Abstract
Although the subscapularis has historically received less attention than posterosuperior rotator cuff tears, repair of a torn subscapularis tendon is critically important to restoring anatomy and achieving the best functional outcome possible. Arthroscopic repair begins with proper recognition of the tear. A systematic approach can then be used to arthroscopically repair all types of subscapularis tendon tears, from partial tears to full-thickness tears, as well as those which are retracted and have adhesions medially. Subscapularis footprint restoration can be accomplished with a variety of repair techniques that must be matched to the extent of the tear and mobility of the tendon.
Tears of the subscapularis were once thought to be uncommon but are now recognized to be present in nearly 30% of all arthroscopic shoulder procedures and approximately 50% of rotator cuff repairs.1-4 Although the subscapularis has historically received less attention than posterosuperior rotator cuff tears, for several reasons, recognition and repair of a torn subscapularis tendon are critically important to restoring anatomy and therefore achieving the best functional outcome possible. The subscapularis is the largest and most powerful of the rotator cuff muscles5 and is more important for arm elevation than either the supraspinatus or infraspinatus.6 Because it is the only anterior rotator cuff muscle, repair must be accomplished to balance the posterior forces of the rotator cuff.7,8 The upper portion of the subscapularis is particularly important because this is the part of the insertion that is broadest superiorly,9 and this site serves as the anterior attachment of the rotator cable.8 Finally, for tears extending into the supraspinatus, repair of the upper subscapularis decreases the stress on the adjacent repair of the supraspinatus.10 For these reasons, we believe that debridement alone of the subscapularis tendon should be contraindicated in the vast majority of cases.
Repair of the subscapularis tendon begins with proper recognition. Once recognized, a systematic approach can used to arthroscopically repair all subscapularis tendon tears regardless of the degree of retraction or fatty degeneration. This technical note describes our current approach to arthroscopic management of subscapularis tendon tears (Videos 1-3).
Surgical Technique
Order of Steps
Repair of the subscapularis requires that the surgeon must be comfortable working in the subcoracoid space. Because this space can become compromised rapidly by soft-tissue swelling from fluid extravasation, it is critical to address the subscapularis before repairing the rest of the cuff. In general, when the subscapularis is torn, the order of steps is as follows:
-
1.
Perform diagnostic arthroscopy
-
2.
Perform biceps tenotomy and whipstitching in preparation for tenodesis
-
3.
Make a window in the rotator interval
-
4.
If the subscapularis tendon has adhesions, then perform skeletonization of the posterolateral coracoid and perform a 3-sided release
-
5.
Perform a coracoplasty if indicated (i.e., if the subcoracoid coracohumeral distance is <7 mm)
-
6.
Prepare the lesser tuberosity bone bed
-
7.
Repair the subscapularis tendon
-
8.
Complete the biceps tenodesis
-
9.
Repair the remainder of the rotator cuff
Diagnostic Arthroscopy
The patient is placed in the lateral decubitus position, and the arm is placed in balanced suspension or an articulating arm holder at 20° to 30° of abduction and 20° of forward flexion. The subscapularis is initially inspected with a 30° arthroscope, viewing through a posterior portal. During subscapularis tendon repair, we view exclusively through a posterior portal and switch between 30° and 70° arthroscopes as needed.
Retracted tears are the most obvious and are located by a torn medial biceps sling, which creates a “comma sign.”11 The medial sling, composed of the medial coracohumeral ligament and the superior glenohumeral ligament, normally inserts at the superior lesser tuberosity adjacent to the superolateral subscapularis footprint (Fig 1). When the upper subscapularis tears away from its bone attachment, the medial sling also tears away from the bone and forms a distinctive comma-shaped arc of soft tissue (comma sign) at the superolateral corner of the subscapularis (Fig 2). Identification of this structure therefore always leads to the superolateral subscapularis tendon, even when the tendon is severely retracted and has adhesions medially.
Fig 1.
