Abstract
Surgical reconstruction of the posterior cruciate ligament (PCL) is technically demanding. Potential challenges include visualization of the tibial footprint and drilling of the tibial tunnel without damaging posterior neurovascular structures, as well as graft selection, deployment, tensioning, and fixation. We present a novel TransMedial all-inside arthroscopic technique (technique designed by A. J. Wilson with support from Arthrex) using a single hamstring tendon graft, fixed with adjustable cortical suspensory devices. The technique simplifies the difficult steps encountered during PCL reconstruction and is safe and reproducible. All arthroscopic viewing is accomplished from the lateral portal, and femoral socket preparation is performed from the medial side with specially contoured instruments, which allow accurate marking, measuring, and anatomic positioning of the graft. The quadrupled semitendinosus graft can be augmented with composite polymer tape for increased strength and initial stability. We use outside-in drilling to create retrograde femoral and tibial sockets. Cortical suspensory fixation on the tibial side can be supplemented with anchor fixation. We use an arthroscopic tibial inlay technique that better approximates native knee anatomy. This also avoids the “killer turn,” a problem seen in transtibial PCL reconstruction techniques, which theoretically induces graft laxity due to abrasion with cyclic loading. This technique can be further adapted to allow a modified double-bundle or TriLink graft (technique designed by A. J. Wilson with support from Arthrex.).
Posterior cruciate ligament (PCL) injuries are uncommon and usually occur in the context of combined ligamentous knee injury. Isolated PCL tears account for approximately 3% of acute knee injuries. Although isolated PCL deficiency has traditionally been treated nonoperatively with reasonable outcomes, a significant proportion of patients have a deterioration in knee function and premature development of medial and patellofemoral compartment osteoarthritis due to abnormally high contact forces.1
The evolution of surgical arthroscopic techniques and instrumentation, combined with an improved understanding of PCL anatomy and biomechanics, has led to an increased impetus for posterior cruciate ligament reconstruction (PCLR). However, the optimal technique for PCLR has not yet been established, with almost every aspect of the surgical procedure and postoperative rehabilitation remaining controversial. Operative challenges include visualization of the tibial footprint and drilling of the tibial tunnel without damaging posterior neurovascular structures. The choice, configuration, deployment, tensioning, and fixation of the graft are also contentious. The TransMedial all-inside technique (technique designed by A. J. Wilson with support from Arthrex) simplifies many of these technically challenging steps. Using specially contoured instruments and lessons learned from the translateral all-inside anterior cruciate ligament (ACL) reconstruction technique previously published by our group,2 the senior author has devised this safe and reproducible technique for PCLR. To our knowledge, it is the only arthroscopic all-inside tibial inlay technique that uses a single hamstring tendon and suspensory cortical fixation on both the tibial and femoral sides of the graft.
Technical Note
Instruments
A specific set of instruments is required for visualizing the PCL footprint, socket preparation, graft preparation, tensioning, and fixation (Video 1). We use both a standard 30° arthroscope and a 70° arthroscope to facilitate visualization of the posterior tibial footprint of the PCL and a curved calibrated radiofrequency (RF) device (Coolcut CaliBlator; Arthrex, Naples, FL) (Fig 1A) to aid soft-tissue clearance in the footprint and define graft positioning. The RF device is preferred to a shaver because it allows better preservation of the bony anatomic landmarks of the footprint. Furthermore, it is contoured so that while the probe tip is being used to debride the tibial footprint, the arm is in an optimal position to retract the posterior capsule, thus protecting the posterior neurovascular structures. The arm of the RF device is calibrated to facilitate direct measurement of the intended retro-socket position, which can be marked with the probe tip in the footprint before drilling (Figs 1B and 1C).
Fig 1.
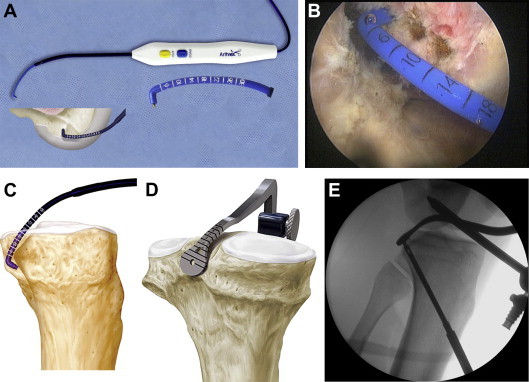
Instruments used in TransMedial PCLR socket preparation. (A) Curved calibrated RF device (Coolcut CaliBlator) used to clear the PCL footprint and to measure and mark the socket position. (B) AL portal view of the RF probe tip used in marking the femoral socket position in a right knee. (C) RF probe tip used to clear the tibial footprint of a left knee as the RF arm retracts the posterior capsule. (D) Tibial aiming guide, positioned over the marked retro-socket position within the tibial footprint of the left knee. (E) Intraoperative fluoroscopic (lateral view) confirmation of guide pin placement in the tibial footprint of a left knee.
