Abstract
Objective
Prostate cancer negatively influences quality of life (QOL) in survivors and the people with whom they are close. The purpose of this investigation was to assess the degree of dyadic interdependence in psychological QOL in dyads adjusting to prostate cancer and its treatment.
Method
Participants were 70 prostate cancer survivors and their partners, most of whom were spouses. Assessments of psychological QOL (i.e., depression, anxiety, fatigue, and positive affect) were made at three points in time, each separated by 8 weeks.
Results
Survivors’ prostate specific function was associated with both their own and their partners’ psychological QOL. There was evidence of longitudinal dyadic interdependence for psychological QOL, particularly from partners to survivors between the T2 and T3 assessments.
Conclusions
Prostate cancer survivors’ psychological QOL is affected substantially by their partners’ psychological QOL, consistent with theories of emotional contagion.
Keywords: prostate cancer, quality of life, psychological distress, emotional contagion
Prostate cancer is the most commonly diagnosed cancer in men. Although the death rate from prostate cancer continues to decline, the incidence of prostate cancer is increasing, due in part to improved screening. With early diagnosis prostate cancer is highly treatable, but men with prostate cancer often experience troublesome side effects associated with treatment that negatively influence their quality of life (QOL) (Penson, Litwin, & Aaronson, 2003).
Side effects associated with prostate cancer treatment include urinary incontinence, erectile dysfunction, loss of libido, fatigue, and hot flashes (Stanford et al., 2000). Sexual dysfunction after treatment for prostate cancer is particularly associated with psychological distress in survivors (Wootten et al., 2007). Fatigue is experienced at some point in time by most men treated for prostate cancer (Danjoux, Gardner, & Fitch, 2007). This constellation of side effects contributes to significant psychological distress that is experienced by at least one third of men with prostate cancer (Balderson & Towell, 2003). Between 25–50% of men have substantial problems with anxiety and associated feelings of nervousness and worrying associated with prostate cancer (Korfage, Essink-Bot, Janssens, Schroder, & de Koning, 2006; Mehnert, Lehmann, Schulte, & Koch, 2007). Although some treatments for prostate cancer are associated with unique side effects, problems such as depression, anxiety, and fatigue appear with comparable frequency in survivors across a range of different treatment modalities (Harrington, Hansen, Moskowitz, Todd, & Feuerstein, 2010; Maliski, Kwan, Elashoff, & Litwin, 2008; Steineck et al., 2002). In some cancer survivors, psychological distress can persist for periods as long as 1 to 10 years (Harrington et al., 2010; Traeger et al., 2009). In addition, prostate cancer often occurs later in life when other comorbid health conditions occur that further complicate health related QOL (Karakiewicz et al., 2008).
The psychological distress that often accompanies prostate cancer and interferes with QOL is not just experienced by cancer survivors themselves. The effects of cancer and its treatment can cause dramatic changes in relationships, roles, and psychological health for survivors as well as their partners and family members. Partners of men with prostate cancer report a major decline in the family’s overall QOL after diagnosis (Mellon & Northouse, 2001). Wives of men with prostate cancer often experience anxiety, stress, depression, and uncertainty along with the physical symptoms that accompany such emotions (Aranda & Hayman-White, 2001; Garos, Kluck, & Aronoff, 2007). These problems are especially pronounced during advanced stages of prostate cancer (Northouse et al., 2007). In some cases spouses of men treated for prostate cancer report higher levels of distress than the men themselves (Eton, Lepore, & Helgeson, 2005). Factors such as low self-esteem, less positive coping strategies, lower marital quality, and dysfunctional problem-solving increase the risk of distress in spouses of men with prostate cancer (Eton et al., 2005; Ko et al., 2005).
Many of the prostate specific functional impairments that are often experienced by men undergoing prostate cancer treatment such as urinary, bowel, and sexual dysfunction can be distressing to their partners (Eton et al., 2005; Ezer et al., 2006; Sanda et al., 2008) just as they are to survivors themselves. Although problems such as sexual dysfunction have obvious implications for intimate partners’ QOL, urinary and bowel problems could also affect the QOL of other supportive partners who provide care and assistance to survivors (e.g., laundry, running errands). Such effects provide some explanation for how and why prostate cancer survivors and their partners experience interdependent QOL.
Research on the psychological QOL of cancer survivors and their supportive partners has significant implications for understanding theories of emotional contagion. Emotional contagion is at least one mechanism that could create dyadic interdependence in psychological QOL indicators among prostate cancer survivors and their partners. According to the emotional contagion hypothesis, people catch the intense emotional states of those with whom they interact through largely unconscious interpersonal processes (Hatfield, Cacioppo, & Rapson, 1992, 1994). Emotional contagion theorists observe that people will mimic and synchronize their nonverbal behaviors with those of the people around them. This similarity in behavior is theorized to provide feedback that generates the same emotional experience as those people whose behaviors are being observed and matched. Social comparison processes have also been advanced as an explanation for emotional contagion (Epstude & Mussweiler, 2009). An important implication of the social comparison effect is that similarly between the actor and observer is theorized to increase the likelihood of emotional contagion. This suggests for example that emotional contagion could be particularly likely in marital and other close relationships where people share numerous similarities (Goodman & Shippy, 2002).
Cancer survivors and their supportive partners represent a useful context for testing emotional contagion effects. As previously noted, similarity would be expected to be higher than average in these close relationships, enhancing the probability of emotional contagion. Further, members of these dyads are coping with a common stressor. Encountering a common threat has been shown to increase emotional contagion (Gump & Kulik, 1997). It is therefore understandable why meta-analytic evidence shows a correlation between cancer survivors’ and their spouses’ distress, although this effect appears strongest when the survivor is female (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne, 2008), and why family members and intimate partners often experience the same or higher levels of emotional distress (e.g., depression, anxiety) as cancer survivors (Manne et al., 2007; Rabin et al., 2009).
There is reason to believe that the psychological distress of cancer patients is related to that of their partners or immediate family members. When advanced cancer patients meet the criteria for psychiatric disorder, their caregivers, 75% of whom were spouses, were 7.9 times more likely to meet the criteria as well, and vice versa (Bambauer et al., 2006). This increased odds ratio was based on concurrent data, but controlled for demographic characteristics and lifetime psychiatric disorders in patients. In women with breast cancer and their supportive partners, 63% of whom were spouses, the psychological distress of one partner predicts the subsequent distress of the other (Segrin, Badger, Dorros, Meek, & Lopez, 2007; Segrin et al., 2005). These dyadic effects were demonstrated over two 6-week intervals, controlling for prior psychological distress in the survivor and partner, as well as preexisting dyadic interdependence in distress at baseline. Surprisingly, results for the Segrin et al. investigations showed that the direction of influence is more commonly from the partner to the survivor. In other words, partners’ psychological distress predicts subsequent psychological distress in survivors.
