Abstract
Problem/Objectives
Permanent childhood hearing loss has major negative impacts on children’s health and development. To improve outcomes, universal newborn hearing screening (UNHS) has been implemented widely. However, high-quality evidence on its efficacy was lacking. To address this evidence gap, we conducted the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study to directly compare outcomes of early- and late-identified children. This paper investigates whether early performance measured shortly after initial amplification predicts language development at 3 years of age.
Methodology
This is a prospective, population-based study. We assessed outcomes at 6- and 12-months after amplification, and then at 3 and 5 years of age. Main outcome measures included directly-assessed language, receptive vocabulary, speech production; and parent-reported functional performance in everyday life. A range of demographic and audiological information was also collected at evaluation intervals.
Results
About 450 children participated, and 3-year outcomes scores were available for 356 participants. Multiple regression analysis revealed that early language scores or functional performance ratings were significant predictors of 3-year outcomes. Other significant predictors included the presence or absence of additional disabilities, severity of hearing loss, and age at cochlear implant activation.
Conclusions
Early performance, either directly-assessed language ability (PLS-4) or parent-reported functional ratings (PEACH), were significant predictors of 3-year outcomes; along with presence or absence of additional disabilities, severity of hearing loss, and age at CI activation. Earlier implantation is possible with early detection of hearing loss via UNHS. Monitoring performance after initial amplification allows preventive strategies to be implemented early to improve outcomes.
Keywords: Child, deafness, universal newborn hearing screening, outcomes
Introduction
About 3/1000 children are fitted with hearing aids or receive cochlear implants by school entry for a permanent hearing loss.1 The presence of hearing loss has major adverse developmental and health impacts on children’s lives2 – including speech and language,3 literacy,4 mental health,5 social and cognitive functioning,6 educational achievement,7 employment and socio-economic opportunity.8 Lifetime cost of all care and lost productivity was estimated to be USD117 million per birth cohort of 80,000 children.9 Universal newborn hearing screening (UNHS) programs offered new hope for treatment to begin in infancy by reliably detecting deafness soon after birth. The ultimate goal of UNHS is to improve long-term developmental outcomes, at a population level. Such programs are very costly, and previous systematic reviews of their efficacy for improving outcomes have revealed a lack of high-quality evidence due to epidemiological and methodological flaws in previous studies.10,11 To address the evidence gap, we commenced a prospective study to directly compare outcomes of early- and late-identified children – the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study (www.outcomes.nal.gov.au).
We took advantage of a narrow time window during which states in Australia were at staggered stages of implementing UNHS programs to recruit sufficiently large numbers of children who had differential access to the programs but received the same post-diagnostic hearing services administered by a single national government-funded service provider, Australian Hearing (AH). The longitudinal study aimed to examine whether UNHS and early intervention improve child outcomes, at a population level; and to determine what factors influence spoken language development. Details of the study were reported in Ching et al.12 Briefly, children were evaluated at 6 and 12 months after initial intervention, and at chronological ages of 3, 5, and 9 years. A range of outcomes, including functional ability, speech perception, speech production, receptive and expressive language, literacy, educational attainment, mental health, social development, and quality of life, were measured using age-appropriate standardized tests. Information about demographic and audiological characteristics that potentially affect outcomes (based on published literature) was collected prospectively around the same time as evaluations.
Early language development paves the foundation for later educational and academic attainment. Quantifying the predictive strength of early development for later outcomes offers the opportunity for preventive intervention early on, thereby reducing the lifelong impact of cumulative disadvantage. The LOCHI study was designed with this purpose in mind. In this paper, we aimed to quantify the contribution of early scores, in combination with other demographic characteristics of the LOCHI cohort, to language outcomes at 3 years of age. The early scores were either directly-assessed English language scores or parent-reported aural/oral functional performance ratings. The former measure is suitable for children from English speaking background; the latter is applicable for children from any language background.
