Abstract
Background and Aims: The 830 nm GaAlAs diode laser has played an extremely active role in low level laser therapy (LLLT) since the early 1980's. Recently, the author modified his original proximal priority laser technique (PPLT), and the current article set out to explain the improved approach and show scientific evidence for its efficacy.
Laser Therapy System: The laser therapy system used was based on the GaAlAs diode (OhLase-3D1, JMLL, Japan), delivering 60 mW in continuous wave at a wavelength of 830 nm in the near infrared with a power density at the tip of the probe head of approximately 1.2 W/cm2.
Proximal Priority Laser Technique: Under the author's PPLT concept, the brain is the control center for the body so every other part of the body is distal to the head. The main blood supply to the head is through the carotid arteries, and the deep penetration of the 830 nm beam applied to the side of the neck can involve and photoactivate the external and internal carotids, increasing the blood supply to the brain and creating a systemic parasympathetic system-mediated whole-body effect. The author has added gentle neck-stretching, trunk-stretching and his distal tissue softening approaches concomitant with the irradiation which enhance treatment efficacy.
Results: Real-time fine-plate thermography has revealed whole-body warming as a result of the PPLT, with applications including chronic pain attenuation, female infertility and functional training of paraplegic cerebral palsy patients. The warming effect had a latency from hours to days, increasing in intensity and latency with subsequent PPLT sessions. Both Doppler flowmetry and SPECT have shown increased cerebral and systemic blood flow following PPLT.
Conclusions: PPLT is easy to deliver and offers tangible results in a large range of conditions, enhancing the efficacy of diode laser LLLT.
Keywords: Whole body warming, parasympathetic system, SPECT, thermography, Doppler flowmetry, chronic pain, female infertility
Introduction
The author started working on developing the first 830 nm GaAlAs diode therapeutic laser in collaboration with Matsushita Electronic Company, Ltd, in 1980, and the efficacy of a 15 mW prototype battery-operated system was first reported for pain attenuation in 1981 during the 4th meeting of the International Society for Laser Surgery and Medicine, “Laser Tokyo 81”. 1) The first commercial system from Matsushita appeared in 1982. Between 1982 and 1988, the author worked on developing his own improved version of the system which was finally available in 1988 as the first generation of the OhLase-3D1, and associated with the birth of the term “Low Level Laser Therapy” (LLLT) from Ohshiro and Calderhead in the same year in the publication of “Low Level Laser Therapy: A Practical Introduction” published by John Wiley and Sons, Chichester UK, 2) and the launching of the journal Laser Therapy's Pilot Issue in the same year, also from Wiley, UK.
In the early days of the use of LLLT at the Ohshiro Clinic weekly Pain Clinic, many different methods and doses were tried empirically for a large range of pain-related conditions to try and elucidate the ideal treatment technique, and the ideal dosimetry for all different pain types. In the course of this treatment evolution period, one particular patient had a great influence on the establishment of the first iteration of the Proximal Priority Technique. An elderly male presented with chronic knee pain, but he was ambulatory. As was the technique at the time, the author concentrated point-by-point treatment in contact mode around the knees. The pain was at first alleviated, but after a few days the pain returned and then was exacerbated to the point where the patient could no longer walk, and he additionally developed severe pain of the lower back. He was admitted to hospital, and X-ray evaluation reveled severe stenosis of the spinal cord at the L4/L5 level. The author therefore started his next LLLT session from above the stenotic area, and worked down towards the knees. All pain was relieved after 6 weeks' treatment, and the patient remained pain free over a long follow-up. From this, the author worked out his orginal proximal priority technique, particularly for chronic pain, and started all treatment for any entity, no matter where the painful site was, from the neck, working around the base of the skull to irradiate the C1/C2 area. The efficacy of this approach was shown in a retrospective study on recalcitrant chronic lumbar pain of various aetiologies in a patient population of 542, achieving an immediate average overall efficacy of 81.6%, which was 82% at the end of an 8-week follow-up period. 3)
Over the recent decade, the author has further refined the technique, and the second generation PPLT has been developed and tested. This has been reported in a number of articles from the author's group on several topics including lower limb lymphangioma, hypertrophic scars and keloids, and therapy-resistant female infertility 4-7). The author's pain clinic has treated a total of 8,889 patients (as of December 4th, 2012), and the results of the present study are based on the experiences of treating this large number of patients, even though they are for the most part without unirradiated controls. The improved technique still involved irradiation of the neck, but on any area on the skin surface of the neck rather than along the base of the skull as before, and began to be combined with some gentle stretching during the irradiation period. This was found not only to loosen up the musculature in the involved area, but to treat the target condition and accentuate the whole body systemic effect, from irradiation of only the neck. The present article explains the proximal priority laser technique in detail and examines some objective assessments of the effect and efficacy of the new generation of PPTL.