As previously described for “all-inside” ACL reconstruction,3 we use a combined guide pin and retrograde drill (second-generation FlipCutter; Arthrex) to create bone-preserving femoral and tibial sockets. Anatomically contoured instruments from the PCL RetroConstruction Drill Guide Set (Arthrex) are used for socket preparation. These instruments include a Tibial PCL Marking Hook (Fig 1D) and Femoral PCL Marking Hook (Arthrex) for the RetroConstruction Drill Guide. The RetroConstruction Drill Guide Handle is rigid so when it is used with the tibial marking hook, the hook arm can be used to firmly and reliably push the posterior capsule away while introducing the guide pin and retrograde drill (Fig 1E). This optimizes safety in drilling the tibial socket by improving the view through retraction and shielding of the posterior neurovascular structures.
Our technique for arthroscopic tibial inlay is a modification of that described by Campbell et al.,4 using a composite autograft. Unlike the graft used by that group, our graft is composed entirely of soft tissue (semitendinosus tendon) secured with cortical suspensory fixation devices on both the tibial and femoral sites (GraftLink; Arthrex). We use a no-button TightRope (TR) ABS Implant and Button (Arthrex) on the tibial side and a reverse-tension ACL TR (Arthrex) on the femoral side. The latter has a smaller button already incorporated into the implant.
In cases in which the diameter of the semitendinosus graft is insufficient, the construct can be augmented with a high-strength composite polymer tape (FiberTape; Arthrex) for increased strength and initial stability. In this circumstance, cortical suspensory fixation can be supplemented by a knotless anchor fixation (SwiveLock; Arthrex) into the anterior tibial cortex (Fig 2).
Fig 2.

Composite polymer tape of a reinforced Arthrex GraftLink is anchored in the anterior tibial cortex, providing supplementary fixation in a right knee.
The key surgical steps are listed in Table 1.
Table 1.
Key Steps in TransMedial PCLR
|
Patient Positioning
The patient is positioned supine on a radiolucent table with the operative knee flexed to 90°, supported with a padded side support and footrest. A high thigh tourniquet is inflated throughout.
Arthroscopy Portals
A high anterolateral (AL) portal is first created adjacent to the patellar tendon. A low anteromedial (AM) portal, also adjacent to the patellar tendon, is then established under direct vision, in line with the ACL and just above the intermeniscal ligament, to facilitate access to the tibial PCL footprint. A standard posteromedial (PM) portal is created under direct vision by use of the 70° arthroscope through the AL portal.
Graft Harvest and Preparation
The semitendinosus is harvested with a tendon stripper through a 2- to 3-cm oblique incision over the pes anserinus (Video 1). This typically provides 27 to 29 cm of graft that is then quadrupled in the standard fashion to form a GraftLink construct (Fig 3A), as previously described for all-inside ACL surgery.3 The graft is typically 8.5 mm in diameter and 70 mm in length. If the GraftLink is of small diameter or there are concerns about graft strength and initial stability, a loop of high-strength composite polymer tape (FiberTape) is incorporated into the construct (Fig 3B).
Fig 3.
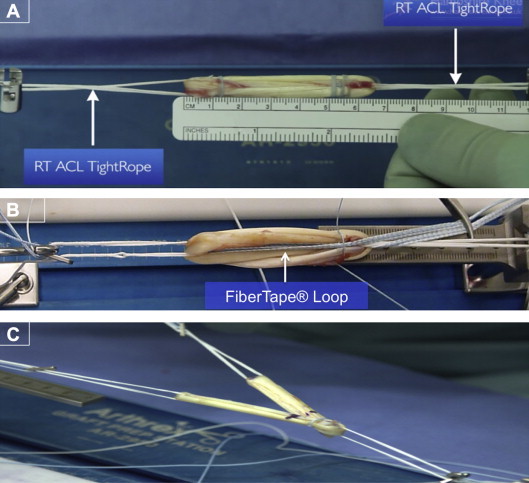
Hamstring grafts used in transmedial PCLR: (A) GraftLink, (B) GraftLink reinforced with FiberTape, and (C) TriLink.
