table 2).
Table 2.
Prevalence of moderate-severe activity limitations pre- and post-primary TKA
| 2-year cohort | 5-year cohort | |||
|---|---|---|---|---|
| Pre-operative (%) | 2-year follow-up (%) | Pre-operative (%) | 5-year follow-up (%) | |
| Moderate-severe limitation in Walking | 69.7% | 24.2% | 70.2% | 32.6% |
| Stair-climbing | 84.6% | 39.1% | 84.0% | 43.5% |
| Rising from Chair | 28.6% | 7.2% | 30.2% | 9.7% |
| Overall activity | 68.4% | 20.7% | 68.7% | 27.1% |
Functional Outcomes 2-years after Primary TKA
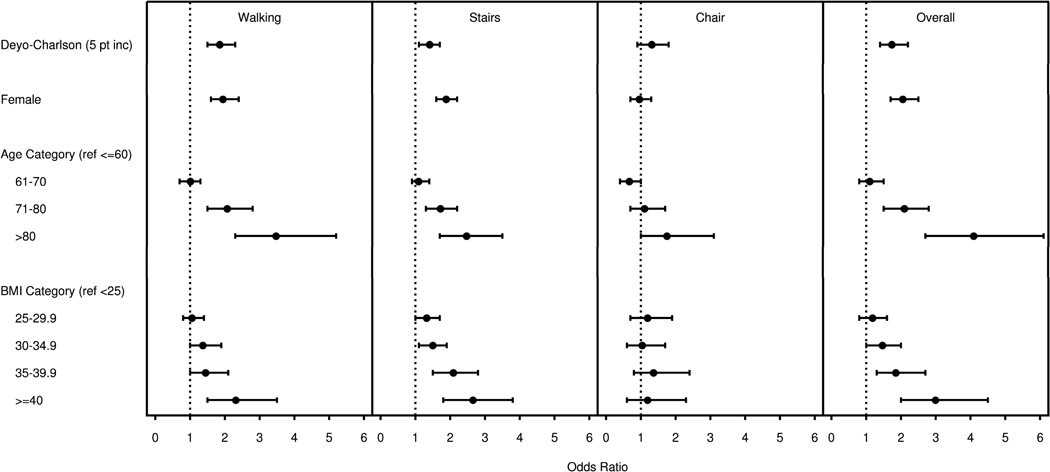
After multivariable adjustment, the significant predictors of overall moderate-severe activity limitation 2-years post-primary TKA included the following: BMI 30–34.9, 35–39.9, and ≥40, (reference, BMI≤25); higher Deyo-Charlson index; age 71–80 and age>80 (reference, age≤60); and female gender (Figure 1).
Figure 1. Multivariable-adjusted Odds ratio (95% confidence interval) for Moderate-Severe Limitations in Walking, Climbing Stairs, Rising from Chair and overall limitation at 2-years post-Primary TKA.
Each figure shows the odds ratio of moderate-severe limitation in each activity (walking, stairs, chair) and for overall limitation for each category of variable as compared to the respective reference category. Each logistic regression analyses for walking, stairs, chair and overall limitation was adjusted for age, gender, BMI, comorbidity, income, distance from medical center, ASA class, operative diagnosis and the type of implant. The dotted line represents an odds ratio of 1. Point estimates of odds ratios are represented by the solid circles; the whiskers represent the upper and lower 95% confidence interval estimates. Variables are significantly associated with the outcome in instances where the 95% confidence interval for the odds ratio does not cross one. For example, 5-point increase in Charlson index, female gender, age 71–80 and >80 and BMI, 30–34.9, 35–39.9 and ≥40 were associated with significantly increased odds of overall moderate-severe activity limitation.
Moderate-severe limitation in stair-climbing was significantly higher in the same groups as described for the overall activity limitation. Moderate-severe limitation in walking was significantly higher in BMI≥40, higher Deyo-Charlson index, age 71–80 and age >80 and female gender. None of the predictors of interest was significantly associated with moderate-severe limitation in rising from a chair (Figure 1).
Sensitivity analyses that adjusted for the year of surgery for analyses of outcomes at 2-years showed that all the factors found to be significant in the main analyses for 3 key activities and overall activity were still significant.
