Abstract
Background: Weight reduction without behavioral modification is not sustainable. However, with a technology application such as teledietetics, the recording process could be a cognitive cue for individuals to change their eating behavior. This study tested obese participants to determine whether teledietetics shows better results in weight reduction. Study Design and Methods: We conducted a double-blinded randomized controlled trial. The participants in the food diary (FD) and electronic diary (ED) groups recorded their dietary intakes in logbooks and on an electronic diary system, respectively. The participants in the control group (CG) did nothing. Subjects were adults 20–60 years of age with a body mass index (BMI) of ≥25 kg/m2. The ED and FD groups were the intervention groups and were compared with the CG group. The participants' body weights, BMIs, fat percentages, waist-to-hip ratios (WHRs), and mean arterial pressures (MAPs) were measured before the study, at Week 6, and at Week 12. Demographic data were collected using self-administered questionnaires. A chi-squared test and descriptive statistics were used to describe the demographic and biomeasurement data. Repeated-measures analysis of variance was used to evaluate the effectiveness of the three groups over time. Results: Significant decreases in body weight (F1.705,86.950=20.508, p<0.001) and BMI (F1.657, 84.486=21.256, p<0.001) and insignificant decreases in fat percentage (F2,94=0.547, p=0.581), WHR (F1.785,91.052=2.888, p=0.067), and MAP (F2,94=7.542, p=0.0001) were observed among the three measurement times. Conclusions: Electronic dietary records were better than food diaries in terms of fat percentage reduction in our trials, indicating that teledietetics increases healthy-eating awareness.
Key words: : e-health, home health monitoring, distance learning
Introduction
The challenge of weight reduction has prompted much research to identify effective strategies for weight loss augmentation. Weight loss cannot be sustained without compliance to behavior-modifying interventions such as formula diets, pharmacologic approaches, and calorie restriction.1–4 Therefore, studies must investigate ways to help obese people deal with barriers and improve their adherence to weight reduction programs. Foster et al.5 concluded that a healthy lifestyle requires significant planning, proficiency in making healthy food choices, effective estimation of portion sizes, and maintenance of exercise regimens. All of these attributes require a great deal of time if the person lacks the appropriate skills. However, once acquired, these skills provide structure and require less decision-making time. Foster et al.5 claimed that the “skill power” (rather than the willpower) required to attain weight loss success and desired behavior cannot be established immediately, but requires education and frequent practice. This process involves cognitive therapy and behavioral treatments. The former incorporates the principles that thoughts affect feelings and behavior directly and that uncontrolled eating is the result of negative feelings such as failure, frustration, and loneliness.6 Taking a different approach, behavioral treatment specifies how to change an individual's eating behavior. It is goal and process directed7 and promotes small rather than large eating modifications. Incremental steps are taken to achieve more distant goals, and goal setting, problem solving, and motivation are the tools that facilitate the changes. Interventions for weight reduction have been shown to have greater effects over both the short and long terms in behavioral treatment.8,9 For example, the LEARN Program for Weight Management 2000 includes self-monitoring, stimulus control, and cognitive therapy as components in its behavioral package.10
A food diary is a self-monitoring method used to record daily diets for a dietician's review. In practice, it serves as a food intake activity record. Technology allows food diaries to work interactively.11–14 Food diaries can be programmed with individuals' online input and are designed to include functions such as food nutrient value reports, energy and nutrient problem identifiers, unhealthy food identifiers, and meal plan designs.15,16 They can serve as cognitive tools that provide instant dietary evaluations to the individual.
The concept of teledietetics is new to dieticians and nutritionists. Its role is to facilitate individuals to apply nutritional knowledge to the balanced diet and portion size information acquired from their dietician consultations. By recording their patients' dietary intakes into a programmed system, dieticians can promptly analyze their food energy and nutrients. The program can then use the data to generate instant and individualized evaluations via online reports. These reports can educate individuals on how to modify their diets and gradually change their behavior to encourage healthy eating. Seeing the factual data on food energy and nutrient values establishes a mindfulness effect in the individual to change. The aim of this study was to test the effectiveness of teledietetics as an intervention for weight reduction.
Materials and Methods
Sampling and Samples
Participants were recruited via radio broadcast in Hong Kong and e-mail messages sent to all of the staff and students at a university. Interested participants 20–60 years of age who had a body mass index (BMI) of 25 kg/m2 or above fit the inclusion criteria and were recruited on a first-come-first-served basis. In total, 60 participants were randomly assigned to an electronic diary (ED) group, food diary (FD) group, or control group (CG), with each group comprising 20 participants. The groups differed according to their dietary recording methods.