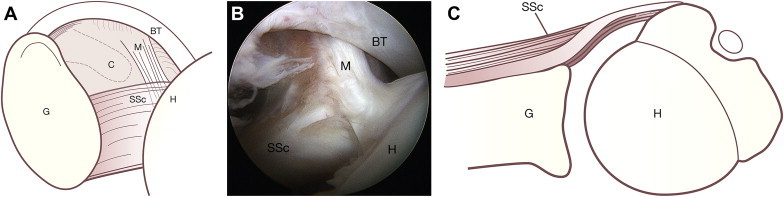
Drawing (A) and corresponding arthroscopic photograph (B) representing view of anterior structures from a posterior viewing portal in a right shoulder. (C) An axial schematic drawing further clarifies the normal anatomy. The medial sling (M) of the biceps tendon (BT) inserts onto the lesser tuberosity of the humerus (H), along with the superolateral margin of the subscapularis (SSc). (C, coracoid; G, glenoid.) (Reprinted with permission.20)
Fig 2.
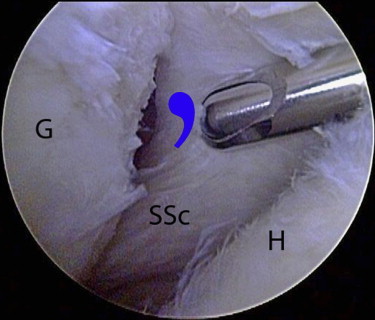
Right shoulder viewed from posterior viewing portal. In the setting of a retracted subscapularis tear, the medial sling tears away from the bone with the subscapularis tendon. The medial sling forms a distinctive comma-shaped arc of soft tissue (blue comma) at the superolateral corner of the subscapularis. As shown in this photograph, the comma sign serves as a landmark for locating a retracted subscapularis tendon. (G, glenoid; H, humeral head, SSc, subscapularis tendon.) (Reprinted with permission.20)
Non-retracted and occult tears of the subscapularis tendon can be overlooked but are equally important to recognize. Non-retracted tears may be either full-thickness tears or partial articular surface tendon avulsions (PASTAs). Occult tears are hidden by an intact medial sling and can be visualized on the articular side or in the bicipital groove. Many of these tears go unrecognized because the footprint is not fully visualized. With a posterior viewing portal, the subscapularis footprint can only be fully visualized with a 70° arthroscope (Fig 3). Visualization can also be enhanced with a posterior lever push and internal rotation of the arm. A bare lesser tuberosity is indicative of tearing and will indicate either a PASTA lesion or full-thickness tear that extends into the bicipital groove. It is important to inspect the medial biceps tendon for abrasive changes at the level of the medial sling, which indicates biceps subluxation and therefore a tear of the upper subscapularis. Next, an inspection is made for occult tears. One type of occult tear is a variant of a short PASTA lesion at the upper subscapularis combined with an intact medial sling. In rare instances of PASTA lesions, the medial sling remains intact and can effectively block the visualization of an upper subscapularis tear. To identify this tear, the 70° arthroscope must be used to “look around the corner” of the intact medial sling to observe the bare footprint under the torn subscapularis. Finally, the 70° arthroscope is used to push the biceps tendon laterally and inspect the medial bicipital groove. Disruption of the medial bicipital groove indicates an occult tear of the subscapularis and occurs in the upper, middle, or lower portions of the tendon insertion.12
Fig 3.
