Abstract
AIM: To perform a meta-analysis of large-balloon dilation (LBD) plus endoscopic sphincterotomy (EST) vs EST alone for removal of bile duct stones.
METHODS: Databases including PubMed, EMBASE, the Cochrane Library, the Science Citation Index, and important meeting abstracts were searched and evaluated by two reviewers independently. The main outcome measures included: complete stone removal, stone removal in the first session, use of mechanical lithotripsy, procedure time, and procedure-related complications. A fixed-effects model weighted by the Mantel-Haenszel method was used for pooling the odds ratio (OR) when heterogeneity was not significant among the studies. When a Q test or I2 statistic indicated substantial heterogeneity, a random-effects model weighted by the DerSimonian-Laird method was used.
RESULTS: Six randomized controlled trials involving 835 patients were analyzed. There was no significant heterogeneity for most results; we analyzed these using a fixed-effects model. Meta-analysis showed EST plus LBD caused fewer overall complications than EST alone (OR = 0.53, 95%CI: 0.33-0.85, P = 0.008); subcategory analysis indicated a significantly lower risk of perforation in the EST plus LBD group (Peto OR = 0.14, 95%CI: 0.20-0.98, P = 0.05). Use of mechanical lithotripsy in the EST plus LBD group decreased significantly (OR = 0.26, 95%CI: 0.08-0.82, P = 0.02), especially in patients with a stone size larger than 15 mm (OR = 0.15, 95%CI: 0.03-0.68, P = 0.01). There were no significant differences between the two groups regarding complete stone removal, stone removal in the first session, post-endoscopic retrograde cholangiopancreatography pancreatitis, bleeding, infection of biliary tract, and procedure time.
CONCLUSION: EST plus LBD is an effective approach for the removal of large bile duct stones, causing fewer complications than EST alone.
Keywords: Balloon dilation, Cholangiopancreatography, Endoscopic retrograde, Choledocholithiasis, Endoscopic sphincterotomy, Meta-analysis
Core tip: This meta-analysis demonstrates that endoscopic sphincterotomy (EST) plus large-balloon dilation (LBD) is an effective approach for the removal of large bile duct stones. Specifically, when compared with the outcomes of EST alone, the combined technique is associated with fewer complications. Furthermore, use of mechanical lithotripsy in the EST plus LBD group decreased significantly, especially in patients with a stone size larger than 15 mm. However, more well-designed trials are required to clarify whether this combined technique is preferable.
INTRODUCTION
During endoscopic retrograde cholangiopancreatography (ERCP), endoscopic sphincterotomy (EST) or endoscopic papillary balloon dilation (EPBD) is the standard method of enlarging the papillary orifice before stone retrieval. However, the extent of orifice dilation with conventional EST or EPBD is limited[1-3], and the use of other methods such as mechanical lithotripsy, intraductal shock-wave lithotripsy, extracorporeal shock-wave lithotripsy or, if those fail, biliary stent placement with repeated ERCP or even surgery may be required in patients with difficult (usually large) stones[1]. These methods are not widely available, and a larger opening of the orifice by large-balloon dilation (LBD) seems to be necessary. Ersoz et al[4] first reported the use of LBD after sphincterotomy for large common bile duct stones and achieved a high stone clearance rate of up to 89%-95% without mechanical lithotripsy. Since then, a number of case series have also suggested that the combination technique facilitated large stone extraction and reduced dependence on mechanical lithotripsy, contributing to higher stone clearance in a single endoscopic session with an acceptable risk of complications[5-9]. However, the comparison of EST plus LBD and EST alone for removal of choledocholithiasis has given inconsistent results.
To the best of our knowledge, the only systematic review on the topic has been published by Liu et al[10]. This included non-randomized controlled trials (non-RCTs); two eligible abstracts[11,12] which were regarded as non-randomized in the review were in fact randomized; this was validated by contacting the authors. More recently, a well-arranged trial has been published and some conflicting results have emerged[13]. Therefore, we believe that an updated meta-analysis is required.
