Abstract
Background and aims: Patients now want a long-lasting youthful appearance but with a minimally-invasive approach. Our unique approach, “AdipoLASER reJuvenation (ALJ)”, involves a variety of minimally-invasive laser- and lipolysis-based techniques, and the present study assessed the impact of this ALJ approach.
Subjects and Methods: From 2008 — 2011, we prospectively enrolled 221 patients into the study. 71 of them, underwent the ALJ approach: 2 reductive techniques via microliposuction and laser-assisted lipolysis (LAL); and 2 regenerative techniques via autologous fat graft and fractional CO2 laser resurfacing. The remaining 150 patients underwent only 1 or 2 of these techniques. Patients were monitored through 1 to 18 months, clinical photography was taken and histological assessments were performed.
Results: ignificantly better and long-lasting results were obtained for the complete ALJ approach regarding all aspects of the face, mandible and neck compared with controls. The combination of the regenerative and the reductive approaches delivered on excellent balance, restoring a youthful, natural appearance to the face.
Conclusions: The fractional CO2 laser has both a photodestructive, or HLLT, effect and an LLLT component in the beam periphery. This LLLT effect possibly prolonged the life and improved the take of the fat grafts, with the well-documented HLLT effect inducing swift collagenesis and better remodeling of the dermal matrix. A natural look in depressed areas was thus restored with the combination of fat redistribution and the HLLT/LLLT effect. Microlipolysis and laser-assisted lipolysis (LAL) could at the same time remove those areas of redundant and prolapsed fat while countering skin laxity, and address both jowl formation and submental flaccidity. The unique combination of all four approaches in our “AdipoLASER reJuvenation” proved to be superior to any other lesser approach in both the long- and short term with very little patient downtime, but did not present much more in terms of treatment time and cost to the patient. We believe that the ALJ approach offers a real minimally-invasive alternative to the classic surgical facelift
Keywords: cervico-facial incision-less skin rejuvenation, HLLT-LLLT synergy, laser-assisted lipolysis, LLLT effect, fat redistribution
Introduction
At the present, plastic surgery has had to face some new facts: the world-wide graying of the population, the increase of public demand for looking younger and better and a global tendency for less aggressive procedures as shown in a survey issued by an American Society for Aesthetic Plastic Surgery (ASAPS) 2010 Survey. This survey concluded that world-wide, only 2.27% from the interviewed patients were operated on for facelift/rhytidectomy. However, 4.51% of the very larger remaining groups were being treated with autologous fat, and 1.2% with laser resurfacing. In other words, there was almost 4.5 times the number of patients who elected to have a fat transposition procedure compared with laser resurfacing. The possible reason for this growing global public reluctance for a full rhytidectomy could be the severity of the sequelae after traditional scalpel facelifts.
In order to produce a more youthful appearance, the current procedures are addressing all layers of the face and the neck: the skin, the fat muscle and sometimes the bones (or the structures related to them). The deeper we operate, the more risks we might encounter: a longer recovery time; transient or long term complications (vascular or neurological, or both); a greater financial burden; psychological disturbances; and at the end of the road, the potential for an unnatural result in both form and function.
Following these foregoing treatment concepts and patient-based considerations the authors decided to offer the patients an alternative, which would still be “surgical”, but much more minimally invasive (a closed approach) and gentler, keeping in mind that the restoration of youth is essentially the combination of the matter of tissue volumes or lack of them, of clear and harmonious arcs and of a better skin quality. To be able to counteract the aging effects, the surgeon has to understand the basic anatomical, physiopathological and histopathological changes related to the aging process at all levels: skin, fat, muscle and bone. At skin level, the quantity and quality of collagen in the dermis decreases and so does the number of fibroblasts which become, at the same time, less competent. In addition to poorly-organized collagen fibers, elastic fibers become elastotic, allowing both gravity and the dynamics of the muscles of mimicry to leave their mark on the dermal matrix and epidermal morphology, leading to sagging and laxity. As a consequence, the skin envelope becomes unable to accommodate for the loss or shifting of the underlying tissue volume.
Regarding the fat layer and the various compartments, a youthful face has an ample volume, evenly distributed with a smooth transition from one area to another with the 3-D topography delineated by a series of arcs and convexities. The changes affecting fat due to aging are loss of fullness due to downward movement of fat, such as the periorbital, forehead, glabellar, malar buccal cheek, and perioral areas: on the contrary, accumulation of fat can occur in or on the infraorbital pouches, paranasolabial and labiomental folds, the jaws and submental areas. Fat pockets can appear like separate entities with forward and downward redistribution, such as malar fat, build-up against the nasolabial fold, and jowls. In time, the underlying bone can suffer from resorption and expansion, and the muscles after repeated contraction, become straight and short, with an increased resting potential.