Functional Outcomes 5-years after Primary TKA
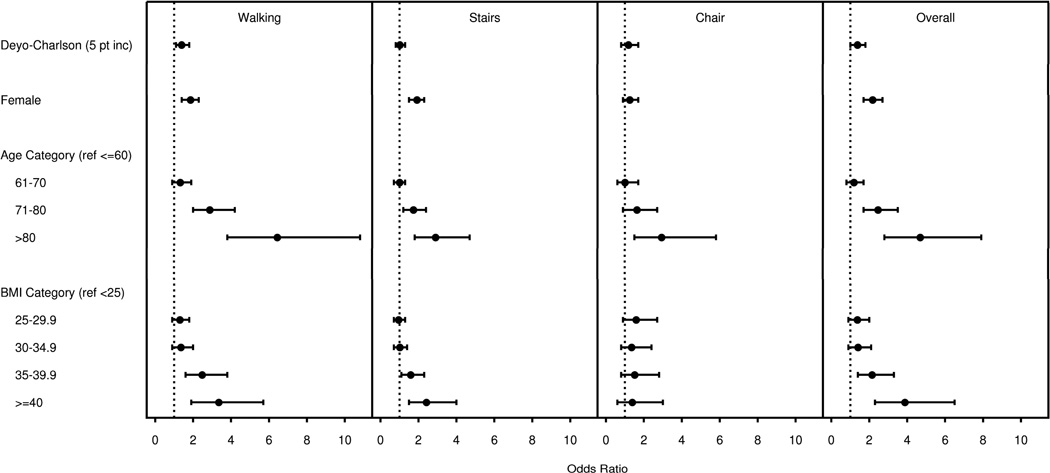
After multivariable adjustment, the significant predictors of overall moderate-severe activity limitation 5-years post-primary TKA included the following: BMI 35–39.9, and ≥40, (reference, BMI≤25); higher Deyo-Charlson index; age 71–80 and age>80 (reference, age≤60); and female gender (Figure 2).
Figure 2. Multivariable-adjusted Odds ratio (95% confidence interval) for Moderate-Severe Limitations in Walking, Climbing Stairs, Rising from Chair and overall limitation at 5-years post-Primary TKA.
Each figure shows the odds ratio of moderate-severe limitation in each activity (walking, stairs, chair) and for overall limitation. Each logistic regression analyses for walking, stairs and chair limitation was adjusted for age, gender, BMI, comorbidity, income, distance from medical center, ASA class, operative diagnosis and the type of implant.
Moderate-severe limitation in walking was significantly higher in the same groups as described for the overall activity limitation. Moderate-severe limitation in stair-climbing was also significantly higher in same groups as for the overall activity limitation, except that Deyo-Charlson index was not significantly associated (Figure 2). Moderate-severe limitation in rising from a chair was significantly higher in patients aged >80 years (Figure 2).
Sensitivity analyses adjusting for the year of surgery showed that all the predictors significant in the main analyses at 5-years were still significant in this new model with one exception- the association of age >80 with stair-climbing was no longer significant.
Use of Walking Aids
In a polychotomous regression model, BMI was not associated with higher odds of dependence on walking aids at 2- or 5-years (Table 3). Higher comorbidity, as indicated by higher Deyo-Charlson index, was associated with significantly higher odds for some dependence and complete dependence on walking aids at 2-years, (OR, 1.6 and 2.3, respectively) and higher odds of complete dependence at 5-years. Female gender was associated with increased odds for complete dependence on walking aids compared to men at 2- and 5-years (OR, 2.8 and 2.2). Age 61–70 was associated with higher odds of some dependence on walking aids at 2-years, age 71–80 with higher odds of some dependence on walking aids at 2- and 5-years and age>80 with higher odds of walking aid dependence, both some and complete at both 2- and 5-years.
Table 3.