MATERIALS AND METHODS
Search strategy
A literature search was performed to identify all relevant studies that compared EST plus LBD and EST alone for removal of bile duct stones. The PubMed, EMBASE, Cochrane Library databases, and the Science Citation Index were searched systematically for all articles published up to May 2013, without language restriction, using the following terms in their titles, abstracts, or keyword lists: “balloon dilation,” “sphincteroplasty,” “sphincterotomy,” “bile duct stone,” and “choledocholithiasis.” The references in retrieved articles were also screened manually. The abstracts of the United European Gastroenterology Week and Digestive Disease Week, from 2004 to 2012, were also searched systematically. An attempt to contact the first author was made when information was not extractable from potentially eligible published abstracts.
Study selection
Papers selected from this initial search were then screened for eligibility using the following criteria: (1) RCTs that evaluated a comparison of EST plus LBD (larger than 12 mm in balloon size) and EST alone in the removal of large common bile duct stones (larger than 10 mm in diameter); and (2) Outcomes of interest included complete stone removal, use of mechanical lithotripsy and complications. If reports came from the same study center, we only included data from the publication with the largest population. Comments, reviews, case reports, and guideline articles were excluded.
Data extraction
Data from eligible studies were extracted independently by two reviewers (Yang XM and Hu B) using standard forms, and consensus was reached on all items. Data were extracted on: first author, year of publication, country of origin, study setting, number, age and sex of patients, stone size, balloon diameter, complete stone removal, stone removal in the first session, use of mechanical lithotripsy, procedure time, and procedure-related complications.
Assessment of study quality
Two independent reviewers (Yang XM and Hu B) assessed the quality score of primary trials according to the Jadad scale[14]. Total scores ranged from 0 to 5. The Cochrane Collaboration’s tool for assessing risk of bias was also used to address potential bias (Table 1). We defined studies with a Jadad score of 3 or more points and a low risk of bias as high quality in this meta-analysis. Disagreements were discussed by the reviewers and resolved through consensus.
Table 1.
Characteristics of the included randomized controlled trials (according to the Cochrane Collaboration’s tool for assessing risk of bias)
| Ref. | Sequence generation | Allocation concealment | Blinding of participants | Incomplete outcome | Selective outcome | Other sources of bias |
| Heo et al[22] 2007 | Computer random number generator | Sealed envelope | Outcome assessment blinded | No missingoutcome data | All prespecifiedoutcomes reported | No |
| Hong et al[11] 2009 | Unclear | Not reported | Unclear | No missingoutcome data | All prespecifiedoutcomes reported | No |
| Kim et al[23] 2009 | The order of the procedure | Not reported | Unclear | No missingoutcome data | All prespecifiedoutcomes reported | No |
| Kim et al[12] 2009 | Unclear | Not reported | Unclear | No missingoutcome data | All prespecifiedoutcomes reported | No |
| Stefanidis et al[24] 2011 | Random number table | Sealed envelope | Outcome assessment blinded | No missingoutcome data | All prespecifiedoutcomes reported | No |
| Teoh et al[13] 2013 | Computer random number generator | Sealed envelope | Outcome assessment blinded | No missingoutcome data | All prespecifiedoutcomes reported | No |
Statistical analysis
For summary statistics in meta-analysis, the odds ratio (OR) is recommended for dichotomous data, and the weighted mean difference is recommended for continuous data. Complete stone removal, stone removal in the first session, use of mechanical lithotripsy and overall complications were summarized as OR with 95%CI. Peto OR with 95%CI was used for separate complications, including post-ERCP pancreatitis, bleeding, infection of biliary tract (including cholangitis and cholecystitis), and perforation, since it could generate the least biased pooled results of studies with zero event in both groups[15]. P values of less than 0.05 were considered significant.
