Abstract
Appropriate identification and precise resection of the pincer lesion are integral parts of the arthroscopic surgical treatment of femoroacetabular impingement. Preoperative radiographic planning of the bone resection, as well as executing the plan intraoperatively using both fluoroscopic and arthroscopic cues, is critical to adequately removing the pincer lesion. We present our surgical technique of removing the impinging bone by defining the focal acetabular rim overcoverage, accessing the pincer lesion with labral detachment, and then performing acetabular rim resection.
Femoroacetabular impingement (FAI) has become a well-recognized pathologic condition that is responsible for many cases of secondary osteoarthritis of the hip in young adults.1 Two distinct bony morphologic subtypes of FAI exist: the acetabular-sided pincer lesion and the femoral-sided cam lesion. However, the majority of cases exist as a combination of both of these subtypes.2 Pincer lesions can result from localized anterolateral overcoverage, anterior overcoverage from true retroversion of the acetabulum, or global overcoverage (present with coxa profunda and acetabular protrusio). More recently, subspine impingement has also been recognized as an etiology of pincer-sided lesions.3 Cam lesions can result either from an aspherical femoral head or from a decreased femoral head–neck ratio.
Pincer and cam subtypes of FAI also result in distinct patterns of labral and articular cartilage injury. The presence of a pincer lesion creates a mechanical conflict in which the labrum is repetitively crushed between the acetabular rim and the abutting femoral neck. This leads to localized anterolateral damage to the labrum, marginal articular cartilage wear, and a contrecoup lesion of the posterior articular cartilage from shear forces as the femoral head is repetitively levered out of the acetabulum. Conversely, cam lesions result in delamination of articular cartilage in the anterosuperior aspect of the acetabulum from shear forces created as the aspherical cam lesion is repetitively forced into a spherical acetabulum.
Surgical management of FAI attempts to address all of the soft-tissue and bony abnormalities present in the patient. With respect to pincer lesions, this often necessitates focal acetabular rim resection and subspine decompression. The focal rim resection can be accomplished either with or without labral detachment, followed by either labral refixation or debridement, as determined by the labral tissue quality. Video 1 describes the technique for acetabular rim resection after labral detachment for a large (>3 mm) pincer lesion.
Surgical Technique
Preoperative Planning
In our experience, preoperative planning of the pincer lesion resection is essential to avoid either under-resection, leading to residual impingement, or over-resection, leading to iatrogenic creation of a dysplastic acetabulum (Table 1). This planning can be accomplished on a true anteroposterior pelvic radiograph (the distance from the pubic symphysis to the tip of the coccyx must be 1 to 3 cm, and the obturator foramina must be symmetric in appearance4) by determining the depth of bony resection required to eliminate the crossover sign. Intraoperative fluoroscopic imaging is then set up to precisely match the preoperative image, allowing for direct comparison of the actual resection and the planned resection throughout the procedure.
Table 1.
Key Points of Acetabular Rim Resection
| Use preoperative radiographic planning to determine the depth of the bony resection required to eliminate the crossover sign. |
| Obtain adequate exposure through an inter-portal capsulotomy, followed by capsular elevation away from the labral edge. |
| Remove all soft tissue from the acetabular rim using an ArthroCare RF wand. |
| Confirm the position and extent of the pincer lesion using fluoroscopy. |
| Detach the labrum to expose all areas of tearing and articular cartilage delamination. |
| Resect the pincer lesion using a hip-specific, 5.5-mm burr. |
| Use fluoroscopy to verify that an adequate resection has been performed. |
| Recognize and resect a prominent AIIS. |
| Remove any excess articular cartilage back to a stable bone-cartilage interface. |
Surgical Exposure
Access to the hip joint is gained in the usual fashion by use of anterolateral and mid-anterior portals. For the majority of the procedure, the anterolateral portal is used as the viewing portal and the mid-anterior as the working portal. Adequate exposure is required to ensure complete resection of the pincer lesion. This necessitates an inter-portal capsulotomy from the anteromedial to posterolateral margin of the acetabular rim. A formal capsulectomy is avoided, particularly in cases for which a capsular repair is planned. After capsulotomy, the capsule is carefully elevated on the acetabular side from the labral edge extending proximally to the attachment of the indirect arm of the rectus tendon and the capsular reflection. Our preference is to use an ArthroCare RF 50° wand (ArthroCare, Austin, TX) to accomplish this (Fig 1), as well as a hip-specific shaver (Stryker, San Jose, CA). The wand is further used to remove all soft tissue remaining on the acetabular rim, and this fully exposes the pincer lesion. The rectus tendon can serve as a useful landmark for orientation during this process because it is located at the 12-o'clock position on the acetabulum. Fluoroscopy can be used to further confirm the position and extent of the pincer lesion, as well as to verify that the pincer lesion, and not a prominent anterior inferior iliac spine (AIIS), is responsible for the radiographic crossover sign.5
Fig 1.

