Abstract
Purpose
Remote monitoring technologies (RMTs) may improve quality of care, reduce access barriers, and help control medical costs. Despite the role of primary care clinicians as potential key users of RMTs, few studies explore their views. This study explores rural primary care clinician interest and the resources necessary to incorporate RMTs into routine practice.
Methods
We conducted 15 in-depth interviews with rural primary care clinician members of the Oregon Rural Practice-based Research Network (ORPRN) from November 2011 to April 2012. Our multidisciplinary team used thematic analysis to identify emergent themes and a cross-case comparative analysis to explore variation by participant and practice characteristics.
Results
Clinicians expressed interest in RMTs most relevant to their clinical practice, such as supporting chronic disease management, noting benefits to patients of all ages. They expressed concern about the quantity of data, patient motivation to utilize equipment, and potential changes to the patient-clinician encounter. Direct data transfer into the clinic’s electronic health record (EHR), availability in multiple formats, and review by ancillary staff could facilitate implementation. Although participants acknowledged the potential system-level benefits of using RMTs, adoption would be difficult without payment reform.
Conclusions
Adoption of RMTs by rural primary care clinicians may be influenced by equipment purpose and functionality, implementation resources, and payment. Clinician and staff engagement will be critical to actualize RMT use in routine primary care.
Keywords: e-health, in-depth interview, primary care, qualitative research, rural health
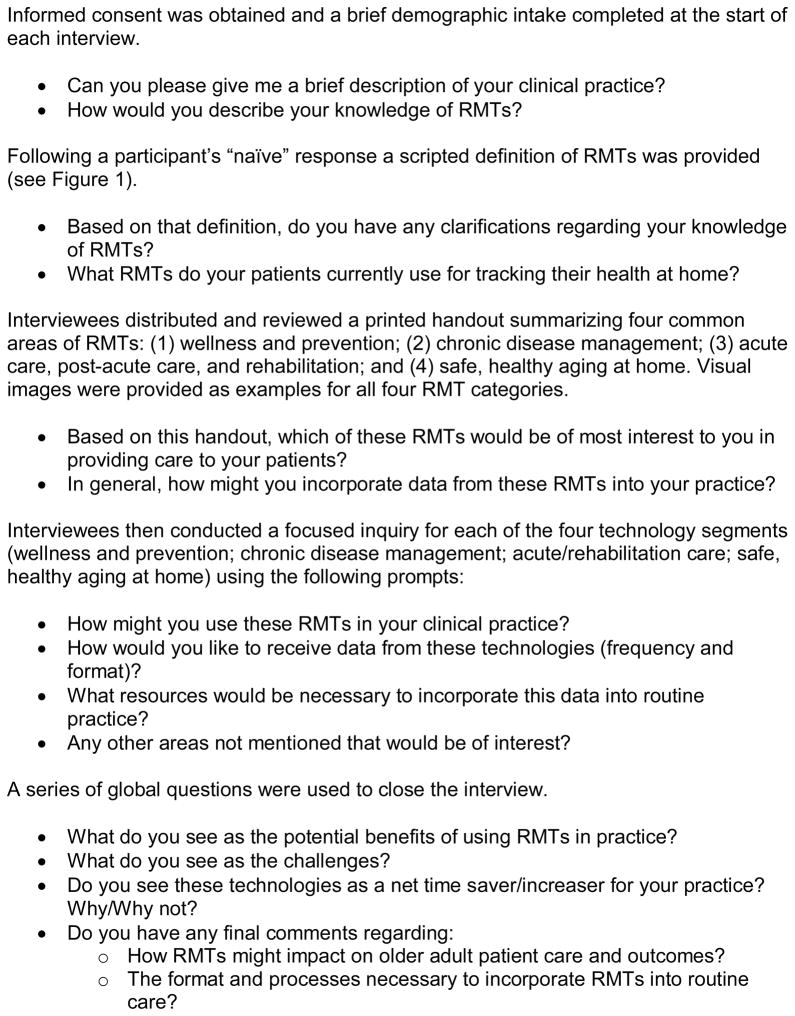
Population aging has contributed to development of new market niches for e-health technologies to support healthy aging, control rising health care costs, and circumvent the limited health workforce availability.1–3 E-health describes a range of information and communication technologies used to provide health care, such as Internet- or computer-based technologies, telemedicine, remote monitoring technologies (RMTs), electronic health records, and videoconferencing.4 As defined in Figure 1, RMTs include any technology that enables the monitoring of an individual’s health status through a remote interface and then transmits this information to a health care provider for clinical review.5 Although numerous media sites tout the potential of RMTs to enhance patient care,6–9 and private sector investment nearly doubled in the first half of 2012,10 limited research explores interest in and feasibility of adopting these technologies in primary care settings.
Figure 1.