Studies of dyadic interdependence in psychological distress and QOL associated with breast cancer most often measure psychological distress in female survivors and male partners. In dyads where one member has cancer or some other serious illness, there are commonly sex differences such that women, be they patients or caregivers, report more psychological distress than men (Hagedoorn et al., 2008; Thompson et al., 2004). Accordingly, it may be possible that psychological distress is more easily transmitted to women than it is to men, regardless of their role in the dyad (i.e., patient or partner). Studying dyadic interdependence in the context of prostate cancer allows for an examination of the potential transmission of psychological distress within the dyad, in a context where gender roles are reversed in comparison to dyads coping with breast cancer.
The primary aim of this investigation is to examine the extent to which there is dyadic interdependence in psychological distress within dyads coping with prostate cancer and its treatment. In the present study, dyadic interdependence in psychological QOL was examined in two ways. First, we assessed the association between prostate specific health related QOL issues (e.g., urinary functioning, sexual functioning) in survivors and psychological QOL in their partners. Although these elements of QOL would certainly be expected to predict psychological distress in prostate cancer survivors, the extent to which they are related to the distress of survivors’ partners is less certain. Second, we tested for dyadic interdependence in psychological distress longitudinally, in dyads participating in a 3-wave longitudinal study of 16 weeks duration. These analyses allow for a stringent test of the extent to which one dyad member’s psychological distress influences that of the other dyad member as they cope with and adjust to prostate cancer and its treatment related side effects. In this investigation, psychological QOL was operationalized with a variety of indicators that reflect the type of psychological (depression, anxiety) and somatic (fatigue) distress that is commonly experienced by cancer patients. In addition, we included a measure of positive affect, as psychological QOL entails more than the mere absence of negative states, but the experience of positive emotions as well.
Method
Participants
The participants were 70 men with prostate cancer, hereafter referred to as “survivors,” and one of their immediate social network members, hereafter referred to as “partners,” who were participating in a larger investigation of psychosocial interventions for cancer survivors and their partners (Badger et al., 2011). Survivors had a mean age of 66.67 years (SD = 9.29), and were 84% White, 9% Black, and 7% Latino. Their highest level of formal education completed was 13% high school, 29% vocational/ technical school or some college, 34% college, and 24% held a postgraduate/professional degree. The majority of the survivors were retired (70%) and currently married (79%). In terms of illness characteristics, among those who knew their disease stage (n = 40), 36% had Stage 1, 19% Stage 2, 19% Stage 3, and 26% Stage 4 cancer. Survivors reported a mean Gleason score of 6.33 (SD = 1.63). The Gleason score is a metric for tumor grading ranging from 2–10, where 10 represents the most aggressive tumor and the poorest prognosis. They were on average 187 weeks (SD = 259) from initial diagnosis (5% trimmed M = 155 weeks), reflecting the fact that prostate cancer is a disease that often progresses very slowly, and that survivorship can be experienced for many years. The treatments experienced by survivors included chemotherapy (14%), radiation (56%), hormone blocking therapy (42%), surgery (39%), complementary/alternative medicine (4%), and watchful waiting (10%). These values add up to >100% because many survivors experienced multiple treatments. It is noteworthy that 30% of the survivors had undergone a prostatectomy in the course of their treatment. There were 49 men in the sample who were in some form of active treatment at the time of baseline assessment. For purposes of this investigation, watchful waiting was considered a form of treatment. All of the survivors listed at least one other chronic illness, with an average of 1.82 (SD = 1.50) illnesses and 4.64 (SD = 3.70) medications.
The partners were 94% female and 6% male, with a mean age of 61.13 years (SD = 10.94). The partners were 81% White, 9% Black, 4% Latina/o, 3% Asian/Pacific Islander, 2% American Indian/Alaskan Native, and 1% other. The highest level of education completed by partners was 1% middle school, 17% high school, 29% vocational/technical school or some college, 31% college, and 21% held a postgraduate/professional degree. Most partners were either retired (46%) or working full time (46%), and most (81%) were currently married. The relationship between the partner and survivor was spouse/significant other in most cases (83%), followed by friend/other (10%), sibling (4%), and son/ daughter (3%).
Procedures
Prostate cancer survivors and their partners were recruited from regional cancer centers, regional Veterans’ Affairs Heath Care Centers, cancer support groups, and from research study websites through which interested individuals could volunteer to enroll. Eligibility criteria included a diagnosis of prostate cancer, currently undergoing or had completed treatment within the past 6 months, ability to speak English, no physical or psychological disabilities that would prevent participating in the interventions, and availability of a social network member who was willing to participate in the investigation. The partner could be anyone within the survivor’s social network whom he felt was significant to his recovery. Although most men selected spouses, they were not restricted to spouses given that some men were widowed, divorced, single, or had spouses unable to participate (e.g., spouse too ill).
Upon enrollment in the study, each dyad was randomly assigned to one of two intervention conditions. One intervention was a telephone delivered interpersonal counseling intervention and the other was a telephone delivered health education intervention. Details of these interventions and their effects have been presented elsewhere (Badger et al., 2011) and only those details relevant to the current report are presented here.
All participants completed baseline assessments over the telephone, conducted by a trained data collector that included the instruments described here plus others not relevant to the present report. Separate calls were made to the survivor and partner for all intervention sessions and assessments at times that were convenient for the individual. Following baseline assessment, all survivors received 8 weekly phone calls and their partners received four calls, one every other week, as part of the interventions. Participants completed the second (T2) assessment (T1 + 8 weeks) within the week of their final intervention session, and the third and final assessment (T3) 8 weeks later (T2 + 8 weeks), for a total of 16 weeks from T1 to T3. The T2–T3 interval of 8 weeks was selected to mirror the duration of the T1–T2 interval. After each assessment, participants were sent a $10 gift card from a local retail merchant to thank them for their time.
At T1, 70 prostate cancer survivors and their partners completed the baseline assessments, and by T2, five survivors and their partners withdrew from the study (T1–T2 attrition rate = 7%). By T3, an additional two dyads were lost to follow-up because they declined to complete the T3 assessment (T1–T3 attrition = 10%). There were no significant differences for demographic or illness characteristics between those that discontinued and those that completed the study.
