Abstract
Patellar instability is a common complaint after traumatic dislocation of the patella. Traumatic dislocation always leads to tearing of the medial patellofemoral ligament (MPFL). Treatment consists of recovery from the traumatic injury, followed by reconditioning and physical therapy to strengthen the dynamic stabilizers of the patella. In patients with recurrent instability, detailed evaluation of the cause is required to determine the needed interventions. In patients with an incompetent MPFL and recurrent instability, reconstruction is indicated, along with other procedures to address other contributing factors. This article details our technique for MPFL reconstruction using semitendinosus autograft, which can be performed alone or in concert with other realignment procedures.
Patellofemoral complaints are common in orthopaedic practice. Most commonly, this is because of pain. A subset of these patients have a chief complaint of patellofemoral instability. The incidence of patellar dislocation is up to 78 in 100,000, and 15% to 40% of first-time dislocations treated conservatively go on to repeat dislocation.1-3 In this subset of patients, there are multiple causes of instability.
Anatomic abnormalities can lead to patellar instability. Valgus alignment at the knee leads to an increased Q angle and increased lateral tension on the patella. Similarly, rotational malalignment of the extremity—specifically, increased femoral anteversion combined with external tibial torsion—leads to increased lateral tension on the patella. With increased flexion at the knee, the bony constraints become more important and trochlear dysplasia can lead to insufficient constraint in flexion.4 Patients with patella alta engage their bony constraints at a deeper flexion angle and can therefore be more prone to subluxation and dislocation. In extension the important static constraint to lateral subluxation and dislocation is the medial patellofemoral ligament (MPFL).5 In this same range, the vastus medialis obliquus acts as a dynamic restraint to instability. The patient may also have a lateralized insertion of the patella leading to lateral tracking of the patella. In any single patient, several of these factors can act together, leading to his or her symptoms.
In patients with traumatic causes, there is always tearing of the MPFL that leads to loss of static medial stabilization (Fig 1).6,7 After these patients have recovered from their traumatic injury and undergone generalized reconditioning with specific physical therapy, including vastus medialis obliquus strengthening for instability,8 they may require surgical reconstruction of their MPFL for stabilization. The other causes highlighted earlier must be evaluated to determine the need for additional procedures. This article describes our technique for MPFL reconstruction with semitendinosus autograft that can be used alone or in combination with other stabilizing procedures.
Fig 1.

A T2-weighted axial magnetic resonance image of the knee of a patient with an MPFL tear (asterisk) after traumatic dislocation.
Surgical Technique
The patient is placed in a supine position on a standard operating table. A tourniquet is then placed on the proximal thigh. The patient is prepared per our standard procedure with ethanol followed by ChloraPrep (Care Fusion, San Diego, CA). A down sheet is then placed under the limb, and the foot and ankle are placed in a stockinet and wrapped in Coban self-adhering wrap (3M, St. Paul, MN). This is followed by sterile U-drapes and an extremity drape. The C-arm fluoroscopy unit is positioned on the operative side, and the scrub nurse's sterile field is positioned at the foot of the bed. The patient is examined under anesthesia to confirm patellar instability. A diagnostic arthroscopy is then completed by the surgeon, noting trochlear morphology and the ability to displace the patella laterally.
The semitendinosus is harvested through an incision over the pes anserine, similar to the incisions used for graft harvest for other reconstructive procedures. The pes anserine is palpated, and a 3- to 4-cm incision is made 2 cm medial to the tibial tubercle. The soft tissue is dissected down to the sartorial fascia, and the semitendinosus is visualized. The fascia is then incised, and the semitendinosus is identified and bluntly dissected with a right-angle clamp. Blunt dissection is continued medially to define the interval between the superficial medial collateral ligament and the semitendinosus. The tendon is then sharply released from its insertion on the tibia and whipstitched with a No. 2 FiberWire (Arthrex, Naples, FL). Blunt dissection is used to identify any adhesions on the tendon. These adhesions are released with Metzenbaum scissors. The index finger is then run along the tendon to the musculotendinous junction to confirm that all adhesions have been released. The tendon is released by use of a tendon stripper and brought to the back table for preparation. The graft is approximately 10 cm in length and 4.5 to 5 mm in diameter. The pes anserine is then closed with a No. 1 Vicryl suture (Ethicon, Somerville, NJ), and the subcutaneous tissue is closed with No. 2-0 Monocryl (Ethicon).