Laser Therapy System
The system used in the author's clinic is the latest and a highly sophisticated generation of the OhLase-3DI (JMLL, Tokyo, Japan, Fig. 1), engineered to full Japanese Ministry of Health, Labour and Welfare (Japanese equivalent of the FDA) compliance, and registered with the Ministry as a therapeutic laser device. This is a standard mains-powered console-based system, with parameters being set by the user from the console which also contains the power supply and the microprocessor-based monitoring circuitry. The console is connected to the ergonomically-designed hand-held probe by a flexible cable. Laser energy is generated by 3 confocal GaAlAs diodes precisely mounted in the probe head, delivering 20 mW each to give a total of 60 mW at the focal point. The diodes are under-pumped (rated output 40 mW each) to avoid overheating which would alter the wavelength, and to prolong diode life. Output from each diode is constantly monitored by the onboard processor control circuitry, and in the extremely unlikely event of the output falling below a certain level an audible warning alerts the user, and a visible indicator on the console display panel indicates to the user which of the three diodes is at fault.
Fig 1:
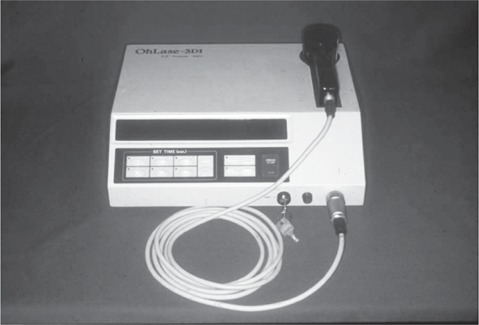
OhLase-3D1 system as used in the present study.
The system delivers the 60 mW output at the deep-penetrating near-infrared wavelength of 830 nm in continuous wave, with an irradiated area in contact mode at the tissue of 0.05 cm2, giving an irradiance at tissue of 1.2 W/cm2. Laser energy is delivered through an antireflective window mounted flush on the replaceable probe tip which both protects the laser diode optics from ingress of any contaminating debris, helps to eliminate loss of laser energy from the stratum corneum through reflection (as high as 14% at 830 nm) and also allows gentle compression of the target tissue in the contact mode. When contact mode is selected, (the system default), skin sensors in the probe tip detect the presence of the target tissue, so that from a safety viewpoint laser emission can only occur with the probe in contact with tissue.
Proximal Priority Laser Technique (PPLT)
The author's PPLT can be classified under three main procedures: the first, second and third procedures. In the first two irradiation is applied on to any area around the neck in contact laser therapy, and the third procedure involves a combination of neck irradiation and distal side irradiation with a number of application techniques. These are described and illustrated with a case report.
1. The 1st Procedure of PPLT (Neck Stretching Approach)
The 1st Procedure of PPLT can be called the “Neck Stretching Approach”
A careful patient work-up is conducted to preclude the presence of any pre-existing pathology (any malignant tumor, pregnancy, existence of implanted pacemaker, etc.,) or medical condition which might contraindicate this technique, and which excess motion of the neck, spine, lower torso or hips might exacerbate. Before treatment, the resting state of the head and neck is measured at rest on a specially-constructed goniometer (Fig. 2a). The open left and right neck angles are both 90° (Fig. 2b). The patient is asked to stretch his head to one side and the other, and the open left and right angles of the neck are measured, respectively, to ascertain which side has the greater freedom of movement. The patient is then asked to lift his leg straight up, and the angle between the leg (i.e., longitudinal axis of the femur) and the horizontal is measured for alternate legs.
Fig 2:
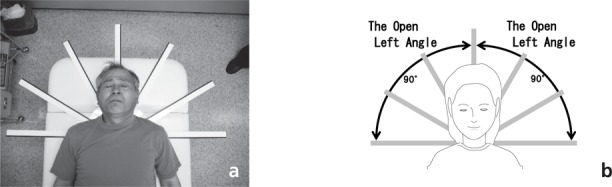
Patient with his head and shoulders on the specially-ted range of motion (ROM) goniometer prior to PPLT session with the he e relaxed central position.
In this patient's case, the pre-treatment open left neck angle (Fig. 3a: 128°) is larger than the pre-treatment open right neck angle (Fig.3c: 120°). The leg angle of the 1st procedure shows the angle between the horizontal line of the lateral condyle of the femur and the leg position after the 1st procedure.