Study Design
This was a randomized controlled trial. Different research assistants administered the randomization and assignment of participants. The research assistant applied a simple randomization method by assigning each participant a number written on a piece of paper. The papers were folded and collected. The research assistant then drew the first 20 papers to determine the ED group, followed by another 20 papers to determine the FD group; the remaining 20 papers determined the CG.
Instruments
The FD comprised a logbook with tables for participants in this group to input their diets each day. Each participant was asked to keep a detailed record of his or her food consumption during breakfast, morning tea, lunch, afternoon tea, dinner, and nighttime snacks. Subjects were also required to record the time, food items, ingredients, amount of food ingredients consumed, cooking methods used in food preparation, and amounts of oil and sauce added. To estimate the portion sizes, each participant was provided with a picture describing the various standard food and beverage portions.
The eDietary Intake Portal (the Portal) was the electronic dietary recording system used by the ED group. It could be accessed by any Internet browser along with a personal login number and password. The Portal has been found to have good reliability and accuracy in food evaluation (intraclass correlation coefficient=0.916, F=17.001, p<0.001)16 and good usability in terms of system usability and information and interface quality.15 The participants captured food images using their cameras or mobile phones and then uploaded them through the Portal to the central database. The food images were then stored in the database and immediately integrated into the food questionnaires. The participants were asked to fill in their dietary intake information by choosing the food items from the food questionnaires they uploaded and selecting the number of servings consumed for each food item. Nutritionists evaluated the food ingredients, corresponding serving sizes, cooking methods, and sauce amounts added according to the uploaded food images. The Portal was programmed to calculate the total calories and total amount of major nutrients consumed daily. Based on these data and the participants' one-time inputs of body height, body weight, sex, and physical activity level in the past 3 months, the Portal calculated the energy requirements for each participant. Nutrient and dietary evaluation reports were generated instantly. The nutrient reports described the nutrient values of each recorded food item along with the number of servings, and the dietary evaluation reports described whether the daily food intakes met the recommended requirements. The participants could receive their dietary evaluations anywhere at any time using a handheld device along with a Wi-Fi, 3G, or 4G connection. They could adjust their food choices and consumption amounts based on the reports' recommendations.
Outcome Measurements
The participants' body weights, BMIs, fat percentages, waist-to-hip ratios (WHRs), and mean arterial pressures (MAPs) were taken at baseline (before the commencement of the study), midpoint (Week 6) and post-intervention (Week 12).
Each BMI was calculated according to the formula (body weight [in kg]/body height2 [in m2]), and each WHR was calculated as the ratio of the waist circumference horizontal to the belly button (in cm) to the widest hip circumference (in cm). Each fat percentage was measured by an InBody 720 bioelectrical impedance analyzer (Biospace, Seoul, Korea).
Systolic and diastolic blood pressures were measured by a mercury blood pressure monitor. Each MAP (i.e., the average arterial pressure during a single cardiac cycle) was calculated according to the following formula: diastolic pressure+(1/3×[systolic blood pressure – diastolic blood pressure]).
Procedure
This research study was approved by an institutional ethics committee. Three groups were examined, including one control (CG) and two experimental (ED and FD) groups. The study lasted for 12 weeks from September to November 2011. The 60 obese participants were given an information sheet describing the purpose of the study and were informed they would be allocated to either the CG or one of the experimental groups. The participants signed the consent forms before the study commenced. All of the participants were kept anonymous.
The participants' demographic data including age, sex, highest education, occupation, and marital status were collected from self-administered questionnaires. All of the participants received a standard healthy-eating information kit from the Department of Health. A registered nutritionist conducted three diet seminar sessions lasting 60–90 min each. The three seminar sessions covered the topics of what comprises a balanced diet, how to lose body weight by eating healthily and expending energy during exercise, and how to identify weight reduction myths. They were conducted separately by group rather than jointly to prevent the participants from communicating and realizing they were in different groups.
Biomeasurements of the participants' body heights, body weights, fat percentages, blood pressures, and waist and hip circumferences were taken before the study started and at Weeks 6 and 12. These measurements were treated as the baseline, midterm, and post-intervention measurements, respectively. To ensure study blindness, one researcher (Staff A) conducted the subject recruitment and random assignment, another researcher (Staff B) conducted the biomeasurements, and a nutritionist (Staff C) conducted the diet seminars. The author (Staff D) performed the data input and analysis. All of the procedures were separated to ensure the researchers were blind to the participants' experimental groups.