Heterogeneity was assessed by visual inspection of a Forest plot, the Cochran Q test, and the I2 statistic. Heterogeneity was considered significant by the Cochran Q test when P < 0.1 or I2 > 50%[16,17]. A fixed-effects model weighted by the Mantel-Haenszel method was used for pooling the OR when heterogeneity was not significant among the studies[18]. When a Q test or I2 statistic indicated substantial heterogeneity, a random-effects model weighted by the DerSimonian-Laird method was used[19]. We performed a sensitivity analysis by removing each study in turn from the overall data to evaluate the influence of a single study on the pooled analysis and by restricting the meta-analysis to high-quality studies. We also assessed the potential for publication bias through visual inspection of funnel plot asymmetry and evaluated the statistical significance of differences according to the methods of Begg et al[20] and Egger et al[21]. Statistical analyses were performed using Review Manager software (version 5.1 for Windows, Cochrane Collaboration, Oxford, United Kingdom).
RESULTS
Identification of eligible studies
The literature search yielded 316 abstracts for review, and 308 were excluded for the reasons shown in Figure 1. The results of two studies were conflated because they were from the same trial. Thus, six studies[11-13,22-24] were included, four of which were available as full texts and were high quality studies. The combined studies enrolled 835 patients who had been randomly allocated to the EST plus LBD group or the EST alone group. The characteristics of the included trials are listed in Tables 1 and 2, and the outcome data are shown in Table 3.
Figure 1.
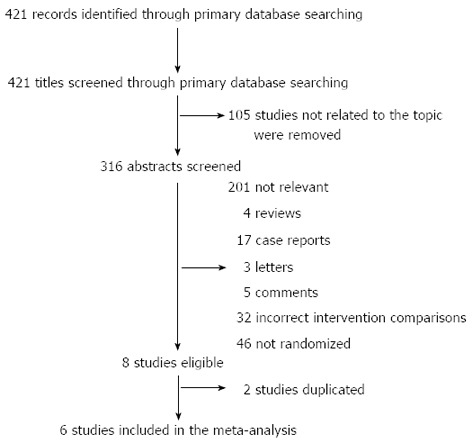
Flow chart of included and excluded trials.
Table 2.
Characteristics of the included randomized controlled trials
| Ref. | Format | Country | Center involved |
EST plus LBD, EST |
Balloon diameter (mm) | Jadad score | |||
| Number (n) | Male, female | Mean age (yr) | Stone size (mm) | ||||||
| Heo et al[22] 2007 | Full text | Korea | 1 | 100 | 48, 52 | 64 | 16.0 ± 0.71 | 12-20 | 4 |
| 100 | 50, 50 | 63 | 15.0 ± 0.71 | ||||||
| Hong et al[11] 2009 | Abstract | Korea | 1 | 70 | Not reported | Not reported | > 15 | 15 or 20 | 1 |
| 65 | > 15 | ||||||||
| Kim et al[23] 2009 | Full text | Korea | 1 | 27 | 12, 15 | 70 | 15-38.3 | 15, 16.5 or 18 | 3 |
| 28 | 14, 14 | 70 | 15-48 | ||||||
| Kim et al[12] 2009 | Abstract | Korea | 1 | 104 | 53, 51 | 70 | > 10 | 12-20 | 1 |
| 100 | 49, 51 | 69 | > 10 | ||||||
| Stefanidis et al[24] 2011 | Full text | Greece | 1 | 45 | 24, 21 | 69 | 12-20 | 15, 18 or 20 | 4 |
| 45 | 22, 23 | 68 | 12-20 | ||||||
| Teoh et al[13] 2013 | Full text | Hong Kong | 2 | 73 | 32, 41 | 72 | ≥ 13 | 13-15 | 4 |
| 78 | 40, 38 | 73 | ≥ 13 | ||||||
Values are mean ± SD. EST: Endoscopic sphincterotomy; LBD: Large-balloon dilation.
Table 3.