Fig 3:
Bending the head (a, c): Bending to the left and right at the pretreatment baseline. (b, d): Result after PPLT session. Increased angles are evident for both the right and left. See the text for details.
From these findings, the right side of the neck is stiffer and in a more severe condition than the left side of the neck. In this case, we should treat the left side of the neck first which is the less stiff and less-severe side of the neck.
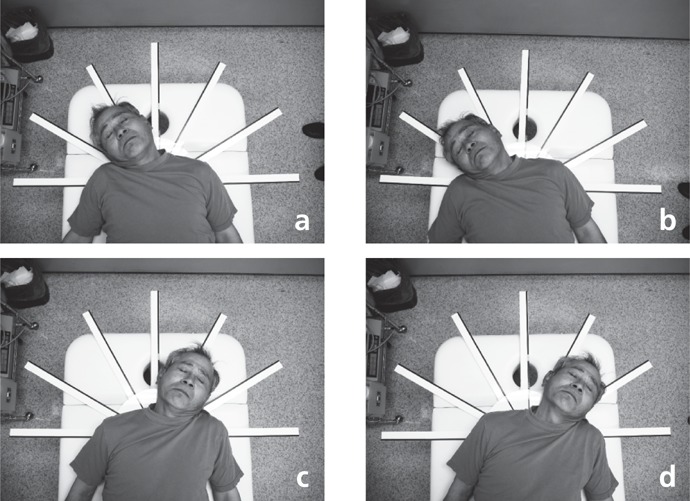
In the 1st PPLT Procedure, the laser should be applied to any area of the skin surface around the neck in contact therapy. After the 1st procedure to the left neck, the left neck muscle could be softened and stretched. The open left neck angle (Fig.3b: 143°) could be expanded compared with the pre-treatment angle (Fig.3a: 128°). The left leg angle after the 1st procedure (Fig.4a: 38°) was also be expanded compared with the pre-treatment angle (Fig.4b: 55°).
Fig 4:
Straight leg lifting. (a,c): Result for both legs at baseline, and (b, d) after the PPLT for the neck-stretching approach. Even though no other point that the neck was irradiated, the patient's leg lifting ahd improved. See the text for details.
After treatment of the left side, the right side of the neck should be treated, followed by softening and stretching of the right neck muscles. The open right neck angle after the 1st procedure (Fig.3d: 135°) could be expanded compared with the pre-treatment angle (Fig.3c: 120°). As with the left leg, the right leg angle after the 1st procedure (Fig. 4d: 62°) was expanded compared with the pre-treatment angle (Fig.4c: 48°).
2. The 2nd Procedure of PPLT (Trunk-Stretching Approach)
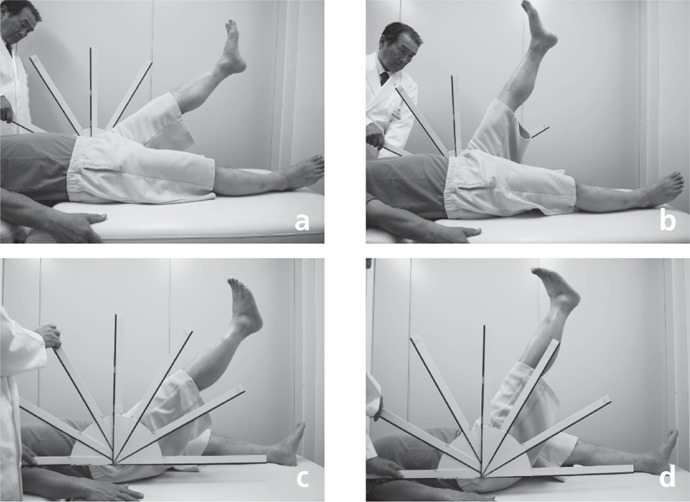
The 2nd Procedure of PPLT can be called the “Trunk Stretching Approach”. In the 2nd Procedure of PPLT, the laser probe should be applied to any area of the skin surface around the neck in contact therapy. The patient twists one leg across the body as far as possible (Fig. 5a), and the angle between the leg and the body is measured, repeated on the other side to obtain the baseline values. The laser is then applied to the neck for 8-15 sec, while the ipsilateral leg is gently stretched, and the angle measured again. This then repeated for the other leg. Finally, straight leg lifts are performed again as in the neck-stretching approach.