Method
The LOCHI study is a prospective, population-based study of outcomes of children with hearing loss. The AH service network provided the sampling frame for this study. Children born between 2002 and 2005 in three Australian states, New South Wales, Victoria, and South Queensland, who were identified with hearing loss and accessed hearing services at AH paediatric centres before 3 years of age, were invited to participate. The only exclusion criterion was an indication by the parent that the family did not wish to be contacted for research purposes. This study was approved by the Human Research Ethics Committee of Australian Hearing.
Procedures
Written information was provided to all invited families, and researchers obtained written informed consent to participation from parents of children. Parents were also asked to provide consent for researchers to access their child’s data held at the AH database or other healthcare service providers as appropriate. At 6 or 12 months after initial hearing-aid fitting, and again when the children turned 3 years of age, parents were requested to complete custom-designed written questionnaires on demographic characteristics and to provide ratings of their child’s development. The questionnaires were sent to parents prior to direct evaluations of children, and were collected either at or soon after the assessments. Children were directly assessed by a team of experienced speech pathologists using standardised normed tests of speech and language. Direct assessments were video- and audio-recorded, and randomly selected samples constituting at least 10 percent of the total were subjected to a second, independent scoring. The inter-rater reliability was 97 percent.
Measures
Direct assessment measures included the Preschool Language Scale, version 4 (PLS-4),13 the Peabody Picture Vocabulary Test (PPVT-4),14 and the Diagnostic Test of Articulation and Phonology (DEAP).15 Parent report tools included the Child Development Inventory (CDI),16 and the Parents’ Evaluation of Aural/oral Performance of Children (PEACH).17 Audiological measures included hearing loss severity, defined as the four-frequency pure-tone average (4FAHL) dB HL across 0.5, 1, 2 and 4 kHz in the better ear within 6 months of the date of evaluation; device, hearing-aid prescription for fitting, presence or absence of auditory neuropathy spectrum disorder (ANSD). Demographic measures included child sex, birth weight, presence or absence of additional disabilities, highest level of education of parents, whether English was the child’s first language, communication mode at home and in early education, and the census-based Relative Advantage and Disadvantage Index for postcode of residence (IRSAD, with higher scores reflecting relatively greater advantage).18
Statistical analysis
The Statistica software19 and R20 with additional R packages were used for analysis. Missing data were handled by using multiple imputations.21 The primary outcome measures were summarised in terms of means and standard deviations. To determine the predictability of 3-year outcomes from earlier performance scores, multiple linear regression analysis was used. Factor analysis was initially performed to combine test scores from 9 measures (PLS-4 Auditory comprehension score, PLS-4 Expressive Communication score, PPVT-4 receptive vocabulary score, DEAP consonant correct score, DEAP vowel correct score, CDI Language Comprehension score, CDI Expressive Language score, CDI Social score, and PEACH score) into a global outcomes score. Fifteen predictor variables were included in the analyses. These included 10 categorical variables: gender, device (hearing aids or cochlear implants), additional disability (present or absent), ANSD (present or absent), communication mode in early education (no intervention, oral mode, other [including oral + manual combined mode as well as manual only]), change in communication mode during educational intervention (not attending or no change, changed from oral mode to other, changed from other to oral mode), communication mode at home (oral mode or other), language used at home (English or other), maternal education (≤ 12 years of schooling, certificate or diploma, university), and hearing-aid prescription (DSL or NAL); and 5 continuous variables: age at first-fitting of hearing aids, age at activation of first cochlear implant, birth-weight, socio-economic status (expressed as IRSAD scores), and 4FA HL. Interaction terms of device x age at fitting and device x 4FA HL were included.
The earlier PLS-4 and PEACH scores were obtained at least one year before the 3-year assessment, at either 6 or 12 months after hearing-aid fitting depending on data availability. Separate multiple regression analyses were performed using the global factor score as a dependent variable and the 15 predictor variables. Firstly, the significance of early PLS-4 score was examined by fitting models without or with early PLS-4 as a predictor. Secondly, the significance of early PEACH score was examined by fitting regression models without or with early PEACH score as a predictor.