Measures
Symptoms of depression
Depressive symptoms were measured using the 20-item Center for Epidemiological Studies-Depression Scale (CES-D) (Radloff, 1977). Scores range from 0 to 60. Cronbach’s alphas were .88, .91, and .95 at T1, T2, and T3 for survivors. Corresponding reliabilities for partners were .89, .91, and .92. Because of a positive skew in the distribution of depression scores, this variable was square root transformed before all subsequent analyses.
Anxiety
The State version of the State-Trait Anxiety inventory was administered to assess current levels of anxiety (STAI) (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). The STAI is a 20-item instrument with a scale range of 20 to 80 that includes items such as “I feel anxious” and “I am worried.” The state version of the instrument asks respondents to focus on how they feel “right now, that is, at this present moment.” Cronbach’s alphas were .94, .95, and .95 at T1, T2, and T3 for survivors. Corresponding reliabilities for partners were .94, .93, and .96.
Fatigue
Participants completed the 20-item Multidimensional Fatigue Inventory (MFI) (Smets, Garssen, Bonke, & De Haes, 1995) as an index of their current experience of fatigue. The MFI assesses general fatigue, physical fatigue, mental fatigue, reduced motivation, and reduced activity and scores on these dimensions can be summed to form a composite index of fatigue. In this analysis, we combined the subscales of the MFI to form a global measure of fatigue with Cronbach’s alphas of .93, .95, and .96 for survivors at T1–T3, respectively. Corresponding reliabilities for partners were .89, .93, and .94.
Positive affect
Participants completed the 10-item positive affect subscale of the Positive and Negative Affect Schedule (PANAS) (Watson, Clark, & Tellegen, 1988). Scores range from 10 to 50, with high scores reflecting higher levels of positive affect. Sample positive affect items include “interested” and “inspired.” Cronbach’s alphas were .87, .88, and .89 for survivors at T1–T3, respectively. Corresponding alphas for partners were .87, .88, and .90.
Prostate specific health related QOL
Prostate cancer survivors completed a shortened version of the UCLA Prostate Cancer Index (PCI) (Litwin et al., 1998) to assess their prostate specific health related QOL at the baseline assessment. For this investigation, participants completed urinary, bowl, and sexual functioning subscales that were also combined to form a global index. For each of the three dimensions of functioning, respondents were asked to rate their functioning over the past 4 weeks in addition to specific problems associated with that function. The PCI is scaled such that high scores indicate better functioning. The reliability of the PCI in this sample was α = .74.
Results
A correlation matrix along with means and standard deviations for all survivor and partner QOL variables appear in Table 1. At the baseline assessment, before either intervention began, survivors completed the PCI that is a measure of prostate specific QOL. To determine the extent to which prostate specific QOL was associated with survivors’ psychological QOL (i.e., depression, anxiety, fatigue, and positive affect), each of the PCI subscales, along with the total score, were correlated with each measure of psychological QOL in survivors. Results of these analyses appear on the top of Table 2 and show uniform associations such that the better survivors’ prostate specific QOL, the better their reported psychological QOL, as would be expected.
Table 1.
Intercorrelations, Means, and SDs for Survivor and Partner QOL Variables at T1–T3 (Depression, Anxiety, Fatigue, Positive Affect)
| T1 | ||||
| Depression | — | .60 | .51 | −.41 |
| Anxiety | .71 | — | .44 | −.43 |
| Fatigue | .77 | .57 | — | −.57 |
| Positive affect | −.61 | −.54 | −.63 | — |
| T2 | ||||
| Depression | — | .76 | .77 | −.61 |
| Anxiety | .74 | — | .70 | −.51 |
| Fatigue | .75 | .58 | — | −.64 |
| Positive affect | −.58 | −.62 | −.69 | — |
| T3 | ||||
| Depression | — | .66 | .77 | −.62 |
| Anxiety | .77 | — | .62 | −.52 |
| Fatigue | .77 | .58 | — | −.69 |
| Positive affect | −.73 | −.57 | −.75 | — |
| T1 M (SD) S | 11.92 (9.27) | 32.46 (10.87) | 27.46 (16.53) | 35.90 (7.02) |
| T2 M (SD) S | 10.23 (9.45) | 30.44 (11.17) | 25.81 (18.21) | 37.27 (6.96) |
| T3 M (SD) S | 10.38 (11.90) | 30.83 (11.65) | 24.33 (19.23) | 36.65 (7.66) |
| T1 M (SD) P | 12.59 (9.90) | 32.40 (10.59) | 23.50 (12.75) | 35.99 (7.46) |
| T2 M (SD) P | 9.94 (9.24) | 31.22 (9.89) | 23.33 (15.49) | 37.48 (6.83) |
| T3 M (SD) P | 9.88 (9.40) | 31.40 (11.95) | 23.48 (16.48) | 36.98 (7.21) |
Note. All correlations are statistically significant at p < .05. Coefficients above each diagonal correspond to partners, and coefficients below each diagonal to survivors. S = Survivor; P = Partner.
Table 2.
Correlations Between Survivor Prostate Specific Functioning, Survivor Psychological QOL, and Partner Psychological QOL
| Urinary functioning |
Bowel functioning |
Sexual functioning |
PCI total | |
|---|---|---|---|---|
| Survivor | ||||
| Depression | −.40*** | −.50*** | −.27* | −.50*** |
| Anxiety | −.41*** | −.48*** | −.21a | −.47*** |
| Fatigue | −.33** | −.52*** | −.35** | −.52*** |
| Positive affect | .28* | .50*** | .17 | .42*** |
| Partner | ||||
| Depression | −.35** | .01 | −.24* | −.23a |
| Anxiety | −.20 | .17 | −.25* | −.11 |
| Fatigue | −.31** | −.06 | −.27* | −.28* |
| Positive affect | .38** | .27* | .22a | .37** |
| Partner, with corresponding survivor QOL partialled out | ||||
| Depression | −.27* | .18 | −.18 | −.12 |
| Anxiety | −.21a | .20 | −.25* | −.12 |
| Stress | −.20 | .09 | −.20 | −.15 |
| Fatigue | −.30* | −.02 | −.26* | −.28* |
| Positive affect | .34** | .18 | .19a | .31 |
Note. PCI = Prostate Cancer Index. All variables assessed at T1. Partial correlations control for the corresponding QOL variable in survivors (e.g., survivors’ depression) when assessing the association between the partners’ QOL and survivors’ prostate specific functioning (e.g. partner depression–survivor urinary functioning).
p = .05 to .08.
p < .05.
p < .01.
p < .001.