Outcome data derived from the included randomized controlled trials n (%)
| Ref. | Intervention | Complete stone removal | Stone removal inthe first session | Mechanical lithotripsy | Overall complications | Pancreatitis | Bleeding | Infection of biliary tract | Perforation |
| Heo et al[22] 2007 | Small EST plus LBD | 97/100 (97) | 83/100 (83) | 8/100 (8) | 5/100 (5) | 4/100 (4) | 0/100 (0) | 1/100 (1) | 0/100 (0) |
| Full EST | 98/100 (98) | 87/100 (87) | 9/100 (9) | 7/100 (7) | 4/100 (4) | 2/100 (2) | 1/100 (1) | 0/100 (0) | |
| Hong et al[11] 2009 | Small EST plus LBD | 70/70 (100) | Not reported | 13/70 (19) | 8/70 (11) | 4/70 (6) | 4/70 (6) | 0/70 (0) | 0/70 (0) |
| Conventional EST | 65/65 (100) | 47/65 (72) | 19/65 (29) | 9/65 (14) | 10/65 (15) | 0/65 (0) | 0/65 (0) | ||
| Kim et al[23] 2009 | Small EST plus LBD | 27/27 (100) | 23/27 (85) | 9/27 (33) | 0/27 (0) | 0/27 (0) | 0/27 (0) | 0/27 (0) | 0/27 (0) |
| Conventional EST | 28/28 (100) | 23/28 (82) | 9/28 (32) | 0/28 (0) | 0/28 (0) | 0/28 (0) | 0/28 (0) | 0/28 (0) | |
| Kim et al[12] 2009 | Small EST plus LBD | 100/104 (96) | 89/104 (86) | 8/104 (8) | 11/104 (11) | 10/104 (10) | 1/104 (1) | 0/104 (0) | 0/104 (0) |
| Conventional EST | 92/100 (92) | 82/100 (82) | 17/100 (17) | 10/100 (10) | 9/100 (9) | 0/100 (0) | 0/100 (0) | 1/100 (1) | |
| Stefanidis et al[24] 2011 | Full EST plus LBD | 44/45 (98) | Not reported | 0/45 (0) | 2/45 (4) | 1/45 (2) | 1/45 (2) | 0/45 (0) | 0/45 (0) |
| Full EST plus ML | 41/45 (91) | 45/45 (100) | 9/45 (20) | 1/45 (2) | 1/45 (2) | 6/45 (13) | 1/45 (2) | ||
| Teoh et al[13] 2013 | Small EST plus LBD | 71/73 (97) | 65/73 (89) | 21/73 (29) | 5/73 (7) | 2/73 (3) | 1/73 (1) | 2/73 (3) | 0/73 (0) |
| Full EST | 78/78 (100) | 69/78 (88) | 36/78 (46) | 8/78 (10) | 3/78 (4) | 0/78 (0) | 3/78 (4) | 2/78 (3) |
EST: Endoscopic sphincterotomy; LBD: Large-balloon dilation.
Efficacy
Six studies reported complete stone removal. Heterogeneity among these studies was not significant (P = 0.28, I2 = 22%, Figure 2A). Thus, we used the fixed-effects model and found that there was no significant difference in complete stone removal between EST plus LBD and EST alone (OR = 1.41, 95%CI: 0.63-3.17, P = 0.40, Figure 2A). Sensitivity analysis by removing each study in turn from the overall data or by restricting the meta-analysis to high-quality studies showed that the result was robust. Four RCTs[12,13,22,23] reported stone removal in the first session, and there was no significant difference in stone clearance between the two methods (OR = 1.02, 95%CI: 0.65-1.61, P = 0.92). A comparison of EST plus LBD and EST alone in patients with stones larger than 15 mm was carried out, and five studies[11,13,22-24] with 377 patients were included. Meta-analysis showed that there was no significant difference in the complete stone removal rate according to the fixed-effects model (OR = 0.99, 95%CI: 0.35-2.81, P = 0.98, Figure 2B).
Figure 2.