The participants in the FD group were asked to record their dietary intakes in logbooks and submit them to a nutritionist for weekly evaluation. Comments were written in the logbooks and posted back to the participants within 24 h. The participants in the ED group were asked to record their dietary intakes on the Portal. The nutritionists evaluated the food according to the nutrient (carbohydrate, protein, saturated fat, total fat, sugar, calcium, cholesterol, vitamin C) and energy inputs in calories. Their reports were available in the online profiles by food item, and comments were given on whether the participants were meeting the energy and nutrient balance requirements. The latter was determined according to guidelines from the U.S. Department of Health and Human Services and the U.S. Department of Agriculture.
Statistical Analysis
The statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) (version 20; SPSS, Inc., Chicago, IL). The demographic data of the three groups were analyzed using a chi-squared test of the homogeneity of the participants' characteristics in each group. Descriptive statistics were used to describe the distribution of the subjects' demographic and biomeasurement data. Repeated-measures analysis of variance (ANOVA) was performed to evaluate the effectiveness of the ED and FD groups compared with the CG over time. Mauchly's test of sphericity was applied to validate whether a sphericity violation occurred between the independent variables. Post hoc tests with least significant differences (LSDs) were conducted to show the differences in the outcome measurements at the three time points.
Results
The mean (standard deviation) ages in the EG and FD groups and the CG were 36.5 (10.1), 36.9 (11.7), and 38.7 (11.7) years, respectively. The distributions of sex, highest education, occupation, and marital status are given in Table 1. No statistical differences were found in any of the demographic data according to the chi-squared test.
Table 1.
Demographic Characteristics of the Participants
| |
GROUP |
|
||
|---|---|---|---|---|
| CONTROL | FOOD DIARY | ELECTRONIC DIARY | P VALUE | |
| Sex | ||||
| Male |
10 (50.0) |
6 (30.0) |
6 (30.0) |
0.317 |
| Female |
10 (50.0) |
14 (70.0) |
14 (70.0) |
|
| Highest education | ||||
| Secondary school |
5 (25.0) |
6 (30.0) |
6 (30.0) |
0.603 |
| Diploma |
1 (5.0) |
3 (15.0) |
2 (10.0) |
|
| Degree |
5 (25.0) |
4 (20.0) |
8 (40.0) |
|
| Postgraduate degree |
9 (45.0) |
7 (35.0) |
4 (20.0) |
|
| Occupation | ||||
| Professional |
0 (0.0) |
2 (10.0) |
0 (0.0) |
0.262 |
| Academic |
7 (35.0) |
3 (15.0) |
3 (15.0) |
|
| Technical |
1 (5.0) |
2 (10.0) |
2 (10.0) |
|
| Administrative/clerical |
7 (35.0) |
8 (40.0) |
13 (65.0) |
|
| Retired |
0 (0.0) |
1 (5.0) |
0 (0.0) |
|
| Student |
5 (25.0) |
4 (20.0) |
2 (10.0) |
|
| Marital status | ||||
| Single |
10 (50.0) |
11 (55.0) |
11 (55.0) |
0.935 |
| Married | 10 (50.0) | 9 (45.0) | 9 (45.0) | |
Data are number (%).
Sixty subjects were recruited for the weight reduction program, and 20 subjects were assigned to each group. Some participants were not available to have a second measurement at Week 6 or a third measurement at Week 12, making incomplete outcome variables collected for data analysis. In this study, only participants with complete measurements at baseline, Week 6, and Week 12 were included for data analysis, and the corresponding numbers of participants in each group are shown in Table 2, which shows the means and standard deviations of the outcome measurements. Mauchly's test of sphericity was first performed to check if any violation of the assumption of sphericity was found. Results of Mauchly's test were insignificant on fat percentage (p=0.795) and MAP (p=0.965), and this indicated the assumption of sphericity had not been violated. But, results were significant on body weight (p=0.009), BMI (p=0.003), and WHR (p=0.041) that the null hypothesis of the variances in baseline–Week 6, Week 6–Week 12, and baseline–Week 12 were not equal. Therefore, correction was achieved by modifying the degrees of freedom used to determine the critical value of F, so as to minimize bias in having Type I error. In this study, a Greenhouse–Geisser correction was applied for the one-way repeated-measures with multifactor designs.
Table 2.