To meet the growing demand for a minimally-invasive but effective and long-lasting alternative to conventional surgical rhytidectomy, which could even address issues that the standard rhytidectomy is not able to do, such as improvement of overall skin tone and condition, we devised a combination approach involving the synergy between 2 reductive and 2 regenerative techniques which we called the “AdipoLASERreJuvenation” approach, or ALJ. The present study sought to evaluate the benefits of this approach over standard minimally-invasive mono- or duo therapy techniques.
Subjects and Methods
Subjects;
From 2008-2011, 221 patients were enrolled in the study. Seventy-one patients underwent our ALJ (69 females and 2 males, average age 52.8 y.o., range 34-72). In the same period, 150 patients (135 females and 15 males, average 50 y.o., range 35-70) were treated with only a single double or triple procedure from our combination: 15 patients had laser-assisted lipolysis (LAL) of the jawline; 23 patients had LAL for the mandibular and submental areas (11 patients with lipoaspiration and 12 patients without); 59 patients underwent LAL of the jawline and submental area with lipoaspiration and fat grafting for the malar and periorbital zones, in addition to whole-face fractional CO2 laser resurfacing; and the remaining 53 patients had a single treatment of whole face fractional CO2 laser resurfacing on its own.
Our unique ALJ approach for cervico-facial rejuvenation is a dual-phase reductive/regenerative approach which is performed in a single session, consisting of standard microliposuction and LAL as the reductive techniques coupled with autologous fat graft and fractional CO2 laser rejuvenation as the regenerative techniques. AdipoLASER reJuvenation is performed generally under orotracheal intubation (OTI) anesthesia (90) together with IV sedation and local anesthesia (10I).
Our ALJ approach was aimed to satisfying the following important criteria regarding fat and skin management, which comprised the restoration of the following:
Fullness of the middle and superior upper third of the face with fat transplants, harvested usually from the abdomen or the anterior part of the neck (when possible).
Definition of the jawline and anterior neck — meaning fat removal (standard microliposuction) and adipocitolysis with laser-assisted lipolysis (LAL) using a 980 nm wavelength from a diode laser delivered via an optical fiber.
Brightness of skin tone and skin tightening using fractional CO2 laser facial resurfacing and LAL with the diode laser, maintaining the optical fiber in the upper part of the subcutaneous fatty layer.
Another goal was to achieve optimized fat survival through gentle harvesting and grafting techniques and the phototherapeutic action (LLLT) in the peripheral tissues concomitant with the creation of the fractional CO2 macroablative columns (MACs).
LAL with the 980 diode lasers (MedArt Diode Laser 980 nm, ASAH MEDICO A/S, Valseholmen 11-13, Denmark) was performed using a 600 µm optical fiber inserted interstitially into the target fatty tissue through a 16 G needle as the cannula to ensure correct place- ment of the fiber and minimize abrasive damage to the tissue at the entry point.
The LAL technique consisted of the following steps:
Marking the entry points and the areas for treatment on the skin.
Ensuring a sterile field for the face and neck.
local anaesthesia — topical anaesthetic cream +lidocaine enriched, cold Klein solution and general iv (the latter was used with intubation anaesthesia if more procedures were combined with the LAL, such as our full ALJ approach)).
Ensure eye protection for the patient and the surgical team.
Create the entry point using a 16 G needle.
Use the labiomental folds for LAL at the jawline.
Mark up the antero-lateral cervical zones of the neck bilaterally.
Place the needle in the subcutaneous layer and insert the fiber through the needle. The red aiming beam will be visible through the skin.
Move the needle and fiber forwards and backwards in the tissue in a fan-like pattern, with the entry point as the base of the fan, and about 0.5 cm between each end point in the fan periphery.
When the fiber reaches the periphery of the marked zone, the needle and fibre should be withdrawn for each stroke in the fan.
The laser energy is emitted in a square wave (switched continuous wave) with an output power of 11 W, pulse width of 900 msec. A total of 60 J/cm2 per treated zone should be delivered. The fiber should be moved at the constant rate of 0.3 — 0.5 cm/sec.