Multiavvriable-adjusted association of BMI, comorbidity, gender and age with dependence on walking aids
| 2-year primary TKA | 5--year primary TKA | |||||||
|---|---|---|---|---|---|---|---|---|
| Some dependence (n=161/3,063) |
p-value | Complete Dependence/ unable (n=113/2,063) |
p-value | Some dependence (n=113/1,879) |
p-value | Complete Dependence/ unable (n=128/1,879) |
p-value | |
| BMI (Ref, <25 kg/m2) | ||||||||
| 25–29.9 | 0.8 (0.5,1.3) | 0.38 | 1.1 (0.6,2.1) | 0.75 | 0.6 (0.4,1.1) | 0.13 | 0.9 (0.4,1.6) | 0.63 |
| 30–34.9 | 1.2 (0.7,2.0) | 0.59 | 0.7 (0.4,1.5) | 0.41 | 0.8 (0.4,1.5) | 0.46 | 1.1 (0.5,2.1) | 0.86 |
| 35–39.9 | 1.2 (0.6,2.2) | 0.62 | 1.7 (0.8,3.6) | 0.13 | 1.2 (0.6,2.3) | 0.64 | 1.0 (0.5,2.3) | 0.92 |
| ≥40 | 1.9 (0.9,3.8) | 0.07 | 1.6 (0.7,3.6) | 0.28 | 1.7 (0.8,3.8) | 0.19 | 2.0 (0.8,4.7) | 0.12 |
| Deyo-Charlson index (5-point change) | 1.6 (1.1,2.3) | <0.01 | 2.3 (1.5,3.3) | <0.01 | 1.1 (0.7,1.7) | 0.74 | 2.1 (1.4,3.2) | <0.01 |
| Female Gender (Ref, Male) | 1.3 (0.9,1.9) | 0.11 | 2.4 (1.5,3.9) | <0.01 | 1.5 (1.0,2.3) | 0.05 | 1.7 (1.1,2.6) | 0.02 |
| Age (Ref, ≤60 yrs) | ||||||||
| 61–70 | 2.8 (1.3,5.9) | <.01 | 0.5 (0.3,1.0) | 0.05 | 1.3 (0.6,2.7) | 0.44 | 0.5 (0.3,1.0) | 0.07 |
| 71–80 | 4.3 (2.0,9.2) | <.01 | 1.4 (0.8,2.6) | 0.23 | 2.9 (1.4,5.8) | <.01 | 1.5 (0.8,2.8) | 0.24 |
| >80 | 13.2 (5.7,30.3) | <.01 | 3.2 (1.6,6.7) | <.01 | 7.7 (3.3,17.8) | <.01 | 5.1 (2.3,11.0) | <.01 |
P<0.05;
p≤0.01,
p≤0.001; All other p-values are ≥0.05, unless indicated as above; Significant odds ratios are in bold
Multivariable model adjusted for: gender, age, Deyo-Charlson index, BMI, ASA score, distance from medical center, operative diagnosis, type of implant (cemented, uncemented, hybrid), income category and pre-operative overall limitations
DISCUSSION
Our study, that included the largest U.S. cohort of primary TKA patients to-date, found that BMI, comorbidity, female gender and older age significantly impact functional outcomes at 2- and 5-years after primary TKA, even after adjustment for pre-operative function and several other patient and surgical risk factors. We noted that at both 2- and 5-years post-primary TKA, several patient-level factors were consistently associated with higher risk of moderate-severe limitation in walking, climbing stairs and overall activity (no significant associations noted for rising from chair). These included BMI ≥40, higher Deyo-Charlson index, age>70 and female gender. Sensitivity analyses that adjusted for the year of surgery did not change any of these associations significantly, confirming the robustness of our findings. Dependence on walking aids was also significantly higher in women, older patients and in those with higher comorbidity, as indicated by a higher Deyo-Charlson index. The observation that almost same factors predict moderate-severe activity limitation at 2-year and 5-year follow-up and walking-aids dependence is important and adds to the literature.
Strengths and Limitations
Our study analyzed functional limitation in one of the largest U.S. cohort of primary TKA patients, adjusted for multiple confounders (socio-demographic, clinical and implant) and provided robust estimates as evident from the similarity of 2- and 5-year odds ratios and sensitivity analyses. There are several limitations to our study. Residual confounding due to variables not measured in this study such depression, involvement of other joints and quadriceps weakness is possible. These and other non-TKA conditions can impact the functional outcomes assessed in our study, since these limitation are not unique/specific to TKA. Non-response bias, referral bias and single-center study limits the generalizability to other populations. The non-responders were more likely to have higher comorbidity which would bias our results towards null, but the younger age of non-responders would bias our results away from the null. Therefore the exact direction of bias is unclear. A 100% follow-up is desirable, but we doubt that a response rate greater than 65% (reported in this study) is practically possible for a 13-year cohort study that included every patient operated upon in a large practice. Our response rate is higher than the average 60% response rate reported for mailed surveys of this size [37]. Only half of the cohort with 2- or 5-year data had pre-operative data on function, an important predictor of post-operative function outcomes [16, 26], that could not be included in multivariable models due to risk of further bias. We think that a prospective multi-center cohort is needed to avoid many study limitations. Such a study can also provide data on longer-term outcomes.
BMI and Functional Limitation
The positive association of BMI ≥40 kg/m2 with limitations in walking, stair climbing and overall activity is an important finding of this study (BMI, 30–35 was associated with some limitations). We studied not only the limitation of three key activities, but also overall activity and use of walking aids. Major limitations of previous studies were small sample size and dichotomization oft BMI with two exceptions- one small study examined >2 BMI categories [19] and one study had <200 patients [13]. Previous studies showed a positive association of higher BMI with worse outcomes [6–12] or no association [13–21]. Our study findings support the hypothesis that only very high BMI (≥40, or in some cases 35–40) is a risk factor for poor functional outcomes after primary TKA. By providing estimates of functional limitation for all BMI categories, our study adds significantly to the literature.