Results from Repeated-Measures Analysis of Variance
| |
|
MEAN (SD) |
|
||
|---|---|---|---|---|---|
| N | BASELINE | WEEK 6 | WEEK 12 | MAUCHLY'S TEST OF SPHERICITY | |
| Body weight (kg) | |||||
| CG |
19 |
71.7 (14.4) |
75.8 (11.8) |
70.2 (13.7) |
M=0.827 (p=0.009) |
| FD |
16 |
71.4 (9.1) |
70.3 (9.5) |
69.7 (9.6) |
|
| ED |
19 |
70.0 (17.7) |
70.4 (13.5) |
68.4 (17.1) |
|
| Body mass index (kg/m2) | |||||
| CG |
19 |
28.1 (2.3) |
27.9 (2.5) |
28.0 (2.6) |
M=0.793 (p=0.003) |
| FD |
16 |
27.3 (2.6) |
26.9 (2.7) |
26.6 (2.7) |
|
| ED |
19 |
27.8 (4.4) |
27.4 (4.1) |
27.3 (4.2) |
|
| Fat (%) | |||||
| CG |
18 |
32.9 (6.1) |
32.7 (7.3) |
33.9 (7.1) |
M=0.990 (p=0.795) |
| FD |
16 |
31.8 (6.1) |
31.5 (6.3) |
31.5 (6.4) |
|
| ED |
16 |
33.8 (6.7) |
33.7 (6.8) |
33.4 (6.5) |
|
| Waist-to-hip ratio | |||||
| CG |
19 |
0.90 (0.058) |
0.89 (0.059) |
0.89 (0.060) |
M=0.880 (p=0.041) |
| FD |
16 |
0.90 (0.050) |
0.89 (0.057) |
0.88 (0.057) |
|
| ED |
19 |
0.89 (0.066) |
0.87(0.069) |
0.87 (0.066) |
|
| Mean arterial pressure | |||||
| CG |
16 |
101.4 (13.9) |
99.4 (12.8) |
93.5 (10.9) |
M=0.998 (p=0.965) |
| FD |
15 |
95.7 (13.2) |
92.8 (7.2) |
92.1 (8.8) |
|
| ED | 19 | 96.8 (11.6) | 95.8 (10.4) | 93.8 (10.7) | |
CG, control group; ED, electronic diary; FD, food diary; SD, standard deviation.
Body Weight
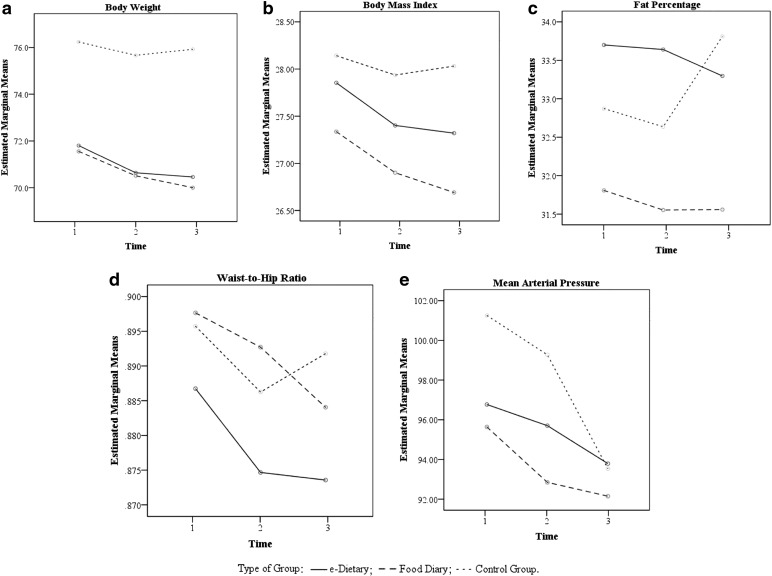
A repeated-measures ANOVA with a Greenhouse–Geisser correction revealed a significant decrease in body weight among the three measurement times: F1.705, 86.950=20.508, p<0.001, with a relatively large effect size (partial η2=0.287). There was no statistically significant difference between the intervention groups and CG over measurement time of body weight: F4,102=1.686, p=0.159 (partial η2=0.062). A post hoc test with LSD comparisons revealed that whereas the means between the baseline and Week 6 measurements (ED versus FD, p=0.008 versus p=0.003) and the baseline and Week 12 measurements (ED versus FD, p=0.003 versus p=0.008) differed significantly, the differences between the Week 6 and Week 12 measurements (ED versus FD, p=1.000 versus p=0.537) were insignificant (Table 3). The CG's body weight values were found to differ insignificantly at each of the time points (Table 3). Figure 1 indicates that although body weight decreased in both the ED and FD groups, the between-group results revealed no significant difference (Table 4). The CG's body weight values decreased slightly at Week 6 and increased at Week 12.
Table 3.
