Abstract
A double-blind clinical trial was conducted on 30 female Temporomandibular Disorders (TMD) patients who had pain as a chief complaint. The patients were randomly allocated into three groups based on Low Intensity Laser (LILT) regimes namely 820 nm Gallium Aluminium Arsenide (GaAlAs) laser at energy densities of 21.4J/cm2, 107 J/cm2 and placebo laser. Each patient had three LILT treatments in a week. The pressure pain threshold (PPT) of trigger points in masticatory muscles, unassisted maximum mouth opening without pain (MOSP) and symptom severity index (SSI) were recorded as baseline data and monitored after every treatment. Jaw kinesiology, electromyography (EMG) and pain rating index from McGill pain questionnaire were also recorded as baseline and final results. The analysis of covariance and further analysis showed that the higher energy density laser group had significant increases in PPT and EMG amplitude recorded from voluntary clenching (cEMG) compared with the placebo group at P values 0.0001 and 0.022 respectively. A significantly greater number of patients recovered from myofascial pain and TMJ arthralgia as assessed clinically in the higher energy group compared with the placebo (P value = 0.02 and 0.006 respectively). There was no statistically significant difference in the other parameters of assessment among the groups at a P value 0.05. At a period of 2 to 4 weeks review after LILT, there was an average 52% reduction of pain as assessed by SSI.
Keywords: Myofascial Pain, Masticatory Muscle, Gallium Aluminium Arsenide Laser, VAS, EMG, Clinical Trial
Introduction
Temporomandibular disorder (TMD) pain may be divided into symptoms of muscular and joint origin. The former have been sub-divided into the progressive stages of protective co-contraction, local muscle soreness, myofascial pain (trigger point myalgia), myospasm and centrally mediated myalgia. In an orofacial pain clinic the commonest presentation is that of myofascial pain with trigger points seen in young females in their late teens and twenties — these are the type of cases reported in the study of Okeson [1]. The predominant attitude to treatment has always been recommended to be conservative treatments including physical self-regulation (PSR), occlusal splint, medication and physical therapy. The surgical treatment has been considered only as a last resort [1,2]. Among various physical therapy interventions, low intensity laser therapy (LILT) has been recognised to be one of the modalities for TMD. From the recent systematic review of a variety of physical therapies also found that the mid- laser therapy, of which the wavelengths at 830 nm and 904 nm can be categorised to be LILT, may reduce TMD pain, and improve total vertical opening. This therapy may be more effective than other electrotherapy modalities in short term [3]. However, two meta-analysis studies showed controversies over the effect of LILT on musculoskeletal pain [4,5]. There have been a number of studies illustrated benefits of LILT for the relief of TMD pain. Bezuur et al [6] found that The 904 nm low intensity laser could improve the mouth opening in an arthrogenous group. Gray et al [7] found that the 904 nm laser produced the larger number of TMD pain patients who had clinical improvement at a 3-month review by comparison with the placebo group. Bradley and Rehbini [8] reported on reported a change of EMG findings of the masticatory muscles after 820 nm GaAlAs irradiation of painful masticatory muscles in 88% of subjects. Conti [9] found that GaAlAs had an effect of pain reduction in a myogenous group and improvement in mouth opening in an arthrogenous group. Fikackova et al [10] found that 830 nm at 10 or 15 J/cm2 had a significant numbers of samples with pain reduction than the sham laser group. A clinical research of Shirani et al [11] stated that the combined 660 nm 6.2 J/cm2 with 890 nm 1 J/cm2 showed the significant pain reduction in the myofascial pain dysfuncation syndrome than the placebo. While the clinical trial by Emshoff et al [12] using 632.8 nm 1.5 J/cm2 in TMJ had no significant pain relief compared with the sham laser.
This may be from a disparity of the optimal LILT dosage for TMD pain relief and a limitation of evaluation method only on pain score. There has been still a wide range of recommendation. Baxter et al [13] suggested energy densities at 8 to 12 J/cm2. On the other hand, Arao et al [14] using a low power Nd:YAG laser at 350 mW for 15 minutes at a much high energy rating of at least 315 joules per point found positive improvement even in chronic internal derangement cases. The standard clinical trial regarded the methodology including placebo LILT, the adequate reports of site of laser exposure and dosage and appropriate outcome measurement as recommended by World Association of Laser Therapy [15] needs to be conducted to explore the influence of LILT on TMD pain.