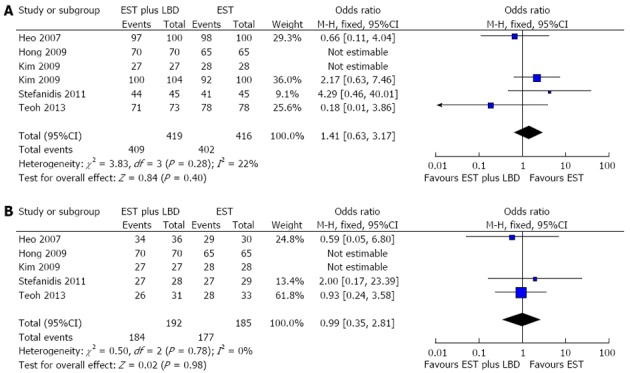
Forest plot demonstrating no significant difference in complete stone removal between endoscopic sphincterotomy plus large-balloon dilation and endoscopic sphincterotomy alone and in patients with stone size larger than 15 mm. A: Endoscopic sphincterotomy (EST) plus large-balloon dilation (LBD) and EST alone; B: EST plus LBD and EST alone and in patients with stone size larger than 15 mm.
Use of mechanical lithotripsy
Six studies reported the use of mechanical lithotripsy during the stone removal process. The trials were heterogeneous (P < 0.001, I2 = 87%), and a random-effects model analysis was performed. The results indicated a significantly reduced dependence on mechanical lithotripsy in the EST plus LBD group (OR = 0.26, 95%CI: 0.08-0.82, P = 0.02). We conducted a sensitivity analysis by excluding the study by Stefanidis et al[24], as no mechanical lithotripsy was used in the LBD group in this trial, and the result did not change (OR = 0.42, 95%CI: 0.18-0.98, P = 0.05). However, after removing the two eligible abstracts[11,12], there was no significant difference in the use of mechanical lithotripsy between EST plus LBD and EST alone (OR = 0.26, 95%CI: 0.05-1.48, P = 0.13). A subgroup analysis in patients with a stone size larger than 15 mm demonstrated that the use of mechanical lithotripsy in the EST plus LBD group decreased significantly (OR = 0.15, 95%CI: 0.03-0.68, P = 0.01, Figure 3A).
Figure 3.
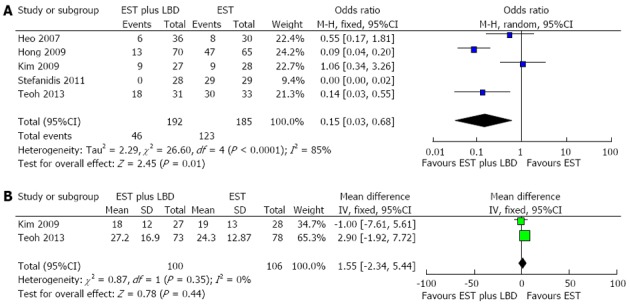
Forest plot demonstrating. A: The use of mechanical lithotripsy in the endoscopic sphincterotomy (EST) plus large-balloon dilation (LBD) group decreased significantly in patients with stone size larger than 15 mm; B: No significant difference in procedure time between EST plus LBD and EST alone.
Safety
Six RCTs evaluated the safety in both groups (Table 4). The statistical results showed that EST plus LBD caused fewer overall complications than EST alone (OR = 0.53, 95%CI: 0.33-0.85, P = 0.008), and the result did not change by restricting the meta-analysis to the four high-quality studies (OR = 0.48, 95%CI: 0.24-0.99, P = 0.05). Subcategory analysis indicated that patients undergoing EST plus LBD had a lower risk of perforation (OR = 0.14, 95%CI: 0.20-0.98, P = 0.05). No significant difference was found in terms of post-ERCP pancreatitis (OR = 0.77, 95%CI: 0.43-1.39, P = 0.39), bleeding (OR = 0.50, 95%CI: 0.20-1.23, P = 0.13), and infection of the biliary tract (OR = 0.34, 95%CI: 0.11-1.02, P = 0.05).
Table 4.
