Abstract
Cutaneous metastases of rectal adenocarcinoma is a rare phenomenon. We present a 65 year-old man with a painless nodule on the scrotal skin. Excisional biopsy of the nodules revealed a metastasis from rectum adenocarcinoma. Afterwards, the left scrotum was treated with a radiation therapy and the patient also received a salvage chemotherapy. The patient is still alive without any distant metastasis after the therapy, which was initiated 12 months ago.
Key words: rectum carcinoma, scrotal skin metastasis, treatment
Introduction
Colorectal cancer is the third most common cancer type in men and the second most common cancer type in women in Turkey and colorectal cancer incidence is approximately 7 per 100,000, with approximately 5000 new cases and 3200 deaths annually.1 The most common sites of colorectal cancer metastases are lymph nodes liver, the lungs and bones. It is an uncommon situation for clinicians to observe skin metastases derived from colorectal cancer in daily practice. While metastases to the urogenital tract from prostate cancer, lung cancer and malign melanoma have been defined in literature, there are only a few cases reported regarding to scrotal skin metastasis from colorectal primary.2-6 For this reason, we would like to share our clinical experience with a lower rectal cancer which has metastases to the scrotal skin.
Case Report
A 65-year-old man reported in March 2010 with rectal bleeding and tenesmus. Colonoscopy demonstrated an exophytic and ulcerated lesion at the lower rectal region (the tumor was 3 cm superior of the anal verge obstructing 1/3 of intraluminal pathway). Incisional biopsies confirmed the presence of adenocarcinoma of the rectum. Computed tomography (CT) of abdomen and pelvis demonstrated a locally invasive distal rectal neoplasm, without evidence of distant metastases. Magnetic resonance imaging (MRI) of a pelvic region confirmed a locally advanced neoplasm. Therefore the tumor was a radiologically T3 N0 M0 low rectal cancer.
In April 2010, preoperative chemoradiotherapy with a total dose of 5040 cGy, given in 28 fractions, five days per week was applied. As a concomitant chemotherapy he received 5-Fluorouracil given in five days bolus injection (400 mg/m2) plus folinic acid (30 mg/m2) per day during the first and fifth weeks of radiotherapy. Then, he was scheduled for low anterior resection six weeks following the completion of chemoradiotherapy. Pathological stage was T4 N0 M0. After the surgery, he received a boost dose of radiotherapy (10 Gy in 5 fractions) due to positive radial margins. He was subsequently treated with 2 cycles 5FU-FA chemotherapy.
In June 2011, one year after surgery, PET/CT (18-Fluorodeoxyglucose positron emission tomography based computerised tomography) demonstrated a recurrence in the lower part of the rectum (Suv max: 10.76). At that time there was no pathologic evidence of recurrence, so the patient only followed up.
In January 2012, subsequent PET/CT showed a progression of the rectal recurrences, including the spermatic cord with increased FDG uptake (Suv max: 22.15). Ultrasonography demonstrated a slightly thickening of the skin of the left scrotum. The patient had the painless, hazelnut-sized slightly reddish nodules affecting the skin of the left scrotum (Figure 1). The nodular lesions were up to 14 mm in diameter. The patient then underwent an excisional biopsy from the left scrotal nodules. Macroscopic examination revealed four noduler formations; the bigger one being 3.5 cm. In microscopic assessment; the tumors were under the squamous epithelium and to form atipic glandular formation (Figure 2). This gland formations consist of cells with scanty cytoplasm, hyperchromatic nuclei and atypic epithelial feature (Figure 3). Biopsy of the skin compared with the original rectal cancer material, both tumor have same histopathology (Figure 4). Resection margin was also involved with the tumoral tissue.
Figure 1.

Multiple, bean, hazelnut-sized slightly reddish nodules on the scrotum.
Figure 2.
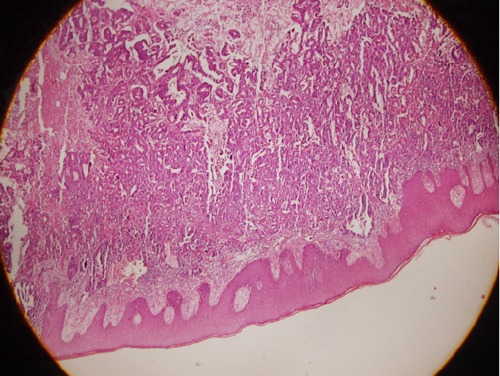
Haematoxylin and eosin stains positive for carcinoma cells under the squamous epithelium.
Figure 3.
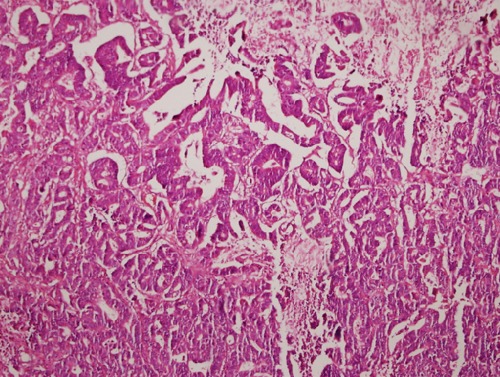
Higher power (100×) histology showing atipic glandular formation.