When there is a concomitant posterolateral corner injury or a suspicion of rotational instability in addition to anteroposterior laxity, we reconstruct the PCL using a modified double-bundle technique proposed by the senior author. Like GraftLink, the TriLink construct (technique designed by A. J. Wilson with support from Arthrex) (Fig 3C) is fashioned using only the semitendinosus tendon. It is constructed into a Y-shaped trifurcate graft (with a single tibial, AL femoral, and PM femoral bundle), and a TR is suspended from each limb of the graft.
Each end of the graft is marked at 15 mm. This acts as an arthroscopic visual aid during graft passage and helps ensure that the correct length of graft enters the retro-sockets. We aim to place 15 to 20 mm of graft in the retro-sockets, which leaves 35 to 40 mm of intra-articular graft. This intra-articular distance is similar to the length of the native PCL (32 to 38 mm).4-6
Tibial Socket Preparation
A 70° arthroscope inserted through the PM portal facilitates visualization of the posterior tibia. We use the RF device to clear the tibial footprint (Fig 1C), before measuring and then marking the intended socket position at approximately 40% of the mediolateral distance (typically 7 mm) between the posterodistal aspect of the posterior horn of the medial meniscus and the lateral cartilage margin of the posterior tibial plateau and 2 mm proximal to the “bundle ridge” (the posteroinferior bony ridge separating the AL and PM bundles). These measurements have recently been validated arthroscopically in cadaveric knees.7
The tibial aiming guide (Fig 1D) is inserted through the AM portal and positioned over the marked area in the PCL footprint. The drill guide handle is typically set between 70° and 80° to avoid placing the socket inferior to the “killer turn.” Fluoroscopy is used to confirm placement and to ensure that the guide pin exits perpendicular to the posterior tibial facet when initially used (i.e., in antegrade mode) (Fig 1E). The retrograde drill is sized according to the graft diameter. A large-bore suction shaver is used through the PM portal to facilitate removal of bony debris during the reaming process (Video 1). Socket depth is measured during retrograde drilling from the calibrated shaft markings on the drill pin. We typically drill a 30-mm socket to accept approximately 20 mm of graft. The additional 10 mm accommodates any graft laxity during final tensioning.
After reaming, a stiffened plastic sleeve containing a striped looped suture (TigerStick; Arthrex) is passed through the drill sleeve and into the joint. The suture loop end is retrieved with a suture grasper and pulled through the AM portal (Video 1) for later graft passage.
Tibial socket preparation is the same for both GraftLink and TriLink reconstruction.
Femoral Socket Preparation
For GraftLink (single-bundle reconstruction), we aim to reconstruct the AL bundle because of its favorable biomechanical properties. In the TransMedial technique, we use the medial portals as working portals and the AL portal for viewing the lateral wall of the medial femoral condyle in the intercondylar notch. The wall is prepared by use of the RF device. Arthroscopic bony landmarks, particularly the medial bifurcate prominence, roof of the notch, and cartilage margins, are identified. The RF device is used to measure and then mark the intended socket position (Fig 1B). The center of the AL bundle is identified at a point triangulated among 3 arthroscopic landmarks: proximal to the medial bifurcate prominence, 7 mm posterior to the cartilage margin at the apex of the notch, and approximately 8 mm proximal to the distal articular cartilage margin, in a line parallel to the long axis of the femur.
For TriLink reconstructions, the AL socket is prepared as described earlier and the PM socket is triangulated to a point distal to the medial bifurcate prominence, 11 mm above the posterior cartilage margin and 8 mm proximal to the distal articular cartilage margin, and approximately in a line parallel to the long axis of the femur. These measurements are similar to those recommended by LaPrade and colleagues7 and other authors.5,8,9
The femoral sockets are also created through the AM portal with the retrograde drill. For GraftLink constructs, a 20-mm socket is created in the AL position, and for TriLink, an additional 20-mm socket is created at a different angle to accommodate the PM bundle. The socket diameter is typically 5.5 or 6 mm to match the diameter of the individual bundles. We aim to leave a minimum of 3 mm between the sockets to avoid confluence and improve footprint fill and consequent PCL biomechanics.9
After socket reaming, a stiffened plastic sleeve containing a plain looped suture (FiberStick; Arthrex) is passed down the drill sleeve into the joint and the suture loop retrieved through the AM portal for later graft passage.