Results
Table 1 summarizes the outcomes data for children at 3 years of age. On average, children’s spoken language scores were below age expectations, achieving language and speech production scores at 1 SD below normative mean. By contrast, receptive vocabulary, social, self-help, fine motor, and gross motor skills were approximately normal, and close to expectations for a typically developing group.
Table 1.
Mean standard scores, standard deviations (SD), 25th, 50th and 75th percentiles.
| Measures | Valid N | Mean | SD | Median (50th percentile) | 25th Percentile | 75th Percentile |
|---|---|---|---|---|---|---|
| PLS_Auditory comprehension | 312 | 78.4 | 24.7 | 76.5 | 53.0 | 102.0 |
| PLS_Expressive communication | 310 | 84.7 | 19.3 | 82.0 | 71.0 | 99.0 |
| PPVT_Receptive vocabulary | 226 | 87.5 | 16.7 | 88.0 | 76.0 | 100.0 |
| DEAP_Consonants | 194 | 80.6 | 16.6 | 78.9 | 68.4 | 92.7 |
| DEAP_Vowels | 194 | 81.4 | 27.6 | 87.2 | 72.1 | 97.9 |
| CDI_Social Quotient | 302 | 86.4 | 36.1 | 80.3 | 66.7 | 105.0 |
| CDI_Self-help Quotient | 302 | 88.8 | 33.4 | 89.2 | 70.0 | 105.3 |
| CDI_Fine motor Quotient | 301 | 93.0 | 28.9 | 94.6 | 81.0 | 108.3 |
| CDI_Gross motor Quotient | 302 | 84.9 | 35.5 | 84.6 | 60.5 | 105.4 |
| CDI_Expressive Language Quotient | 284 | 75.8 | 30.6 | 77.1 | 62.8 | 89.6 |
| CDI_Language Comprehension Quotient | 284 | 72.2 | 28.1 | 74.3 | 55.3 | 91.7 |
| PEACH | 241 | 71.0 | 21.2 | 75.0 | 59.1 | 86.4 |
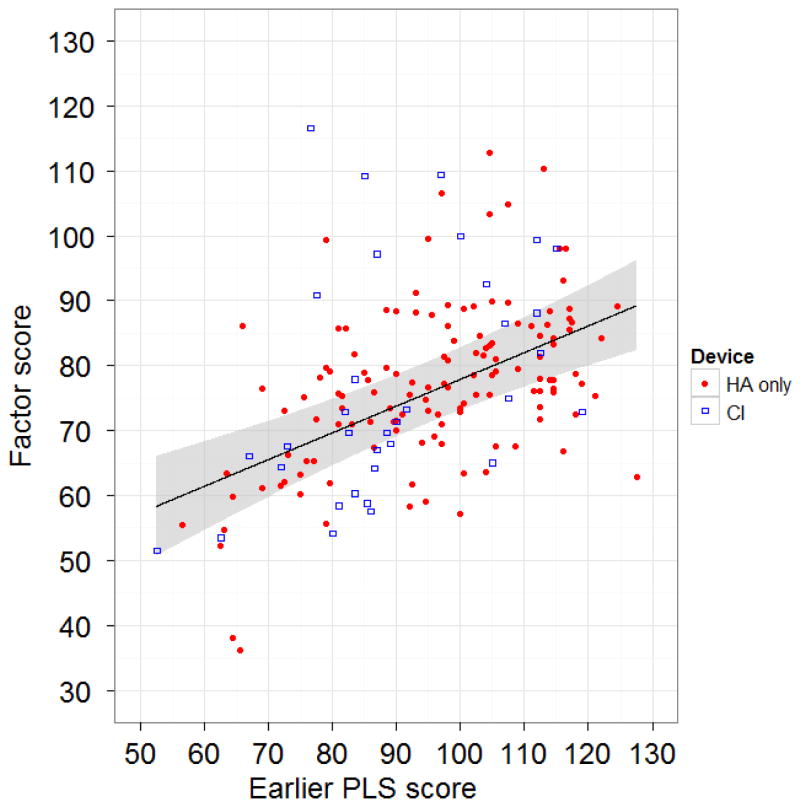
Data from 356 children who had scores on at least two test instruments were included in the factor analysis to derive a global outcomes score. Of these, 169 had an earlier PLS-4 score that was obtained at least one year before the 3-year assessment. Table 2 compares the models fit without or with early PLS-4 score as a predictor. The average R2 value was 0.40 for the model without the early PLS-4 score, and 0.49 for the model with early PLS-4. The statistical significance (p value) of predictor variables and the associated impact in terms of global outcomes scores are shown. The impact represents the effect size associated with a change from one category to another for categorical variables; or a change from one value to another as specified for continuous variables. Significant predictors of developmental outcomes at 3 years included the presence or absence of additional disabilities, gender, severity of hearing loss, maternal education and age at cochlear implant (CI) activation. Once early PLS-4 was included as a predictor, gender and maternal education were no longer significant at the 5% probability level. Figure 1 shows the 3-year global outcomes score in relation to early PLS-4 scores, separately for children with hearing aids (HA) and those for cochlear implants (CI).