Post Hoc Tests at Three Time Points
| MEAN DIFFERENCES (95% CI) | P VALUE | |
|---|---|---|
| Body weight | ||
| ED | ||
| Baseline versus Week 6 |
1.242 (0.305, 2.179) |
0.008 |
| Week 6 versus Week 12 |
0.189 (−0.395, 0.774) |
1.000 |
| Baseline versus Week 12 |
1.432 (0.476, 2.388) |
0.003 |
| FD | ||
| Baseline versus Week 6 |
1.114 (0.388, 1.839) |
0.003 |
| Week 6 versus Week 12 |
0.544 (−0.495, 1.582) |
0.537 |
| Baseline versus Week 12 |
1.657 (0.424, 2.891) |
0.008 |
| CG | ||
| Baseline versus Week 6 |
0.611 (−0.080, 1.301) |
0.095 |
| Week 6 versus Week 12 |
−0.279 (−1.002, 0.444) |
0.967 |
| Baseline versus Week 12 |
0.332 (−0.0673, 1.336) |
1.000 |
| BMI | ||
| ED | ||
| Baseline versus Week 6 |
0.459 (0.119, 0.800) |
0.007 |
| Week 6 versus Week 12 |
0.083 (−0.146, 0.312) |
1.000 |
| Baseline versus Week 12 |
0.543 (0.172, 0.913) |
0.003 |
| FD | ||
| Baseline versus Week 6 |
0.442 (0.154, 0.730) |
0.003 |
| Week 6 versus Week 12 |
0.214 (−0.174, 0.602) |
0.474 |
| Baseline versus Week 12 |
0.656 (0.180, 1.131) |
0.006 |
| CG | ||
| Baseline versus Week 6 |
0.208 (−0.034, 0.450) |
0.107 |
| Week 6 versus Week 12 |
−0.097 (−0.350, 0.156) |
0.977 |
| Baseline versus Week 12 |
0.111 (−0.252, 0.475) |
1.000 |
| Fat (%) | ||
| ED | ||
| Baseline versus Week 6 |
0.063 (−1.259, 1.384) |
1.000 |
| Week 6 versus Week 12 |
0.362 (−0.916, 1.641) |
1.000 |
| Baseline versus Week 12 |
0.425 (−0.898, 1.748) |
1.000 |
| FD | ||
| Baseline versus Week 6 |
0.269 (−0.959, 1.496) |
1.000 |
| Week 6 versus week 12 |
−0.006 (−1.294, 1.281) |
1.000 |
| Baseline versus Week 12 |
0.262 (−1.085, 1.610) |
1.000 |
| CG | ||
| Baseline versus Week 6 |
0.250 (−1.130, 1.630) |
1.000 |
| Week 6 versus Week 12 |
−1.239 (−2.481, 0.003) |
0.051 |
| Baseline versus Week 12 |
−0.989 (−2.436, 0.458) |
0.262 |
| WHR | ||
| ED | ||
| Baseline versus Week 6 |
0.013 (−0.001, 0.026) |
0.067 |
| Week 6 versus Week 12 |
0.001 (−0.024, 0.027) |
1.000 |
| Baseline versus Week 12 |
0.014 (−0.009, 0.037) |
0.396 |
| FD | ||
| Baseline versus Week 6 |
0.005 (−0.014, 0.025) |
1.000 |
| Week 6 versus Week 12 |
0.009 (−0.012, 0.030) |
0.778 |
| Baseline versus Week 12 |
0.014 (−0.010, 0.038) |
0.401 |
| CG | ||
| Baseline versus Week 6 |
0.010 (0.008, 0.665) |
0.665 |
| Week 6 versus Week 12 |
−0.006 (−0.027, 0.016) |
1.000 |
| Baseline versus Week 12 |
0.004 (−0.022, 0.030) |
1.000 |
| MAP | ||
| ED | ||
| Baseline versus Week 6 |
1.088 (−3.649, 5.825) |
1.000 |
| Week 6 versus Week 12 |
1.947 (−2.368, 6.263) |
0.748 |
| Baseline versus Week 12 |
3.035 (−2.335, 8.405) |
0.459 |
| FD | ||
| Baseline versus Week 6 |
2.844 (−3.241, 8.930) |
0.674 |
| Week 6 versus Week 12 |
0.711 (−3.325, 4.747) |
1.000 |
| Baseline versus Week 12 |
3.556 (−2.485, 9.596) |
0.396 |
| CG | ||
| Baseline versus Week 6 |
2.021 (−4.381, 8.423) |
1.000 |
| Week 6 versus Week 12 |
5.854 (−2.355, 14.064) |
0.222 |
| Baseline versus Week 12 | 7.875 (1.603, 14.147) | 0.012 |
BMI, body mass index; CG, control group; CI, confidence interval; ED, electronic diary; FD, food diary; MAP, mean arterial pressure; WHR, waist-to-hip ratio.
Fig. 1.
Repeated-measures analysis of variance (ANOVA) on body weight, body mass index (BMI), fat percentage, waist-to-hip ratio (WHR), and mean arterial pressure (MAP) among three time points. e-Dietary, electronic diary.
Table 4.