This double blind- randomised placebo-controlled trial was set up in order to explore the influence of LILT on treatment outcomes of three groups of TMD patients (a conventional energy regimen, a modified high energy regimen and a placebo group) who had myofascial pain of masticatory muscle. The objective clinical outcomes were recorded using pressure pain threshold as a main assessment and other related parameters namely range of mandibular movements and electromyography. Subjective pain assessments using McGill pain questionnaire and Symptom Severity Index (SSI) were also compared among the groups
Materials and methods
Study population
Female TMD patients, attending the Royal London Dental Teaching Hospital were invited to take part in a double blind trial of LILT approved by the ethical committee of the Trust. The diagnosis was based on the research diagnostic criteria (RDC) for TMD [16]. The inclusion and exclusion criteria were summarised as follows:
1. Unilateral myogenous TMD with at least one trigger point in the muscles of mastication
2. Ages of 20-50 years
3. Chronic pain status; pain duration not less than 3 months
4. No severe systemic disease
5. No radiological abnormalities of the temporomandibular joint
Sample size assumption and allocation
The sample size estimation was calculated from the data of a previous study [17]. The study was conducted on 30 patients; 10 patients in each group. The sample allocation was based on a double blind randomised control trial and block allocation. All participants were randomly allocated into three groups depending on LILT regimes as follows:
Group 1; A conventional low energy LILT (CLILT) : 21.4 J/cm2, 4 J per point, 60 mW irradiance
Group 2; A modified high energy LILT (MLILT) : 107 J/cm2, 20 J per point, 300 mW irradiance
Group 3; Inactive laser (Placebo)
Laser apparatus and application
A Unilaser 301P (Asah Medico) comprising a 820 nm GaAlAs variable power probe (0 to 300 mW power) and 670 nm 1mW light guide was used in this trial (figure 1). The built in programme memory was set by another clinician. From the patient's viewpoint there was no possibility of recognising when the laser was active or inactive, or when it was delivering CLILT or MLILT. An insulating sleeve was used to prevent detection of any heating effect on the probe from the high energy MLILT regimen. Hence double-blinding was maintained. The placebo probe had no detectable 820 nm radiation but maintained the visible red 670 nm light guide active.
Fig.1:
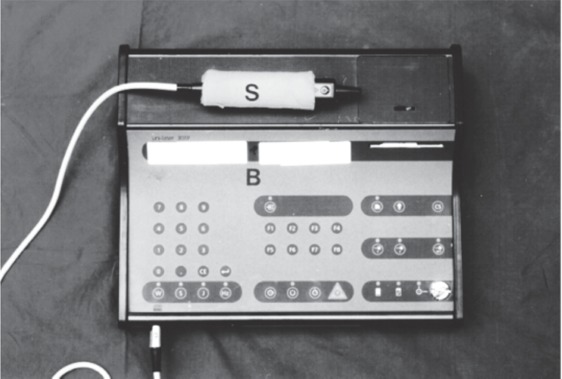
The modification of laser apparatus for the double blind trial
The modification for double blind purposes are shown namely: the laser apparatus with screen information cover blanked out (B), laser probe with an insulating sleeve (S) to prevent the experimenter detecting heating effects from the higher energy MLILT regime and the built in programme memories
The allocated energy dose was given by stationary in skin contact procedure to each patient at 6 sites:
1. Posterior aspect of the affected TM joint to irradiate the richest part of the innervation namely the auriculotemporal nerve. (jaw open) as shown in figure 2.
2. Sigmoid notch to irradiate the motor nerve to masseter and other elements of the mandibular division of the trigeminal nerve plus lateral pterygoid muscle insertion (jaw closed)
3. Joint interface to irradiate the synovium (jaw open) 4, 5, 6 Each of the three most tender trigger spots in the masticator muscles ellicited by palpation
Fig. 2:

The irradiation of the auriculotemporal nerve at the posterior aspect of the TMJ
Treatment and follow-up descriptions and schedules
The general format of the trial was that patients had baseline investigations carried out on the Thursday of the week preceding the start of LILT (day minus three). LILT and preliminary routine assessments were carried out on the following Monday, Wednesday and Friday with each regimen totalling 3 treatments. On Monday of the following week, full investigations were undertaken after the first 3 treatments which were used as the basis for assessment of response. The following investigations were undertaken during this overall period:
A. Base line investigation (day minus three)
1. Full oral and maxillofacial examination was performed. This annotates all aspects of TMJ function, oral status and muscular palpation. The standard questionnaires of RDC [16] McGill pain questionnaire and Symptom Severity Index (SSI) were completed.