Be sure to keep the needle and fiber moving constantly, never remaining in the one spot for any length of time.
The procedure for the fat harvesting and facial grafting technique is as follows:
Marking the treatment site; Mark up both the donor and treatment sites.
Harvesting: Harvest fat from the flanks or the abdomen with a 10, 20 or 60 cc syringe attached to a 14 or 16 G needle or 12-hole Khouri 12 G cannula.
When using a 14 G needle, 60-80 cc of fat should be extracted.
Allow the fat to stand for a moment followed by gentle centrifugation.
Discard the upper and lower fractions (oil and water, respectively).
Perform fat face transplantation to the marked areas of the face with a 1 cc syringe and a Fischer cannula ϕ1.2 — 1.4, placing small droplets of fat in the tissue following Coleman's Lipostructure technique. 1)
The average amounts of fat transplanted into each area in our ALJ approach were as follows: malar zone, 5-8 cc each; orbitomalar junction, 1 cc each; nasolabial folds, 3-4 cc each; melomental folds, 3-4 cc each; and lips ( 2-3 cc each ).
For face resurfacing we used a fractional carbon dioxide (CO2) (λ=10,600) ( MedArt 610 FRx, ASAH MEDICIO A/S, Valseholmen 11-13, Denmark) at the following parameters: periocular power 6-8 W, mean 7 W; time 5 ms, high density, and for the rest of the face power 8-10 W, time 4 ms, medium density. The laser parameters were matched on an individual basis with the severity of the skin and the necessary surface.
AdipoLASERreJuvenation is performed generally under orotracheal intubation (OTI) anesthesia (90%) and IV sedation and local anesthesia (10%).
The patients undergoing our ALJ approach all follow a pre- and post- operating protocol. The pre-operating process consists of blood tests (biochemistry and coagulation), anti-bruising and antiviral medication. The postoperative process consists of antibiotic and non-steroidal anti-inflammatory drug (NSAID) therapy and compressive dressings for the neck and mandibular line (24-48 hours).
The patients returned for follow-up assessments at 1 day, 1 week, 3, 6, and 9 months and 1 year after treatment and the effects were monitored using clinical photography obtained at every check-up (Canon camera in natural and artificial light, under standardized conditions).
In our practice and in addition to our standard ALJ approach, although not covered in the present study but as a point of interest, we have lately introduced an additional treatment on a regular basis with platelet rich plasma to correct wrinkles and accelerate healing.
Results
The patients were monitored for 1 to 18 months, and the following aspects were assessed on a 4-point scale as excellent, good, fair, or poor. (Table. 1): the contour correction, the improvement of the face volume, the skin condition, edema, ecchymosis, the exfoliating time, and the recovery time. Regarding the patients' overall satisfaction rate: 63.2% were rated excellent, 30.8% good, 4.2% fair, and 1.8% poor, compared with the control group: poor, 6.8%; fair, 53.3%; good, 27.1%; and excellent, 12.9%. When these findings were compared with the satisfaction rate from the control group (Figure 1), the significant difference between them is clearly visible, with a p value of less than 0.001 (Student's t test). The Satisfaction Indices for the ALJ and control groups were 94.0% and 40.0%, respectively, (p <0.001), calculated by the sum of the excellent and good scores.
Table 1: Postoperation assessment of patient satisfaction in the ALJ group at 2 months post-treatment.