Definition of Remote Monitoring Technologies (RMTs) for Health
Older adults, caregivers, and health care professionals are identified as the target users for many RMTs. Primary care clinicians may play a key role in monitoring and responding to RMT data.11 Use of RMTs may reduce care access barriers12 and enable early detection of disease onset.13 Various characteristics of rural regions may promote RMT adoption. Rural populations tend to be older and in poorer health than their urban counterparts,14 characteristics that may warrant RMT tracking and monitoring. Additionally, rural patients have access to fewer health care providers, frequently receive care in facilities with a limited scope of service, have longer distances to travel and higher costs associated with accessing health care, and experience disparities in the receipt of medical services.15–17 Use of RMTs in rural primary care may enable proactive patient management and alleviate some of the barriers rural populations experience in receipt of medical care. However, scarcity in technical infrastructure and expertise as well as limited financial resources may make adoption of health information technologies (HIT) especially challenging for rural providers.18,19
Although studies explore the views of elders and caregivers toward RMTs,20–23 these technologies are often developed without investigating clinician preferences.24–26 Given the potential use of RMTs in primary care, it is important to explore what type of technologies clinicians value and how they might use this information to deliver care. Therefore, we conducted this study to: (a) understand rural primary care clinician interest in RMTs with an emphasis on improving care for elders and (b) determine the infrastructure and processes necessary to incorporate data from RMTs into routine practice.
METHODS
Study Setting and Design
In this cross-sectional qualitative study, we conducted in-depth interviews with family medicine clinician members of the Oregon Rural Practice-based Research Network (ORPRN).27 Based on the 2009–2010 ORPRN member survey, the network included 153 clinicians in 41 primary care practices located in rural Oregon communities. ORPRN membership is 63% physician and 37% non-physician clinicians; 61% of the clinics reported using an electronic health record (EHR) system. This study was approved by the Oregon Health & Science University Institutional Review Board.
Sampling Strategy
We reviewed the list of 114 clinicians completing the 2009–2010 ORPRN member survey that reported providing care to patients over 65 years of age. We invited a purposive sample to participate based on geographic diversity (eg, large rural, small rural, and isolated—using ZIP code-level Rural-Urban Commuting Area [RUCA] classifications),28 demographic characteristics (eg, age, gender), clinical training (eg, physician, non-physician provider), and practice characteristics (eg, size, EHR status, ownership, proportion of patients over 65 years of age). We sampled along these dimensions anticipating that participants may have greater interest in RMTs if they practiced in more rural settings, were younger, had access to an EHR, and provided care to a higher proportion of elder patients. We collected data until we reached saturation, the point at which findings repeated or recurred, across the sample.29,30
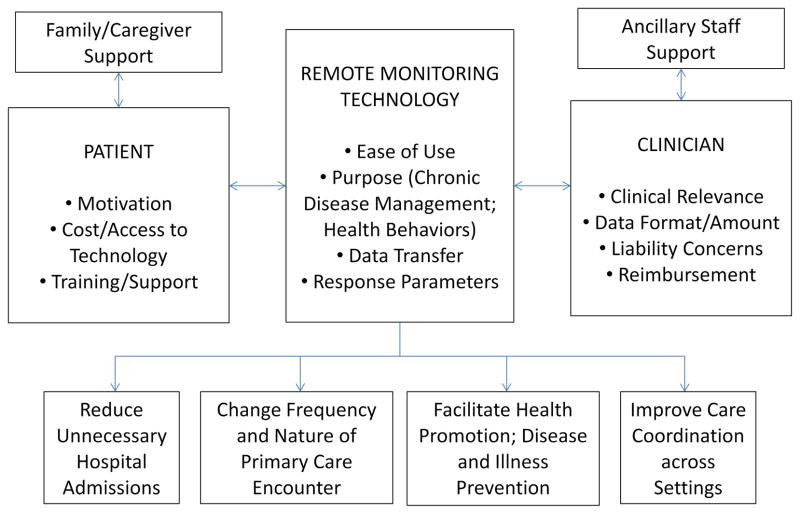
Data Collection
From November 2011 to April 2012, 2 authors (JC, MRD) who are familiar with RMTs conducted all interviews using a semi-structured guide (see Figure 2). At the start of each session participants provided informed consent and completed a brief demographic intake survey. During the interview participants were provided with a precise definition of RMTs (see Figure 1) and reviewed a printed handout with visual examples describing 4 common RMT categories (wellness and prevention; chronic disease management; acute care, post-acute care, and rehabilitation; safe, healthy aging at home).
Figure 2.
Overview of the Remote Monitoring Technology (RMT) Semi-Structured Interview Guide
We audio-recorded sessions (average length 37 minutes) and took field notes to capture non-verbal communication. Recordings were transcribed, de-identified, and transferred to Atlas.ti (Version 7.0, Atlas.ti Scientific Software Development GmbH, Berlin, Germany) for data analysis and retrieval. Data collection proceeded iteratively and concurrent analysis allowed the study team to identify areas warranting additional inquiry and to refine the interview guide. Drawing on the existing literature we initially focused our study on the use of RMTs to enhance elder care. However, based on findings from our initial interviews we chose to explore use of RMTs for patients across the lifespan with latter participants.