Attention is then brought to the patella: a 2.5- to 3-cm longitudinal incision is made along the medial aspect of the upper one-third of the patella (Fig 2A). Soft-tissue dissection is then taken down to the bone, which is exposed subperiosteally. A guidewire with the C-arm positioned for a lateral view of the knee is used to localize the junction between the proximal and middle third of the patella (Figs 2B and 2C). It is then drilled into the patella by approximately 25 mm. C-arm fluoroscopy is used to confirm that the guidewire is centered in the anterior-to-posterior direction with a slight angulation posteriorly in the patella so that reaming will not violate either cortex. A 5-mm cannulated reamer from the Bio-Tenodesis set (Arthrex) is then used to ream the patella by approximately 20 to 25 mm, with frequent cleaning of the reamer blade every few millimeters or so to avoid thermal insult to the patella (Fig 2D, Video 1).
Fig 2.
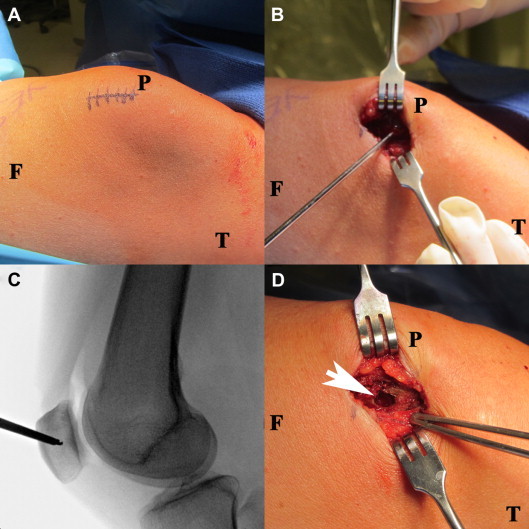
The patient is in the supine position with the left leg draped with an extremity drape. (F, femur; P, patella; T, tibia.) (A) An image from the right side of the patient with the skin incision marked on the superior and medial aspect of the left patella. (B) The skin is incised, and dissection is completed down to the patella; the guidewire for reaming the patellar tunnel is then placed at the junction of the middle and proximal third of the patella. (C) A fluoroscopic lateral image of the left knee is then obtained to localize the guidewire for proper drilling of the patella at the middle and superior third. (D) The patella is reamed to create the tunnel on the medial aspect (arrowhead) using a 5-mm reamer to ream a tunnel with a length of 20 mm, as pictured.
Attention is then brought to the femur. The knee is flexed, and a perfect lateral view of the knee is obtained with the C-arm (Fig 3A). A radiopaque clamp is used to visualize the Schottle point, the intersection of the anterior aspect of the posterior cortical line of the femur and the Blumensaat line. This is the natural anatomic insertion of the MPFL. This site is marked on the skin, a 2- to 3-cm incision is made, and the soft tissues are dissected down to the femur. A Beath pin is then advanced in a proximal and anterior direction through the femur. The C-arm is used to confirm the position of the pin. A 6- or 7-mm cannulated reamer is then reamed to a distance of 45 mm into the femur (Fig 3B). The Beath pin is used to pass an Ethibond passing suture (Ethicon) through the femur. Then, an extrasynovial tunnel that is deep to the subcutaneous soft tissues is created by blunt dissection between the anterior incision on the patella and the posterior incision on the femur. A clamp is used to place another passing stitch from the femoral incision to the patellar incision (Video 1).
Fig 3.
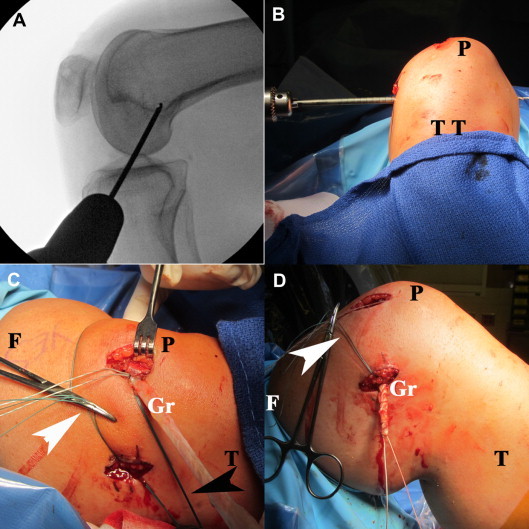
The patient is positioned in the supine position with the left leg draped with an extremity drape. (F, femur; Gr, graft; P, patella; T, tibia; TT, tibial tubercle.) (A) Fluoroscopic lateral image of the knee with the drill bit placed at the Schottle point to localize drilling of the femoral tunnel. (B) Image taken from the foot of the bed with the reamer engaged on the medial side of the femur. Reaming of the femoral tunnel was performed from the medial side of the femur (left) to lateral (right). One can see the guide pin out of the lateral aspect of the femur (right). (C) The semitendinosus graft is secured in the medial aspect of the patella with the passing sutures in place to pass the graft to the femoral insertion. The extrasynovial passing suture (black arrowhead) and femoral passing suture (white arrowhead) are clamped in position, ready to pass the graft. (D) Image after the graft has been passed through the extrasynovial/subcutaneous tunnel from the patellar insertion to the femoral insertion site. It has been whipstitched and is ready to be tensioned and secured in the femur after use of the passing suture (white arrowhead) to place the graft in the femoral tunnel.