Fig 5:
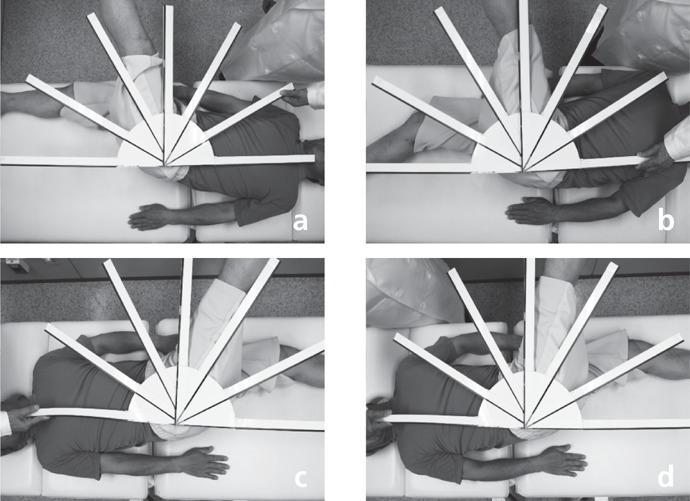
Trunk stretching approach. (a, c): Baseline results. (b, d) After a single PPLT session. The angle has improved for both legs. See the text for details.
In the same patient as in Fig. 5, the cross-body angles were 70° and 65° for the left and right legs, respectively (Fig. 5 a, c), and after treatment the angles were 85° and 80°, an increase of 15° for both legs (Fig. 5 b, d). The angles of lift for straight legs for left and right legs were 70° for both legs, respective increases of 15° and 8° for the left and right legs compared with the previous measurement at the end of the neck stretching approach (Fig. 6 a, b).
Fig 6:

Straight leg lifting performed after the trunk-stretching PPLT approach. The angle of lift is greater for both legs. See the text for details.
3. The 3rd Procedure of PPLT (Distal Tissue Softening Approach)
The 3rd Procedure of PPLT can be called the “Distal Tissue Softening Approach”. For conditions which fail to respond to the previous approaches, the author has developed a series of protocols which involve the distal tissue targets directly, with application of the laser to these distal areas, or with a manual manipulation of the area of interest with the laser applied to the neck as discussed above. In applying the PPLT, the laser system is usually used in pressure contact with the tissue, but users should be aware that a variety of techniques can be employed to vary the depth and volume of the penetration of LLLT energy.
Laser therapy can be applied to target tissue in two basic methods: the contact mode, and the noncontact mode. In the contact mode, as the name suggests, the laser is placed with the probe head in contact with the target tissue. Contact mode can be further subdivided into three different application types depending on the depth of the specific targets for the therapy. In noncontact mode, the laser is aimed and held at some distance from the target tissue. In both contact and noncontact modes it is important to keep the probe head at right angles to the plane of the target tissue to optimize penetration. And so, the 3rd Procedure of PPLT is subdivided into 3-1. Contact Mode and 3-2. Noncontact Mode.
3-1. Contact Mode:
With a laser system held in contact with the target tissue, the air gap is nonexistent and the reflection loss from the skin surface is minimized: this is enhanced in the current system by the nonreflective probe tip window. A higher incident photon density and more useful penetration depth are thus achieved, especially with the design of the OhLase-3D1 probe tip. The author has subdivided the contact mode into three different techniques: Probe Control, Clinician Digital Control and Patient Auto-control.
3-1-a. Probe Control
This method is controlled by the probe head of the laser machine.
3-1-a-1. Sweeping Method (Fig. 7a, Fig. 8a)
Fig 7:
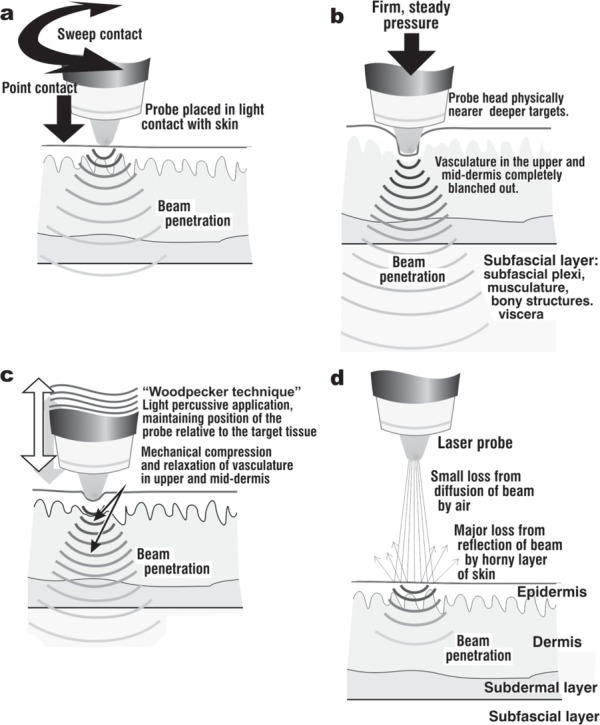
Techniques for probe control in the PPLT approach. (a): Noncontact method. (b): Contact sweeping method. (c): The author's “Woodpecker” technique. (d): Pressure contact mode. This is the mode usually recommended during PPLT sessions.