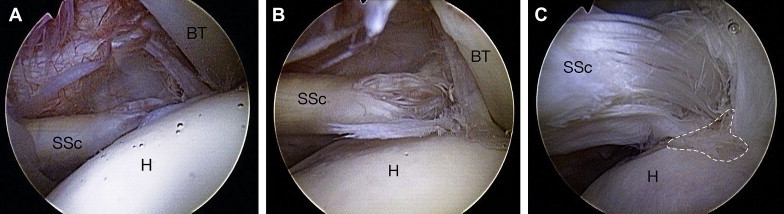
(A) Right shoulder viewed from posterior viewing portal with 30° arthroscope. The footprint of the subscapularis (SSc) is poorly visualized. (B) In the same shoulder, the use of a 70° arthroscope improves visualization, but in the standard lateral decubitus position, the subscapularis tendon is draped over the lesser tuberosity, obstructing the view of the lesser tuberosity footprint. (C) The same shoulder viewed with a 70° arthroscope and a posterior lever push. This maneuver dramatically increases the exposure of the subscapularis footprint, providing much more room for visualization, instrumentation, and bone bed preparation. In this case an exposed subscapularis footprint (white dashes) is quite evident at the 4-o'clock position in this picture. (BT, biceps tendon; H, humeral head.) (Reprinted with permission.18)
Biceps Tenodesis
In almost all cases of a subscapularis repair, we perform a biceps tenodesis, typically with an interference screw. After the surgeon identifies a subscapularis tear, an anterosuperolateral (ASL) portal is established, viewing with a 30° arthroscope, using an 18-gauge spinal needle as a guide. This portal is typically 1 to 2 cm lateral to the anterolateral acromion, but placement can vary and should be such that it provides a 5° to 10° angle of approach to the lesser tuberosity and is parallel to the subscapularis tendon. An 8.25 mm threaded clear cannula is placed in this portal.
Our technique for arthroscopic biceps tenodesis is summarized in brief in this article but has been described in detail previously.13 Through the ASL portal, 2 half-racking No. 2 FiberWire sutures (Arthrex, Naples, FL) are placed as traction sutures in the biceps tendon, and then a tenotomy is performed. The biceps is exteriorized, secured with a whipstitch, sized, allowed to retract into the shoulder, so that it can later be retrieved for tenodesis. Greater access to the subscapularis insertion is provided by performing the biceps tenotomy first.
Accessing Subcoracoid Space
Accessing the subcoracoid space is an essential component of subscapularis repair. A 30° arthroscope is used to initially locate the coracoid tip. In non-retracted tears the coracoid tip is usually just anterior to the upper subscapularis tendon and can be palpated with a shaver inserted through the ASL portal. Using the 30° arthroscope in the initial steps helps to maintain proper orientation so as to avoid inadvertent inferior dissection. At the level of the coracoid tip, a shaver or electrocautery is used to make a window in the rotator interval just superior to the subscapularis tendon (Fig 4). Care is taken to preserve the comma tissue laterally and the conjoined tendon inserting on the coracoid. Once the coracoid tip is identified, the arthroscope is pushed through the window and the posterolateral aspect of the coracoid undergoes skeletonization (Fig 5). It is helpful at this point to view with a 70° arthroscope. In addition, by withdrawing the cannula in the ASL portal slightly, instruments in this portal can be redirected to work anterior to the subscapularis.
Fig 4.
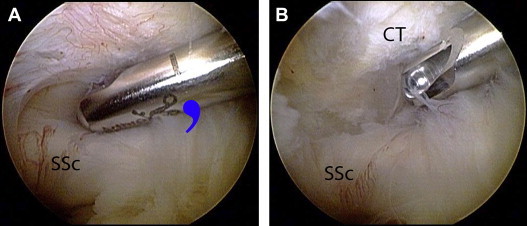
Right shoulder viewed from posterior viewing portal. (A) A shaver is used to make a window in the rotator interval medial to the comma tissue (blue comma). (B) The coracoid tip is located by palpation with the shaver. (CT, coracoid tip; SSc, subscapularis tendon.) (Reprinted with permission.20)
Fig 5.