2. Orthotomographic x-rays of both joints in open and closed positions (4 in 1 views).
3. The maximum mouth opening without pain (MOSP) was recorded by Willis Bite Guage.
4. An electronic algometer (Somedic AB, Stockholm, Sweden) with 1 cm2 probe tip and patient operated switch was used to measure PPT of standardised trigger point landmarks [18] on masseter and temporalis muscles on the affected side and the corresponding points on the control side. The slope of the exerted force was controlled at 10 kilopascal (Kpa) per second. The patient was sat upright in a high back rest arm chair position slightly clenching in the intercuspal position and informed to activate a switch when pressure turned to pain which stabilised the recorded value (figure 3). The records of PPT were shown in kpa.
5. Electromyography of masseter and anterior temporalis muscles was recorded by using the Myo-Tronics Computerised System (K6-I). The bipolar electrodes (Duo-trode disposable EMG electrode) were placed on the anterior temporalis and masseter muscles parallel to the fibres of the muscle on the sites of maximal contraction. Recording was taken in the relaxed position and also as an integrated recording during voluntary maximum clenching compriseing triple 2 second clenches with 2 second rest intervals.
6. Jaw tracking by using the Myo-Tronics Computerised System (K6-I) was recorded for a range of mandibular movements. Velocity of mouth opening and closing were also recorded.
7. Acetate templates were made individually for the positions of the EMG electrodes and algometry measurements to allow reproducibility.
Fig. 3:
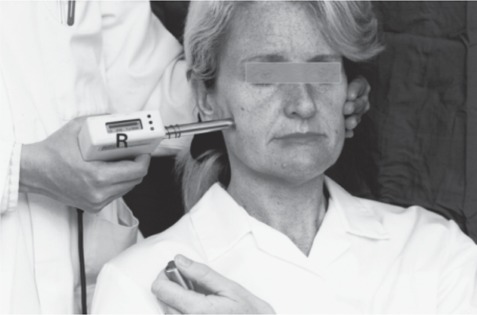
The irradiation of the auriculotemporal nerve at the posterior aspect of the TMJ
PPT of a trigger point on the masseter muscle being measured using the algometer. A constant force was applied at a 90 degree angle to the muscle with counterpressure support. The patient is holding the switch which is activated when the pressure turns to pain. The registration screen (R) is clearly seen.
B. Week 1 (Days 1, 3 and 5):
Pain score record, MOSP and PPT measurements followed by LILT
Final (Days 8)
Repeat of investigations of day minus 3 to assess response to the first three treatments.
C. Week following trial
For ethical reasons to ensure that all patients received therapy and for blinding the clinician, the control group was treated using MLILT for 3 alternate days in the second week while the experimental groups received the sham LILT also on 3 alternate days. The methods of assessments were similar to the first week.
Statistical analysis
Analysis of covariance (ANCOVA) fitting the repeated measure design was applied to compare the responses to the interventions among the groups. In the case where the data did not match the assumptions for ANCOVA, non-parametric statistical methods were performed using the Kruskal-Wallis method comparing the difference among groups. For comparing the categorical data between the groups, the Fisher's exact test was performed.
Results
General data
The average age of patients in the trial was 35 years old (SD = 9 years) in the range of 20 to 50 years old. The mean pain duration of symptoms of the total sample was 33 months in the range of 5 to 120 months.
Pain pressure threshold (PPT)
The pain pressure threshold of the worst trigger point as measured with the electronic algometer twice before treatment and after each treatment was regarded as the main result of this study. The means and the standard deviations (SD) measured at different time points are shown in table 1. The means of PPT of each groups at the time of assessments are also shown in line graph (figure 4).