Table 2.
Multiple regression summary table for 3-year outcomes, without or with earlier PLS-4 score as a predictor. Estimates of the impact of significant predictors (marked by asterisks), together with 95% confidence interval (CInt) are shown for the change in the mean of the dependent variable associated with a change in the predictor from the first to the second value specified in the Predictor column, with the other predictors held constant.
| Predictor | Without earlier PLS | With earlier PLS | ||
|---|---|---|---|---|
| p value | Impact (95% CInt) | p value | Impact (95% CInt) | |
| Other disability (present re absent) | <0.001* | −10.3 (−14.5, −6.1) | 0.004* | −6.5 (−11.0, −2.1) |
| Gender (Female re male) | 0.02* | 3.8 (0.6, 6.9) | 0.09 | - |
| Maternal education (university re school) | 0.007* | 6.2 (2.2, 10.3) | 0.14 | - |
| 4FA HL (43 to 85 dB HL) | 0.04* | −7.5 (−13.9, − 1.1) | 0.03* | −6.4 (−12.3, −0.5) |
| Age at CI activation (10 to 24 months) | 0.02* | −9.1 (−15.3, − 2.9) | 0.04* | −8.0 (−14.1, −1.9) |
| Birth weight | 0.07 | - | 0.98 | - |
| Communication mode in early intervention | 0.06 | - | 0.12 | - |
| Mode change in early intervention | 0.42 | - | 0.49 | - |
| SES | 0.07 | - | 0.05 | - |
| English at home | 0.13 | - | 0.65 | - |
| Communication mode at home | 0.39 | - | 0.57 | - |
| Hearing aid prescription | 0.59 | - | 0.68 | - |
| Age at HA fitting | 0.55 | - | 0.12 | - |
| Auditory neuropathy | 0.65 | - | 0.67 | - |
| Device: HA or CI | 0.74 | - | 0.61 | - |
| Early PLS-4 (each unit score) | <0.001* | 0.4 (0.3, 0.6) | ||
Figure 1.
Outcomes at 3 years (global outcome factor score) in relation to earlier PLS-4 score. The solid line is the predicted value of the factor score as the earlier PLS-4 score varies, with early intervention mode fixed at oral only, no change in intervention mode over the first 3 years, maternal education fixed at diploma or certificate level, and other predictors fixed at their mean values. The shaded area shows the pointwise 95% confidence intervals for the mean values. Filled symbols depict scores of children with hearing aids (HA only), and open symbols depict scores of children with cochlear implants (CI).