Fig 8:

Sweeping, Woodpecker and contact pressure methods illustrated in practice.
In the sweeping method, the laser is swept lightly backwards and forwards over the target tissue: this gives the most superficial penetration for targeting cells or organelles in the epidermal basal layer and the superficial dermis, and is useful for covering larger treated areas, but in a superficial manner. When the patient has some abnormal feeling over a large area of the skin surface, the clinician can sweep the skin surface with the probe head. In the probe control method, the local pathological area should be irradiated with the laser energy, in contact therapy.
3-1-a-2. Pressure Method (Fig.7b, Fig.8b)
This is the method recommended for the PPLT, and involves holding the probe head against the target point and applying firm but gentle pressure. The design of the probe head of the currently described system allows movement of the probe into the target tissue, blanching out blood vessels, gently moving muscle tissue aside and bringing the probe tip (and hence the laser energy) nearer to the main targets which in the case of PPTL are the carotid arteries. Penetration of 830 nm laser energy for some centimeters into tissue can be achieved with this method (Fig.7b). Fig. 8b illustrates probe control in action, with the exception of the noncontact mode. The probe head can be pressed onto any kind of pressure point (tender point, acupuncture point, trigger point, sympathetic ganglion etc.).
3-1-a-3. Percussive Technique (Fig. 7c, Fig. 8c and 8d)
In this method the laser is gently struck against the target tissue in a series of gentle percussive “Woodpecker” motions. It has the effect of mechanically moving the laser probe head intermittently nearer the deeper tissue by pure pressure, and at the same time it mechanically compresses and releases the blood microvasculature and lymphatic vessels in the target tissue. In the case of venules, veins and lymphatics, this has the effect of increasing flow rate and volume. This method enables penetration of the 830 nm beam to targets in the deeper dermis and fascia layer (Fig. 7c).
When the patient has some abnormal feeling in the deep layer and over a large area of the skin, the clinician can hit the skin with the probe head in the woodpecker manner.
3-1-b. Clinician Digital Control:
Clinician digital control, as the name suggests, is practiced by the clinician in addition to the laser therapy aspect, and has two subsets.
3-1-b-1. Two-point Finger Pressure (Fig. 9 a, c)
Fig 9.
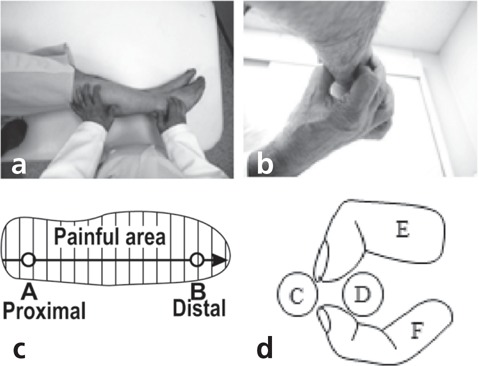
Clinician digital control illustrated in practice and schematically. (Left panel): Two-point finger pressure, observing proximal priority. (Right panel): Pinch pressure technique with (e, f) tendons or bone being pinched by finger and thumb (e, f).
This is used for a painful condition which is located over a larger or longer area. The laser is held against the lateral aspect of the neck using the pressure contact method on the side corresponding to the pain, but this is not essential. While this is done with the usual 8-15 s exposure time, the doctor then locates the patient's painful or tender zone, identifying it in a linear pattern, running from the proximal starting point to the distal ending point (Fig. 9a, c). This line may be along the anatomical pathway of an artery, nerve or muscle, or a combination of these. The clinician then applies alternating pressure to the proximal and distal points. This is repeated till the pain or discomfort is controlled. This method is controlled by the doctor's fingertips. In the case of this method, any area of the skin around the neck should be irradiated in the contact method. The clinician then places his or her fingertips along the line corresponding to the patient's abnormal tender feeling. These lines are usually identified along the pathway of the nerve, artery, vein, lymph duct and others. Any kind of the tenderness should be taken from the proximal to distal point of the line. (Proximal Priority Technique: PPT)
3-1-b-2. Pinch Pressure (Fig. 9b, d)
This can be used when treating pain in a bony structure or tendon. In this case, as for the previous two-point method, the laser is held against the lateral aspect of the neck using the pressure contact method. With his or her finger or thumb, the clinician then firmly pinches and holds the target tendon or bone between finger and thumb (Fig. 9b, d). This is repeated until the pain has been controlled.