Data Analysis
The multidisciplinary team (with expertise in family medicine, gerontology, qualitative methods, RMT, and implementation research) used the 6 phases of thematic analysis to identify emergent themes: familiarizing with data; generating initial codes; searching for, reviewing, then defining and naming themes; and producing a scholarly report.31 Five authors (MMD, JMC, MRD, NV, SH) read early transcripts and defined a preliminary coding scheme. Using an iterative process we independently coded transcripts; then small groups met to discuss codes, identify emergent themes, and resolve discrepancies through consensus.32 Two authors (LB, LJF) helped refine themes during multiple retreats with the full analysis team. We conducted a cross-case comparative analysis by participant (eg, training, age, interest in new technologies) and practice (eg, size, EHR status) characteristics to examine differences among perspectives.33
RESULTS
Participant training, practice characteristics, and self-reported interest in information technology are summarized in Table 1. All 15 participants specialized in family medicine, and physicians made up 73.3% of the sample (n = 11). Clinicians provided care in practices that ranged in size from 2 to 8 clinicians (Mean = 4.5, SD = 1.9). Mean participant age was 46.8 years (range 29–73, SD = 12.9) and 66.7% were male (n = 10). All participants reported using desktop or laptop computers and all indicated they were “very comfortable” or “comfortable” using computers. More than half (53%) used smartphones (n = 8), and most (80%, n = 12) accessed online health information daily. All participants were aware of the RMT concept; however, 40% (n = 6) reported some and 60% (n = 9) reported limited familiarity with these technologies.
Table 1.
Summary of Participant Characteristics
| No | Traininga | Gender | Age | Years in Practice | Practice Size (n clinicians) | Practice Ruralityb | Electronic Health Record (EHR) Implementationc | % of patients over 65 years in age on panel | Interest in new technologiesd | Knowledge and Familiarity with RMTs | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Completed | Currently Implementing or Considering | ||||||||||
| 1 | PA | Male | 34 | 0.5 | 8 | Small | X | 40 | 5 | Limited | |
| 2 | MD | Male | 44 | 12 | 8 | Small | X | 80 | 5 | Limited | |
| 3 | MD | Male | 32 | 2 | 6 | Isolated | X | 60 | 4 | Some | |
| 4 | MD | Male | 40 | 13 | 4 | Isolated | X | 50 | 4 | Limited | |
| 5 | MD | Female | 54 | 12 | 4 | Isolated | X | 40 | 5 | Limited | |
| 6 | MD | Male | 54 | 17 | 5 | Large | X | 40 | 3 | Limited | |
| 7 | MD | Male | 73 | 41 | 3 | Large | X | 10 | 5 | Some | |
| 8 | MD | Male | 51 | 15 | 2 | Large | X | 30 | 5 | Some | |
| 9 | PA | Male | 34 | 6 | 4 | Small | X | 20 | 3 | Limited | |
| 10 | MD | Female | 36 | 6 | 6 | Isolated | X | 29 | 5 | Some | |
| 11 | PA | Female | 29 | 4 | 3 | Large | X | 25 | 5 | Limited | |
| 12 | PA | Female | 62 | 11 | 2 | Isolated | X | 39 | 5 | Some | |
| 13 | DO | Male | 43 | 12 | 3 | Isolated | X | 40 | 3 | Some | |
| 14 | MD | Male | 60 | 30 | 5 | Isolated | X | 40 | 4 | Limited | |
| 15 | MD | Female | 56 | 30 | 5 | Small | X | 50 | 3 | Limited | |
MD = Medical Doctor; DO = Doctor of Osteopathy; PA = Physician Assistant
Rurality determined based on Rural-Urban Commuting Area (RUCA) Classifications: Large Rural City/Town (micropolitan) focused, Small Rural Town focused, Isolated Small Rural Town focused
On the 2009–2010 ORPRN Member survey, 61% of the member clinics reported using an EHR
Likert scale from 1 (not very) to 5 (very)
Across our sample we found that neither participant nor practice characteristics (eg, age, gender, practice size, proportion of patients on panel over 65 years of age, interest in new technologies) appeared to drive perspectives toward RMTs. Instead, participants expressed interest or hesitation in response to potential RMTs based on their alignment with the goals of primary care, and their perceived ease of use versus hassle to integrate in routine practice. As one physician stated:
I think you could over monitor [patients] to the point that it gives them almost too much information…And they dwell on it and it consumes them. And then it consumes us as a doctor, and all our time [is spent] trying to describe and break [the information] down and see what’s useful and what is not…I think the biggest part is what’s going to be useful to your practice to help you improve your patient care…not just overwhelm you with esoteric details that don’t mean anything. You know, I’m interested. I’m good about looking into new things. It’s just how useful are [RMTs] going to be versus are they going to be more pain for us to implement…and [for] our patients? (#13, Physician)
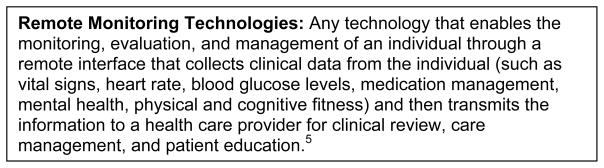
Figure 3 summarizes participants’ perspectives on using RMTs in rural primary care, highlighting how clinician, technology, and patient characteristics, as well as supportive contexts (eg, staffing, caregiver/family), shape perceptions. Key emergent themes are described in greater detail below.