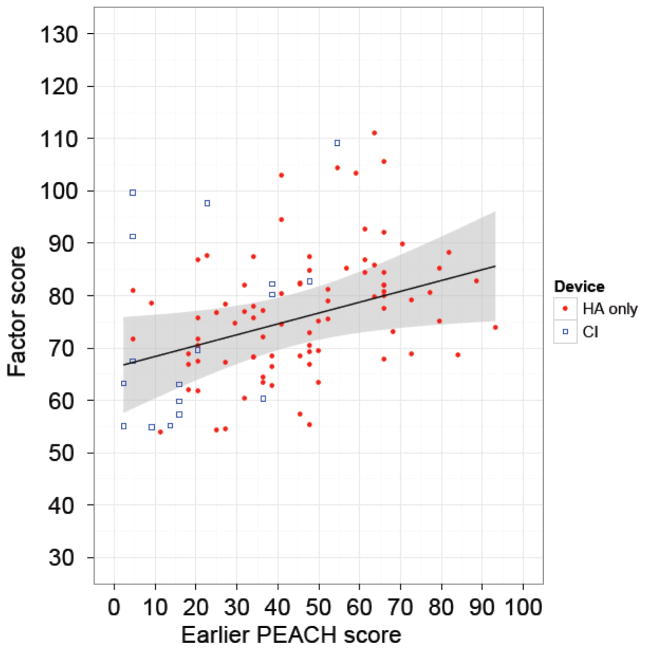
Of the 356 children with a global outcomes score at 3 years of age, 102 had an earlier PEACH score. The average R2 value was 0.40 for the model without early PEACH score, and 0.45 for the model with early PEACH score. Table 3 summarises the two models. Without the early PEACH score in the model, presence of additional disabilities, gender, severity of hearing loss, maternal education, birth weight, and age at CI activation were significant predictors of 3-year outcomes. Once early PEACH score was included, birth weight, gender and maternal education were no longer significant. Figure 2 shows the 3-year global outcomes score in relation to early PEACH scores, separately for children with HA and CI.
Table 3.
Multiple regression summary table for 3-year outcomes, without or with earlier PEACH score as a predictor. Estimates of the impact of significant predictors (marked by asterisks), together with 95% confidence interval (95% CInt) are shown for the change in the mean of the dependent variable associated with a change in the predictor from the first to the second value specified in the Predictor column, with the other predictors held constant.
| Predictor | Without PEACH | With PEACH | ||
|---|---|---|---|---|
| p value | Impact (95% CInt) | p value | Impact (95% CInt) | |
| Other disability (present re absent) | <0.001* | −10.4 (−14.3, −6.5) | 0.002* | −8.4 (−13.8, −3.0) |
| Gender (Female re male) | 0.01* | 4.0 (0.9, 7.1) | 0.10 | - |
| Maternal education (university re school) | 0.005* | 6.6 (2.5, 10.7) | 0.05 | - |
| 4FA HL (43 to 85 dB HL) | 0.04* | −7.8 (−14.8, − 0.8) | 0.04* | −6.5 (−13.5, 0.4) |
| Age at CI activation (10 to 24 months) | 0.02* | −9.1 (−15.5, − 2.7) | 0.03* | −9.3 (−16.1, −2.5) |
| Birth weight (2.6 to 3.6 kg) | 0.02* | 2.3 (0.04, 4.7) | 0.17 | - |
| Communication mode in early intervention | 0.05 | 0.11 | ||
| Mode change in early intervention | 0.42 | 0.36 | ||
| SES | 0.05 | 0.11 | ||
| English at home | 0.10 | - | 0.17 | - |
| Communication mode at home | 0.38 | - | 0.24 | - |
| Hearing aid prescription | 0.54 | - | 0.70 | - |
| Age at HA fitting | 0.61 | - | 0.20 | - |
| Auditory neuropathy | 0.56 | - | 0.99 | - |
| Device: HA or CI | 0.70 | - | 0.55 | - |
| Early PEACH (each unit score) | 0.03* | 0.2 (0.02, 0.4) | ||
Figure 2.