In this method, the skin surface on any area around the neck is irradiated with the laser in the contact method. The clinician pinches the space between the bones C and D or the space behind the D tendon, with his or her thumb and finger.
3-1-c. Patient auto-control (Fig.10a, b)
Fig 10:
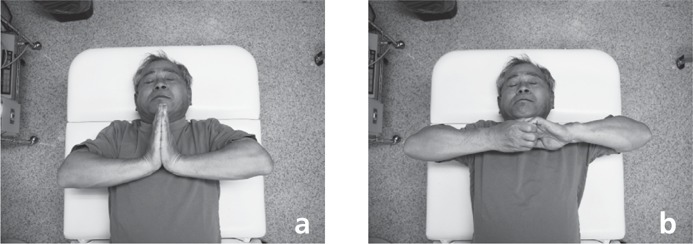
Patient auto-control approach, showing two calisthenic exercises with the patient in the supine position and the laser probe being applied to the neck. (Left panel) the hands pushing against each other with as much force as possible and (right panel) trying to pull apart from each other.
This method is controlled by the bilateral hands of the patient. The patient him- or herself then performs a set of calisthenic exercises by either pushing their hands against flat each other, or trying to pull their clasped hands apart.
3-3-1. Hands Pressure Method (Fig. 10a)
In this method, the skin surface on any area around the neck is irradiated with the laser in the contact method. The patient should press his or her bilateral palms together strongly, with as much force as they can for the duration of the laser irradiation (Fig. 10a). This is repeated till the desired result is achieved.
3-3-2. Hands Pull-out Method (Fig. 10b)
In this method, the skin surface on any area around the neck is irradiated with the laser in the contact method. At the same time, the patient should grasp his or her bilateral hands strongly and try to pull them apart (Fig.10), with as much force as they can for the duration of the laser irradiation (Fig. 10b). This is repeated till the desired result is achieved.
3-2. Noncontact Mode: (Fig.7d)
Noncontact mode is usually only applied for conditions which prohibit the contact mode, such as infected lesions including examples such as vasculogenic or other ulcers, or burn wounds. There are several important considerations when using an LLLT system in noncontact mode.
3-2-a. Highly Devergent
The diode laser beam is usually highly divergent, so the incident power density will dramatically drop with the increase in spot size, which in turn decreases the useful penetration depth.
3-2-b. Air Gap
The air gap between the laser head and the target tissue will weaken the incident power of the beam by scattering, again limiting the penetration depth. The beam will be more prone to penetration loss by reflection from the surface of the target tissue.
From the foregoing, it is clear that noncontact mode is useful only for extremely superficial targets, but in the therapy of long-term vasculogenic ulcers and burn wounds the target cells are actually very often located in the superficial zones, and noncontact therapy can be accompanied by contact treatment around the periphery of the target wound to increase the efficacy, which can be enhanced in combination with PPLT.
Results and Discussion
The results from the PPLT studies referenced above in the past few years have borne out the efficacy of LLLT plus PPLT, including one trial which compared the efficacy of LLLT on its own with the combination of the two in the treatment of hypertrophic scars and keloids. 6) The efficacy of laser therapy applied via the PPLT to induce fertility in females who have not responded to conventional infertility therapy has been well-covered in the journal, especially in the review by the author of his own personal experience. 8)
There many theories as to why this approach works. However the literature has pointed to the efficacy of irradiation of the stellate ganglion for a number of entities, where the main mechanism was shown to be related to activation of the parasympathetic system. 9-11) In addition to irradiating the carotids, there is no doubt that the laser energy delivered by PPLT may also involve the stellate ganglions, thereby activating the descending inhibitory pathway and further enhancing whole-body messaging.
Fig. 11 shows the whole body warming phenomenon in a female patient being treated with PPLT for serious infertility. This system, the ‘rest and digest' system, ensures whole body relaxation and removes any sympathetic hypertension caused by the other component of the autonomous nervous system, the sympathetic ‘fight or flight' system. With the relaxation of the muscles which is part of parasympathetic dominance, the arterial walls will also relax promoting increased blood flow and oxygenation of the tissues being fed by the vessels. At the same time, hypertensive patients may experience a drop in blood pressure towards normal.