Analyses of procedure-related complications n (%)
| Complications |
All 6 studies |
Four full-text studies (high-quality) |
||||||||
| Incidence EST plus LBD, EST | OR/Peto OR (95%CI) | P value |
Heterogeneity |
Incidence EST plus LBD, EST | OR/Peto OR (95%CI) | P value |
Heterogeneity |
|||
| I2 | P value | I2 | P value | |||||||
| Overall | 31/419 (7.4) | 0.53 (0.33-0.85) | 0.008 | 28% | 0.24 | 12/245 (4.9) | 0.48 (0.24-0.99) | 0.05 | 0% | 0.37 |
| 53/416 (12.7) | 24/251 (9.6) | |||||||||
| Pancreatitis | 21/419 (5.0) | 0.77 (0.43-1.39) | 0.39 | 0% | 0.74 | 7/245 (2.9) | 0.89 (0.32-2.49) | 0.83 | 0% | 0.95 |
| 26/416 (6.3) | 8/251 (3.2) | |||||||||
| Bleeding | 7/419 (1.7) | 0.50 (0.20-1.23) | 0.13 | 22% | 0.27 | 2/245 (0.8) | 0.68 (0.12-3.93) | 0.66 | 31% | 0.24 |
| 13/416 (3.1) | 3/251 (1.2) | |||||||||
| Infection of biliary tract | 3/419 (0.7) | 0.34 (0.11-1.02) | 0.05 | 28% | 0.25 | 3/245 (1.2) | 0.34 (0.11-1.02) | 0.05 | 28% | 0.25 |
| 10/416 (2.4) | 10/251 (4.0) | |||||||||
| Perforation | 0/419 (0.0) | 0.14 (0.02-0.98) | 0.05 | 0% | 1.00 | 0/245 (0.0) | 0.14 (0.01-1.35) | 0.09 | 0% | 0.98 |
| 4/416 (1.0) | 3/251 (1.2) | |||||||||
EST: Endoscopic sphincterotomy; LBD: Large-balloon dilation.
Procedure time
Only two studies reported the total procedure time[13,23]. Meta-analysis showed no difference in ERCP duration between EST plus LBD and EST alone (OR = 1.55, 95%CI: -2.34-5.44, P = 0.44, Figure 3B).
Publication bias
The funnel plot did not show an asymmetrical pattern (Figure 4). In addition, neither the Begg test nor the Egger test revealed significant publication bias (P = 0.148 and P = 0.426, respectively).
Figure 4.
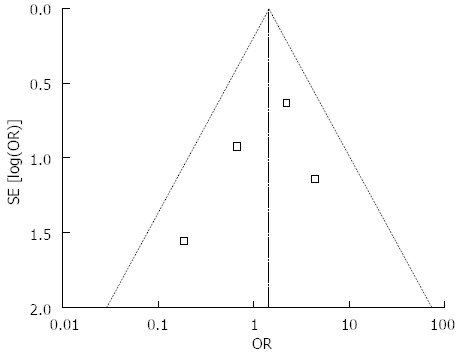
Funnel plot did not show publication bias.
DISCUSSION
We performed this meta-analysis mainly to investigate whether EST plus LBD was feasible and safe for the removal of large stones. Theoretically, a large enough opening to the papilla may facilitate the extraction of large bile duct calculi. Our meta-analysis suggested that EST plus LBD achieved an equivalent success rate in stone clearance to that of EST alone. The use of mechanical lithotripsy in the EST plus LBD group decreased significantly, especially in patients with a stone size larger than 15 mm. Mechanical lithotripsy is a challenging technique and may create many stone fragments that are then difficult to clear[25], thus it is worth reducing dependence on mechanical lithotripsy.
Recent data has suggested that LBD does not cause serious complications such as severe pancreatitis and bile duct perforation if performed strictly under established guidelines[5,6,22]. Similarly, the current meta-analysis demonstrated that the incidence of overall complications was significantly lower in the EST plus LBD group. When standard EST is performed to remove large stones, a full or large incision may be made, possibly leading to bleeding or perforation. Our review showed that perforation occurred in four patients in the EST alone group, and in none in the EST plus LBD group. Furthermore, bleeding was rarer when balloon dilation was performed (1.7% vs 3.1%) after limited sphincterotomy, although no significant difference was observed. We presume that this may be due to the small incision made before LBD.
Many concerns have been raised about post-ERCP pancreatitis with increasing balloon size, especially for those over 15 mm. However, our meta-analysis showed that LBD did not increase pancreatitis. Theoretically, the initial sphincterotomy may orientate the direction of subsequent dilation, leading to a resultant tear away from the pancreatic orifice, which might decrease the risk of pancreatitis. Post-ERCP pancreatitis may also be associated with other factors such as cannulation time and stone removal time. Only two studies reported the total procedure time[13,23], and meta-analysis showed no difference in ERCP duration between the two groups. We cannot estimate the effect of procedure duration on the risk of pancreatitis.