Arthroscopic view of right acetabulum and labrum (asterisk) as viewed through anterolateral portal. The ArthroCare RF wand is being used through a mid-anterior portal to elevate the capsule (plus sign) to fully expose the pincer lesion. The pound sign indicates the femoral head.
Labral Detachment
Once all of the soft tissue has been successfully removed, the next step is labral detachment. Although small pincer lesions (<3 mm) can be resected without labral detachment, larger lesions cannot be adequately addressed without first detaching the labrum.6 First, the wand is used to gently tease the labrum away from the most distal portion of the pincer lesion (Fig 2A). This provides visualization of the chondrolabral junction so that further labral separation can be performed by use of a freer elevator (Arthrex, Naples, FL) and/or a sharp surgical blade, such as the Arthrex Banana Blade (Fig 2B). Enough labrum is detached so that all areas of tearing and articular cartilage delamination are exposed.
Fig 2.
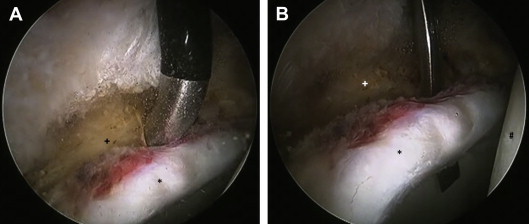
(A) Arthroscopic view of right acetabulum and labrum (asterisk) as viewed through anterolateral portal. The ArthroCare RF wand is being used through the mid-anterior portal to initiate detachment of the labrum at the chondrolabral junction. (B) A freer elevator can also be used to facilitate detachment of the labrum (asterisk). The plus sign indicates the acetabular rim, and the pound sign indicates the femoral head.
Bony Resection
Once the labrum is fully detached, the bony pincer lesion can be resected with a hip-specific, 5.5-mm round burr (Stryker) (Fig 3). We use this burr in the reverse setting because we find that this allows for removal of any remaining soft tissue and for a more controlled bony resection. The resection is initiated anteromedially and is transitioned back toward the camera going anteriorly, anterolaterally, and finally, posterolaterally as needed. The appropriate amount of bony resection is determined and verified in numerous ways. First, the preoperatively planned depth of resection (based on elimination of the crossover sign) is compared with the width of the burr (5.5 mm) to set an initial resection level. Second, once the pincer lesion has been adequately removed, the yellowish-white color and firm texture of the pincer lesion bone give way to a pinkish hue and softer texture of cancellous bone that are indicative of native acetabular bone. Third, evaluation of the bone–articular cartilage junction may influence the intraoperative decision to perform further acetabular rim resection if a large area of damaged articular cartilage is found. Lastly, fluoroscopy is used to ensure that the preoperative resection plan is achieved (Fig 4).
Fig 3.