Table 1: Means and the standard deviations (SD) of baseline and post-treatment PPT by group and time of assessments.
| Group & time | means PPT in kpa (SD) | ||||
|---|---|---|---|---|---|
| Baseline 1 | Baseline 2 | After 1 treatment | After 2 treatments | After 3 treatments | |
| CLILT Low energy | 66.1 (19.55) | 68.8 (22.08) | 71.0 (24.26) | 80.0 (24.73) | 85.2 (27.27) |
| MLILT High energy | 61.1 (16.89) | 62.4 (21.26) | 82.7 (35.68) | 99.0 (29.84) | 102.6 (32.21) |
| Placebo | 55.2 (19.16) | 57.9 (18.71) | 60.4 (15.19) | 61.2 (26.65) | 61.1 (27.57) |
Fig. 4:
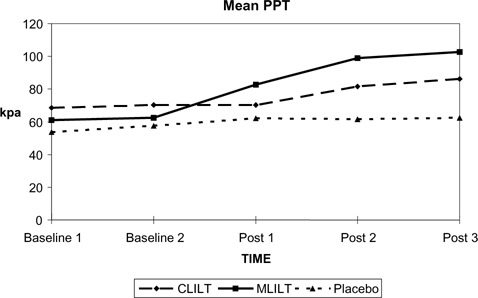
Means of pain pressure threshold (PPT) measured at pre and post-treatment
The means of PPT of the CLILT group was slightly increased after the second treatment (post 2). In the MLILT group, the mean PPT was markedly increased after the first treatment (post 1). The placebo group showed no obvious change after intervention. The ANCOVA which can correct the difference of baseline as observed performed to detect the differences of PPT among groups (table 2).
Table 2: Comparison of average PPT response to treatments over time by ANCOVA with the average of two baselines as a covariate.
| Sources of variation | Degree of Freedom | Mean Square | F | sig. of F | Observed power at the 0.05 level |
|---|---|---|---|---|---|
| Within + Residual | 26 | 243.62 | |||
| Regression | 1 | 12039.49 | 49.42 | <0.001 | 1.000 |
| Experimental group | 2 | 2155.71 | 8.85 | 0.001 | 0.953 |
Note: The normality of every dependent variable and covariate was tested by Shapiro-Wilks test (P value >0.05). The homogeneity of variance was tested by Cochrans C and Baretlett-Box F (P value = 0.366 and 0.543 respectively)
The significance of F for regression indicated that the slope of the average PPT after treatments predicted by the average PPT of baselines was not zero. The overall difference of PPT after three episodes of treatments among groups was compared using the mean of two baselines as a covariate variable and the mean of three post-treatment assessments used as a dependant variable. There was a statistically significant difference of the average PPT over the time of treatment among groups at P value 0.001. The power of the test for 30 patient sample size at the 0.05 level was 95%.
Further analysis was performed in order to examine the differences of the average PPT between groups using the adjusted means by the average of two baselines. Comparison of the differences of the average PPT between groups over time by T-test with adjustment for the average of two baselines as a covariate revealed the following results:
1. There was a statistically significant increase in the average PPT in the MLILT group compared with the placebo group at P value 0.0001. The difference of the mean PPT between these two groups was 27.99 kpa with a 95% confidence interval of the difference between means 13.14 to 42.82 kpa.
2. There was no significant difference of the average PPT between the CLILT and placebo groups at P value less than 0.05 although a trend towards increase was observed.
3. The average PPT of the MLILT group was also significantly increased in comparison with the average PPT of the CLILT group at P value 0.003. The difference between the means was 22.58 kpa (95% confidence interval of the difference 8.43 to 36.72 kpa).
4. A statistically significant difference of the average PPT after treatment between CLILT and placebo groups could not be obtained at P value less than 0.05.
Other related objective assessments
Other related assessments were undertaken on the maximum mouth opening without pain, the range of the mandibular movement and the electromyographic records in the rest position (rEMG) and maximum voluntary clenching (cEMG). The results from statistical analyses as follows:
1. A marginal statistically significant difference among the groups at P value = 0.051 (power of the test 58%) was found from the cEMG while no statistical significant differences among the groups at P value less than 0.05 could not be found from other assessments.