Figure 3.
Rural Primary Care Clinician Views toward Remote Monitoring Technologies (RMTs)
Alignment With Primary Care
Clinicians noted that the RMT concept closely aligned with the goals of primary care: its use could help reduce hospital admissions and make visits to the clinic timelier.
[Remote monitoring supports] the core premise of primary care, which is promoting health and preventing disease or illness. And the goal of doing these things is to be able to track over time, see early warning signs of decompensation, either of a person or of their disease and intervene before it becomes a problem. (#10, Physician)
For patients that are pretty stable and I see every 6 months to a year, having [remote monitoring] data would make me feel…more confident that they were doing well. For [other patients] it would allow us to monitor things without them having to come in weekly or twice a week. We’d be able to have an idea what was going on and potentially save them some trips [to the clinic]. (#2, Physician)
In addition, RMTs could provide a richer understanding of patient behavior outside of the medical encounter, enabling improved care coordination with other medical professionals (eg, occupational therapists, physical therapists, specialists) and family members/caregivers.
Participants expressed the most interest in technologies aligned with common clinical practice experience, specifically, chronic disease management.
…the [technologies] I would use the most would be for chronic disease management. Almost all of our patients have some kind of chronic disease that we’re keeping track of at home…. I would continue to do what I’ve been doing if I don’t have any better technology…I only see a patient for a few minutes every few months or so. They’re the ones that live with their body continually… the more information I have the better. (#1, Physician )
Although wellness and prevention technologies could help motivate patients and provide objective measures of health behaviors, clinicians found these most useful in relation to a patient’s medical conditions. One physician (#15) stated, “In populations that I was concerned about medically, I would be interested in seeing [wellness and prevention data].” Clinicians emphasized that RMTs had the potential to benefit all of their patients with a need or disease–not just elders. Another physician (#4) commented, “If they have diabetes, it doesn’t matter how old they are… [these technologies are] useful for all ages, but older folks as well.”
Clinicians indicated RMTs to support aging in place or post-hospital care may be more pertinent for use by other health professionals, family members, or caregivers. Some clinicians were hesitant to review data from post-hospitalized patients, noting that if a patient needs to be monitored that closely the patient should remain in the inpatient setting. Although some participants wished they had access to aging in place RMTs for use with their own parents, many expressed concern about how to utilize this data in treating patients.
[The data for aging in place] is a little overwhelming. I think stuff like this is all useful. Now how practical it is, I don’t know…if I got this information, it would probably be useful. But, is it worth it?…I guess I wouldn’t know what to do with all this information. (#4, Physician)
Data Quantity and Timing
Clinicians wanted enough data from RMTs to act, but not so much that it would overshadow the time they spend providing direct patient care. Participants noted a fine line between having enough information at the right time, and getting so much that review required more time than actual patient care. A physician assistant (#1) noted, “If we have too many things to monitor…and time spent looking at all their information is more than the time we’re spending with the patient, then I don’t know if that’s really helping at all.
Clinicians noted that the desired timing and frequency of data review varied based on the type of technology and the patient’s condition. A physician (#2) commented, “…frequency [of review] would depend on the acuity or the level of worry that we had regarding the clinical situation. [It]…would be a little bit variable. If it was something that was stable, then every 6 weeks to 3 months [would be fine]. Participants wanted to review chronic disease data in real time to facilitate rapid interventions. Data on health behavior change could be reviewed at the point of care and used to motivate and reinforce behavior. Review of aging in place data would be influenced by the patient’s other resources, such as support from the family.
Data Transfer and Presentation
Clinicians wanted RMT data to integrate with the clinic’s EHR, be available in multiple display formats, and be accessible across care settings. Clinicians preferred that RMT data be imported directly to their EHRs. However, many were skeptical about this capacity noting that, at a minimum, they need to be able to attach data summaries to the patient’s record.
If [the data] could come directly into our EHR that would be great. Then it would be recorded and I could manage it through there…. Faxes and printouts are okay, but it’s more paper to be shuffled and something else to scan into the record…. It’s still useful information, but the ideal would be if somehow it directly links to the EHR. (#3, Physician)
Clinicians also wanted to be able to vary RMT data presentations based on their audience; reviewing numbers for themselves but trending out data in graphic form to share with patients or caregivers. Additionally, clinicians wanted data to transfer across organizations within a community (eg, primary care, hospital, nursing home) so that patient care could be coordinated. A few participants suggested that patients should be able to annotate the data collected by these technologies (eg, “I’m feeling poorly” when a reading is low or high), which would help the clinician assess the patient’s condition and enhance care delivery.