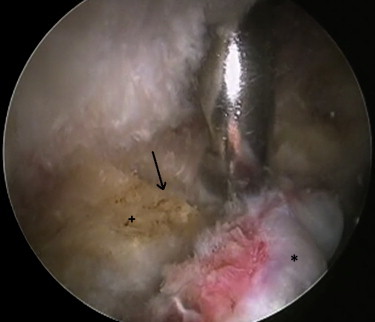
Arthroscopic view of right acetabular rim (plus sign) as viewed through anterolateral portal. The burr is being used through the mid-anterior portal to resect the pincer lesion. The arrow points to a ledge of remaining bone and shows the depth of the bony resection. The asterisk indicates the labrum.
Fig 4.
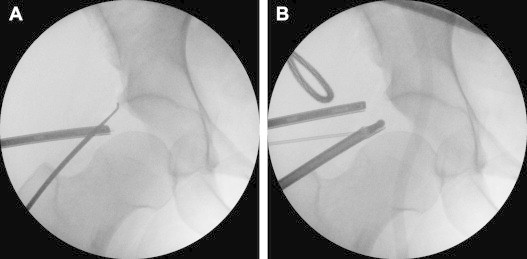
Anteroposterior fluoroscopic images of right hip from before (A) and after (B) pincer resection, with resolution of crossover sign.
During the process of bony resection, it is also important to address subspine impingement caused by a prominent AIIS. This is an area visualized as a “second teardrop” on fluoroscopy at the 11-o'clock position on the lateral acetabulum, and it may also contribute to formation of the radiographic crossover sign.5 Adequate resection can be verified by swapping the viewing and working portals. Once the surgeon is viewing from the mid-anterior portal, the arthroscope is positioned immediately adjacent to the rectus attachment and capsular reflection. From this viewing position, the area of pincer resection should be completely smooth and flat and there should be no remaining overhang from the previously prominent AIIS.3
Delaminated Cartilage Resection
Once the bony resection has been completed, there may be remaining proud articular cartilage. A medium, straight-tip, 3.4-mm punch (Arthrex) is used to remove this excess cartilage back to a stable bone-cartilage interface (Fig 5). At this point, the pincer resection has been completed, and the area has been adequately prepared for labral reattachment (Fig 6).
Fig 5.

Arthroscopic view of right acetabulum and labrum (asterisk) as viewed through anterolateral portal. The medium straight punch is being used through a mid-anterior portal to remove excess cartilage to achieve a stable bone-cartilage interface. The plus sign indicates the acetabular rim.
Fig 6.

Arthroscopic view of right acetabulum and labrum (asterisk) as viewed through anterolateral portal, showing completed pincer resection. The plus sign indicates the acetabular rim.
Discussion
Surgical treatment of pincer lesions by labral detachment and acetabular rim resection is an integral part of the surgical treatment of FAI. These procedures are most commonly combined with either labral debridement or refixation, as determined by tissue quality, and femoral neck osteoplasty to treat FAI. A recent systematic review reported that surgical management of FAI (arthroscopic and/or open procedures) is efficacious in improving patient symptoms, particularly in those patients without advanced osteoarthritis or chondral damage.7 Other recent studies specifically report on the ability of arthroscopic procedures to improve quality of life8 and hip-specific outcome scores9 and to return athletes to high-level activities.10 Although the ultimate outcome would be to delay or prevent the progression of osteoarthritis, there is insufficient long-term follow-up currently to support this in comparison to the natural history of the condition.7
Pincer resection was initially developed as an open surgical procedure. Two recent systematic reviews similarly concluded that open, mini-open, and arthroscopic surgeries are equally efficacious in improving pain and function but that arthroscopic methods have a lower rate of major complications when performed by experienced surgeons and have a shorter rehabilitation period.11,12 Certain FAI cases, however (namely, the retroverted acetabulum with posterior undercoverage and the dysplastic acetabulum with a center-edge angle ≤20°), are potentially inappropriate for arthroscopic management. Resection of the anterior acetabular rim, in these instances, may result in global undercoverage and hip instability. A periacetabular osteotomy should be considered in these cases.