| poor | Fair | good | Excellent | |
|---|---|---|---|---|
| Contour correction | 1 | 3 | 22 | 45 |
| Improvement of face volume | 2 | 2 | 22 | 45 |
| Skin condition | 1 | 3 | 22 | 45 |
| Oedema | 1 | 4 | 26 | 40 |
| Ecchymosis | 1 | 5 | 20 | 45 |
| Exfoliating time | 1 | 3 | 24 | 43 |
| Recovery time | 2 | 2 | 21 | 46 |
Figure 1:
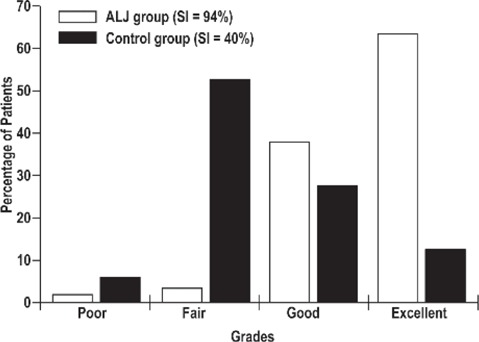
Average satisfaction rates compared for the ALJ (n=71) and control groups (n=150) over the 4 grades from poor to excellent. The satisfaction index (sum of the excellent + good scores) was 94% for the ALJ group and 40% for the control group (Student's t test, P < 0.001)
Compared with the baseline findings, a significant improvement was noted regarding the fat distribution, the skin condition and the contour correction in all the patients treated with this technique, which was noticeable at 10 days post-treatment, through a combination of the fat grafting and laser-specific reactions as a result of both HLLT and LLLT effects. LAL with the diode laser addressed redundant fat deposits and skin laxity in the lower face and neck and the primary effect of the fractional CO2 laser treatment rejuvenated the skin of the entire face and assisted with general overall dermal tightening. On the other hand, the secondary LLLT effect of the fractional ablative CO2 LASER treatment could have led to a better survival rate of the fat graft in the upper face and improved the skin texture. Swelling was observed in 90% of patients which had mostly disappeared by 10 days, and local ecchymosis was experienced in 40% of patients which resolved spontaneously after 1 week. We also observed an improvement in the exfoliating and healing period if we concomitantly used PRP after fractional CO2 treatment (from 7 — 9 days to 5 - 6 days), so the fractional ablative approach may have been acting as a drug delivery system, and this interesting technique merits further research.
Case reports
Representative case 1: A 52-year-old woman presented to our clinic for facial rejuvenation, and she was treated with our ALJ approach. For the mandibular and cervical LAL (180 cm2), the settings were 10 W power, 1000 ms exposure and total energy delivered, 6300 J. She had fat grafting to the malar, nasolabial folds and melomental folds. She underwent microliposuction around the chin, and received full-face fractional ablative CO2 resurfacing. The baseline findings are seen in Figure 2a,c and the excellent results in Figure 2b,d, 2 months after the ALJ procedure. The patient was very satisfied with the final result.
Figure 2:

(Case 1) This 52 y.o. female presented or facial rejuvenation is seen at baseline (a & c) and at 2 months after our ALJ procedure. An excellent result and a highly satisfied patient. The result (b & d) will be even better as the remodeling process takes place over the following months.
Representative case 2: A 50-year-old woman came to our clinic for facial rejuvenation. This is a very good example of the significant difference between undergoing only one or two parts of our full ALJ approach, and having the complete treatment. When she first presented (Figure 3a,e), she was treated with LAL for the mandibular line and full face fractional CO2 resurfacing. The result was fair, as seen in Figure 3b,f, one month after the procedures.
Figure 3:

(Case 2) This 50 y.o. female presented for facial rejuvenation (a & e), and was treated with LAL for the mandibular line and a full-face fractional CO2 resurfacing. (b & f): The findings 1 month post-treatment can be seen with fair improvement. (c & g): She returned 8 months later (9 months after the first treatments). The result has held reasonably well, but she wanted to complete the full ALJ programme. She underwent fat grafting to the malar region, nasolabial and melomental folds, and another full-face fractional CO2 laser treatment. (d & h): The very good results at 2 months post-treatments are seen with a satisfied patient. She can expect the result to improve even more over the next few months due to tissue remodeling.
She returned to the clinic a second time 8 months later ([Figure 3c,g] 9 months postop) where the result was seen to be holding up well, and requested the rest of the ALJ process. She underwent fat grafting in the malar area, nasolabial folds and melomental folds, and a second full face fractional CO2 rejuvenation treatment. Figure 3d,e shows the findings 2 months after the second set of procedures, with good results. The patient was satisfied with the final result.