Based on these findings, the surgeons can inform patients with BMI higher than 35 and 40 regarding their risk of sub-optimal functional outcomes. This will allow patients to have realistic expectations regarding their outcomes. Second, a weight reduction program before undergoing TKA may improve the outcomes in those with very high BMI, an important hypothesis that needs to be tested. These findings are important, since obesity is a modifiable known risk factor for TKA [14] and its prevalence is increasing in the U.S. [5].
Higher Comorbidity and Function
Higher comorbidity was associated with poorer function outcomes and walking aids dependency at 2- and 5-years post-primary TKA. Our findings confirm previous similar findings in patients with primary TKA [9, 16, 25], but are in contrast to other studies [7, 15, 17, 26, 27]. Findings that diabetes and hypertension are associated with higher post-arthroplasty complication rates [38] indicates that at least some functional limitation associated with comorbidity may result from higher post-operative complication rates in patients with higher comorbidity load. Further studies are needed, to examine if optimizing comorbidity treatment prior to TKA can improve function outcomes.
Gender and Age Associations
Women had poorer function and higher dependence on walking aids at both 2- and 5-years post-primary TKA, even after adjustment for preoperative functional limitation, demographics and comorbidity compared to men. Our study raises the awareness of the association of gender with functional outcomes. However, our study was not designed to address the debate as to whether use of gender-specific implants impacts functional outcomes in female patients [39]. Our findings of higher functional limitation in patients older than 70 years (relative to <60) undergoing primary TKA are similar to significantly greater functional decline in the ability of adults >75 years in performing basic activities of daily living in a national sample [40]. These age and gender associations add to our recent findings of associations of age and gender with moderate-severe pain 2- and 5-years post-TKA [29].
In conclusion, we found that higher BMI, comorbidity, older age and female gender were independently associated with functional outcomes 2- and 5-year after primary TKA. These factors are also significantly associated with dependence on walking aids. It is possible that strategies focused at reducing obesity and treating comorbid conditions more effectively prior to TKA may improve functional outcomes following TKA. Surgeons can risk-stratify patients based on these characteristics and better inform patients about expected outcomes, thus reducing the gap between patient expectations and outcomes.
Supplementary Material
ACKNOWELGEMENTS
We thank Youlonda Lochler of the Mayo Clinic for assistance in data extraction and programming and Ruth Brady, Amy Anderson and Perlita Ochoa of the Minneapolis VA medical center for their administrative assistance.
Grant support: NIH CTSA Award 1 KL2 RR024151-01 (Mayo Clinic Center for Clinical and Translational Research) and the Department of Orthopedic Surgery, Mayo Clinic School of Medicine, Rochester, MN.
Footnotes
Financial Conflict: One of the authors (DL) has received royalties/speaker fees from Zimmer, has been a paid consultant to Zimmer and has received institutional research funds from DePuy, Stryker and Zimmer.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
REFERENCES
- 1.NIH Consensus Statement on total knee replacement December 8–10, 2003. J Bone Joint Surg Am. 2004;86-A:1328–1335. doi: 10.2106/00004623-200406000-00031. [DOI] [PubMed] [Google Scholar]
- 2.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1719–1724. doi: 10.2106/JBJS.D.02714. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 4.CDC. Public Health and Aging: Trends in Aging --- United States and Worldwide Mortality and Morbidity Weekly Report. 2003 Feb 14;52:101–106. [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 6.Amin AK, Clayton RA, Patton JT, Gaston M, Cook RE, Brenkel IJ. Total knee replacement in morbidly obese patients. Results of a prospective, matched study. J Bone Joint Surg Br. 2006;88:1321–1326. doi: 10.1302/0301-620X.88B10.17697. [DOI] [PubMed] [Google Scholar]
- 7.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Krushell RJ, Fingeroth RJ. Primary Total Knee Arthroplasty in Morbidly Obese Patients: a 5- to 14-year follow-up study. J Arthroplasty. 2007;22:77–80. doi: 10.1016/j.arth.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86-A:2179–2186. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Naylor JM, Harmer AR, Heard RC. Severe other joint disease and obesity independently influence recovery after joint replacement surgery: an observational study. Aust J Physiother. 2008;54:57–64. doi: 10.1016/s0004-9514(08)70067-9. [DOI] [PubMed] [Google Scholar]