Although the possibility of creating an unstable hip because of over-resection does exist, a more common complication is the persistence of FAI because of an inadequate resection. In series reported by Philippon et al.13 and Heyworth et al.,14 either inadequate resection or complete failure to address a bony lesion was the operative indication in 92% and 79%, respectively, of revision cases. The previously described technique of labral detachment before pincer resection allows for excellent visualization of anterosuperior pincer lesions, which—in combination with fluoroscopic imaging—increases the likelihood of an adequate resection. This is important because dynamic assessment of impingement is not possible during arthroscopy of the central compartment.15 In addition, with this technique, the depth of pincer resection that can be performed is not limited by a need to maintain the stability of the chondrolabral junction; in fact, small areas of chondral delamination can be resected after labral detachment and bony resection and before labral repair. A cadaveric study by Zumstein et al.,15 however, did show that pincer resection performed without a posterolateral portal tends to inadequately address posterosuperior pincer lesions. Because the posterolateral portal endangers significant neurovascular structures, they recommend that hip arthroscopy be limited to the treatment of anterosuperior, and not posterosuperior, pincer lesions.
Acetabular rim resection is a powerful tool in the treatment of FAI. This article and the accompanying video have described our preferred technique for planning and performing arthroscopic labral detachment and acetabular rim resection. Careful selection of patients, preoperative planning, and performing adequate pincer resection are important determinants of successful outcome.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Arthroscopic technique for acetabular rim resection after labral detachment for a large (>3 mm) pincer lesion in the right hip.
References
- 1.Ganz R., Parvizi J., Beck M., Leunig M., Notzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Beck M., Kahlhor M., Leunig M., Ganz R. Hip morphology influences the pattern of acetabular cartilage damage. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Larson C.M., Kelly B.T., Stone R.M. Making a case for anterior inferior iliac spine/subspine hip impingement: Three representative case reports and proposed concept. Arthroscopy. 2011;27:1732–1737. doi: 10.1016/j.arthro.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Clohisy J.C., Carlisle J.C., Beaulé P.E. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaltz I., Kelly B.T., Hetsroni I., Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471:2192–2198. doi: 10.1007/s11999-012-2689-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fry R., Domb B. Labral base refixation in the hip: Rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26(suppl 1):81–89. doi: 10.1016/j.arthro.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 7.Ng V.Y., Arora N., Best T.M., Pan X., Ellis T.J. Efficacy of surgery for femoroacetabular impingement: A systematic review. Am J Sports Med. 2010;38:2337–2345. doi: 10.1177/0363546510365530. [DOI] [PubMed] [Google Scholar]
- 8.Malviya A., Stafford G.H., Villar R.N. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg Br. 2012;94:466–470. doi: 10.1302/0301-620X.94B4.28023. [DOI] [PubMed] [Google Scholar]
- 9.Nho S.J., Magennis E.M., Singh C.K., Kelly B.T. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39(suppl 1):14S–19S. doi: 10.1177/0363546511401900. [DOI] [PubMed] [Google Scholar]
- 10.Fabricant P.D., Heyworth B.E., Kelly B.T. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop Relat Res. 2012;470:261–269. doi: 10.1007/s11999-011-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsuda D.K., Carlisle J.C., Arthurs S.C., Wierks C.H., Philippon M.J. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27:252–269. doi: 10.1016/j.arthro.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Botser I.B., Smith T.W., Jr., Nasser R., Domb B.G. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: A comparison of clinical outcomes. Arthroscopy. 2011;27:270–278. doi: 10.1016/j.arthro.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 14.Heyworth B.E., Shindle M.K., Voos J.E., Rudzki J.R., Kelly B.T. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 15.Zumstein M., Hahn F., Sukthankar A., Sussmann P.S., Dora C. How accurately can the acetabular rim be trimmed in hip arthroscopy for pincer-type femoral acetabular impingement: A cadaveric investigation. Arthroscopy. 2009;25:164–168. doi: 10.1016/j.arthro.2008.09.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic technique for acetabular rim resection after labral detachment for a large (>3 mm) pincer lesion in the right hip.


