Abstract
The promotion of physical activity for people with multiple sclerosis (MS) would benefit from information about the common types of physical activity self-selected by this population. This study examined the most frequent types of physical activity self-reported by a large sample of people with MS. The data were collected as part of the baseline assessment of a longitudinal investigation of physical activity in relapsing-remitting MS (RRMS). The participants (N = 272) were sent a battery of questionnaires through the US Postal Service that included the Modifiable Activity Questionnaire for assessing types of physical activity performed during the previous year. Walking was ranked number 1 for both the first and second most common types of physical activity self-selected by people with MS, and it was ranked number 4 as the third most common type of self-selected physical activity. Collectively, 79% of the sample reported walking as a frequent form of self-selected physical activity in the previous year. Other notable types of physical activities self-selected by people with MS were gardening (44%), weight training (34%), bicycling (30%), and calisthenics (20%). This information may assist clinicians and practitioners in the development of physical activity programs and recommendations for people with MS.
The study of physical activity behavior and its consequences among people with multiple sclerosis (MS) is of increasing interest. Existing research has indicated that individuals with MS are generally physically inactive and sedentary,1 but that physical activity is associated with many desirable outcomes in this population, including improvements in symptoms, function, disability, and quality of life.2,3 This paradox may be related to the recommendation by clinicians of a sedentary lifestyle among people with MS as a means of avoiding fatigue. This belief has been refuted by more recent evidence-based research, and there is emerging interest among clinicians and practitioners in the promotion of physical activity as an integral part of treatment and health maintenance in those with MS.
In order to promote physical activity in this population, a comprehensive understanding of the actual types of physical activity self-selected by people with MS would be beneficial. To date, limited information is available on the different modes of physical activity performed by individuals with MS,1 but such information is important for four primary reasons. First, clinicians and practitioners who recommend physical activity to their patients with MS would benefit from knowing the most frequent types of physical activity self-selected in this population. Second, such information would set the research agenda for evaluating the consequences of the most frequent types of physical activity self-selected in people with MS. Third, this information would better inform the development and validation of outcome measures for quantifying frequent types of physical activity in people with MS. Finally, such information would facilitate the development of interventions that are tailored to the most common physical activities, although such interventions might appropriately target multiple common modes of movement, including those that are infrequent but have significant benefit for patients.
The present study examined the most frequent types of physical activity self-selected by people with MS. Further, it examined variation in the frequency of the most common types of physical activity across demographic (sex and body-mass index [BMI]) and clinical (disability and disease duration) variables. The purpose of the study was to determine the primary modes of physical activity self-selected by people with MS to both aid in the promotion of physical activity and encourage further research in this population.
Methods
Participants
The data presented in this article are from the baseline assessment of an ongoing, longitudinal investigation of symptoms and physical activity behavior in people with relapsing-remitting multiple sclerosis (RRMS) funded by the National Multiple Sclerosis Society.4 The recruitment, screening, and inclusion criteria have been thoroughly described elsewhere.5 The initial goal of recruitment was a sample of 250 individuals with RRMS who were interested in participating in a study on symptoms and physical activity. This goal was exceeded, with a final sample for this analysis of 272 individuals with RRMS.
Measures
Sex, height, weight, and disease duration were measured with a standard demographics scale. Disability was measured with the Patient-Determined Disease Steps (PDDS) scale.6 The frequency of types of physical activity was measured using the Modifiable Activity Questionnaire (MAQ). The MAQ is an interviewer-administered assessment of leisure time and occupational physical activity over a year.7,8 This study included only the assessment of leisure time physical activity (LTPA). The LTPA portion of the MAQ contains a list of 40 common physical activities for adults. The participants identified all LTPAs performed ten or more times over the past 12 months, and then reported the number of months per year, average number of times per month, and average number of minutes per time for each identified LTPA. The frequency of the identified LTPAs was computed by multiplying the number of months per year by the average number of times per month, and this frequency was then used for ranking the first, second, and/or third most frequent LTPAs for each participant. The weekly frequency (ie, number of months per year multiplied by the average number of times per month divided by 52 weeks) and duration per session (ie, average number of minutes per time) were further reported for the top three most frequent LTPAs. Importantly, the MAQ has been identified as a valid and reliable assessment of physical activity in adults without MS based on correlations with activity counts from activity monitors and energy expenditure from doubly labeled water,9,10 but it has not been validated in people with MS.