To examine potential dyadic effects associated with prostate specific QOL, survivors’ prostate specific QOL was correlated with their partners’ psychological QOL. Results of these analyses appear in the middle of Table 2. Although not as uniformly significant as the correlations between survivors’ prostate specific QOL and survivors’ psychological QOL, these results revealed far more significant associations with partners’ psychological QOL than what would be expected by chance. Nine of the correlation coefficients in this matrix are statistically significant at p < .05, whereas only one would be significant by chance alone at this alpha level.
A core assumption of any dyadic analysis is that members of the dyad do not vary randomly on all variables. Rather, they exhibit nonindependence because of a variety of phenomena inherent in forming and maintaining a relationship. One might therefore suspect that the significant correlations between survivors’ prostate specific QOL and partners’ psychological QOL could be an artifact of this nonindependence. If survivors and partners are possibly matched on psychological QOL, variables that correlate with survivors’ QOL would be expected to correlate with partners’ QOL as well. To control for this possibility, a third series of correlation coefficients was calculated. These partial correlation coefficients reflect the association between survivors’ prostate specific QOL and their partners’ psychological QOL, controlling for survivors’ psychological QOL. These results appear on the bottom of Table 2. As evident from Table 2, even after controlling for the effect of survivors’ psychological QOL, survivors’ prostate specific QOL was still significantly correlated with some indicators of their partners’ psychological QOL. For example, survivors’ urinary functioning was correlated r = −.27, p < .05 with their partners’ depression and r = .28, p < .05 with their partners’ positive affect even after controlling for the survivors’ depression and positive affect, respectively. Survivors’ sexual functioning was correlated r = −.25, p < .05 with their partners’ anxiety, controlling for survivors’ anxiety. The results confirm that the association between survivors’ prostate cancer specific QOL and their partners’ psychological QOL is in at least some cases more than just an artifact of dyadic nonindependence in psychological QOL.
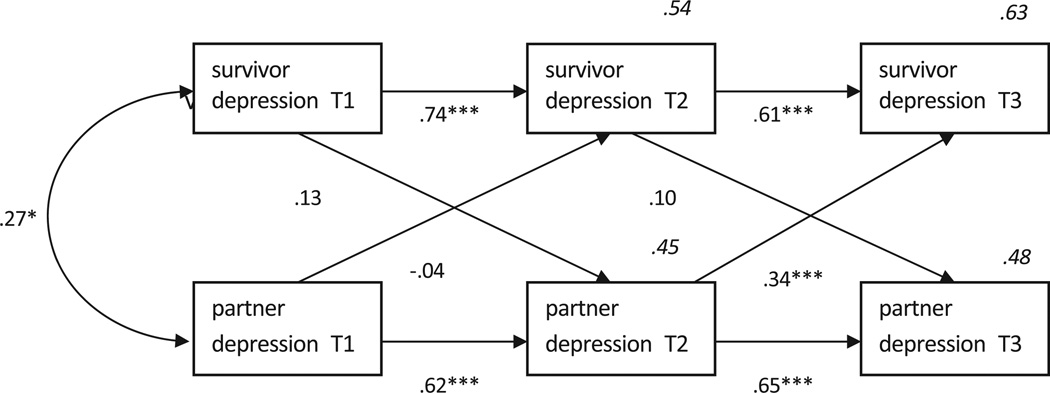
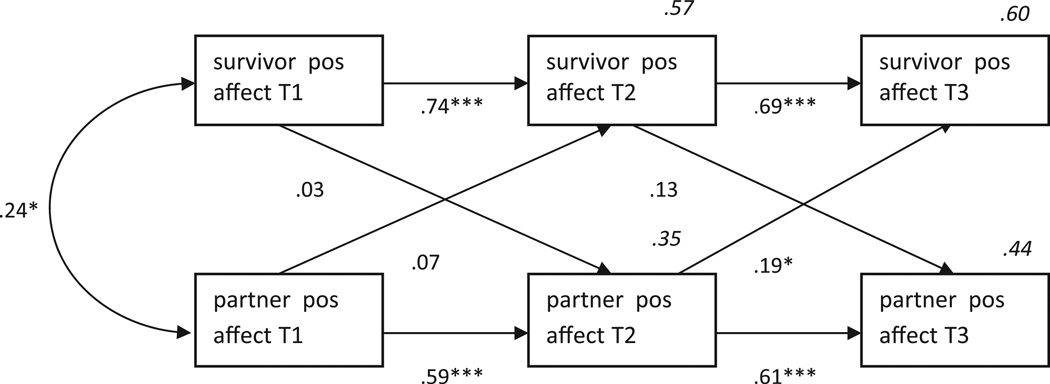
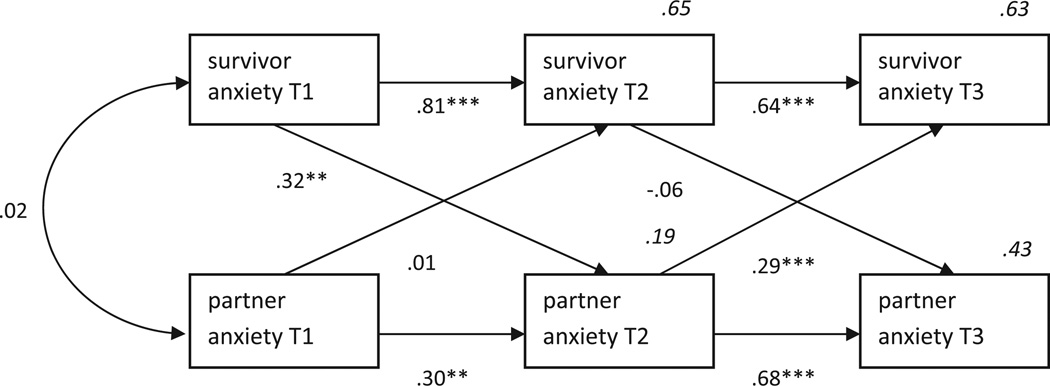
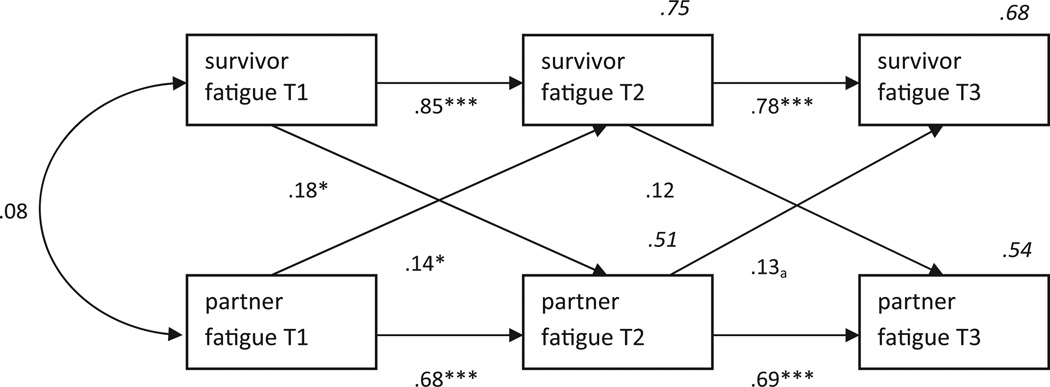
The next set of analyses tested for dyadic interdependence in psychological QOL over time. For these analyses, regression coefficients were estimated using structural equation modeling based on the actor-partner interdependence model (APIM) (Kashy & Kenny, 2000), as conceptualized by Kenny and Cook (1999). In short, these analyses treat the dyad as the unit of analysis and use participants’ scores on various independent variables (e.g., T1 depression) to predict both their own (actor effect) and their partner’s (partner effect) scores on the dependent variable (e.g., T3 depression) after taking into account the dyad’s interdependence on the independent variable. In the APIM, actor effects are estimated while controlling for partner effects and partner effects are estimated while controlling for actor effects. The APIM is commonly tested via path models that specify the actor and partner effects of interest while also specifying their existing interdependence on the independent variable (in this case, survivors’ and partners’ psychological QOL). As suggested by Kenny and Cook (1999) a correlation was specified for the error terms of the endogenous variables in the model in recognition of potential sources of nonindependence aside from partner effects. One such model was tested for each psychological QOL variable. For all models there were 27 elements of the variance-covariance matrix and 23 distinct parameters to be estimated, including two means and four intercepts, resulting in df = 4 for all models. Results of these analyses appear in Figures 1–4.