Fig 11:
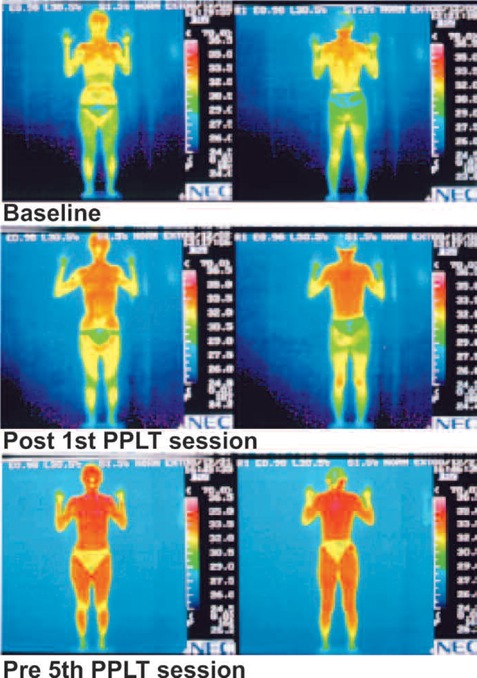
Sequence of whole body warming illustrated with fine-plate thermography for a female patient with severe infertility undergoing the PPLT approach, comparing base-line pretreatment with the findings after the first treatment and prior to the 5th treatment. Degree of full-body heating is clearly apparent. Left hand images: Front view. Right-hand images: Rear view.
A study demonstrated increased flow in the carotid arteries following a session of PPLT. 12) Following PPLT on one side of the neck in 12 human subjects, increased blood flow was seen in the irradiated side (63%), and the cross-sectional diameter of the external carotid increased (69%) as assessed objectively with color Doppler flowmetry. Interestingly, on the unirradiated side, increased blood flow and cross-sectional volume were also seen (71% and 52%, respectively), so the blood flow on the unirradiated side actually increased to a greater extent than on the irradiated side. These changes persisted for more than an hour before they started to decrease back to the normal baseline readings.
Single photon emission tomography (SPECT) is a diagnostic technique whereby a radioactive isotope tracer, the radionuclide, is injected into the subject. A scanner based on a i-camera then captures real-time 3-dimensional images of the tracer in the cerebral arteries, and a computer image is then able to depict changes in the cerebral blood flow in 3-D or in 2-D in any plane. Fig. 12 shows SPECT imaging compared between baseline and after a PPLT session in the same patient. Increased cerebral blood flow was clearly visible throughout the brain after the PPLT in both the transverse (Fig. 12 a-d) and sagittal planes (Fig. 12 c, d, top left images only,). Table 1 shows the computer-calculated rate of increased blood flow at two selected regions of interest (ROIs) of the brain compared between the baseline and post-PPLT images.
Fig 12:
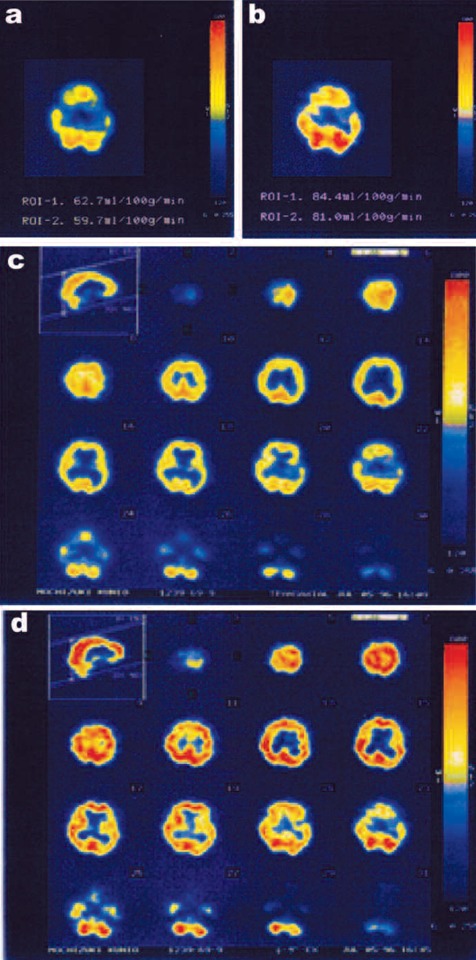
SP{ECT images showing increased cerebral blood flow comparing post-PPLT images with unirradiated baseline findings. (a, b) Transverse SPECT mages used to calculate increased blood flow in selected regions of interest (ROIs — see also Table 1) of the brain: ROI 1, right basal nuclei; ROI 2, posterior lobe. (c,d) Sagittal (top left) image and a complete series of transverse slices showing universal increased blood flow post-PPLT.