Graft Deployment
The looped sutures from the tibial and femoral sockets are collectively retrieved with a suture grasper passed through the AM portal. A single end of each suture is withdrawn, ensuring that there is no soft-tissue entrapment. A snare at the retrieved end of each suture is individually linked to the TR of the GraftLink or TriLink and used as a lead suture to draw the graft into the sockets (Video 1).
Under arthroscopic visualization, 15 mm of the tibial end is pulled into the tibial retro-socket through the AM portal. The adjustable button for the TR ABS is applied to the tensioning sutures and seated onto the anterior tibial cortex for cortical fixation and, later, final tensioning. The femoral ends are then pulled into the joint (PM bundle first for TriLink) and partially seated in the respective retro-socket(s) by advancing the TRs through the guide pin tunnels on their lead sutures (Video 1). The buttons are flipped beyond the femoral cortices. Care is taken to ensure that there is no soft-tissue interposition because this would reduce the quality of graft tensioning and fixation.
Graft Fixation and Tensioning
Our tensioning regimen reflects the differing tension profile of each bundle of the native PCL during knee flexion. We tension the GraftLink construct with the knee in 90° of flexion and concomitant anterior tibial translation. With the button flipped and docked firmly against the medial femoral cortex, the free ends of the femoral tensioning suture of the TR are pulled back and forth to tension the residual length of graft within the retro-socket. The same process is repeated on the tibial side.
It is vital to ensure that the retro-sockets have sufficient depth to accommodate any slack in the graft. Insufficient socket depth will cause the graft to “bottom out,” leaving residual laxity, a difficult problem to correct at this stage of the procedure. Therefore we drill the tibial socket to a depth of 30 mm and the femoral sockets to 20 mm for this purpose. Conversely, pulling too much graft into the sockets by over-tensioning will reduce the intra-articular length of graft and over-constrain the knee.
The knee is cycled several times through full range of movement before the TR button fixation is verified and readjusted at 90° of flexion. Before the tensioning sutures are cut, the posterior drawer test and arthroscopic visualization are used to verify satisfactory fixation and restoration of normal anteroposterior laxity. For reinforced GraftLink constructs, the free ends of the polymer tape loop are then anchored distally in the tibia (Fig 2).
With TriLink constructs, the femoral ends are tensioned in 30° and then 90° of flexion because at these angles, the PM and AL bundles of the native PCL are most taut. We do not tension the PM bundle in full extension because at 30°, the PM bundle is thought to be active whereas the capsular and collateral structures are slack, thereby allowing the PM graft to function independently. After cycling the knee, final tensioning of the tibial and AL bundles is performed at 90° of flexion. Before closure, the wounds and hamstring harvest tract are infiltrated with a large volume of dilute local anesthetic.10
Postoperative Rehabilitation
Our standardized protocol is similar to the recommendations made in a recent review by LaPrade and colleagues.11 Although there are no established guidelines for optimal PCL rehabilitation, it is agreed that proper functioning of the quadriceps musculature is essential to recovery because it aids in dynamic stabilization of the knee. After surgery, a hinged knee brace is worn continuously for 12 weeks. For the first 6 weeks, patients are restricted to partial weight bearing with the brace locked in extension. The focus is on quadriceps activation, passive prone knee flexion from 0° to 90°, and active extension exercises. From 6 to 12 weeks, the patient is allowed to fully bear weight with the brace in situ and range of movement is increased to 0° and 120° of flexion. Patients are restricted from squatting or sudden deceleration for 6 months. At 6 months, patients may begin straight-line jogging if quadriceps and hamstring deficits are less than 20%. Once the patients can run straight ahead at full speed, they are allowed to progress to lateral running, crossovers, and cutting exercises before returning to sport at 9 to 12 months.
Discussion
The TransMedial technique is the first arthroscopic all-inside tibial inlay approach that uses a single hamstring tendon and suspensory cortical fixation on both the tibial and femoral sides of the graft, conferring several potential benefits over traditional approaches. The use of a single semitendinosus autograft eliminates morbidity associated with bone-tendon autografts and the risks of allografts.12 In addition, by preserving the gracilis, the patient does not lose deep knee flexion and internal rotation strength as reported by some authors,13 although a more recent study refutes this.14 Another benefit of preserving the gracilis is that it can be used to reconstruct other ligaments in patients with multiligament injuries.