Figure 1.
APIM for survivor and partner symptoms of depression. Values in italics are R2. χ2 = 6.55, df = 4, p = .162, χ2/df = 1.64, CFI = .99. * p < .05. ***p < .001.
Figure 4.
APIM for survivor and partner positive affect. Values in italics are R2. χ2 = 17.07, df = 4, p = .002, χ2/df = 4.27, CFI = 0.93. ** p < .01. *** p < .001.
The values in Figures 1–4 are standardized regression coefficients. These are included for ease of comparison between models, but the significance of the various actor and partner effect was tested based on the unstandardized coefficients. In all four models, there were powerful actor effects as would be expected. All of the psychological QOL variables exhibited considerable construct stability over the 16-week course of the investigation. Of more relevance are the partner effects, indicated on the diagonal paths. There is a statistically significant partner effect from partners’ T2 psychological QOL to survivors’ T3 psychological QOL for depression (β = .34, p < .001), anxiety (β = .29, p < .001), and positive affect (β = .19, p < .001). The corresponding partner effect for partners’ T2 to survivors’ T3 fatigue was not statistically significant (β = .13, p = .09). Nevertheless, the overall pattern is remarkably consistent: The better partners’ psychological QOL was at T2, the better survivors’ QOL was at T3, or, the worse partners’ psychological QOL was at T2, the worse survivors’ QOL was at T3. Partner effects emanating from survivor to partner were comparatively rare and only apparent during the T1–T2 interval. Specifically, the more anxious survivors were at T1, the more anxious their partners were at T2 (β = .32, p < .01), and the more fatigued survivors were at T1, the more fatigued their partners were at T2 (β = .18, p < .05). There were otherwise no significant partner effects from survivor to partner.
To further deconstruct the dyadic effects depicted in Figures 1–4, we formally tested for dyadic mediation associated with each psychological QOL variable. Specifically we tested whether the T1→T3 effect for one person’s QOL was mediated by the other person’s T2 QOL. Although it is customary to test meditational effects with cross-sectional data, in true mediation the mediating variable must follow the independent variable, but precede the dependent variable. This is why all such analyses are set up to test one partner’s T2 QOL as the mediator of the other’s T1→T3 QOL effect. The estimation and significance of these effects was tested with bootstrapping procedures described by Preacher and Hayes (Preacher & Hayes, 2004), and an effect size estimation procedure for the mediation effect developed by Fairchild, MacKinnon, Taborga, and Taylor (Fairchild, Mackinnon, Taborga, & Taylor, 2009). Results of these tests appear in Table 3. As evident in Table 3, partner T2 psychological QOL mediated the T1→T3 effect for survivor depression and anxiety. Estimates of the magnitude of these mediation effects are R2 = .18 in both cases. Stated differently, partner T2 depression or anxiety explains 18% of the T1→T3 variance in survivor depression or anxiety. The corresponding APIMs in Figures 1 and 2 depict the direction of these effects as positive, indicating an increase in survivor distress as a function of increased partner distress. The remaining indirect effects for survivor T1→T3 distress were nonsignificant, although the associated effect sizes were in the R2 = .06 to .10 range. In contrast, none of the partner T1→T3 distress effects were significantly mediated by survivor T2 distress. Further, a comparison of R2 effect sizes for the mediation effects shows that all of the partner mediation effects of changes in survivor distress are larger in magnitude than the corresponding mediation effects for survivor distress on changes in partner distress. Simply put, partner distress accounts for more variance in T1–T3 changes in survivor distress than vice versa.
Table 3.
Dyadic Mediation of Survivor and Partner Distress (Survivor T1→Partner T2 → Survivor T3, Partner T1 → Survivor T2 → Partner T3)
| Distress variable | b | z | R2 | b | Z | R2 |
|---|---|---|---|---|---|---|
| Depression | .15 | 2.14* | .18 | .05 | 1.20 | .06 |
| Anxiety | .11 | 2.04* | .18 | .01 | 0.04 | .01 |
| Fatigue | .06 | 1.42 | .10 | .05 | 1.19 | .07 |
| Positive affect | .04 | 0.90 | .06 | −.05 | −1.15 | .03 |
Note. b = unstandardized regression coefficient and R2 = variance accounted for by indirect effect.
p < .05.
Figure 2.
APIM for survivor and partner symptoms of anxiety. Values in italics are R2. χ2 = 19.55, df = 4, p = .001, χ2/df = 4.89, CFI = 0.91. ** p < .01. ***p < .001.