Post Hoc Tests on Electronic Diary, Food Diary, and Control Groups
| MEAN DIFFERENCES (95% CI) | P VALUE | |
|---|---|---|
| Body weight | ||
| Between ED and FD |
0.296 (−7.882, 8.475) |
0.942 |
| Between ED and CG |
−5.304 (−13.124, 8.475) |
0.179 |
| Between FD and CG |
−5.600 (−13.778, 2.578) |
0.175 |
| BMI | ||
| Between ED and FD |
0.558 (−1.6377, 2.7544) |
0.612 |
| Between ED and CG |
−0.520 (−2.6193, 1.5803) |
0.622 |
| Between FD and CG |
−1.0779 (−3.2739, 1.1182) |
0.329 |
| Fat (%) | ||
| Between ED and FD |
2.008 (−2.612, 6.629) |
0.386 |
| Between ED and CG |
0.463 (−4.028, 6.629) |
0.837 |
| Between FD and CG |
−1.546 (−6.036, 2.945) |
0.492 |
| WHR | ||
| Between ED and FD |
−0.014 (−0.0527, 0.0253) |
0.485 |
| Between ED and CG |
0.013 (−0.0238, 0.0507) |
0.472 |
| Between FD and CG |
0.000 (−0.0388, 0.0392) |
0.991 |
| MAP | ||
| Between ED and FD |
1.912 (−5.0714, 8.8960) |
0.584 |
| Between ED and CG |
−2.6502 (−9.5109, 4.2105) |
0.441 |
| Between FD and CG | −4.5625 (−11.8293, 4.2105) | 0.213 |
BMI, body mass index; CG, control group; CI, confidence interval; ED, electronic diary; FD, food diary; MAP, mean arterial pressure; WHR, waist-to-hip ratio.
BMI
A within-subject test with a Greenhouse–Geisser correction indicated a significant decrease in BMI among the three measurement times: F1.657, 84.486=21.256, p<0.001, with a relatively large effect size (partial η2=0.294). There was no statistically significant difference between the intervention groups and CG over measurement time of BMI: F4, 102=1.836, p=0.128 (partial η2=0.067). Table 3 indicates that whereas the BMI value between the baseline and Week 6 measurements (ED versus FD, p=0.007 versus p=0.003) and the baseline and Week 12 measurements (ED versus FD, p=0.003 versus p=0.006) differed significantly, the differences between the Week 6 and Week 12 measurements were insignificant at each of the CG time points. Figure 1 shows that although the BMI values decreased in both the ED and FD groups, the between-group testing results indicated no significant difference (Table 4). The CG's BMI values decreased at Week 6 and increased at Week 12.
Fat Percentage
A within-subjects test indicated an insignificant decrease in fat percentage between the three measurement times (F2,94=0.547, p=0.581), although the effect size was relatively small (partial η2=0.011). There was no statistically significant difference among the intervention groups and CG over measurement time of fat percentage: F4,94=1.748, p=0.146 (partial η2=0.069). Insignificant decreases in fat percentage were found (ED versus FD, p=1.000 versus p=1.000) at each of the time points (Table 3). The CG's fat percentage values were found to be insignificantly different at each of the time points (Table 3). Figure 1 indicates that although the fat percentage values decreased in both the ED and FD groups, the between-group testing results indicated no significant difference (Table 4). The CG's fat percentage values decreased at Week 6 and increased drastically at Week 12.
WHR
A within-subject test with a Greenhouse-Geisser correction indicated insignificant WHR decreases among the three measurement times: F1.785, 91.052=2.888, p=0.067 (partial η2=0.054). There was no statistically significant difference among the intervention groups and CG over measurement time of WHR: F4,102=0.450, p=0.772 (partial η2=0.017). The LSD comparisons (shown in Table 3) revealed that the means between the baseline and Week 6, baseline and Week 12, and Week 6 and Week 12 measurements were insignificant. Figure 1 shows that although the WHR values decreased in both the ED and FD groups, the between-group testing results indicated no significant difference (Table 4). The CG's WHR values decreased at Week 6 and increased again at Week 12.
MAP
A within-subject test indicated MAP value decreases among the three measurement times: F2,94=7.542, p=0.0001 (partial η2=0.138). There was no statistically significant difference among the intervention groups and CG over measurement time of MAP: F4,94=1.0, p=0.412 (partial η2=0.041). The LSD comparisons (shown in Table 3) revealed that no significant difference was found among the three time points in any of the groups, except between baseline and Week 12 (p=0.012). Figure 1 shows that although the MAP values decreased in both the ED and FD groups, the between-group testing results indicated no significant difference (Table 4). The CG's MAP values decreased at Week 6 and further decreased at Week 12.