Outcomes at 3 years (global outcome factor score) in relation to earlier PEACH score. The solid line is the predicted value of the factor score as the earlier PEACH score varies, with early intervention mode fixed at oral only, no change in intervention mode over the first 3 years, maternal education fixed at diploma or certificate level, and other predictors fixed at their mean values. The shaded area shows the pointwise 95% confidence intervals for the mean values. Filled symbols depict scores of children with hearing aids (HA only), and open symbols depict scores of children with cochlear implants (CI).
Discussion
The primary goal of this paper was to investigate the strength of early performance, together with a range of predictor variables, for predicting developmental outcomes at 3 years of age. We found that performance scores obtained at 6 or 12 months after initial amplification, whether they were specific English language scores obtained through direct assessment of a child (PLS-4) or general functional performance scores based on parent reports (PEACH), accounted for a significant proportion of variation in 3-year global outcome scores. This finding has important clinical implications. The identification of increased risk of low language or functional status within a year of initial amplification makes it possible for early remediation. Alternative strategies, including but not limited to cochlear implantation, more intensive educational intervention, or alternative communication modes, would be necessary to avoid further delays for children at risk of language deficits. Standard care of children with permanent childhood hearing loss needs to include vigilant monitoring of child performance for optimising outcomes.
Early English language (PLS-4) scores, or early functional performance (PEACH) ratings, combining with severity of hearing loss, presence of additional disabilities, and early age of CI activation explained 45% – 49% of the variation in language development at 3 years of age. Delaying implantation from 10 to 24 months of age was associated with a reduction of 8–9 global factor score points. Given that the global factor score has been scaled so that a normal population should have a mean of 100 and a standard deviation of 15 points, a reduction of 8 points represents a more than one-half standard deviation shift in outcomes, which is a substantial decrement. Previous studies have reported on the advantage of early CI,22 but none reported on the effect of age at CI activation at a population level after controlling for a range of demographic variables, nor quantified the degradation of outcomes as a function of age at CI activation. Consistent with previous population studies,23 we found that more severe hearing loss was associated with poorer outcomes. For children with hearing aids, a change from moderate to severe degrees of 4FA HL in the better ear was associated with a decrease in 6.4 factor score points.
For the models which did not include early scores (PLS-4 or PEACH) as a predictor, maternal education, gender, and birth weight were also significant at the 5% probability level. These findings are consistent with other studies on outcomes of young children with normal hearing.24 None of these variables was significant after allowing for the effects of early scores.
Other predictor variables that would be of clinical interest were the presence of ANSD and choice of hearing-aid prescription for fitting. Neither of the variables met the 5% significance level, after allowing for the effects of other variables in the models. No previous studies had quantified the impact of ANSD at a population level and allowed for the range of demographic characteristics as in the present study; and reported findings were mostly based on case studies or convenience samples (see a review by Roush et al).25 The choice of hearing-aid prescription was not a significant predictor, even though one prescription provided much higher gain than the other for the same degree of hearing loss.26 The mean effect size of each of these variables is very close to zero, which is neither statistically nor clinically significant.
Strengths of the study
This is the first population-based study to directly examine whether early performance predicted later outcomes in children with hearing loss. This study extends findings from previous studies by measuring a range of outcomes prospectively and controlling for the effects of a wide range of demographic characteristics collected during the same time period.
Limitations
These findings are applicable only to children at 3 years of age. Whether outcomes at later ages may be predicted on the basis of early performance remains to be investigated. By design, this longitudinal study will assess the children at 5 and 9 years of age. It will then be possible to quantify the predictive strength of early measures for outcomes at an older age.
Conclusion
This population study shows that early measures of either language ability or functional performance shortly after initial amplification were significant predictors of 3-year outcomes; along with presence or absence of additional disabilities, severity of hearing loss, and age at CI activation. Early implantation is possible with early detection of hearing loss via UNHS. Monitoring of performance after initial amplification allows preventive intervention to be implemented to optimise outcomes.