Discussion
Each component of our ALJ approach has its own advantages when used alone, but when used in combination we believe the synergistic effect gives results which are superior to the sum of the individual components. Fat grafting is a well-established method of recovering the correct contour in areas of the face which have lost volume due to fat slippage through the aging process. However, persuading the graft to survive and maintain the good effect can be problematic, as the grafted fat is almost inevitably reabsorbed by the body. Likewise, laser-assisted lipolysis (LAL) offers proven advantages. Small blood vessels in the area of interest are coagulated, helping to reduce bleeding during the operation. 2) The effect is well distributed and the skin surface is less uneven after the operation. LAL stimulates the formation of collagen in the dermal layer overlying the fatty layer being treated through secondary photothermal effect, enhancing the elasticity of the skin and facilitating the skin contraction in the operative region but with mild trauma. 3)
Conventional surgical lasers produce photothermal and other effects in tissue which are destructive in nature: there is a permanent change in the irradiated tissue following laser irradiation. This is true of incision, vaporisation and coagulation. The reaction in tissue following such laser irradiation is therefore above the survival threshold of normal tissue, causing death or disruption, classed as high level laser treatment (HLLT). Even with surgical lasers, concomitant effects leave tissue alive and well but also stimulate the tissue, and these are classified as low level laser therapy (LLLT). 4)
HLLT occurs at temperatures from above 40°C and 200°C and, depending on the temperature, can achieve carbonisation, vaporisation, coagulation, denaturation and degradation of proteins. In our ALJ, the major photosurgical effects are coagulation and protein degradation, which are sufficient to induce the wound healing process. LLLT on the other hand works at temperatures under 40°C, or with no temperature rise at all, and induces photobioactivation without any damage. The resulting photochemical, photodynamic, photoenzymatic, and photoimmune effects act directly on cells at a subcellular organelle level to achieve a variety of results including cell repair, enhancement of cellular function and cellular proliferation.
It is well accepted that the energy of photons when absorbed directly in cells or tissue during the LLLT process may affect cellular metabolism and signaling pathways. The major molecular target is cytochrome c oxidase or the cell membrane, depending on the wavelength of the light. In our AJL approach, the energy from the 980 nm near IR beam which is not quenched in the lipoaspiration process will work primarily on the cell membranes, inducing a direct photophysical effect, followed by an indirect photochemical cascade resulting in increased adenosine triphosphate (ATP) production, modulation of reactive oxygen species, and initiation of cellular signaling through calcium ion (Ca++) and proton (H+) generation. Reported results include increased cell proliferation and migration (particularly by fibroblasts), increased tissue oxygenation, modulation in the levels of cytokines, growth factors and inflammatory mediators. 5)
HLLT with the diode laser LAL induces adipocitolysis in the fatty later with simultaneous photothermal effects in the lower epidermal layers to induce neocollagenesis followed by remodeling : the latter is also the case in CO2 laser resurfacing. The macroablative columns (MACs) associated with ablative CO2 fractional resurfacing also induce wound healing, with elastinogenesis and neocollagenesis in the upper and mid dermal layers, resulting in a much better-organised dermal matrix and younger-looking epidermis. Both of these photosurgical approaches have an associated zone of low photon intensity surrounding the damaged tissues, thereby assisting with acceleration of the wound healing process and also photobioactivation of the transplanted fat cells to ensure better graft take with less initial resorption. It would appear that the more complex treatment approach which addresses simultaneously all cervical - facial levels and layers through multi-laser treatment and fat redistribution (aspiration and grafting) gives a better rejuvenation result: the more complex the approach, perhaps, the better the result.
Based on the evidence on 50 cases in which laser treatment enhanced the post fat graft appearance, we started a study in cooperation with our patients preparing for abdominoplasty (ProEstetica Medical Center Research Ethics Committee — Institutional Review Board — Resolution 7/2011). Histological examination of fat with and without laser stimulation (power 12W, time 4ms, medium density) showed a significant difference in the collagen structure, the number of adipocytes and the presence of young adipocytes (Figure 4). Laser-stimulated fat grafts also showed better collagen fibre arrangement in the host tissue, and more adipocytes in the donor tissue, indicating enhanced survival and take of the graft (Figure 5).
Figure 4:
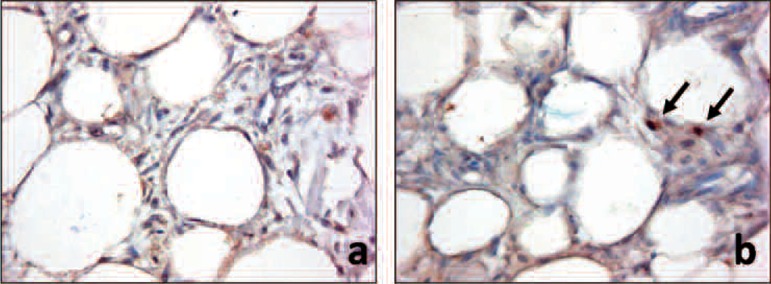
Adipocytes seen without laser stimulation (a) and with laser stimulation (b). = Immunohistochemical staining forDlk1 (400x) using MAb (mouse antibody) to Dlk1 (human) at dilution 1:500, shows cytoplasmic staining of preadipocytes (black arrow) in the laser-stimulated specimen.