2. Further analysis was undertaken to examine differences of cEMG between groups comparing means adjusted by baseline. The cEMG of the MLILT group after the final treatment was statistically significantly higher than the placebo and CLILT group at P value 0.022 (95% confident interval of the difference = 5.96 to 68.66 microV) and 0.055 (95% confidence interval of the difference = −0.66 to 63.17 microV) respectively.
3. There was no statistically significant difference of cEMG between the CLILT and placebo groups.
Overall clinical improvement
The patients were diagnosed based on RDC for masticatory muscledisorder and arthralgia [16] before and after the final treatment.
Muscle disorders
All of the patients had myofascial pain as the inclusion criteria of the trial. The patients who did not have a possitive myofascial pain diagnosis (which was based on absence of pain on palpation of the masticatory muscles) were categorised to be in recovery status. The non-recovery category was the group of patients who still had myofascial pain of the masticatory muscle. The change of muscle disorder diagnosis is presented in table 3.
Table 3: The change of diagnosis for muscle disorders after the final treatment by groups.
| Group | Number of patients | |
|---|---|---|
| Recovery | Non-recovery | |
| CLILT | 4 | 6 |
| MLILT | 7 | 3 |
| Placebo | 1 | 9 |
Note: Recovery = No myofascial pain after treatments, Non-recovery = Patients still had myofascial pain after the final treatment.
From table 3, the largest number of the patients who had no myofascial pain diagnosis after the final treatment was in the MLILT group. In the CLILT group, there were 4 patients who had recovery while there was only one patient in the placebo group who had recovery. The Fisher's exact test was performed in order to compare differences of recovery from myofascial pain based on muscle disorder diagnosis.
The number of patients who recovered from myofascial pain in the MLILT group was significantly greater than the placebo group at P value = 0.0198. Moreover, the relative risk of the comparison showed that the MLILT was 3.5 times (95% confidence interval = 1.3 to 9.7) more effective than the placebo in terms of the numbers of patients who had myofascial pain relieved while there was no such difference by comparing the CLILT group with the placebo group at P value less than 0.05.
Fig. 5:
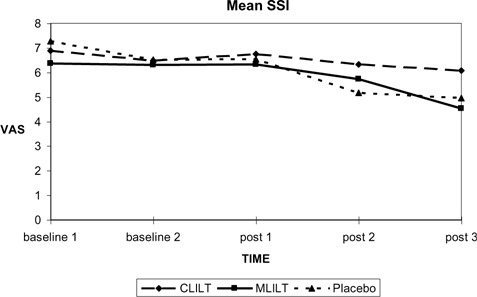
Means of SSI measured at pre and post treatments
Arthralgia
The diagnosis for the TMJ was categorised either as nil diagnosis for TMJ or arthralgia as determined by clinical examination according to RDC which involves determining whether there is pain on palpation over the capsule of the TMJ. The patients who did not have a TMJ arthralgia diagnosis were categorised to be in recovery status. The non-recovery category was the group of patients who still had TMJ arthralgia. The change of TMJ arthralgia after the final treatment is shown in table 4.
Table 4: The change of TMJ arthralgia diagnosis after the final treatment.
| Group | Number of patients | |
|---|---|---|
| Recovery | Non-recovery | |
| CLILT | 4 | 6 |
| MLILT | 8 | 2 |
| Placebo | 1 | 9 |
Note: Recovery = No TMJ arthralgia was diagnosed after the final treatment, Non-recovery = Patients still had or developed TMJ arthralgia after the final treatment
The majority of patients (8 patients) in the MLILT group had no diagnosis for arthralgia after the final treatment. In the CLILT group, 4 patients had no diagnosis for arthralgia after the final treatment. There was one patient who recovered from arthralgia after the placebo treatment.
Fisher's exact test was performed in order to compare differences of recovery from TMJ arthralgia between groups. The number of patients who recovered from arthralgia of TMJ in the MLILT group was significantly greater than the placebo group at P value = 0.0055. Moreover, the relative risk of the comparison showed that MLILT was 4.9 times (95% confidence interval = 1.4 to 17.5) more effective than placebo in terms of the numbers of patients who had arthralgia relieved. There was no such difference obtained by comparing the CLILT group with the placebo group at P value less than 0.05.