Data Management and Processing
Most participants acknowledged that additional resources would be necessary to process data from RMTs, including added clinician time or support from ancillary staff located in or out of the practice. Some participants stated that certain tasks, such as those associated with chronic disease management, could fall to medical assistants or nursing staff as this overlapped with current activities. Participants familiar with team-based approaches suggested that ancillary staff could provide initial data review and respond using specified protocols, allowing clinicians to limit their own engagement to high-risk patients. A physician (#7) noted, “…the data needs to go into a data hub [which] has alert parameters if anything is out of the normal range…. When we start getting patients that are out of range—our care coordinator [could] get on the telephone and intervene. Another stated,
…it would be overwhelming for an individual provider [to review the data]…you really have to be functioning with a care manager and with teams…so that the teams would have the same sort of plan of action that you talk about with the families for an asthma action planner…this is the red zone, this is the yellow zone, this is the green zone…and the medical assistant can manage this in the yellow zone, but when they’re getting into the red zone, they may have to bring the doctor on. (#10, Physician)
Barriers to Use
Perceived challenges to using RMTs in rural primary care included current payment structures, lack of patient motivation, limited staff capacity, and concerns over liability and potential changes to the doctor-patient encounter. Because clinicians relied on face-to-face encounters for revenue, some participants indicated they were unlikely to use RMTs unless payment reform occurred.
[Asking me about which technologies I’d prefer] is putting the cart before the horse…the ones that we would get reimbursed for would be the first ones we implement…. The reason we would have remote monitoring of whatever condition we’re following is to save the patient the expense of the office visit. So essentially we’re providing free care. So I wouldn’t see much…more of this happening without the issue of reimbursement being addressed. Then, depending on which ones [are] getting reimbursed, I would see that one getting utilized the most. (#6, Physician)
Other participants noted that even within current payment structures, clinicians were not paid to help manage a patient’s weight or deliver health behavior change counseling.
As noted earlier, clinicians expressed concerns over who would process and respond to the information, noting additional infrastructure would be needed. Clinicians wondered who would provide and service RMT hardware, as well as educate patients on use. Although some participants indicated that certain devices could be loaned to patients by the practice (eg, blood pressure monitors for a time-limited period), many indicated that equipment costs could not be covered by the practice. In particular, support for set-up and training on aging in place RMTs was perceived as occurring outside of the primary care setting.
…We have a nurse available in the clinic who is well versed in blood pressure and glucose monitoring and…I’m sure [she] could learn how to use the device and teach somebody to use it. Other than that, if the company had a representative that came out… [or if] they had a helpline [to call and say], ‘My [device] isn’t working’…. Maybe we can help them figure out the blood pressure monitor…but [for] the actual technical parts of the device…we have enough phone calls already. If we’re trying to troubleshoot technical difficulties…I don’t think we could support that very well. (#3, Physician)
Patient characteristics (eg, motivation, finances) were also noted as potential barriers to using RMTs in routine care. One physician (#8) stated, “My worry would be level of [patient] compliance…it would definitely be something that I could offer to a sufficiently motivated individual…[But] my worry is, it’s an excellent tool, but how often will it be used?” Participants also expressed concern that patients wouldn’t be able to afford the RMTs. A physician assistant (#9) described barriers in terms of monetary costs and capacity to use technologies, commenting: “[These technologies] probably would not be practical for the majority of [my] patients…. Most of them can’t read or write…and most…don’t have [access to] that kind of technology anyway.”
Finally, some participants noted that clinician characteristics could influence adoption of RMTs. A few clinicians raised questions about how RMT use would impact the patient-clinician interaction.
…there are probably some docs…who might not be so excited about these [technologies]. Whether it’s because they’re not tech savvy themselves or they worry about it affecting the face-to-face patient/doctor interaction, ‘cause now they’re interacting with numbers and computers. (#3, Physician)
Participants also expressed concern about legal responsibilities if health issues were detected, specifically who would be liable should the RMT identify a problem. A physician (#5) stated, “I see [these technologies as providing] more comprehensive care…you’re looking at more information and you know how a patient is doing…but if you become aware of it, then you have to deal with it.” For clinicians, a necessary step in technology adoption included developing parameters that could describe the appropriate values and determine who should respond to the data from the RMTs.
DISCUSSION
This study explored the interests and concerns of rural primary care clinicians to incorporating RMTs into routine patient care. Clinicians in our sample expressed interest in RMTs that closely aligned with the goals of primary care and could be implemented with minimal hassle for providers and patients. In our cross-case comparison we detected no consistent differences in perceptions toward RMTs by clinician training, age, gender, practice size, or other anticipated characteristics. Although we initially focused on the use of RMTs to enhance care for adults over 65 years in age, an emergent finding was that clinicians noted relevant technologies could be used with patients of all ages, not just for elders. Participants expressed interest in using RMTs to improve management of chronic disease and, in some cases, to support wellness activities. Although participants recognized the potential system-level benefits of using RMTs for post-hospital care and to enable aging in place, they raised questions regarding the feasibility of monitoring this data in primary care given current practice constraints. In particular, respondents indicated monitoring some types of RMT data might be better suited for other health professionals and/or families and caregivers.
Despite the potential role primary care clinicians play in responding to RMTs, few studies have explored their views regarding use and feasibility of adoption.24,25 As highlighted in Figure 3 and described in the results, participants noted how clinician, technology, patient, and supportive factors could influence technology adoption. Participants acknowledged the importance of effective RMT data management procedures, including direct transfer into EHR systems, availability in multiple formats, and the right amount of information to support action without inundating providers. Although ancillary staff could help review RMT data and potentially alleviate some of the additional time required to manage this new information, resources would be necessary to support such changes. Current payment models, patient motivation, underdeveloped data management parameters, and concerns about the impact on the patient-doctor encounter were noted as potential barriers to adoption of RMTs in rural primary care.