Figure 5:
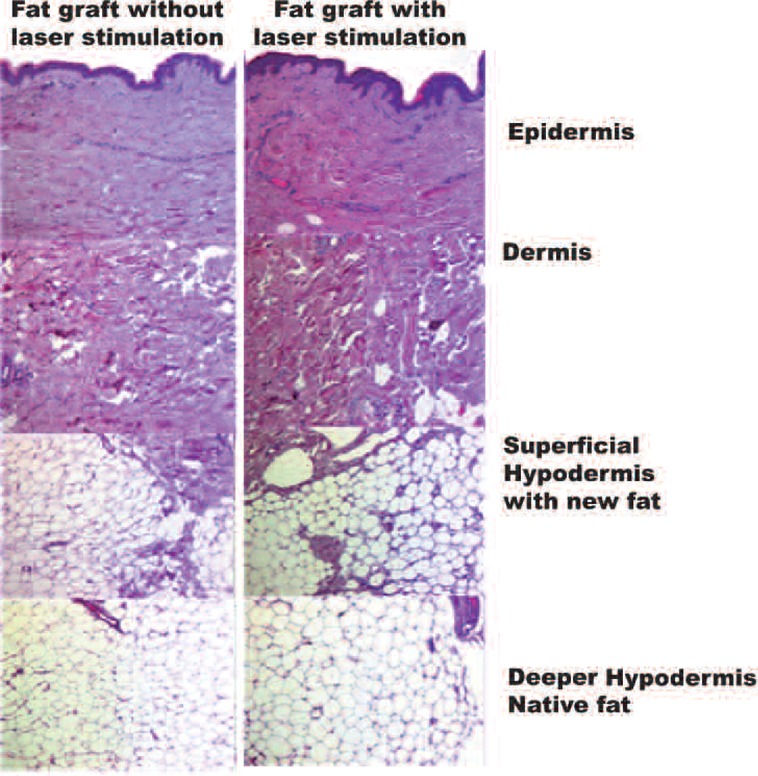
Montages of fat grafts in tissue without (left column) and (right column) with laser stimulation. Laser stimulation shows improvement in collagen fibers in the dermis and in the number of adipocytes in the superficial and even deep- er hypodermis (H&E, 100x).
Conclusions
The global tendency in cervico—facial rejuvenation is showing a greater demand for fat graft and laser procedures and less demand for the classical surgical facelift. Our “AdipoLASERreJuvenation” approach is a personal complex method, a simultaneous combination of 4 surgical techniques with standard microliposuction and laser-assisted lipolysis as the reductive techniques and fat grafting and full-face fractional CO2 laser resurfacing as the regenerative techniques, but all embodied in a single session. We believe that combination is the key to prove individual solutions to each patient. The fractional ablative CO2 treatment improves the skin texture and tightness and also offers a photobioactivation reaction, as does the LAL in the periphery of the actual lipolysis: this achieves LLLT simultaneously with an HLLT reaction. 6) This LLLT component is a possible optimizing factor for the fat graft survival, offering new opportunities for research and clinical applications. This “closed” minimally-invasive surgical approach could benefit patients seeking to improve their appearance and quality of life: a natural yet visible rejuvenation with a shortened “down time” (one week on average) and a low rate of complications. Further studies with much larger population are warranted to confirm the result of this preliminary study.
References
- 1: Coleman SR. (1997): Facial recontouring with lipostructure. ClinPlast Surg, 24: 347-367 [PubMed] [Google Scholar]
- 2: Goldman A. (2006) Submental Nd: Yag laser-assisted liposuction. Lasers Surg Med 38:181-184 [DOI] [PubMed] [Google Scholar]
- 3: Badin AZ, Moraes LM, Gondek L, Chiaratti MG, Canta L. (2002) Laser Lypolysis: flaccidity under control. AesthPlast Surg 26: 335-339 [DOI] [PubMed] [Google Scholar]
- 4: Ohshiro T. (1991): Low reactive — level LASER Therapy. Practical Application. [DOI] [PubMed] [Google Scholar]
- 5: Christian Raulin. SyrusKarsai. Laser and IPL technology in Dermatology and Aesthetic Medicine [Google Scholar]
- 6: Ohshiro T. (2011): New classification for single-system light treatment. Laser Therapy, 20: 11-15] [DOI] [PMC free article] [PubMed] [Google Scholar]