The anatomy of the native PCL has been well documented in the literature.6,15 According to Hoher et al.,12 the ideal graft for PCLR would replicate an intact native PCL, with a large fan-shaped femoral footprint and comparatively smaller tibial insertion footprint. In addition, harvest-site morbidity should be minimal, with easy graft passage, secure fixation in an anatomic position, and expedient graft incorporation. Although a quadrupled semitendinosus graft is not perfect by this definition, we believe that our graft constructs, particularly the TriLink, approach this description of an ideal PCL graft.
Using GraftLink for single-bundle (AL) PCLR, we use a 28-cm length of tendon to achieve a graft diameter of at least 8.5 mm and an intra-articular length between 35 mm and 40 mm with at least 15 mm of length docked into the retro-sockets. Zantop et al.16 have reported that a 1.5-cm graft-tunnel interface is adequate for satisfactory pullout strength for hamstring tendons used in cruciate ligament reconstruction. Interestingly, Hoher et al.12 suggested that PCL grafts should be longer than those used in ACL reconstruction because the intra-articular distance for a PCL substitute approximates 4 cm. However, our 6.5- to 7-cm GraftLink, which we also use for ACL reconstruction, reproduces the length of the native PCL and replicates the superior biomechanics (ultimate load to failure, stiffness, initial stability) of a 4-stranded hamstring graft.17 In a cadaveric study comparing 3 different graft constructs, a quadrupled tendon graft had the greatest translation during continuous loading when compared with patellar tendon and tendo-Achilles grafts.17 Therefore 1 potential concern with this soft-tissue construct is that the graft will stretch and potentially cause residual PCL laxity. We overcome this risk postoperatively by having the patient wear a brace for 12 weeks to restrict posterior translation of the tibia while tendon-bone integration occurs.
TriLink PCLR is technically more difficult than single-bundle reconstruction, but it re-creates the native PCL anatomy more accurately. Anatomic studies have shown that the tibial attachment of the PCL is substantially more compact than the femoral attachment; therefore a single tibial tunnel and 2 femoral sockets are hypothesized to allow good restoration of the anatomy of the native PCL.7 Biomechanical studies have shown that the key determinant in controlling posterior tibial laxity in anatomic PCLR is the femoral tunnel placement on the medial wall and roof of the intercondylar notch.18 Consequently, a trifurcate graft is the construct of choice for surgeons performing both open19 and arthroscopic tibial inlay9,20 PCLR.
The advantages and disadvantages of double-bundle and single-bundle PCLR are still unclear. Biomechanical studies have shown that the double-bundle technique may have a stability advantage over the single-bundle technique21; however, this has not yet been confirmed in clinical trials.6,22 Like Kohen and Sekiya,22 we believe that double-bundle PCLR is a better option for controlling knee rotational stability in the presence of combined PCL/posterolateral corner instability.
Femoral tunnel positioning in PCLR is unreliable, and despite a wide range of published techniques,18 there remains no consensus on how to determine optimal placement. We use direct measurement from consistently recognizable arthroscopic landmarks to locate the center of the sockets in the footprint. This method devised by the senior author appears to be reliable and reproducible but has not yet been validated for PCLR. A recent cadaveric study has provided quantitative measurements of tunnel positions from arthroscopic landmarks that can be used for a direct measurement technique,7 although in contrast to ACL reconstruction,23 no in vivo studies are available.
The optimal method for graft deployment and fixation in PCLR remains controversial. The superiority of transtibial, open inlay, and arthroscopic inlay techniques has not yet been established in clinical studies.24,25 Laboratory testing suggests that transtibial and inlay techniques (arthroscopic or open) have similar stability at the time of initial fixation but that inlay techniques protect graft integrity and prevent graft attenuation with cyclic loading around the killer turn.6 The arthroscopic inlay technique does minimize the potential morbidity and the neurovascular risks associated with posterior capsulotomy used in the open tibial inlay technique. Drawbacks, however, include the need for removal of residual PCL tissue in the footprint to identify bony landmarks, which may be beneficial to ligament healing and postoperative rehabilitation.26 Another possible limitation is the potential for over-constraint of the knee when tensioning the graft.