Table 1: Rate of increase of cerebral blood flow in selected regions of interest (ROI) at baseline and post PPLT as monitored by SPECT.
| Region of Interest | Location | Blood flow | Rate of Increase | |
|---|---|---|---|---|
| Baseline | Post PPLT | |||
| ROI 1 | Right basal nuclei | 62.7 ml/100 g/min | 84.4 ml/100 g/min | 36% |
| ROI 2 | Posterior lobe | 59.7 ml/100 g/min | 81.0 ml/100 g/min | 35% |
Conclusions
From both subjective assessment and objective assays, there is clearly apparent increased local, cerebral and systemic blood flow following PPLT procedures, with pain relief and feelings of general well-being in treated patients. Increased parasympathetic control is one of the major suggested reasons and would tend to be proved by the objective thermography, Doppler flowmeter and SPECT assessments. The results of this article would strongly suggest that the author's revised proximal priority laser technique is a viable manner in which to increase the efficacy of LLLT with the 830 nm GaAlAs laser as used in the parameters reported in the present study.
References
- 1: Calderhead RG, Ohshiro T, Itoh E, Okada T, Kato Y: The Nd:YAG and GaAlAs lasers; a comparative analysis in pain therapy. In Atsumi K, Nimsakul N, (eds). “Laser Tokyo 81”, Section 21 (Laser Acupuncture). Japan Society for Laser Medicine, Tokyo, Japan: 1981. pp 1-4 [Google Scholar]
- 2: Ohshiro T, Calderhead RG. Low Level Laser Therapy: A Practical Introduction. 1988, John Wiley & Sons, Chichester, UK [Google Scholar]
- 3: Ohshiro T, Shirono Y: Retroactive study in 524 patients on the application of the 830 nm GaAlAs diode laser in low reactive-level laser therapy (LLLT) for lumbago. Laser Therapy, 1992: 4: 121-126 [Google Scholar]
- 4: Ohshiro T: The proximal priority technique: how to maximize the efficacy of laser therapy. Laser Therapy, 2005, 14: 121-128 [Google Scholar]
- 5: Fujii S, Ohshiro T, Ohshiro T, Sasaki K, Taniguchi Y: Proximal priority treatment using the neck irradiator for adjunctive treatment of female infertility. Laser Therapy, 2007; 16: 133-136 [Google Scholar]
- 6: Sasaki T, Ohshiro T, Ohshiro T, FujiiSand Taniguchi Y: A prospective comparison between original LLLT and proximal priority theory (PPT) approaches for the treatment of hypertrophic scars and keloids. Laser Therapy, 2008; 17: 209-216 [Google Scholar]
- 7: Taniguchi Y, Ohshiro T, Ohshiro T , Sasaki K, Fujii S: Proximal priority treatment for lower extremity lymphangioma. Laser Therapy, 2009, 18:1 45-49 [Google Scholar]
- 8: Ohshiro T: Personal overview of the application of LLLT in severely infertile Japanese females. Laser Therapy, 2012; 21: 97-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9: Asagai Y, Sujaritpong T, Tranvan L, Ohshiro T: Assessment of changes in carotid blood flow following LLLT of the neck: Laser Therapy, 2007;16: 127-132 [Google Scholar]
- 10: Otsuka H, Okubo K, Imai M, Kaseno S, Kemmotsu O: Polarized light irradiation near the stellate ganglion in a patient with Raynaud's sign. Masui, 1992. November; 41: 1814-1817 (Japanese: abstract in English) [PubMed] [Google Scholar]
- 11: Lee CH, Chen GS, Yu HS: Effect of linear polarized light irradiation near the stellate ganglion in skin blood flow of fingers in patients with progressive systemic sclerosis. Photomed Laser Surg, 2006; 24: 17-21 [DOI] [PubMed] [Google Scholar]
- 12: Monobe H, Miyano K, Kagoya R, Tojima H: Case of progressive facial hemiatrophy with cervical sympathetic hyperactivity as underlying aetiology. J Laryngol Otol, 2012; 126: 725-728 [DOI] [PubMed] [Google Scholar]