To determine if the findings depicted in Figures 1–4 were influenced by the nature of the dyads (i.e., spousal/significant other vs. nonspousal) all four models were reanalyzed using just the data from the spousal dyads. The results were virtually identical to those in Figures 1–4. In addition, dyadic interdependence on all four variables (i.e., depression, anxiety, fatigue, positive affect) at all three waves of assessment was assessed with correlations that were calculated separately for spousal versus nonspousal dyads. The correlations for these two types of dyads were compared with the test for significant difference between two independent correlation coefficients. Only 1 of the 36 pairs of correlation coefficients was significantly different at p < .05, two-tailed.
Finally, to evaluate whether intervention condition influenced the nature of the actor and partner effects, each APIM model depicted in Figures 1–4 was reanalyzed separately for dyads in the telephone counseling and health education groups. Only 1 of the 16 actor effects tested in these four models was significant (p < .05) in one intervention condition but not the other. However, 7 of the 16 partner effects tested in these models were statistically significant in one intervention condition but not the other. Where there were such differences, four of the seven partner effects were statistically significant only in the telephone counseling condition (T1 survivor depression→T2 partner depression, T1 survivor anxiety→T2 partner anxiety, T2 partner anxiety→T3 survivor anxiety, T1 survivor positive affect→T2 partner positive affect), and 3 of the 7 partner effects were statistically significant only in the health education condition (T2 partner depression→T3 survivor depression, T1 survivor fatigue→T2 partner fatigue, T2 partner positive affect→T3 survivor positive affect). Because there are four potential partner effects in each model, it is not possible to identify a clear pattern of significant partner effects for a particular psychological QOL variable, or for a particular intervention condition. Collectively, these results suggest that intervention condition had a negligible effect on the actor effects and a modest and inconsistent effect on the partner effects, but there was no clear evidence of one condition producing more dyadic interdependence than the other.
Discussion
The primary aim of this investigation was to examine the extent of dyadic interdependence in psychological QOL in dyads adjusting to prostate cancer and its treatment. Toward that end, dyads completed three waves of measurement over the course of 16 weeks. The findings revealed that survivors’ prostate specific QOL is associated with both their own and their partner’s psychological QOL. Longitudinally, there was evidence that partners’ psychological QOL at T2 predicted survivors’ psychological QOL at T3.
Associations between the damaging side effects of prostate cancer treatment (e.g., sexual dysfunction) and survivors’ psychological distress have been abundantly documented in the literature (Wootten et al., 2007). It has also been show that survivors’ partners can also be negatively affected by these problems and the associated distress experienced by survivors (Ezer et al., 2006). The present investigation adds to these findings in two ways. First, for understandable reasons research on interpersonal consequences of prostate cancer has focused on spouses. However, many men with prostate cancer are widowed, divorced, or otherwise without a spouse, but still reliant on the support of other social network members. The sample in this study included nonspouse significant others in 17% of the dyads, yet the distress of the partners in association with survivors’ prostate specific QOL was still evident. Second, we found that even when controlling for the survivors’ QOL, the partners’ psychological QOL (e.g., depression, anxiety, positive affect) was still significantly associated with some aspects of survivors’ prostate specific QOL (e.g., urinary and sexual functioning). This finding has theoretical significance in that it rules out the possibility that partners’ psychological distress is really yoked to survivors’ psychological distress, which is confounded with their prostate specific QOL. By controlling for survivors’ psychological distress, it can be concluded that some aspects of survivors’ prostate specific functioning is associated with psychological distress in their partners, and this association is more than what could be explained by the partners’ reactions to the survivors’ own distress. For example, a survivor who experiences significant urinary and bowel problems would be likely to have reduced psychological QOL. In addition, he may generate greater amounts of laundry than in the past, have to restrict his leisure and travel, awaken more frequently in the middle of the night, and so on. These changes in routines could easily affect his spouses’ psychological QOL, regardless of his psychological distress in response to these changes.
To test for dyadic interdependence in psychological QOL, APIMs were analyzed for each of the four QOL variables. There was a remarkable partner effect that appeared in all of these models. Specifically, the more distressed the partner was at T2, the more distressed the survivor was at T3, even after controlling for initial nonindependence in psychological QOL, as well as any prior actor or partner effects between T1 and T2. It is noteworthy that this partner effect was statistically significant in three of the four models, and p = .09 in the fourth. Between T1 and T2, survivors and their partners were participating in an intervention on a weekly basis. However, between T2 and T3 there was no contact with the interventionist, so any natural sources or processes of mutual influence within the dyad were free to occur without any outside intercession. The pattern of the effect, flowing from partner to survivor, is consistent with findings from dyads adjusting to breast cancer where all the survivors were female (Segrin et al., 2007; Segrin et al., 2005). They also speak to the issue of whether dyadic interdependence in psychological distress and QOL is exclusively a process of male to female transmission. In this investigation all of the cancer survivors were male and 94% of the partners were female. It can therefore be concluded that even though women experience more distress than men in dyads adjusting to cancer (Hagedoorn et al., 2008), dyadic interdependence in psychological distress and QOL does not just take the form of male to female influence. Male survivors may have the same propensity to experience contagion of affective states from their partners as female survivors do.
Even though most of the dyadic interdependence in psychological QOL appeared to run in the direction of partner to survivor, there were at least some cases where the opposite was true. The more anxious and fatigued survivors were at T1, the more anxious and fatigued their partners were at T2 (controlling for any initial nonindependence in distress at T1). This suggests that the survivors’ distress can predict their partners’ distress in some instances, and replicates comparable findings documented in studies of breast cancer survivors and their partners (Gaston-Johansson, Lachica, Fall-Dickson, & Kennedy, 2004).
A set of follow up analyses to the APIMs for psychological distress showed that partners’ depression and anxiety at T2 significantly mediated the association between survivors’ T1 and T3 depression and anxiety. In other words, partners’ distress at T2 explained significant T1–T3 variation in survivors’ distress. This finding is new to the literature. It demonstrates rather conclusively that part of the fluctuation in prostate cancer survivors’ distress, namely depression and anxiety, can be predicted by the prior distress of their partners. Practitioners seeking to manage QOL in cancer survivors would be well advised to consider the reactions and responses of survivors’ key relational partners and social support providers. The psychological QOL of these often overlooked individuals could be playing a significant role in alleviating or exacerbating distress in the survivor.