The goal of graft fixation is to provide support to the graft-bone interface until biologic incorporation is complete. Sharpey-like fibers form within 4 weeks postoperatively and typically mature by 8 to 12 weeks. Their size and number correlate positively with graft pullout strength and are influenced by several variables including fixation type. Although composite tendon-bone grafts provide theoretical advantages of superior fixation strength and shorter graft incorporation periods when compared with our technique, recent studies have shown comparable stability using arthroscopic techniques with suture fixation when compared with the traditional open inlay techniques with bone block tibial ends.25,27 Furthermore, biomechanical testing of GraftLink versus interference screws in porcine knees showed an ultimate load of 1,012 ±102 N, cyclic displacement of 2.5 ± 0.8 mm, and a common mode of failure at the suture-tendon junction.28,29 These results were all superior to those for interference screws and are within the limits expected for PCL graft constructs,17 though still not as strong as the native PCL.17
Additional pullout strength can be achieved by adding a supplementary fixation device to the graft.30,31 With cyclic loading, the maximum load to failure and stiffness of such hybrid soft-tissue fixations are similar to those of bone plug fixation.32
The indications, advantages, and limitations are highlighted in Table 2.
Table 2.
Indications, Contraindications, Advantages, and Limitations of TransMedial All-Inside PCLR
| Indications |
| • Acute isolated complete rupture of PCL in athletic patients |
| • Acute complete PCL rupture in a multiple ligament–injured knee |
| • Symptomatic chronic PCL deficiency or chronic grade II PCL laxity that has been unresponsive to conservative management |
| Contraindications |
| • Grade I PCL laxity |
| • PCL insertion-site avulsion injuries |
| Advantages |
| • Single semitendinosus hamstring graft |
| • Gracilis preserved as secondary stabilizer or for use as further graft |
| • Graft versatility: single-bundle, double-bundle, and graft reinforcement options are available by use of same technique |
| • Graft reinforcement provides initial stability by preventing stretching and graft laxity during healing phase |
| • Anatomically contoured instruments that protect posterior neurovascular structures |
| • Direct measurement methods used for anatomic placement of sockets |
| • Bone-preserving retro-sockets instead of full-length intraosseous tunnels |
| • Cortical suspensory fixation with adjustable tensioning used at both tibial and femoral sites |
| • Supplementary tibial fixation with knotless anchor ensures initial stability during healing |
| • Arthroscopic tibial inlay technique, avoiding killer turn of transtibial PCLR and avoiding morbidity of open tibial inlay PCLR |
| Pitfalls and risks |
| • Inadequate graft length |
| ○ Care must be taken to identify and harvest only the semitendinosus; if length is inadequate (<28 cm), a quadrupled semitendinosus and gracilis tendon can be used to create a mega-GraftLink |
| • Longer graft preparation time (as compared with time taken for traditional whipstitching) |
| • Suture entanglement during graft passage |
| ○ When pulling the suture loops through the AL portal, they may become entangled; to avoid this, snares are formed at the single end of each lead suture so that they cannot become intertwined; the snares are used to lasso the graft into the knee joint and then into the sockets |
| • Graft bottoming out before final tensioning |
| ○ Retro-sockets must have sufficient depth (10 mm greater than expected intra-socket graft length) to accommodate any slack in the graft; insufficient socket depth will cause the graft to bottom out, leaving residual intra-articular graft laxity |
| • Over-constraining knee |
| ○ Pulling too much graft into the sockets by over-tensioning will reduce the intra-articular length of graft and over-constrain the knee |
Conclusions
The TransMedial technique is a safe, reproducible, and versatile approach that simplifies many of challenging aspects associated with PCLR. Thus far, we have only performed 5 cases and only have short-term radiographic (Fig 4) and clinical outcome results (mean, 6 months). Work is ongoing to define the biomechanical and longer-term clinical efficacy of the technique.
Fig 4.
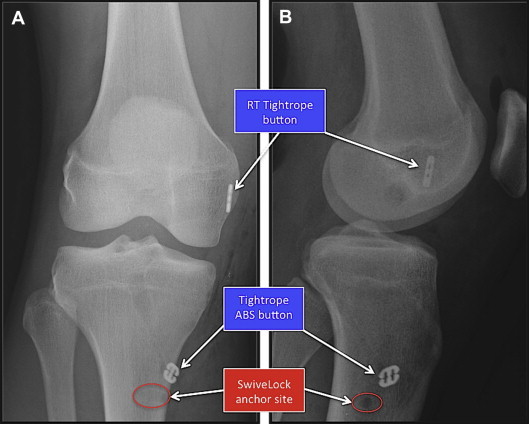
Postoperative radiographic appearance after right PCLR with a reinforced GraftLink construct: (A) anteroposterior view and (B) lateral view.
Acknowledgment
We acknowledge Arthrex for supplying materials, facilities, and expertise in developing the described technique.
Footnotes
The authors report the following potential conflict of interest or source of funding: A.J.W. is a consultant for Arthrex.