The graft is now placed. The FiberWire end of the graft is threaded through a 4.75- or 5.5-mm Bio-Tenodesis screw and inserted into the patellar bone tunnel until it is secure (Fig 3C). The graft is then passed through the extrasynovial tunnel to the femoral incision (Fig 3D). The free end of the graft is whipstitched with a No. 2 Vicryl suture. The knee is placed in 50° to 60° of flexion, and an interference screw guide pin is placed in the femoral tunnel, replacing the Beath pin. The graft is then passed through the femur with the passing stitch. The slack is taken out of the graft with the knee at 50° to 60° of flexion, with care taken not to overtension it, and a 7 × 23–mm Arthrex interference screw is placed in the femoral tunnel until good purchase is obtained (Video 1).
Physical examination of the patella is then completed to confirm stability of the patella without over-constraint. The arthroscope is placed back in the knee, and patellar tracking is observed and the graft is visualized medially in its extra-articular position (Fig 4). The arthroscope is then removed, and the incisions are copiously irrigated with normal saline solution. The FiberWire from the Bio-Tenodesis screw is used to close the periosteum over the patella, and the subcutaneous tissue is closed with No. 2-0 Monocryl. The skin is then closed with a running stitch by use of No. 3-0 Prolene (Ethicon). The patient is placed in a knee immobilizer, and therapy is started postoperatively with unrestricted range of motion. The patient is allowed to bear weight as tolerated in the knee immobilizer. Return to sports is generally allowed at the 12- to 16-week range. Key points for each step of the procedure are further emphasized in Table 1.
Fig 4.
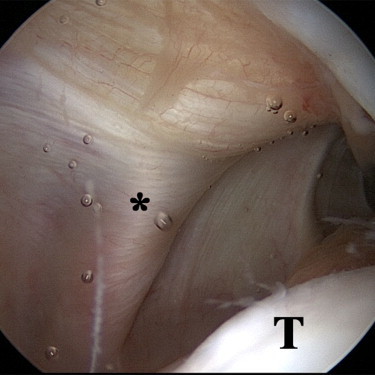
An arthroscopic image from the anterolateral portal of the left knee, in extension, shows the extra-articular semitendinosus graft (asterisk) used to reconstruct the MPFL. (T, trochlea.)
Table 1.
Summary of Main Steps of MPFL Reconstruction Technique With Associated Key Points for Each Step of Procedure
| Steps | Key points |
|---|---|
| Hamstring tendon harvest | Complete dissection of adhesions from semitendinosus, avoidance of damage to superficial medial collateral ligament |
| Patellar preparation | Placement at junction of proximal and middle third of patella, avoidance of violation of anterior cortex or subchondral bone, sequential reaming as described to avoid thermal insult to patella |
| Femoral preparation | Identification of Schottle point by fluoroscopy on true lateral view of knee for anatomic placement of graft |
| Graft placement | Extrasynovial dissection of tunnel for graft, proper placement of shuttling sutures to pass graft, avoidance of over-tightening of graft during femoral fixation |
Discussion
In patients with recurrent instability after patellar dislocation that continues after conservative management, MPFL reconstruction is indicated. There have been multiple techniques described for reconstruction of the medial constraints on the patella, from medial plication to ligament reconstruction. There is not sufficient evidence for any of these techniques over the others.9,10 Advantages of the described technique are that it is minimally invasive, it restores the main anatomic restraint to lateral patellar displacement, and the secure fixation technique allows for early motion and rehabilitation. A limitation of this technique is that it is designed to re-create the anatomic neutralizing force on the patella; it does not function to medialize the patella. Therefore other procedures may be needed along with this technique to address lower-limb malalignment, including valgus, rotational, and patellar malalignment. Other risks include patellar fracture and patellar femoral pain from over-tightening the graft, causing medial tracking (Table 2).
Table 2.