Our findings echo the views from studies of diverse clinical professionals and academicians conducted in 3 unique settings: Korea,34 metropolitan United States,24 and the United Kingdom.35 Clinicians in these studies noted: 1) the main driver for remote monitoring should be clinical need, 2) concern that RMTs could lead to changes in the patient-clinician encounter that could potentially reduce perceived quality of care, 3) uncertainty about responsibilities for data monitoring and the associated medical-legal implications, and 4) the potential additional burden on clinician and staff time resulting from poorly integrated systems and under-developed data management parameters.24,34,35 Our study adds to this body of literature by raising questions about the ideal target users of RMTs; although technologies supporting chronic disease management may align well with primary care, others may not. Additionally, findings indicate that changes in reimbursement structure may be necessary before widespread adoption is feasible. Data parameters and response guidelines, that are actionable by diverse members of a primary care team, are also needed.
There are a few limitations of the present study. First, our study was not restricted to a specific RMT device. Instead, we explored 4 broad categories noted in the literature by which health conditions and behaviors might be monitored. It is possible that exploring technologies for a specific condition may yield different findings. Second, participants had limited experience with RMTs, they but reported relative comfort using and interest in new types of HIT and consumer technologies. Engaging clinicians with greater experience using RMTs may have yielded more nuanced findings. Additionally, our clinician sample may have more positive views toward RMTs than would be found in the general primary care clinician population. However, we think skeptical yet receptive providers are the ideal target to inform HIT development and implementation studies. Finally, we interviewed rural clinicians from only 1 state, we did not include any nurse practitioners in our sample, and provision of care to older adults was a necessary characteristic for participant selection. To address some of these limitations, we recommend that future studies engage clinicians across multiple settings (urban, suburban and rural) and include other members of the primary care team (eg, medical assistants, nurses, billing staff, and office managers) who play an active role in the adoption of RMTs. Additionally, research is needed to explore how clinicians may use RMTs with pediatric populations. A survey utilizing a larger sample size may enable detection of nuances by participant and clinic characteristics that we were unable to find using a qualitative study design.
Despite these limitations our study presents critical findings that can inform development and adoption of RMTs in rural primary care settings and may also apply in urban contexts. Our study team utilized various approaches to ensure qualitative validity.36,37 This included using an ethical approach to data collection and having multiple reviewers independently review study transcripts and participate in the analysis. Use of multiple reviewers helps control for researcher bias, ensures internal validity of results, and allows for peer review/debriefing. We also engaged in external audits with senior qualitative researchers and informal member checking with rural clinicians.
Although participants expressed interest in some RMTs, it is unclear whether rural characteristics will facilitate or impede adoption over time. For example, although longer travel distances and fewer medical professionals may promote use of RMTs, the higher prevalence of uninsured or underinsured patients in rural areas may limit affordability and access to these emerging technologies.15,16 Although HIT adoption may lag in rural settings, recent studies suggest that a similar proportion of rural and urban practices have EMR systems.38 These delays in EHR adoption may be driven by practice size; smaller practices are less likely to have implemented systems.39,40 Therefore, despite clinician interest, mobilizing the financial and infrastructure resources to enable implementation of new technologies, such as RMTs, may be especially challenging for small, rural primary care practices. Policy makers interested in expanding RMT adoption are therefore encouraged to support payment reform that enables reimbursement for remote care and to aim incentives and support at small, rural practices.
RMTs represent a dynamic and emerging field. Our study and previous research emphasize the importance of engaging target users in all phases of technology development, from proof of concept through implementation. Hardisty and associates found that the primary challenge will be to address 2 translational research gaps: first in moving prototypes into the field through efficacy studies, then in supporting widespread implementation in routine practice.35 A recent review on the outcomes of e-health interventions noted that variability may be related to differential attendance to contextual factors during implementation.4 We speculate that implementation of patient-centered medical homes (PCMH)41 and emergence of accountable care organizations (ACOs)42 may reduce current barriers to RMT use in primary care by providing incentives to collaborate and proactively manage patient care. For example, Community Health Workers, one element of some PCMH and ACO initiatives, may extend the boundaries of primary care and facilitate adoption of RMTs. Ultimately, for RMTs to benefit all potential users, practicing primary care clinicians must be involved in product development, testing, and implementation.43
Acknowledgments
Funding: Funding for this project is provided by the Oregon Roybal Center for Translational Research on Aging (P30AG024978) at Oregon Health & Science University (OHSU), Portland, Oregon, and by a Clinical and Translational Science Award to OHSU (National Institute of Health/National Center for Research Resources Grant No. 1 UL1 RR024140 01).