Supplementary Data
Overview and arthroscopic footage of transmedial PCLR technique.
References
- 1.Fanelli G.C., Beck J.D., Edson C.J. Current concepts review: The posterior cruciate ligament. J Knee Surg. 2010;23:61–72. doi: 10.1055/s-0030-1267466. [DOI] [PubMed] [Google Scholar]
- 2.Logan J.S., Elliot R.R., Wilson A.J. Translateral ACL reconstruction: A technique for anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1289–1292. doi: 10.1007/s00167-011-1745-0. [DOI] [PubMed] [Google Scholar]
- 3.Lubowitz J.H., Ahmad C.S., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Campbell R.B., Jordan S.S., Sekiya J.K. Arthroscopic tibial inlay for posterior cruciate ligament reconstruction. Arthroscopy. 2007;23:1356.e1–1356.e4. doi: 10.1016/j.arthro.2007.01.020. www.arthroscopyjournal.org Available at: [DOI] [PubMed] [Google Scholar]
- 5.Edwards A., Bull A.M., Amis A.A. The attachments of the fiber bundles of the posterior cruciate ligament: An anatomic study. Arthroscopy. 2007;23:284–290. doi: 10.1016/j.arthro.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Voos J.E., Mauro C.S., Wente T., Warren R.F., Wickiewicz T.L. Posterior cruciate ligament: Anatomy, biomechanics, and outcomes. Am J Sports Med. 2012;40:222–231. doi: 10.1177/0363546511416316. [DOI] [PubMed] [Google Scholar]
- 7.Anderson C.J., Ziegler C.G., Wijdicks C.A., Engebretsen L., LaPrade R.F. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94:1936–1945. doi: 10.2106/JBJS.K.01710. [DOI] [PubMed] [Google Scholar]
- 8.Lopes O.V.J., Ferretti M., Shen W., Ekdahl M., Smolinski P., Fu F.H. Topography of the femoral attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 2008;90:249–255. doi: 10.2106/JBJS.G.00448. [DOI] [PubMed] [Google Scholar]
- 9.Markolf K.L., Jackson S.R., McAllister D.R. Single- versus double-bundle posterior cruciate ligament reconstruction: Effects of femoral tunnel separation. Am J Sports Med. 2010;38:1141–1146. doi: 10.1177/0363546509359072. [DOI] [PubMed] [Google Scholar]
- 10.Logan J.S., Elliot R.R., Wilson A.J. A new technique for hamstring donor site blockade in anterior cruciate ligament reconstruction. Ann R Coll Surg Engl. 2011;93:326. doi: 10.1308/003588411X570909h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pierce C.M., O’Brien L., Griffin L.W., Laprade R.F. Posterior cruciate ligament tears: Functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013;21:1071–1084. doi: 10.1007/s00167-012-1970-1. [DOI] [PubMed] [Google Scholar]
- 12.Hoher J., Scheffler S., Weiler A. Graft choice and graft fixation in PCL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2003;11:297–306. doi: 10.1007/s00167-003-0408-1. [DOI] [PubMed] [Google Scholar]
- 13.Gobbi A. Single versus double hamstring tendon harvest for ACL reconstruction. Sports Med Arthrosc. 2010;18:15–19. doi: 10.1097/JSA.0b013e3181cdb4a6. [DOI] [PubMed] [Google Scholar]
- 14.Barenius B., Webster W.K., McClelland J., Feller J. Hamstring tendon anterior cruciate ligament reconstruction: Does gracilis tendon harvest matter? Int Orthop. 2013;37:207–212. doi: 10.1007/s00264-012-1672-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bowman K.F., Sekiya J.K. Anatomy and biomechanics of the posterior cruciate ligament and other ligaments of the knee. Oper Tech Sports Med. 2009;17:126–134. doi: 10.1097/JSA.0b013e3181f917e2. [DOI] [PubMed] [Google Scholar]
- 16.Zantop T., Ferretti M., Bell K.M., Brucker P.U., Gilbertson L., Fu F.H. Effect of tunnel-graft length on the biomechanics of anterior cruciate ligament-reconstructed knees: Intra-articular study in a goat model. Am J Sports Med. 2008;36:2158–2166. doi: 10.1177/0363546508320572. [DOI] [PubMed] [Google Scholar]
- 17.Chen C.H., Chou S.W., Chen W.J., Shih C.H. Fixation strength of three different graft types used in posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:371–375. doi: 10.1007/s00167-003-0457-5. [DOI] [PubMed] [Google Scholar]