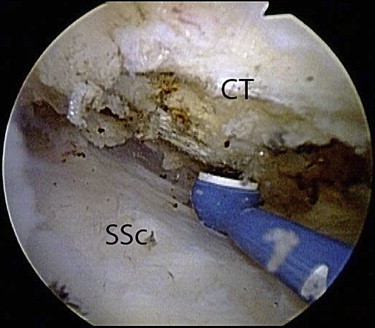
A right shoulder viewed from a posterior viewing portal with a 70° arthroscope showing skeletonization of the coracoid tip with an electrocautery device. (CT, coracoid tip; SSc, subscapularis tendon.) (Reprinted with permission.20)
Retracted tears often require a traction stitch in the subscapularis tendon to create the window in the rotator interval and access the subcoracoid space. Again, starting with a 30° arthroscope, the comma sign is used to identify the superolateral corner of the subscapularis. A traction suture is placed in the superolateral tendon medial to the comma tissue by use of an antegrade suture passer (FastPass Scorpion; Arthrex). To maintain freedom in the ASL working portal, it is helpful to briefly remove the cannula and replace it so that the traction suture remains in the ASL portal but outside of the cannula. While one is pulling laterally on the traction suture, the coracoid is then identified and a window is created in the rotator interval as described previously.
Three-Sided Subscapularis Tendon Release
Retracted tears of the subscapularis require a 3-sided release. Skeletonization of the posterolateral coracoid constitutes the anterior release. Next, a superior release is performed between the coracoid neck and the tendon with a 30° arthroscopic elevator. The elevator is inserted only to the base of its blade, which is enough to release the adhesions to the coracoid; it is not necessary and is potentially detrimental to dissect any further medially than that because of the risk of neurovascular damage. The posterior release of the subscapularis tendon is performed by introducing a 15° elevator between the posterior subscapularis tendon and the anterior glenoid neck. This is a safe, relatively avascular plane in which the elevator can safely be manipulated blindly to perform the posterior release. This completes the 3-sided release (anterior, superior, and posterior). After the 3-sided release, we have found that we can always mobilize the subscapularis to the lesser tuberosity or, at the very worst, to within 5 mm of the lesser tuberosity.
Coracoplasty
Before performing repair of the subscapularis, we always assess the coracohumeral interval. If the distance between the coracoid and the anterior subscapularis tendon is less than 7 mm (approximately 1.5 diameters of the barrel-shaped bur), then a coracoplasty is performed through the ASL portal to create a subcoracoid space that is at least 7 mm.
Bone Bed Preparation
Next, the lesser tuberosity bone bed is prepared through the ASL portal with light use of a bur to create a bleeding base. Ring curettes are useful to create a sharp medial margin. For retracted tears, footprint restoration of the subscapularis tendon depends on defining the medial and lateral margins of the lesser tuberosity. The normal medial margin is 2 to 3 mm lateral to the articular surface. The lateral margin can be less obvious to delineate but can be determined by identifying the bicipital groove, which marks the lateral border of the lesser tuberosity. Even though there is usually a 2- to 3-mm gap between the articular cartilage and the anatomic footprint of the subscapularis, we prepare the lesser tuberosity footprint all the way to the articular margin. In cases in which mobilization does not create enough lateral excursion for an arthroscopic repair of the subscapularis, we perform medialization of the footprint by 5 to 7 mm and have observed no decrease in functional outcome with this medialized position.14
Repair of Subscapularis Tendon
PASTA Lesions
Our preferred technique for repair of PASTA lesions is a knotless technique (SpeedFix; Arthrex).15 A FiberTape (Arthrex) is passed antegrade through the superolateral subscapularis through the ASL portal. An anterior portal is then established for anchor placement by use of an 18-gauge spinal needle with an outside-in technique. This is a percutaneous stab portal only that begins somewhat more medial than a standard anterior portal; in determining placement, the surgeon should pass the needle just lateral to the coracoid tip, but medial to the comma tissue, and approach the lesser tuberosity at a 30° to 45° angle. Both FiberTape limbs are retrieved out of the anterior portal. A punch is then placed through the anterior portal to create a bone socket for anchor insertion. The punch is not removed at this point. The free ends of the FiberTape are threaded through the eyelet of a 4.75-mm BioComposite SwiveLock C anchor (Arthrex). The punch is then removed, and the SwiveLock anchor is immediately placed. The eyelet of the anchor is docked in the bone socket, suture slack is removed, and the anchor is seated flush with the cortical bone. The FiberTape limbs are then cut flush at the anchor surface, completing the repair (Fig 6).