We thank the rural clinicians who participated in this research and the clinic staff who made it possible. We appreciate the input of Drs. Kaye and Eckstrom on study development. Nicole Larimer, Tracy Zitzelberger, and the Oregon Center for Aging and Technology (ORCATECH) provided training on emerging remote monitoring technologies (RMTs). Deborah Cohen, PhD provided assistance with study methods and manuscript revisions. The authors also gratefully acknowledge the editing and publication assistance from Ms. LeNeva Spires.
Footnotes
The authors report no conflicts of interest.
References
- 1.Demiris G, Hensel BK. Technologies for an aging society: a systematic review of “smart home” applications. Yearb Med Inform. 2008:33–40. [PubMed] [Google Scholar]
- 2.Frisardi V, Imbimbo BP. Gerontechnology for demented patients: smart homes for smart aging. J Alzheimers Dis. 2011;23(1):143–146. doi: 10.3233/JAD-2010-101599. [DOI] [PubMed] [Google Scholar]
- 3.Martin S, Kelly G, Kernohan WG, McCreight B, Nugent C. Smart home technologies for health and social care support. Cochrane Database Syst Rev. 2008;(4):CD006412. doi: 10.1002/14651858.CD006412.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morrison LG, Yardley L, Powell J, Michie S. What design features are used in effective e-health interventions? A review using techniques from critical interpretive synthesis. Telemed J E Health. 2012;18(2):137–144. doi: 10.1089/tmj.2011.0062. [DOI] [PubMed] [Google Scholar]
- 5.Sarasohn-Kahn J. The connected patient - charting the vital signs of remote health monitoring. California Health Foundation; [Accessed March 29, 2013]. Available at: http://www.chcf.org/publications/2011/02/the-connected-patient. [Google Scholar]
- 6.Hill C. Tech to track your aging parents. [Accessed January 20, 2011];Smart Money. 2011 Jan 13; Available at: http://www.smartmoney.com/personal-finance/elder-care/tech-to-track-your-aging-parents-1294880369537/
- 7.Olson EG. The virtual doctor visit: Health monitoring at home. [Accessed March 29, 2013];The Washington Post. 2009 Nov 17; Available at: http://www.washingtonpost.com/wp-dyn/content/article/2009/11/16/AR2009111602900.html.
- 8.Singer N. In a graying population, business opportunity. [Accessed March 29, 2013];The New York Times. 2011 Feb 5; Available at: http://www.nytimes.com/2011/02/06/business/06aging.html?pagewanted=all&_r=0.
- 9.Terry K. Home monitoring devices: why innovation doesn’t pay in healthcare. [Accessed February 3, 2011];MoneyWatch. 2010 May 25; Available at: http://www.bnet.com/blog/healthcare-business/home-monitoring-devices-why-innovation-doesn-8217t-pay-in-healthcare/1396.
- 10.Burrill & Company. [Accessed August 27, 2012];Digital Health Takes Hold with Venture Investors, says Burrill & Company: First half of 2012 sees private financings nearly double for the emerging sector. Available at: http://www.burrillandco.com/content/news/PR-Month-End%20July%202012-v4.pdf.
- 11.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. [Accessed February 11, 2011];Joint principles of the patient-centered medical home. Available at: http://www.pcpcc.net/content/joint-principles-patient-centered-medical-home.
- 12.Kaye J, Hayes T. Home health monitoring: A system to assess motor and cognitive function. Generations. 2006 Summer;:61–63. [Google Scholar]
- 13.Alwan M, Nobel J. State of Technology in Aging Services: Summary. Center for Aging Services Technologies; Mar, 2008. [Accessed August 27, 2012]. Available at: http://www.leadingage.org/uploadedFiles/Content/About/CAST/Resources/state_technoloy_summary.pdf. [Google Scholar]
- 14.Tai-Seale T, Chandler C. Nutrition and Overweight Concerns in Rural Areas: A Literature Review. Rural Healthy People 2010: A companion document to Healthy People 2010. College Station, TX: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- 15.Geyman JP, Norris TE, Hart LG. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001. [Google Scholar]
- 16.Loue S, Quill BE. Handbook of Rural Health. New York, NY: Kluwer Academic/Plenum Publishers; 2001. [Google Scholar]
- 17.Health Resources and Services Administration (HRSA) [Accessed January 16, 2011];HRSA Data Warehouse. 2009 Available at: http://datawarehouse.hrsa.gov/
- 18.Institute of Medicine. Committee on the Future of Rural Health Care. Quality Through Collaboration: The Future of Rural Health. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 19.Schoenman J, Keeler J, Moiduddin A, Hamlin B. Roadmap for the Adoption of Health Information Technology in Rural Communities. Bethesda, MD: NORC Walsh Center for Rural Health Analysis; 2006. [Google Scholar]
- 20.Mountain G, Craig C. What do people really want? Meeting the needs of people with early dementia and their carers through technology. Gerontechnology. 2010;9(2):69–70. [Google Scholar]
- 21.Demiris G, Hensel BK, Skubic M, Rantz M. Senior residents’ perceived need of and preferences for “smart home” sensor technologies. Int J Technol Assess Health Care. 2008;24(1):120–124. doi: 10.1017/S0266462307080154. [DOI] [PubMed] [Google Scholar]
- 22.Boise L, Wild K, Mattek N, Ruhl M, Kaye J. Attitudes of non-naïve older adults toward continuous, unobtrusive in-home monitoring of activity. Gerontology. In press. [Google Scholar]
- 23.Demiris G, Rantz M, Aud M, et al. Older adults’ attitudes towards and perceptions of “smart home” technologies: a pilot study. Med Inform Internet Med. 2004 Jun;29(2):87–94. doi: 10.1080/14639230410001684387. [DOI] [PubMed] [Google Scholar]
- 24.Thompson HJ, Thielke SM. How do health care providers perceive technologies for monitoring older adults? Conf Proc IEEE Eng Med Bio Soc. 2009:4315–4318. doi: 10.1109/IEMBS.2009.5333599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin S, Rankin G. Using commercially available technology to assist in the delivery of person-centered health and social care. J Telemed Telecare. 2002;8 (Suppl 2):60–62. doi: 10.1177/1357633X020080S228. [DOI] [PubMed] [Google Scholar]
- 26.Kang JM, Yoo T, Kim HC. A wrist-worn integrated health monitoring instrument with a tele-reporting device for telemedicine and telecare. IEEE Trans Instrum Meas. 2006;55(5):1655–1661. [Google Scholar]
- 27.Oregon Health & Science University (OHSU). Oregon Rural Practice-based Research Network (ORPRN) [Accessed September 1, 2012]; Available at: www.ohsu.edu/orprn.