Acknowledgments
We gratefully thank all the children, their families and their teachers for their participation.
We also thank the many persons who served as habilitationists for the study participants or assisted in other clinical or administrative capacities at Australian Hearing, Cochlear Implant Centre of the Royal Victorian Eye and Ear Hospital, Hear and Say Centre, St Gabriel’s School, the Royal Institute for Deaf and Blind Children, the Shepherd Centre, and the Sydney Cochlear Implant Centre. We also thank Linda Cupples, Greg Leigh, Patricia Van Buynder, Sanna Hou, Vicky Zhang, Angela Wong, Jessica Thomson, Lauren Burns, Scott Brewer, Jessica Sjahalam-King, Christopher Flynn, Kathryn Crowe, and Nicole Mahler-Thompson for their assistance and support.
Sources of funding:
The project described was partly supported by Award Number R01DC008080 from the National Institute On Deafness And Other Communication Disorders. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute On Deafness And Other Communication Disorders or the National Institutes of Health. Support was also provided by the Office of Hearing Services in Australia, Department of Health in New South Wales, Phonak Ltd., and the Oticon Foundation. We also acknowledge the financial support of the Commonwealth of Australia through the establishment of the HEARing CRC and the Cooperative Research Centres Program.
Footnotes
To be presented at:
Annual Congress of the Belgian ENT Society, 14–16, November, 2013, Brussels, Belgium.
References
- 1.Australian Hearing. Report on demographics of persons under the age of 21 years with hearing aids. Australian Hearing; Chatswood, Australia: 2011. [Google Scholar]
- 2.Helfand M, Thompson DC, Davis R. Systematic Evidence Review Number 5. Oregon Health & Science University Evidence-based Practice Center; Rockville: 2001. Newborn Hearing Screening. [Google Scholar]
- 3.Moeller MP, Tomblin JB, Yoshinaga-Itano C, Connor CM, Jerger S. Current state of knowledge: Language and literacy of children with hearing impairment. Ear Hear. 2007;28(6):740–753. doi: 10.1097/AUD.0b013e318157f07f. [DOI] [PubMed] [Google Scholar]
- 4.Conrad R. The Deaf Schoolchild: Language and Cognitive Functioning. Harper & Row; London: 1979. [Google Scholar]
- 5.Hindley PA, Kitson N. Mental Health and Deafness: a multidisciplinary handbook. Whurr Publishers; London: 2000. [Google Scholar]
- 6.Marschark M. Cognitive functioning in deaf adults and children. In: Marschark M, Spencer PE, editors. Deaf studies, language and education. Oxford University Press; New York: 2003. pp. 464–477. [Google Scholar]
- 7.Powers S. The educational attainments of deaf students in mainstream programs in englad: examination results and influencing factors. Am Ann Deaf. 1999;144(3):10. doi: 10.1353/aad.2012.0154. [DOI] [PubMed] [Google Scholar]
- 8.Dye MW, Kyle JG. Deaf People in the Community: Demographics of the Deaf community in the UK. Deaf Studies Trust; Bristol: 2000. [Google Scholar]
- 9.Keren R, Helfand M, Homer C, McPhillips H, Lieu TA. Projected cost-effectiveness of statewide universal newborn hearing screening. Pediatrics. 2002;110(5):855–864. doi: 10.1542/peds.110.5.855. [DOI] [PubMed] [Google Scholar]
- 10.Thompson DC, McPhillips H, Davis RL, Lieu TL, Homer CJ, Helfand M. Universal newborn hearing screening: Summary of evidence. JAMA. 2001;286(16):2000–2010. doi: 10.1001/jama.286.16.2000. [DOI] [PubMed] [Google Scholar]