Comparison of Means
Figure 1 illustrates the estimated marginal means from the repeated-measures ANOVA on body weight, BMI, fat percentage, WHR, and MAP and shows the effect of each outcome measurement at the different time points. Although Figure 1a–d indicates better results for the FD and ED groups than for CG, similar results were found for the three groups on MAP (Fig. 1e). A better fat percentage reduction was found in the ED group than in the FD group and CG, particularly during the second 6 weeks (Fig. 1c).
Discussion
Although food diaries have been used as food intake activity logs, few studies have explored their use as behavioral interventions for weight reduction. Little is known about the effect of activity logs on behavioral changes in eating. This study compared the weight loss results of two groups of participants using different dietary recording tools and one group of participants using no dietary recording tool. In this randomized controlled trial, body weight, BMI, fat percentage, and WHR values were compared to investigate the effects of weight loss on the three groups. MAP was measured to determine whether blood pressure improved with healthy eating.
The weight reduction results were positive in both experimental groups. The 12-week weight loss program equipped the participants with nutrition skills and knowledge, emphasized the importance of exercise, and provided tips on healthy eating. The three groups were asked to apply the skills they learned to losing weight. However, the CG participants were not required to take part in interactive follow-up activities, which would have provided them with feedback. They did not know whether their approaches to eating were cutting their calorie intakes or whether they were eating a balanced diet with the nutrients sufficient for body maintenance. We compared the results of the FD group and CG and the results of the ED group and CG, respectively, to determine whether the awareness of the FD and ED group participants increased during their weight loss progress. The food and electronic diaries reminded participants what they had eaten over the course of a whole day. Nutritionists then commented on the records so that the participants could determine how to further improve their eating behavior or food item combinations to fit their interests and follow the principles of a balanced diet. This was important, as the participants could only lose weight when they engaged their individual interests in making food choices. It was revealed that the FD and ED groups achieved better results in terms of body weight, BMI, fat percentage, WHR, and MAP. Although the CG participants achieved some reduction in the first 6 weeks, they experienced rebounds of body weight, BMI, fat percentage, and WHR in the second 6 weeks, indicating that activity logs are crucial for healthy eating in a weight reduction program. According to Pallant,17 standard measures of partial η2 in ANOVA are 0.01, 0.06, and 0.14 for small, medium, and large effect sizes, respectively. The findings here reflected large effect sizes in time factors and the interaction of time with groups in body weight. Large effect size also happened in time factors in BMI, which suggested further exploration would be required.
Post hoc tests in ANOVA are designed for additional exploration of the differences among means in baseline–Week 6–Week 12. The results provided specific information on which interaction of pairs (baseline–Week 6, Week 6–Week 12, baseline–Week 12) was significantly different from one another. According to the results, the ED group performed better than the FD group because the ED group showed more reduction in fat percentage compared with the CG and FD group, and it showed further reduction in fat percentage from Week 6 to Week 12. In the same period, however, participants in CG and the FD group regained fat, with those in CG regaining more than they lost from baseline to Week 6. The application of an electronic food diary incorporated the food nutrient information into online reports, providing useful nutrition education instantly to the participants along with prompt feedback and comments. The feedback generated by the online reports was helpful, as it allowed the participants to modify their eating attitudes, food choices, and portion sizes the following day. In addition, their eating behavior was reflected in their food information input and thus promptly displayed by the online reports. This established an interactive component in the eating modification process that became the critical mass for the participants' weight loss achievements. The findings showed that although the ED group achieved a greater fat percentage reduction than the FD group, the groups showed similar body weight and BMI reductions, confirming that the participants who used the electronic dietary records had a better understanding of healthy eating. It should be noted that body weight constitutes both lean body mass and body fat and that reduction in lean body mass lowers our metabolic rate, which makes weight reduction more difficult in the latter stage. In contrast, reduction in body fat was the targeted outcome because accumulated body fat was the cause of many obesity-related metabolic syndromes. This also explained although body weight reduction were similar for participants in FD and ED groups, by interpreting the body fat, body weight, and BMI results together, the participants in the ED group lost fat instead of lean muscle mass, which was the desired outcome. Meanwhile, the participants in the FD group lost fat and lean body mass simultaneously, which was a less desirable outcome. As fat percentage is a critical indicator for successful weight reduction, therefore, the ED group participants were shown to be more effective at modifying their eating behavior than those in the FD group.
Limitations
Cautions must be taken when the numbers of participants are small when applying Mauchly's test of sphericity because it has been criticized for its failing to detect variances in small samples. However, it is a common test, and this test is still a readily available tool for testing sphericity in this study.