Subjective assessments (McGill pain questionnaire and SSI)
McGill pain questionnaire
The McGill pain questionnaire was used as one of the methods of subjective assessments. Patients were invited to complete the questionnaires before treatment and after the final treatment. Pain rating index (PRI) was calculated on the basis of weight rank score as suggested by Melzack et al [19].
Owing to a non-normal distribution of the score, non-parametric statistical tests were used for description of data and analysis. The differences of PRI-T among groups before treatment and after the final treatment were analysed by using Kruskal-Wallis. Significant differences of PRI-T among groups were not found at P value less than 0.05 either before treatment or after the final treatment.
Symptom severity index (SSI) using visual analogue pain scale
SSI were recorded twice before the first treatment and then after each treatment. The maximum score was 10 representing the worst pain that can be imagined. Zero was the score for no pain.
The means and SD of SSI at different time points are detailed in table 5.
Table 5: Means and the SD of baselines and post-treatment symptom severity index (SSI) by group and time of assessments.
| Group & time | Means SSI (SD) | ||||
|---|---|---|---|---|---|
| Baseline 1 | Baseline 2 | After 1 treatment | After 2 treatments | After 3 treatments | |
| CLILT | 6.8 (2.17) | 6.5 (1.68) | 6.7 (1.65) | 6.3 (2.07) | 6.1 (2.29) |
| MLILT | 6.3 (2.06) | 6.3 (1.97) | 6.3 (2.64) | 5.7 (2.69) | 4.5 (2.58) |
| Placebo | 7.3 (1.45) | 6.5 (2.64) | 6.5 (2.71) | 5.2 (3.31) | 5.0 (3.38) |
The mean SSI of each group by time of assessments is also plotted in figure 4.
The means of SSI showed differences among groups at the first baseline. At the second baseline the means among groups were about the same level (6.3 to 6.5). A slight decline of mean SSI was found in the CLILT group by the end of treatment. The mean SSI of the MLILT group was decreased gradually after the second treatment. Although a distinct decrease in mean SSI was found in the placebo group after the second treatment, there was no change in mean SSI after the third treatment. SSI among groups was compared by ANCOVA using two baselines as a covariate. There was no statistically significant difference of the mean SSI among groups at P value less than 0.05 after the treatments.
It was shown that a difference of SSI responding to CLILT, MLILT and placebo could not be observed over the period of treatments.
The results from the follow up after the period of the trial
After the last assessment for the final treatment in trial, there was routine follow up at about 2 to 4 weeks after the final treatment. It should be emphasised that the placebo group received MLILT in the second week. Therefore, the results of 2 to 4 weeks follow up for all three groups were response to either CLILT or MLILT. Apart from routine assessments, SSI based on VAS was also recorded.
The percent pain score reduction calculated by mean VAS from the baseline and mean VAS at 2 to 4 weeks follow up were 44%, 50% and 63% in the groups treated with CLILT, MLILT and MLILT after placebo respectively. Overall, the mean of percent VAS reduction after LILT was 52%.
The follow up of all patients who were treated by either CLILT or MLILT after a period of 3 to 7 months showed that 33% of patients (10 patients from 30 patients) did not need any other treatments apart from LILT in the trial. The remainder of the patients requiring further treatments were treated by MLILT or defocused CO2 laser for recurrent myofascial pain, an occlusal splint for a history of bruxism representing parafunction of the mandibular movements or arthrocentesis for internal derangement of the intraarticular disc with limitation of the mouth opening.
Discussion
MLILT regime used in this trial showed a distinct benefit in improvement of PPT in comparison with CLILT and placebo. This result was corresponded to the in vitro study on myoblast cultures. It was founded 820 nm laser irradiation at 19J/cm2 inhibited the prostaglandin E2 synthesis stimulated by Interleukin 1 while the lower energy density (4J/cm2) failed to do so [20]. Regarding the clinical significance of these results, the standard threshold force based on RDC is 2 pounds by using index finger palpation [16]; this amount of force is equal to 89 kpa. The mean of the MLILT group was higher than 89 kpa after the second treatment while the means of the other groups failed to reach that point particularly the placebo group.
The same record and analysis were also conducted on the normal side which showed no statistically significant difference among groups (the data is not shown in this source). This confirms an objective increase in PPT in the MLILT group not related to the effect of time of measurement.