- 11.Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am. 2004;86-A:1609–1615. doi: 10.2106/00004623-200408000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998;80:1770–1774. doi: 10.2106/00004623-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006;88:335–340. doi: 10.1302/0301-620X.88B3.16488. [DOI] [PubMed] [Google Scholar]
- 14.Bourne R, Mukhi S, Zhu N, Keresteci M, Marin M. Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res. 2007;465:185–188. doi: 10.1097/BLO.0b013e3181576035. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L, et al. Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum. 2004;51:100–109. doi: 10.1002/art.20090. [DOI] [PubMed] [Google Scholar]
- 16.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161:454–460. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 17.Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Ther. 2003;83:696–706. [PubMed] [Google Scholar]
- 18.Naal FD, Neuerburg C, Salzmann GM, Kriner M, von Knoch F, Preiss S, et al. Association of body mass index and clinical outcome 2 years after unicompartmental knee arthroplasty. Arch Orthop Trauma Surg. 2008 doi: 10.1007/s00402-008-0633-7. [DOI] [PubMed] [Google Scholar]
- 19.Nunez M, Nunez E, Segur JM, Macule F, Sanchez A, Hernandez MV, et al. Health-related quality of life and costs in patients with osteoarthritis on waiting list for total knee replacement. Osteoarthritis Cartilage. 2007;15:258–265. doi: 10.1016/j.joca.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Sharma L, Sinacore J, Daugherty C, Kuesis DT, Stulberg SD, Lewis M, et al. Prognostic factors for functional outcome of total knee replacement: a prospective study. J Gerontol A Biol Sci Med Sci. 1996;51:M152–M157. doi: 10.1093/gerona/51a.4.m152. [DOI] [PubMed] [Google Scholar]
- 21.Spicer DD, Pomeroy DL, Badenhausen WE, Schaper LA, Jr, Curry JI, Suthers KE, et al. Body mass index as a predictor of outcome in total knee replacement. Int Orthop. 2001;25:246–249. doi: 10.1007/s002640100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffin FM, Scuderi GR, Insall JN, Colizza W. Total knee arthroplasty in patients who were obese with 10 years followup. Clin Orthop Relat Res. 1998:28–33. doi: 10.1097/00003086-199811000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 24.Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford Study. J Rheumatol. 1993;20:331–335. [PubMed] [Google Scholar]
- 25.Wasielewski RC, Weed H, Prezioso C, Nicholson C, Puri RD. Patient comorbidity: relationship to outcomes of total knee arthroplasty. Clin Orthop Relat Res. 1998:85–92. [PubMed] [Google Scholar]
- 26.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–1728. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD. Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty. 2006;21:559–566. doi: 10.1016/j.arth.2005.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ritter MA, Lutgring JD, Davis KE, Berend ME. The effect of postoperative range of motion on functional activities after posterior cruciate-retaining total knee arthroplasty. J Bone Joint Surg Am. 2008;90:777–784. doi: 10.2106/JBJS.F.01022. [DOI] [PubMed] [Google Scholar]
- 29.Singh JA, Gabriel S, Lewallen D. The impact of gender, age, preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466:2717–2723. doi: 10.1007/s11999-008-0399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGrory BJ, Morrey BF, Rand JA, Ilstrup DM. Correlation of patient questionnaire responses and physician history in grading clinical outcome following hip and knee arthroplasty. A prospective study of 201 joint arthroplasties. J Arthroplasty. 1996;11:47–57. doi: 10.1016/s0883-5403(96)80160-4. [DOI] [PubMed] [Google Scholar]
- 31.WHO. Obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 32.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 33.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 34.Charlson ME, Sax FL, MacKenzie CR, Braham RL, Fields SD, Douglas RG., Jr Morbidity during hospitalization: can we predict it? J Chronic Dis. 1987;40:705–712. doi: 10.1016/0021-9681(87)90107-x. [DOI] [PubMed] [Google Scholar]
- 35.Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA. 1961;178:261–266. doi: 10.1001/jama.1961.03040420001001. [DOI] [PubMed] [Google Scholar]
- 36.Weaver F, Hynes D, Hopkinson W, Wixson R, Khuri S, Daley J, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty. 2003;18:693–708. doi: 10.1016/s0883-5403(03)00259-6. [DOI] [PubMed] [Google Scholar]
- 37.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 38.Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005:232–238. doi: 10.1097/01.blo.0000156479.97488.a2. [DOI] [PubMed] [Google Scholar]
- 39.Barrett WP. The need for gender-specific prostheses in TKA: does size make a difference? Orthopedics. 2006;29:S53–S55. [PubMed] [Google Scholar]
- 40.Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52:1274–1282. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.