Fig 6.
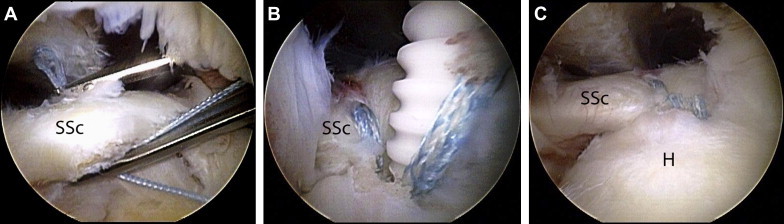
A right shoulder viewed from a posterior viewing portal showing knotless repair of an upper subscapularis tendon tear. (A) A FiberTape suture is passed antegrade through the upper subscapularis tendon. (B) The tape is secured to the prepared bone bed with a BioComposite SwiveLock C anchor. (C) The final view shows restoration of the footprint with a low-profile knotless repair. (H, humerus; SSc, subscapularis tendon.) (Reprinted with permission.15)
Full-Thickness Tears
Full-thickness tears can be repaired with a variety of techniques. If the subscapularis is minimally retracted or not retracted, a double-row repair is sometimes possible, although we have found this to be possible in fewer than 25% of cases. For short full-thickness tears of the upper subscapularis, we use a knotless double-row technique with a FiberTape and 2 BioComposite SwiveLock C anchors. A FiberTape and medial anchor are placed as described for PASTA lesions. However, rather than cutting the residual limbs of the FiberTape, these limbs are passed anterior to the comma-sign tissue and fixed superolaterally with a second SwiveLock C anchor. Alternatively, the biceps tenodesis interference screw can be used to simultaneously secure the limbs laterally and accomplish a biceps tenodesis.16 This technique is useful when there is a tight space (i.e., no associated supraspinatus tear) or in a small patient in whom it may not be possible to place both a superolateral anchor and an interference screw. However, tensioning the lateral suture limbs is more difficult with the technique.
If the full-thickness tear involves more than the upper 1.5 cm of the subscapularis (from superior to inferior), a double-row repair requires 2 medial and 2 lateral anchors to adequately re-establish the footprint. We most commonly use a SutureBridge technique (Arthrex). A double-loaded inferomedial anchor (5.5-mm BioComposite Corkscrew FT; Arthrex) is first placed adjacent to the articular margin in a percutaneous fashion through an anterior portal. This portal is as described for PASTA lesions with the exception that it begins more inferiorly. The suture limbs are then passed as mattress stitches through the subscapularis tendon; most commonly, an antegrade suture passer is used through the ASL portal, but a retrograde instrument may also be used through the anterior portal. The FastPass Scorpion (Arthrex) is particularly useful for antegrade passage because its spring-loaded trapdoor in the upper jaw allows for “blind” capture of the suture, even with limited visualization in the subcoracoid space. These suture limbs are retrieved out of the same portal used for anchor placement. The second medial anchor is then placed superomedially, and these suture limbs are passed antegrade through the superolateral subscapularis tendon (medial to the comma tissue) as simple stitches. By placing the sutures there, the tendon edge inverts against the bone bed and the comma tissue acts as a rip-stop to suture cutout through soft tissue (because the fibers of the comma tissue are oriented at right angles to the fibers of the subscapularis tendon). The suture limbs are then tied sequentially from inferior to superior with a Surgeon's Sixth Finger Knot Pusher (Arthrex). At least 4 suture limbs are preserved, criss-crossed, and secured laterally with 2 SwiveLock C anchors. Importantly, the superior suture limbs are passed anterior to the comma tissue when they are incorporated in the lateral row. If the tear is not retracted, the inferior anchor may be placed in a transtendon manner, in which case we then place the superior-medial anchor and use a FiberLink (Arthrex) to pass the superior sutures. This is followed by a double-pulley technique to create a double-mattress stitch between the 2 medial anchors.