Future Research
Within the 12-week study time frame, the rebounding of all of the outcome measurements except MAP showed less sustainable weight reduction results in the CG participants. We suspect that the participants lost contact with the nutritionists after the three seminar sessions and that they could not sustain their efforts to eat healthily. Body weight rebounding is a common problem in weight reduction programs because participants are deemed successful only when their weight loss is sustained. According to this study's findings, both the FD and ED group participants sustained the effects of weight reduction over the 12 weeks. It would be valuable to determine whether electronic dietary records perform better on weight loss sustainability. Further research that can take advantage of longer study periods is required.
Conclusions
The food diaries and electronic dietary records applied in teledietetics produced better weight reduction results than the results of our CG. The electronic dietary records were more successful than food diaries in fat percentage reduction rather than lean body mass, indicating that desirable weight reduction could be facilitated by the higher healthy-eating awareness promoted by electronic dietary records.
Disclosure Statement
No competing financial interests exist.
References
- 1.Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed S, Szapary PO, Rader DJ, Edman JS, Klein S. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 2003;348:2082–2090 [DOI] [PubMed] [Google Scholar]
- 2.Heymsfield SB, van Mierlo CAJ, van der Knaap HCM, Heo M, Frier HI. Weight management using a meal replacement strategy: Meta and pooling analysis from six studies. Int J Obes 2003;27:537–549 [DOI] [PubMed] [Google Scholar]
- 3.Astrup A, Caterson I, Zelissen P, Guy-Grand B, Carruba M, Levy B, Sun X, Fitchet M. Topiramate: Long-term maintenance of weight loss induced by a low-calorie diet in obese subjects. Obes Res 2004;12:1658–1669 [DOI] [PubMed] [Google Scholar]
- 4.Deibert P, König D, Schmidt-Trucksaess A, Zaenker KS, Frey I, Landmann U, Berg A. Weight loss without losing muscle mass in pre-obese and obese subjects induced by a high-soy-protein diet. Int J Obes 2004;28:1349–1352 [DOI] [PubMed] [Google Scholar]
- 5.Foster GD, Makris AP, Bailer BA. Behavioral treatment of obesity. Am J Clin Nutr 2005;82(Suppl):230S–235S [DOI] [PubMed] [Google Scholar]
- 6.Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. J Consult Clin Psychol 2000;68:95–102 [PubMed] [Google Scholar]
- 7.Wadden TA, Foster GD. Behavioural treatment of obesity. Med Clin North Am 2000;84:441–461 [DOI] [PubMed] [Google Scholar]
- 8.Jeffery RW, Wing RR, Thorson C, Burton LR. Strengthening behavioural interventions for weight loss: A randomized trial of food provision and monetary incentives. J Consult Clin Psychol 1993;6:1038–1045 [DOI] [PubMed] [Google Scholar]
- 9.Wing RR, Jeffery RW, Burton LR, Thorson C, Nissinoff KS, Baxter JE. Food provision vs structured meal plans in the behavioural treatment of obesity. Int J Obes Relat Metab Disord 1996;20:56–62 [PubMed] [Google Scholar]
- 10.Brownell KD. The LEARN program for weight management 2000. Dallas: American Health Publishers Co., 2000 [Google Scholar]
- 11.Yon BA, Johnson RK, Harvey-Berino J, Gold BC, Howard AB. Personal digital assistants are comparable to traditional diaries for dietary self-monitoring during a weight loss program. J Behav Med 2007;30:165–175 [DOI] [PubMed] [Google Scholar]
- 12.Boushey CJ, Kerr DA, Wright J, Lutes KD, Ebert DS, Delp EJ. Use of technology in children's dietary assessment. Eur J Clin Nutr 2009;63:S50–S57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guillen S, Sanna A, Ngo J, Meneu T, Hoyo ED, Demeester M. New technologies for promoting a healthy diet and active living. Nutr Rev 2009;67:S107–S110 [DOI] [PubMed] [Google Scholar]
- 14.Long JD, Littlefield LA, Estep G, Martin H, Rogers TJ, Bosewell C, Shriver BJ, Roman-Shriver CR. Evidence review of technology and dietary assessment. World Evid-Based Nutr 2010;7:191–204 [DOI] [PubMed] [Google Scholar]
- 15.Chung LMY, Chung JWY, Wong TKS. Usability test of an interactive dietary recording. Int Electron J Health Educ 2009;12:123–134 [Google Scholar]
- 16.Chung LMY, Chung JWY. Tele-dietetics with food images as dietary intake records in nutrition assessment. Telemed J E Health 2010;16:691–698 [DOI] [PubMed] [Google Scholar]
- 17.Pallant JF. SPSS survival manual: A step by step guide to data analysis using SPSS, 4th ed. Maidenhead, United Kingdom: Open University Press/McGraw-Hill Education, 2010 [Google Scholar]