An improvement of EMG recorded during maximum clenching of the natural occlusion was found to be another positive response to the MLILT. Although it achieved a marginal significance at P value 0.051, the 95% confidence interval was not zero overlapping. Owing to the fact that there was no statistically significant difference of cEMG among the groups from the analysis on the non-painful muscle on the opposite side, the effect on the painful muscle of repeated measurement could be excluded (the data was not shown in this source). Therefore, the benefit of MLILT could be counted in terms of statistics. From the clinical consideration, there has still been no standardised range of maximum clenching EMG reported in the literature.
Overall clinical assessment based on RDC was recorded in the MLILT group; 70% and 80% of cases recovered from myofascial pain and TMJ arthralgia respectively while there was only a 10% recovery in the placebo group. This showed a statistical significance with a 3.5 relative risk in a favour of MLILT compared with placebo. The CLILT group had a higher number of recovered patients (40%) than the placebo group but failed to show a statistical difference. According to the impression of Dahlstrom [21], which was based on an extensive review of other conservative treatments for TMD, between 72 and 97% of the patients had been described as successfully treated. Therefore, the benefits of MLILT on myofascial and TMJ arthralgia patients should be considered in the range of effective conservative treatments.
This study used two pain questionnaires namely the McGill pain questionnaire and SSI based on VAS for measuring the results of pain relief after LILT. There was no significant difference in pain score either from SSI or McGill among groups after the final treatment which was about 10 days after the first baseline assessment and 2 days after the final treatment.
In a study by Conti [9] treating TMD by LILT once a week for three weeks, there was found to be a statistically significant differences of VAS between the baseline assessment (mean VAS = 5.6) and 5 minutes after the second (mean VAS = 2.4) and third treatments (mean VAS = 2.0) within the myogenous group of TMD. However, in that study there were no statistically significant differences of VAS between the control and experimental groups. It should be noted that in the study by Conti [9], the pain scores were recorded a short time after treatment while in this study the pain was assessed at least 24 hours after each treatment.
It could be argued that the period of pain assessment in the present trial should have been extended. However, this would have had to outweigh ethical reasons in the placebo group. In this study, it was decided to treat the patients who had placebo in the first week with MLILT in the second week so that every group ultimately had active treatment for humanitarian reasons. Therefore, the control placebo group was ended after that stage.
The effect on SSI was demonstrated at a period of 2-4 weeks after the final treatment with a mean 52% reduction. It can be hypothesised that the pain score which is a subjective assessment was reduced sometime later than the beneficial objective assessments namely improvement in PPT and cEMG and overall recovery from myofascial pain and arthralgia.
LILT is considered to have a definite role in the management of painful TMD. For the practical view point, LILT can be considered as one of the conservative treatments for TMD pain. In order to obtain the most satisfactory clinical outcome, this therapy may need to be combined for about two thirds of patients with other forms of management for TMD such as splint therapy for the patients who also have parafunctional habits and arthrocentesis for those with internal derangement of the meniscus with limitation of mouth opening. Regarding the dosage, the MLILT regimen has more effective for TMD pain relief than the CLILT regimen.
Conclusion
According to this randomized placebo control trial, 820 nm Gallium Aluminium Arsenide (GaAlAs) laser at energy densities of 107 J/cm2 had a significant improvement of pressure pain threshold and voluntary clenching EMG in the myofascial pain and TMJ arthralgia patients over the group of sham laser.