Only the study by Teoh et al[13] compared the direct cost of the procedures between the two groups. A significant reduction in overall cost was noted in the EST plus LBD group [USD $5025 (interquartile range, $4140-$5235) vs $6005 (interquartile range, $4462-$5441), P = 0.034]. Whether this combined technique is less expensive requires clarification by conducting further trials.
Our findings are similar to those of the previous meta-analysis by Liu et al[10]. This previous meta-analysis included three RCTs[22,23,26], and summarized the results of RCTs and non-RCTs separately. One trial included in the previous meta-analysis which performed dilation using a small (8 mm) balloon[26] was excluded in our review. A well-arranged trial was excluded in the previous meta-analysis because mechanical lithotripsy was used in all the patients in the EST group, but in none of the patients in the EST plus LBD group[24], which did not accurately reflect the use of mechanical lithotripsy. We conducted a sensitivity analysis by excluding this study, and the result did not change. By contacting the authors, we found two eligible abstracts[11,12] regarded as non-randomized in the previous meta-analysis, which were in fact randomized. Furthermore, our meta-analysis included a recently published well-designed trial by Teoh et al[13]. The previous meta-analysis showed a significant reduction in the use of mechanical lithotripsy and overall complications for non-RCTs, but not for RCTs. However, our meta-analysis showed that EST plus LBD caused fewer overall complications than EST alone, and the result did not change by restricting the meta-analysis to high-quality studies. In addition, our meta-analysis showed that the use of mechanical lithotripsy in the EST plus LBD group decreased significantly, especially in patients with a stone size larger than 15 mm.
This meta-analysis also has some limitations. Firstly, it included two low-quality trials. It has been well documented that in RCTs and meta-analyses, low-quality studies are vulnerable to bias and may lead to exaggerated results. However, subgroup analysis of high-quality studies was also significant, which strengthened the results. Secondly, only a few studies were included, which might decrease the robustness of the analysis and mask publication bias. Our meta-analysis showed that the significant reduction in perforations in the EST plus LBD group was marginal (P = 0.05), this was probably attributable to the small number of subjects with perforation (n = 4, all in the EST alone group).
In conclusion, large-balloon dilation following limited sphincterotomy appears to be an effective approach for large stone extraction. This method may cause fewer complications and reduce dependence on mechanical lithotripsy. However, it warrants more well-designed studies to clarify whether this combined technique is outweighed.
COMMENTS
Background
Endoscopic sphincterotomy (EST) or endoscopic papillary balloon dilation (EPBD) is the standard method for stone retrieval. However, the extent of orifice dilation with conventional EST or EPBD is limited, and the use of other methods, such as mechanical lithotripsy, may be required in patients with large stones. A larger opening of the orifice by large-balloon dilation (LBD) may facilitate stone removal. For the past few years, LBD following limited EST appears to be an alternative to EST alone for removing large bile duct stones. However, which one is predominant remains controversial.
Research frontiers
The current meta-analysis was carried out to comparatively assess LBD plus EST and EST alone for removal of large bile duct stones. The main outcome measurements included complete stone removal, stone removal in first session, use of mechanical lithotripsy, procedure time, and procedure-related complications.
Innovations and breakthroughs
The current meta-analysis demonstrated that EST plus LBD is an effective approach for the removal of large bile duct stones, causing fewer complications than EST alone. Furthermore, this combined technique may decrease dependence on mechanical lithotripsy during stone extraction.
Applications
The results from this meta-analysis suggest that LBD following limited EST is an effective alternative to EST alone for removing large bile duct stones, warranting routine clinical use.
Peer review
This is an interesting and well performed meta-analysis addressing the efficacy of EST plus LBD vs EST alone for removal of bile duct stones. The research design is solid, and its results have clinical relevancy as they demonstrate that EST plus LBD decreases complications and the usage of mechanical lithotripsy.