- 28.University of Washington Rural Health Research Center. [Accessed December 31, 2012];Using RUCA Data. Available at: http://depts.washington.edu/uwruca/ruca-uses.php.
- 29.Cohen DJ, Crabtree BF. Evaluative Criteria for Qualitative Research in Health Care: Controversies and Recommendations. Ann Fam Med. 2008;6(4):331–339. doi: 10.1370/afm.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuzel A. Sampling in qualitative inquiry. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research. 2. Thousand Oaks, CA: Sage Publications; 1999. pp. 33–45. [Google Scholar]
- 31.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 32.Crabtree BF, Miller WL. Doing Qualitative Research. 2. Thousand Oaks, CA: Sage Publications, Inc; 1999. [Google Scholar]
- 33.Khan S, VanWynsberghe R. Cultivating the under-mined: Cross-case analysis as knowledge mobilization. Forum Qual Soc Res. 2008;9(1):Art 34. [Google Scholar]
- 34.Kim J, Kim S, Kim H, Kim K, Yang S, Shin Y. Development of implementation strategies for u-health services based on the healthcare professionals’ experiences. Telemed J E Health. 2011;17(2):80–87. doi: 10.1089/tmj.2010.0124. [DOI] [PubMed] [Google Scholar]
- 35.Hardisty AR, Peirce SC, Preece A, et al. Bridging two translation gaps: A new informatics research agenda for telemonitoring of chronic disease. Int J Med Inf. 2011;80(10):734–744. doi: 10.1016/j.ijmedinf.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Cohen DJ, Crabtree BF. Evaluative Criteria for Qualitative Research in Health Care: Controversies and Recommendations. The Annals of Family Medicine. 2008;6(4):331–339. doi: 10.1370/afm.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Whittemore R, Chase SK, Mandle CL. Validity in Qualitative Research. Qual Health Res. 2001;11(4):522–537. doi: 10.1177/104973201129119299. [DOI] [PubMed] [Google Scholar]
- 38.Singh R, Lichter MI, Danzo A, Taylor J, Rosenthal T. The Adoption and Use of Health Information Technology in Rural Areas: Results of a National Survey. J Rural Health. 2012;28(1):16–27. doi: 10.1111/j.1748-0361.2011.00370.x. [DOI] [PubMed] [Google Scholar]
- 39.DesRoches CM, Worzala C, Joshi MS, Kralovec PD, Jha AK. Small, Nonteaching, And Rural Hospitals Continue To Be Slow In Adopting Electronic Health Record Systems. Health Aff (Millwood) 2012;31(5):1092–1099. doi: 10.1377/hlthaff.2012.0153. [DOI] [PubMed] [Google Scholar]
- 40.Decker SL, Jamoom EW, Sisk JE. Physicians In Nonprimary Care And Small Practices And Those Age 55 And Older Lag In Adopting Electronic Health Record Systems. Health Aff (Millwood) 2012;31(5):1108–1114. doi: 10.1377/hlthaff.2011.1121. [DOI] [PubMed] [Google Scholar]
- 41.Stange K, Nutting P, Miller W, et al. Defining and Measuring the Patient-Centered Medical Home. J Gen Intern Med. 2010;25(6):601–612. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luft HS. Becoming Accountable — Opportunities and Obstacles for ACOs. N Engl J Med. 2010;363(15):1389–1391. doi: 10.1056/NEJMp1009380. [DOI] [PubMed] [Google Scholar]
- 43.Bitterman N. Design of medical devices--a home perspective. Eur J Intern Med. 2011 Feb;22(1):39–42. doi: 10.1016/j.ejim.2010.09.017. [DOI] [PubMed] [Google Scholar]