Advantages and Limitations/Risks of MPFL Reconstruction Technique
| Advantages |
| Limited dissection/percutaneous technique |
| Secure fixation of graft, allowing early motion and rehabilitation |
| Reconstruction of main anatomic restraint to lateral displacement |
| Limitations/risks |
| The technique does not function to medialize the patella, but it does restore the anatomic restraint/neutralizing force. |
| Incorrect anatomic placement can lead to stiffness, pain, and the need for revision. |
| Other procedures may be necessary to correct alignment issues (rotational osteotomy, patellar distalization/medialization, varus-producing osteotomy, and so on). |
| Over-tightening can lead to medial tracking of the patella and knee stiffness. |
| Incorrect reaming can lead to patellar fracture. |
Complications of MPFL reconstruction techniques include recurrent dislocation, patellar fracture, improper anatomic placement of graft, and over-tightening, leading to stiffness and pain.11,12 Because of the risk of patellar fracture, some surgeons advocate not drilling the patella. When we drill the patella using this technique, the tunnel is small (5 mm in diameter) and short (20 to 25 mm in length). It is performed under fluoroscopic guidance to make sure not to violate the subchondral bone or anterior cortex. In addition, when drilling, we only drill a few millimeters at a time and sequentially clean the drill to remove bony debris and limit thermal damage. In taking these precautions, we have not had a patellar fracture to date. With regard to over-tightening of the graft, all tightening and fixation are performed in 50° to 60° of flexion. This provides bony constraint to over-tightening of the graft because the patella is constrained in the trochlea at this range of flexion. Minimal force of tensioning is emphasized to avoid over-constraining the graft and altering patellofemoral contact pressures.13 In addition, if a lateral release is performed, this is always performed after tensioning the graft to prevent over-tightening medially. With the rigid fixation that we use with interference fit in bone tunnels, we are able to start early range of motion and rehabilitation without concern regarding graft subsidence. Patients are allowed immediate range of motion and weight bearing as tolerated in a knee immobilizer. The immobilizer is used for 2 to 3 weeks until patients regain control of their quadriceps function.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.T.B. receives support from Arthrex.
Supplementary Data
MPFL reconstruction technique with semitendinosus autograft. Semitendinosus graft is harvested in the normal fashion. The patellar and femoral tunnels are then created, followed by an extrasynovial soft-tissue tunnel between them. The graft is placed in the patella by use of an Arthrex Bio-Tenodesis screw, gently tensioned, and secured in the femur with an Arthrex interference screw.
References
- 1.Mehta V.M., Inoue M., Nomura E., Fithian D.C. An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc. 2007;15:78–81. doi: 10.1097/JSA.0b013e318042b695. [DOI] [PubMed] [Google Scholar]
- 2.Sillanpaa P., Mattila V.M., Iivonen T., Visuri T., Pihlajamaki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40:606–611. doi: 10.1249/MSS.0b013e318160740f. [DOI] [PubMed] [Google Scholar]
- 3.Trikha S.P., Acton D., O'Reilly M., Curtis M.J., Bell J. Acute lateral dislocation of the patella: Correlation of ultrasound scanning with operative findings. Injury. 2003;34:568–571. doi: 10.1016/s0020-1383(02)00382-0. [DOI] [PubMed] [Google Scholar]
- 4.Bollier M., Fulkerson J.P. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19:8–16. doi: 10.5435/00124635-201101000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 6.Mountney J., Senavongse W., Amis A.A., Thomas N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36–40. [PubMed] [Google Scholar]
- 7.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23:260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc. 2007;15:95–104. doi: 10.1097/JSA.0b013e318054e35c. [DOI] [PubMed] [Google Scholar]
- 9.Buckens C.F., Sarins D.B. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: A systematic review. Am J Sports Med. 2010;38:181–188. doi: 10.1177/0363546509353132. [DOI] [PubMed] [Google Scholar]
- 10.Ma L.F., Wang F., Chen B.C., Wang C.H., Zhou J.W., Wang H.Y. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: A randomized controlled trial. Arthroscopy. 2013;29:891–897. doi: 10.1016/j.arthro.2013.01.030. [DOI] [PubMed] [Google Scholar]
- 11.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bollier M., Fulkerson J., Cosgarea A., Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27:1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Beck P., Brown N.A., Greis P.E., Burks R.T. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557–1563. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
MPFL reconstruction technique with semitendinosus autograft. Semitendinosus graft is harvested in the normal fashion. The patellar and femoral tunnels are then created, followed by an extrasynovial soft-tissue tunnel between them. The graft is placed in the patella by use of an Arthrex Bio-Tenodesis screw, gently tensioned, and secured in the femur with an Arthrex interference screw.