Footnotes
P- Reviewers: Messori A, Shi ZJ S- Editor: Qi Y L- Editor: Rutherford A E- Editor: Wang CH
References
- 1.Katanuma A, Maguchi H, Osanai M, Takahashi K. Endoscopic treatment of difficult common bile duct stones. Dig Endosc. 2010;22 Suppl 1:S90–S97. doi: 10.1111/j.1443-1661.2010.00979.x. [DOI] [PubMed] [Google Scholar]
- 2.Attam R, Freeman ML. Endoscopic papillary large balloon dilation for large common bile duct stones. J Hepatobiliary Pancreat Surg. 2009;16:618–623. doi: 10.1007/s00534-009-0134-2. [DOI] [PubMed] [Google Scholar]
- 3.Attam R, Freeman ML. Endoscopic papillary balloon dilation for stone extraction: if, when, and for how long? Gastrointest Endosc. 2010;72:1163–1166. doi: 10.1016/j.gie.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 5.Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958–961. doi: 10.1055/s-2007-966784. [DOI] [PubMed] [Google Scholar]
- 6.Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–2182. doi: 10.3748/wjg.v13.i15.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy. 2008;40:209–213. doi: 10.1055/s-2007-967040. [DOI] [PubMed] [Google Scholar]
- 8.Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560–565. doi: 10.1038/ajg.2008.67. [DOI] [PubMed] [Google Scholar]
- 9.Kim TH, Oh HJ, Lee JY, Sohn YW. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg Endosc. 2011;25:3330–3337. doi: 10.1007/s00464-011-1720-3. [DOI] [PubMed] [Google Scholar]
- 10.Liu Y, Su P, Lin Y, Lin S, Xiao K, Chen P, An S, Bai Y, Zhi F. Endoscopic sphincterotomy plus balloon dilation versus endoscopic sphincterotomy for choledocholithiasis: A meta-analysis. J Gastroenterol Hepatol. 2013;28:937–945. doi: 10.1111/jgh.12192. [DOI] [PubMed] [Google Scholar]
- 11.Hong GY, Park SW, Seo KS, Moon H. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of large common bile duct stones. Gastrointest Endosc. 2009;69:AB148. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 12.Kim TH, Oh HJ, Im CJ, Choi CS, Kweon JH, Sohn YW. A comparative study of outcomes between endoscope sphincterotomy plus endoscope papillary large balloon dilation and endoscopic sphincterotomy alone in patients with large extrahepatic bile duct stones. Gastrointest Endosc. 2009;69:AB156. [Google Scholar]
- 13.Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, Chiu PW, Wong SK, Chan FK, Lau JY. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology. 2013;144:341–345.e1. doi: 10.1053/j.gastro.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 14.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 15.Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985;27:335–371. doi: 10.1016/s0033-0620(85)80003-7. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robins J, Breslow N, Greenland S. Estimators of the Mantel-Haenszel variance consistent in both sparse data and large-strata limiting models. Biometrics. 1986;42:311–323. [PubMed] [Google Scholar]
- 19.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 20.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 21.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–726; quiz 768, 771. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 23.Kim HG, Cheon YK, Cho YD, Moon JH, Park do H, Lee TH, Choi HJ, Park SH, Lee JS, Lee MS. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298–4304. doi: 10.3748/wjg.15.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M, et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278–285. doi: 10.1038/ajg.2010.421. [DOI] [PubMed] [Google Scholar]
- 25.Leung JW, Tu R. Mechanical lithotripsy for large bile duct stones. Gastrointest Endosc. 2004;59:688–690. doi: 10.1016/s0016-5107(04)00174-9. [DOI] [PubMed] [Google Scholar]
- 26.Liu F, Li F, Zhou Y, Li Z. Minor endoscopic sphincterotomy plus endoscopic balloon dilation is an effective and safer alternative for endoscopic sphincterotomy during ERCP in patients with periampullary diverticula and bile duct stones. Gastrointest Endosc. 2008;67:AB230. [Google Scholar]