In the vast majority of chronic full-thickness subscapularis tears, however, footprint coverage is only adequate for a single-row repair. The steps are the same as just described, with the exception that the suture limbs are all cut and no lateral row is used (Fig 7).
Fig 7.
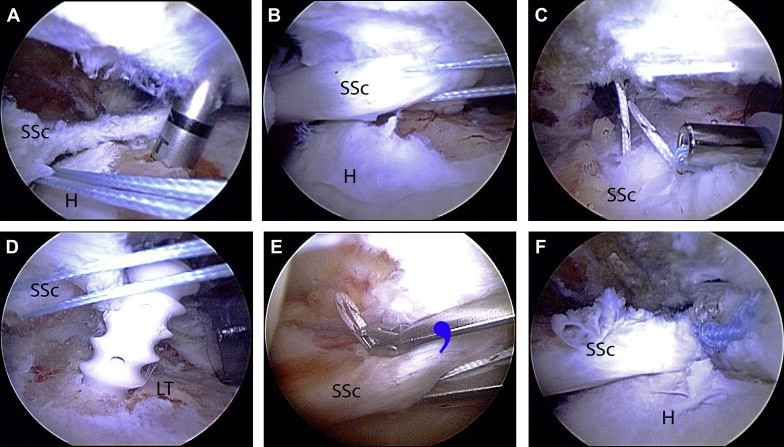
Two-anchor repair of a retracted full-thickness subscapularis tendon tear in a right shoulder viewed from a posterior glenohumeral portal. (A) A bone socket is created in the inferior lesser tuberosity for placement of a BioComposite Corkscrew FT suture anchor. (B) After suture passage, a provisional reduction is obtained with a traction stitch in the upper subscapularis tendon. (C) The arthroscope is placed through a window in the rotator interval, and the sutures from the inferior anchor are tied while tension is maintained on the traction stitch. (D) A second anchor is then placed in the superior lesser tuberosity. (E) Sutures from the superior anchor are passed antegrade, medial to the comma tissue (blue comma). (F) Completed repair, showing restoration of subscapularis footprint. (H, humerus; LT, lesser tuberosity; SSc, subscapularis tendon.) (Reprinted with permission.20)
Biceps Tenodesis and Subsequent Rotator Cuff Repair
After the subscapularis has been repaired, the biceps tenodesis is performed at the top of the bicipital groove with a BioComposite Tenodesis screw. Then the comma sign can be followed to the anterolateral border of the supraspinatus tendon, which can be mobilized and repaired.
Discussion
Arthroscopy has dramatically improved the ability to recognize and repair subscapularis tendon tears. In our opinion recognition and repair of these tears are critical to achieving the best outcome possible for both isolated subscapularis tears and combined rotator cuff tears involving the subscapularis. With the principles and techniques described in this article, repair of the subscapularis tendon has led to good or excellent functional outcomes at both short- and long-term in the vast majority of cases.17-19
Footnotes
The authors report the following potential conflict of interest or source of funding: Arthrex.
Supplementary Data
Repair of upper subscapularis by SpeedFix technique.
Repair of complete subscapularis tear: part 1.
Repair of complete subscapularis tear: part 2.