Findings from this investigation have a number of implications for theories of emotional contagion. One common explanation for emotional contagion is based on behavioral mimicry that is a phenomenon that happens in the moment of observing another person’s emotional reaction (Hatfield et al., 1992). This theoretical account predicts that emotional contagion occurs in close proximity to the emotional display by the other member of a dyad. The findings from this investigation demonstrate longer reaching emotional contagion effects under stringent conditions (i.e., controlling for initial dyadic interdependence in psychological QOL and controlling for prior psychological QOL in both the self and the partner). Prostate cancer survivors in this investigation showed evidence of emotional contagion from their partners as long as 2 months from the assessment of affect in the partner. Results from this investigation also provide further confirmatory evidence for theoretical accounts of emotional contagion that highlight its propensity under conditions of similarity between members of the dyad (Epstude & Mussweiler, 2009), confrontation by a common threat (Gump & Kulik, 1997), and depression in one member of the dyad (Coyne, 1976).
There are several qualities of this investigation that place limits on interpretation of its conclusions. First, the sample of prostate cancer survivors was diverse with respect to time since diagnosis. Some of the dyads had received the diagnosis several weeks before enrolling in the investigation whereas others had learned of the diagnosis over 5 years ago. There are clearly major variations in coping and adjustment as a function of time since diagnosis, and it would be worthwhile to investigate these in more homogeneous subgroups of survivors and their partners (see, e.g., Northouse et al., 2007). Second, this is a fairly well-educated sample of survivors and partners. The resources available to such individuals, both financial and informational, could potentially mitigate some of the psychological distress and uncertainty experienced by cancer survivors and their partners. Exploration of the interactive effects of socioeconomic disadvantage on survivorship and dyadic interdependence would also be a worthy enterprise for future investigations. In addition, all of the participants were volunteers and the sample may therefore not be representative of the general population of prostate cancer survivors. Finally, all dyads were participating in some form of intervention that could have influenced the extent of dyadic interdependence, although it is unclear why that would run almost exclusively from partner to survivor and only from T2 to T3.
In conclusion, the results of this study show that prostate specific functioning of prostate cancer survivors is associated with their own and their partners’ psychological QOL. Furthermore, partners’ psychological QOL is predictive of subsequent psychological QOL experienced by survivors. This implies that it is beneficial to the prostate cancer survivor’s QOL to have a partner with low levels of depression and anxiety, and high levels of positive affect. Accordingly, health care providers would be well-advised to consider the role of partners’ emotional state on the adjustment of their prostate cancer patients. The results of this investigation suggest that including these partners in support groups and providing services to them as needed has the potential to improve the QOL of prostate cancer survivors.
Figure 3.
APIM for survivor and partner fatigue. Values in italics are R2. χ2 = 10.51, df = 4, p = .033, χ2/df = 2.63, CFI = 0.97. a p = .09. * p < .05. *** p < .001.
Acknowledgments
Funding for this study was provided by the National Cancer Institute to Terry Badger (R21CA113409). We gratefully thank our recruitment sites: Arizona Cancer Center, Veterans’ Affairs Health Care Systems in Phoenix and Tucson, AZ. This material is the result of work supported with the resources and the use of facilities at the Veteran’s Affairs Health Care Systems in Phoenix and Tucson. We thank Kate Sheppard, Stacey Passalacqua, Maria Figueroa, Xochitl Gaxiola, Jeannine Thomas, Jen Riech, and Karina Othon-Tapia. The contents of this publication do not represent the views of the Department of Veterans Affairs or the United States Government.
Contributor Information
Chris Segrin, Department of Communication, The University of Arizona.
Terry A. Badger, College of Nursing, The University of Arizona
Joanne Harrington, Phoenix Veterans’ Affairs Health Care System.
References
- Aranda SK, Hayman-White K. Home caregivers of the person with advanced cancer: An Australian perspective. Cancer Nursing. 2001;24:300–307. doi: 10.1097/00002820-200108000-00011. [DOI] [PubMed] [Google Scholar]
- Badger TA, Segrin C, Figueredo AJ, Harrington J, Sheppard K, Passalacqua S, Bishop M. Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Quality of Life Research. 2011;20:833–844. doi: 10.1007/s11136-010-9822-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balderson N, Towell T. The prevalence and predictors of psychological distress in men with prostate cancer who are seeking support. British Journal of Health Psychology. 2003;8:125–134. doi: 10.1348/135910703321649114. [DOI] [PubMed] [Google Scholar]
- Bambauer KZ, Zhang B, Maciejewski PK, Sahay N, Pirl WF, Block SD, Prigerson HG. Mutuality and specificity of mental disorders in advanced cancer patients and caregivers. Social Psychiatry and Psychiatric Epidemiology. 2006;41:819–824. doi: 10.1007/s00127-006-0103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC. Toward an interactional description of depression. Psychiatry. 1976;39:28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- Danjoux C, Gardner S, Fitch M. Prospective evaluation of fatigue during a course of curative radiotherapy for localised prostate cancer. Supportive Care in Cancer. 2007;15:1169–1176. doi: 10.1007/s00520-007-0229-8. [DOI] [PubMed] [Google Scholar]
- Epstude K, Mussweiler T. What you feel is how you compare: How comparisons influence the social induction of affect. Emotion. 2009;9:1–14. doi: 10.1037/a0014148. [DOI] [PubMed] [Google Scholar]
- Eton DT, Lepore SJ, Helgeson VS. Psychological distress in spouses of men treated for early-stage prostate carcinoma. Cancer. 2005;103:2412–2418. doi: 10.1002/cncr.21092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezer H, Ricard N, Bouchard L, Souhami L, Saad F, Aprikian A, Taguchi Y. Adaptation of wives to prostate cancer following diagnosis and 3 months after treatment: A test of family adaptation theory. International Journal of Nursing Studies. 2006;43:827–838. doi: 10.1016/j.ijnurstu.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Fairchild AJ, Mackinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analysis. Behavioral Research Methods. 2009;41:486–498. doi: 10.3758/BRM.41.2.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garos S, Kluck A, Aronoff D. Prostate cancer patients and their partners: Differences in satisfaction indices and psychological variables. Journal of Sexual Medicine. 2007;4:1394–1403. doi: 10.1111/j.1743-6109.2007.00545.x. [DOI] [PubMed] [Google Scholar]