- 18.Apsingi S., Bull A.M.J., Deehan D.J., Amis A.A. Review: Femoral tunnel placement for PCL reconstruction in relation to the PCL fibre bundle attachments. Knee Surg Sports Traumatol Arthrosc. 2009;17:652–659. doi: 10.1007/s00167-009-0747-7. [DOI] [PubMed] [Google Scholar]
- 19.Stannard J.P., Riley R.S., Sheils T.M., McGwin G., Volgas D.A. Anatomic reconstruction of the posterior cruciate ligament after multiligament knee injuries: A combination of the tibial-inlay and two-femoral-tunnel techniques. Am J Sports Med. 2003;31:196–202. doi: 10.1177/03635465030310020701. [DOI] [PubMed] [Google Scholar]
- 20.Slullitel D., Galan H., Ojeda V., Seri M. Double-bundle “all-inside” posterior cruciate ligament reconstruction. Arthrosc Tech. 2012;1:e141–e148. doi: 10.1016/j.eats.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petersen W., Lenschow S., Weimann A., Strobel M.J., Raschke M.J., Zantop T. Importance of femoral tunnel placement in double-bundle posterior cruciate ligament reconstruction: Biomechanical analysis using a robotic/universal force-moment sensor testing system. Am J Sports Med. 2006;34:456–463. doi: 10.1177/0363546505281239. [DOI] [PubMed] [Google Scholar]
- 22.Kohen R.B., Sekiya J.K. Single-bundle versus double-bundle posterior cruciate ligament reconstruction. Arthroscopy. 2009;25:1470–1477. doi: 10.1016/j.arthro.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Bird J.H., Carmont M.R., Dhillon M. Validation of a new technique to determine midbundle femoral tunnel position in anterior cruciate ligament reconstruction using 3-dimensional computed tomography analysis. Arthroscopy. 2011;27:1259–1267. doi: 10.1016/j.arthro.2011.03.077. [DOI] [PubMed] [Google Scholar]
- 24.Papalia R., Osti L., Del Buono A., Denaro V., Maffulli N. Tibial inlay for posterior cruciate ligament reconstruction: A systematic review. Knee. 2010;17:264–269. doi: 10.1016/j.knee.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Zehms C.T., Whiddon D.R., Miller M.D. Comparison of a double bundle arthroscopic inlay and open inlay posterior cruciate ligament reconstruction using clinically relevant tools: A cadaveric study. Arthroscopy. 2008;24:472–480. doi: 10.1016/j.arthro.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 26.Wang C.J., Chan Y.S., Weng L.H. Posterior cruciate ligament reconstruction using hamstring tendon graft with remnant augmentation. Arthroscopy. 2005;21:1401. doi: 10.1016/j.arthro.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 27.Ruberte Thiele R.A., Campbell R.B., Amendola A., Sekiya J.K. Biomechanical comparison of figure-of-8 versus cylindrical tibial inlay constructs for arthroscopic posterior cruciate ligament reconstruction. Arthroscopy. 2010;26:977–983. doi: 10.1016/j.arthro.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 28.GraftLink biomechanical testing—Tibial side. Arthrex (Research and Development); Naples, FL: 2012. [Google Scholar]
- 29.GraftLink with ACL tightrope: Biomechanical testing. Arthrex (Research and Development); Naples, FL: 2011. [Google Scholar]
- 30.Nagarkatti D.G., McKeon B.P., Donahue B.S., Fulkerson J.P. Mechanical evaluation of a soft tissue interference screw in free tendon anterior cruciate ligament graft fixation. Am J Sports Med. 2001;29:67–71. doi: 10.1177/03635465010290011601. [DOI] [PubMed] [Google Scholar]
- 31.Weiler A., Richter M., Schmidmaier G., Kandziora F., Sudkamp N.P. The EndoPearl device increases fixation strength and eliminates construct slippage of hamstring tendon grafts with interference screw fixation. Arthroscopy. 2001;17:353–359. doi: 10.1053/jars.2001.21531. [DOI] [PubMed] [Google Scholar]
- 32.Lim H.C., Bae J.H., Wang J.H. The biomechanical performance of bone block and soft-tissue posterior cruciate ligament graft fixation with interference screw and cross-pin techniques. Arthroscopy. 2009;25:250–256. doi: 10.1016/j.arthro.2008.10.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Overview and arthroscopic footage of transmedial PCLR technique.