Figure 4.
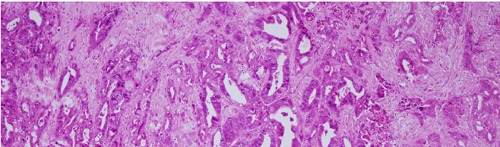
Histopathology of the tumors.
At this stage, the patient was given orally twice a day, Xeloda (Capecitabine) treatment (1250 mg/m2, in total; 2500 mg/m2). He also received palliative radiotherapy to the left scrotal region with electron beams. Radiotherapy was applied with 6 MeV energy, 300 cGy daily fractions, a total dose of 4500 cGy. During treatment and in the early period, we saw only grade 2 skin side effects according to RTOG acute toxicity criteria. Then, as a late side effect we observed grade 2 skin toxicity (patichy atrophy and hair loss) and grade 3 subcutaneous toxicity (severe induration and contracture). The patient is still alive without any distant metastasis after the therapy which was initiated 12 months ago.
Discussion
Cutaneous metastases originating from internal malignancy are unusual.2 The most frequent sites of cutaneous metastases originating from colorectal cancer have been found to be the chest, abdomen and pelvis.7 On the other hand, cutaneous metastases derived from colorectal cancer to the scrotum are rare. In literature, the average time from diagnosis of cutaneous metastases from colorectal carcinoma to death is between 6-18 months.7
Although cutaneous metastases from colorectal cancer on other sites including extremities, genitalia other than scrotum head and neck region have been reported,8,9 to our knowledge, there is a few data regarding scrotal skin metastases of rectal primary.
Several mechanisms of cutaneous metastases have been predicted including haematogenous spread, lymphatic spread, direct extension, expanding through the ligaments of embryonic origin and seeding of exfoliated tumor cells. Patients with scrotal metastasis usually have widespread metastatic disease and thereby poor general health. The common presentation of scrotal metastasis is cutaneous nodule without pain. Diagnosis is usually made by biopsy. Management of scrotal metastasis is mainly palliative. The treatment modalities include radiotherapy, chemotherapy and surgery although the survival benefit remains controversial. But prognosis is usually poor and patients with scrotal metastasis die within 1-1.5 year. We report our experience of managing this patient with radiochemotherapy and surgery with very good results of regional control and without any distant metastasis. These data provide strong support for a policy of using radiochemotherapy with surgery as a salvage therapy. To the best of our knowledge, this is the first reported case in the literature of scrotal skin metastasis managed with chemoradiotherapy and surgery.
Conclusions
In summary, we presented a patient with advanced rectal cancer who has scrotal skin lesions. A knowledge is needed in such cases to rule out cutaneous metastases. Although, patients with scrotal cutaneous metastases of rectal cancer have poor prognoses with limited effective treatment options, excision followed by short course radiotherapy can be a good palliative treatment option for these tumors.
References
- 1.Tatar M, Tatar F. Colorectal cancer in Turkey: current situation and challenges for the future. Eur J Health Econ 2010;10Suppl 1:S99-S105 [DOI] [PubMed] [Google Scholar]
- 2.Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the sign of internal carcinoma. J Am Acad Dermatol 1990;22:19-8 [DOI] [PubMed] [Google Scholar]
- 3.Boucher Kw, Heymann WR. Ulcerated papules of the scrotum. Arch Dermatol 2001;137:495-6 [PubMed] [Google Scholar]
- 4.Reuter J, Bruckner-Tuderman L, Braun-Falco M. Epidermotropic scrotal metastasis of colorectal cancer. Int J Colorectal Dis 2007;22: 1133-2 [DOI] [PubMed] [Google Scholar]
- 5.Hayashi H, Shimizu T, Shimizu H. Scrotal metastases originating from colorectal carcinoma. Clin Exper Dermatol 2003;28: 222-10 [DOI] [PubMed] [Google Scholar]
- 6.McWeeney D, Martin ST, Ryan RS, et al. Scrotal metastases from colorectal carcinoma: a case report. Cases J 2009;2:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: retrospective study of 4020 patients. J Am Acad Dermatol 1993;29: 228-36 [DOI] [PubMed] [Google Scholar]
- 8.Stavrianos SD, Mclean NR, Kelly CG. Cutaneous metastasis to the head and neck from colonic carcinoma. Eur J Surg Oncol 2000;26:518-9 [DOI] [PubMed] [Google Scholar]
- 9.Wright PK, Jha MK, Barrett PD. Colonic adenocarcinoma presenting as a cutaneous metastasis in an old operative scar. J Postgrad Med 2003;49:157-8 [PubMed] [Google Scholar]