- Gaston-Johansson F, Lachica EM, Fall-Dickson JM, Kennedy MJ. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncology Nursing Forum. 2004;31:1161–1169. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- Goodman CR, Shippy RA. Is it contagious? Affect similarity among spouses. Aging and Mental Health. 2002;6:266–274. doi: 10.1080/13607860220142431. [DOI] [PubMed] [Google Scholar]
- Gump BB, Kulik JA. Stress, affiliation, and emotional contagion. Journal of Personality and Social Psychology. 1997;72:305–319. doi: 10.1037//0022-3514.72.2.305. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Harrington CB, Hansen JA, Moskowitz M, Todd BL, Feuerstein M. It’s not over when it’s over: Long-term symptoms in cancer survivors-a systematic review. International Journal of Psychiatry in Medicine. 2010;40:163–181. doi: 10.2190/PM.40.2.c. [DOI] [PubMed] [Google Scholar]
- Hatfield E, Cacioppo JT, Rapson RL. Primitive emotional contagion. In: Clark MS, editor. Emotion and social behavior. Newbury Park, CA: Sage; 1992. pp. 151–177. [Google Scholar]
- Hatfield E, Cacioppo JT, Rapson RL. Emotional contagion. New York: Cambridge University Press; 1994. [Google Scholar]
- Karakiewicz PI, Bhojani N, Neugut A, Shariat SF, Jeldres C, Graefen M, Kattan MW. The effect of comorbidity and socioeconomic status on sexual and urinary function and on general health-related quality of life in men treated with radical prostatectomy for localized prostate cancer. Journal of Sexual Medicine. 2008;5:919–927. doi: 10.1111/j.1743-6109.2007.00741.x. [DOI] [PubMed] [Google Scholar]
- Kashy DA, Kenny DA. The analysis of data from dyads and groups. In: Judd M, editor. Handbook of research methods in social and personality psychology. New York, NY: Cambridge University Press; 2000. pp. 451–477. [Google Scholar]
- Kenny DA, Cook W. Partner effects in relationship research: Conceptual issues, analytic difficulties, and illustrations. Personal Relationships. 1999;6:433–448. [Google Scholar]
- Ko CM, Malcarne VL, Varni JW, Roesch SC, Banthia R, Greenbergs HL, Sadler GR. Problem-solving and distress in prostate cancer patients and their spousal caregivers. Supportive Care in Cancer. 2005;13:367–374. doi: 10.1007/s00520-004-0748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korfage IJ, Essink-Bot ML, Janssens AC, Schroder FH, de Koning HJ. Anxiety and depression after prostate cancer diagnosis and treatment: 5-year follow-up. British Journal of Cancer. 2006;94:1093–1098. doi: 10.1038/sj.bjc.6603057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA Prostate Cancer Index: Development, reliability, and validity of a health-related quality of life measure. Medical Care. 1998;36:1002–1012. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- Maliski SL, Kwan L, Elashoff D, Litwin MS. Symptom clusters related to treatment for prostate cancer. Oncology Nursing Forum. 2008;35:786–793. doi: 10.1188/08.ONF.786-793. [DOI] [PubMed] [Google Scholar]
- Manne SL, Norton TR, Ostroff JS, Winkel G, Fox K, Grana G. Protective buffering and psychological distress among couples coping with breast cancer: The moderating role of relationship satisfaction. Journal of Family Psychology. 2007;21:380–388. doi: 10.1037/0893-3200.21.3.380. [DOI] [PubMed] [Google Scholar]
- Mehnert A, Lehmann C, Schulte T, Koch U. Presence of symptom distress and prostate cancer-related anxiety in patients at the beginning of cancer rehabilitation. Onkologie. 2007;30:551–556. doi: 10.1159/000108578. [DOI] [PubMed] [Google Scholar]
- Mellon S, Northouse LL. Family survivorship and quality of life following a cancer diagnosis. Research in Nursing & Health. 2001;24:446–459. doi: 10.1002/nur.10004. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, Montie JE, Sandler HM, Forman JD, Hussain M, Kershaw T. Living with prostate cancer: Patients’ and spouses’ psychosocial status and quality of life. Journal of Clinical Oncology. 2007;25:4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- Penson DF, Litwin MS, Aaronson NK. Health related quality of life in men with prostate cancer. Journal of Urology. 2003;169:1653–1661. doi: 10.1097/01.ju.0000061964.49961.55. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavioral Research Methods, Instrumentation, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Rabin EG, Heldt E, Hirakata VN, Bittelbrunn AC, Chachamovich E, Fleck MP. Depression and perceptions of quality of life of breast cancer survivors and their male partners. Oncology Nursing Forum. 2009;36:E153–E158. doi: 10.1188/09.ONF.E153-E158. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, Wei JT. Quality of life and satisfaction with outcome among prostate-cancer survivors. New England Journal of Medicine. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger T, Dorros SM, Meek P, Lopez AM. Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psycho-Oncology. 2007;16:634–643. doi: 10.1002/pon.1111. [DOI] [PubMed] [Google Scholar]
- Segrin C, Badger TA, Meek P, Lopez AM, Bonham E, Sieger A. Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. Journal of Social and Personal Relationships. 2005;22:673–689. [Google Scholar]
- Smets EM, Garssen B, Bonke B, De Haes JC. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. Journal of Psychosomatic Research. 1995;39:315–325. doi: 10.1016/0022-3999(94)00125-o. [DOI] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch R, Lushene R, Vagg P, Jacobs G. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Stanford JL, Feng Z, Hamilton AS, Gilliland FD, Stephenson RA, Eley JW, Potosky AL. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: The Prostate Cancer Outcomes Study. Journal of the American Medical Association. 2000;283:354–360. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- Steineck G, Helgesen F, Adolfsson J, Dickman PW, Johansson JE, Norlen BJ. Scandinavian Prostatic Cancer Group Study Number 4 Quality of life after radical prostatectomy or watchful waiting. New England Journal of Medicine. 2002;347:790–796. doi: 10.1056/NEJMoa021483. [DOI] [PubMed] [Google Scholar]
- Thompson RL, Lewis SL, Murphy MR, Hale JM, Blackwell PH, Acton GJ, Bonner PN. Are there sex differences in emotional and biological responses in spousal caregivers of patients with Alzheimer’s disease? Biological Research in Nursing. 2004;5:319–330. doi: 10.1177/1099800404263288. [DOI] [PubMed] [Google Scholar]
- Traeger L, Penedo FJ, Gonzalez JS, Dahn JR, Lechner SC, Schneiderman N, Antoni MH. Illness perceptions and emotional well-being in men treated for localized prostate cancer. Journal of Psychosomatic Research. 2009;67:389–397. doi: 10.1016/j.jpsychores.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wootten AC, Burney S, Foroudi F, Frydenberg M, Coleman G, Ng KT. Psychological adjustment of survivors of localised prostate cancer: Investigating the role of dyadic adjustment, cognitive appraisal and coping style. Psycho-Oncology. 2007;16:994–1002. doi: 10.1002/pon.1159. [DOI] [PubMed] [Google Scholar]