References
- 1: Okeson JP. (2005) Orofacial Pains: The Clinical Management of Orofacial Pain. Sixth Edition Chicago: Quintessence Publishing Co: pp 287-379 [Google Scholar]
- 2: Bradley PF. (1987) Conservative treatment for temporomandibular joint pain dysfunction. Br J Oral Maxillofac Surg 25:125-137 [DOI] [PubMed] [Google Scholar]
- 3: Medlicott MS, Harris SR. (2006) A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training and biofeedback in the management of temporomandibular disorder. Phys Ther 86:955-973 [PubMed] [Google Scholar]
- 4: Beckerman H., de Bie R.A., Bouter L.M., De Cuyper H.J., Oostendorp R.A. (1992) The efficacy of laser therapy for musculoskeletal and skin disorders: a criteria-based meta-analysis of randomized clinical trials. Phys Ther 72:483-491 [DOI] [PubMed] [Google Scholar]
- 5: Gam A.N., Thorsen H., Lonnberg F. (1993) The effect of low-level laser therapy on musculoskeletal pain: a meta-analysis. Pain 52:63-66 [DOI] [PubMed] [Google Scholar]
- 6: Bezuur N.J., Habets L.L.M.H., Hansson T.L. (1988) The effect of therapeutic laser treatment in patients with craniomandibular disorders. J Craniomandib Disord 2:83-86 [PubMed] [Google Scholar]
- 7: Gray R.J., Quayle A.A., Hall C.A., Schofield M.A. (1994) Physiotherapy in the treatment of temporomandibular joint disorders: a comparative study of four treatment methods. Br Dent J 176:257-261 [DOI] [PubMed] [Google Scholar]
- 8: Bradley P.F., Rehbini Z. (Eds.) Low intensity laser therapy (LILT) for temporomandibular joint pain: Clinical, Electromyographic and Thermographic Study. Abstracts of XI Congress of Int Soc for Laser Surgery & Medicine Buenos Aires: Oct 1995 [Google Scholar]
- 9: Conti P. (1997) Low level laser therapy in the treatment of temporomandibular disorders (TMD): a double-blind pilot study. The journal of craniomandibular pratice 15:144-149 [DOI] [PubMed] [Google Scholar]
- 10: Fikackova H, Dostalova T, Novratil L, Klaschaka J. (2007) Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed Laser Surg 25:297-303 [DOI] [PubMed] [Google Scholar]
- 11: Shirani AM, Gutknecht N, Taghizadeh M, Mir M. (2009) Low-Level Laser therapy and myofascial pain dusfunction syndrome: a randomized controlled clinical trial. Lasers Med Sci 24:715-720 [DOI] [PubMed] [Google Scholar]
- 12: Emshoff R, Bosh R, Pumpel E, Schoning H, Strobl H. (2005) Low- level laser therapy for treatment of temporamandibular joint pain: a double-blind and placebo- controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol. Endod 105:452-456 [DOI] [PubMed] [Google Scholar]
- 13: Baxter GD, Diamantopoulos C, O'Kane S, Shields TD. (1992) Therapeutic Lasers: Theory and Practice, London: Churchill Livingstone: pp 208-209 [Google Scholar]
- 14: Arao M, Fukaya M, Tange K. (1995) The clinical study of low power laser treatment for temporomandibular arthosis>. In: The 4th International Congress on Lasers in Dentistry, pp. 245-250 Bologna Italy: The 4th International Congress on Lasers in Dentistry [Google Scholar]
- 15: World Association of Laser Therapy (2004) Consensus agreement on the design and conduct of clinical studies with low level laser therapy and light therapy for musculoskeletal pain and disorders. Photomed Laser Surg 24:761-762 [DOI] [PubMed] [Google Scholar]
- 16: Dworkin SF, LeResche L. (1992) Research diagnosis criteria for temporomandibular disordrs: Review, criteria, examination and specification critique. J Craniomandibular Disorders Facial Oral Pain 4:301-355 [PubMed] [Google Scholar]
- 17: Rehbini ZA. (1995) A study of the effect of low intensity laser therapy (LILT) on painful dysfunction of the muscles of matication. University of London: pp.1-96 M.Sc. Thesis [Google Scholar]
- 18: McMillan AS, Blasberg B. (1994) Pain-pressure threshold in painful jaw muscles following trigger point injection. J Orofac Pain 8:384-390 [PubMed] [Google Scholar]
- 19: Melzack R, Katz J, Jeans ME. (1985) The role of compensation in chronic pain: analysis using a new method of scoring the McGill Pain Questionnaire. Pain 23:101-112 [DOI] [PubMed] [Google Scholar]
- 20: Sattayut S, Hughes F, Bradley P. (1999) 820 nm gallium aluminium arsenide laser modulation of prostaglandin E2 production in interleukin I stimulated myoblasts. Laser Therapy 11:88-94 [Google Scholar]
- 21: Dahlstrom L. (1992) Conservative treatment methods in craniomandibular disorder. Swed Dent J 16:217-230 [PubMed] [Google Scholar]