- 11.Nelson HD, Bougatsos C, Nygren P 2001 US Preventive Services Task Force. Universal newborn hearing screening: Systematic review to update the 2001 US Preventive Services Task Force recommendation. Pediatrics. 2008;122(1):e266–276. doi: 10.1542/peds.2007-1422. [DOI] [PubMed] [Google Scholar]
- 12.Ching TY, Dillon H, Marnane V, Hou S, Day J, Seeto M, Crowe K, Street L, Thomson J, Van Buynder P, Zhang V, Wong A, Burns L, Flynn C, Cupples L, Cowan RS, Leigh G, Sjahalam-King J, Yeh A. Outcomes of early- and late-identified children with hearing loss at 3 years of age: Findings from a prospective population-based study. Ear Hear. 2013 doi: 10.1097/AUD.0b013e3182857718. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmerman I, Steiner VG, Pond RE. Preschool Language Scale. 4. The Psychological Corporation; San Antonio, Texas: 2002. (PLS-4) [Google Scholar]
- 14.Dunn LM, Dunn LM. Peabody picture vocabulary test. 4. Pearson Assessments; Minneapolis: 2007. [Google Scholar]
- 15.Dodd B, Zhu H, Crosbie S, Holm A, Ozanne A. Diagnostic Evaluation of Articulation and Phonology. Harcourt; London: 2002. [Google Scholar]
- 16.Ireton H. Child Development Inventory. Child Development Review; Minneapolis: 2005. [Google Scholar]
- 17.Ching TY, Hill M. The Parent’s Evaluation of Aural/Oral Performance of Children (PEACH) Scale: Normative data. J Am Acad Audiol. 2007;18(3):220–235. doi: 10.3766/jaaa.18.3.4. [DOI] [PubMed] [Google Scholar]
- 18.Australian Bureau of Statistics. [Last accessed 1st November, 2011];Information paper: an introduction to Socio-Economic Indexes for Areas (SEIFA) 2006 (ABS cat. No. 2039.0) Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2039.0Main%20Features32006.
- 19.Statsoft Inc. STATISTICA software. 7.1. Statsoft Inc; Tulsa, OK: 2005. [Google Scholar]
- 20.R Development Core Team. R: A language and environment for statistical computing. 2.13.1. R Foundation for Statistical Computing; [Last accessed 1st November, 2011]. Retrieved from http://www.r-project.org/ [Google Scholar]
- 21.Rubin DB. Multiple imputation for nonresponse in surveys. Wiley; New York: 1987. [Google Scholar]
- 22.Tomblin JB, Barker BA, Spencer LJ, Zhang X, Gantz BJ. The effect of age at cochlear implant initial stimulation on expressive language growth in infants and toddlers. J Speech Lang Hear Res. 2005;48(4):853–867. doi: 10.1044/1092-4388(2005/059). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wake M, Hughes EK, Poulakis Z, Collins C, Rickards FW. Outcomes of children with mild-profound congenital hearing loss at 7 to 8 years: A population study. Ear Hear. 2004;25(1):1–8. doi: 10.1097/01.AUD.0000111262.12219.2F. [DOI] [PubMed] [Google Scholar]
- 24.Reilly S, Wake M, Ukoumunne OC, Bavin E, Prior M, Cini E, Conway L, Eadie P, Bretherton L. Predicting language outcomes at 4 years of age: Findings from early language in Victoria study. Pediatrics. 2010;126(1):e1530–e1537. doi: 10.1542/peds.2010-0254. [DOI] [PubMed] [Google Scholar]
- 25.Roush P, Frymark T, Venediktov R, Wang B. Audiologic management of auditory neuropathy spectrum disorder in children: A systematic review of the literature. Am J Audiol. 2011;20(2):159–170. doi: 10.1044/1059-0889(2011/10-0032). [DOI] [PubMed] [Google Scholar]
- 26.Ching TY, Dillon H, Hou S, Zhang V, Day J, Crowe K, Marnane V, Street L, Burns L, Van Buynder P, Flynn C, Thomson J. A randomised controlled comparison of NAL and DSL prescriptions for young children: Hearing aid characteristics and performance outcomes at 3 years of age. Int J Audiol. 2013 doi: 10.3109/14992027.2012.705903. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]