References
- 1.Arai R., Sugaya H., Mochizuki T., Nimura A., Moriishi J., Akita K. Subscapularis tendon tear: An anatomic and clinical investigation. Arthroscopy. 2008;24:997–1004. doi: 10.1016/j.arthro.2008.04.076. [DOI] [PubMed] [Google Scholar]
- 2.Bennett W.F. Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of “hidden” rotator interval lesions. Arthroscopy. 2001;17:173–180. doi: 10.1053/jars.2001.21239. [DOI] [PubMed] [Google Scholar]
- 3.Lafosse L., Jost B., Reiland Y., Audebert S., Toussaint B., Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89:1184–1193. doi: 10.2106/JBJS.F.00007. [DOI] [PubMed] [Google Scholar]
- 4.Barth J.R., Burkhart S.S., De Beer J.F. The bear-hug test: A new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;22:1076–1084. doi: 10.1016/j.arthro.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Keating J.F., Waterworth P., Shaw-Dunn J., Crossan J. The relative strengths of the rotator cuff muscles. A cadaver study. J Bone Joint Surg Br. 1993;75:137–140. doi: 10.1302/0301-620X.75B1.8421011. [DOI] [PubMed] [Google Scholar]
- 6.Kuechle D.K., Newman S.R., Itoi E., Morrey B.F., An K.N. Shoulder muscle moment arms during horizontal flexion and elevation. J Shoulder Elbow Surg. 1997;6:429–439. doi: 10.1016/s1058-2746(97)70049-1. [DOI] [PubMed] [Google Scholar]
- 7.Kelly B.T., Williams R.J., Cordasco F.A. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J Shoulder Elbow Surg. 2005;14:165–171. doi: 10.1016/j.jse.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: An anatomic description of the shoulder's “suspension bridge.”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 9.Richards D.P., Burkhart S.S., Tehrany A.M., Wirth M.A. The subscapularis footprint: An anatomic description of its insertion site. Arthroscopy. 2007;23:251–254. doi: 10.1016/j.arthro.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 10.Ticker J.B., Burkhart S.S. Why repair the subscapularis? A logical rationale. Arthroscopy. 2011;27:1123–1128. doi: 10.1016/j.arthro.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Lo I.K., Burkhart S.S. The comma sign: An arthroscopic guide to the torn subscapularis tendon. Arthroscopy. 2003;19:334–337. doi: 10.1053/jars.2003.50080. [DOI] [PubMed] [Google Scholar]
- 12.Koo S.S., Burkhart S.S. Subscapularis tendon tears: Identifying mid to distal footprint disruptions. Arthroscopy. 2010;26:1130–1134. doi: 10.1016/j.arthro.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 13.Lo I.K., Burkhart S.S. Arthroscopic biceps tenodesis using a bioabsorbable interference screw. Arthroscopy. 2004;20:85–95. doi: 10.1016/j.arthro.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 14.Denard P.J., Burkhart S.S. Medialization of the subscapularis footprint does not affect functional outcome of arthroscopic repair. Arthroscopy. 2012;28:1608–1614. doi: 10.1016/j.arthro.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 15.Denard P.J., Burkhart S.S. A new method for knotless fixation of an upper subscapularis tear. Arthroscopy. 2011;27:861–866. doi: 10.1016/j.arthro.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Denard P.J., Ladermann A., Burkhart S.S. Double-row fixation of upper subscapularis tears with a single suture anchor. Arthroscopy. 2011;27:1142–1149. doi: 10.1016/j.arthro.2011.02.033. [DOI] [PubMed] [Google Scholar]
- 17.Burkhart S.S., Tehrany A.M. Arthroscopic subscapularis tendon repair: Technique and preliminary results. Arthroscopy. 2002;18:454–463. doi: 10.1053/jars.2002.30648. [DOI] [PubMed] [Google Scholar]
- 18.Adams C.R., Schoolfield J.D., Burkhart S.S. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24:1381–1389. doi: 10.1016/j.arthro.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Denard P.J., Jiwani A.Z., Ladermann A., Burkhart S.S. Long-term outcome of a consecutive series of subscapularis tendon tears repaired arthroscopically. Arthroscopy. 2012;28:1587–1591. doi: 10.1016/j.arthro.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 20.Burkhart SS, Lo IK, Brady PC, Denard PJ. The cowboy's companion: A trail guide for the arthroscopic shoulder surgeon. Philadelphia: Lippincott Williams & Wilkins, 2012).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Repair of upper subscapularis by SpeedFix technique.
Repair of complete subscapularis tear: part 1.
Repair of complete subscapularis tear: part 2.