Procedure
The procedure was approved by an institutional review board at the University of Illinois, Urbana-Champaign. After initial telephone contact, inclusion screening, and completion of informed consent and MS verification documentation, the participants were sent a battery of questionnaires through the US Postal Service that included the demographic scale, PDDS, and MAQ. The project coordinator called to make sure the participants received the materials and understood the instructions, and then assisted them in the completion of the MAQ. Participants returned their study materials through the US Postal Service using a prestamped, preaddressed envelope that was provided. Participants were contacted by telephone or e-mail up to three times to remind them to return their study materials. Of those who returned study materials, three follow-up attempts were made to collect missing data. Participants received remuneration of $20 upon the return of their study materials.
Data Analysis
Frequency and descriptive analyses and then χ2 tests were performed using SPSS, version 18.0 for Windows (SPSS, Chicago, IL). The frequency analysis identified the most and least common types of physical activity (ie, rates of the first, second, and third most frequent LTPAs for each participant) reported by participants. The descriptive analyses (mean ± standard deviation) were provided for the weekly frequency and duration per session of the most common types of physical activity. The χ2 tests identified differences in the frequencies of the most commonly reported types of physical activity between groups dichotomized for sex (women vs. men), weight status (BMI <25 vs. BMI ≥25), mobility disability (PDDS <3 vs. PDDS ≥3), and disease duration (duration <10 years vs. duration ≥10 years). Statistical significance was noted with a P value of <.05 and a two-tailed test.
Results
Sample Characteristics
The final sample included 272 individuals with RRMS: 235 women, 36 men, and 1 person not reporting gender. As for weight status, 123 individuals reported having normal body weight (BMI <25) and 143 reported being overweight (BMI ≥25); 6 people did not provide height and weight. A total of 177 participants reported no problems with mobility, whereas 89 participants reported onset of mobility disability (PDDS ≥3); 6 people did not provide PDDS data. For disease duration, the sample included 194 individuals who had had MS for less than 10 years and 77 individuals who reported a longer duration (duration ≥10 years); 1 person did not report disease duration.
Frequency of Physical Activities
All 272 participants reported engaging in at least one type of physical activity in the previous year, with 241 and 191 individuals reporting performing two or three types of physical activity, respectively, in the previous year. The rank and associated frequency, average weekly frequency, and average duration per session of the top five first, second, and third most common types of physical activity self-reported by individuals with MS are shown in Table 1. Walking was ranked number 1 for both the first and second most common types of physical activity, and it was ranked number 4 as the third most common type. Collectively, 79% of the sample reported walking as a frequent self-selected form of physical activity in the previous year. Of those who reported walking as the first most frequent self-selected physical activity, the weekly frequency and duration per session were 3.6 ± 2.1 days per week and 33.8 ± 22.4 minutes per session, respectively.
Table 1.
Ranking of the first, second, and third most common physical activities self-selected by individuals with relapsing-remitting multiple sclerosis
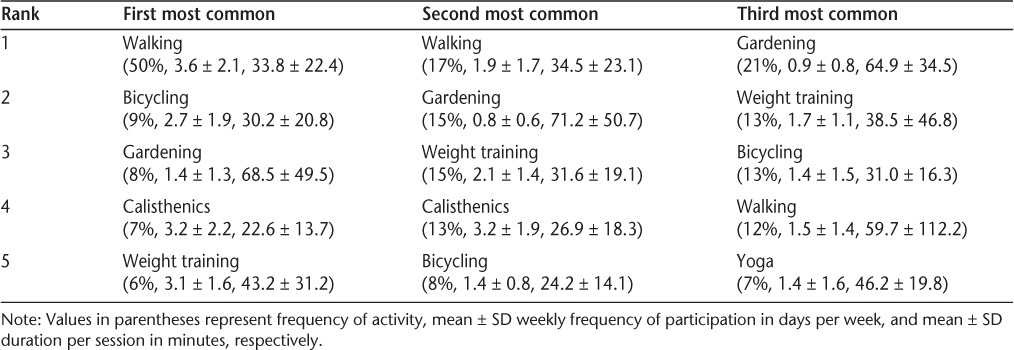
Other notable types of physical activities self-selected by people with MS were bicycling, gardening, calisthenics, and weight training. These activities were ranked numbers 2 through 5 as the most frequent type of physical activity self-selected by individuals with MS. Interestingly, gardening was ranked number 3, 2, and 1 for the first, second, and third most frequent types of self-selected physical activity, respectively. Bicycling and weight training were also common types of physical activity. Collectively, 44% of participants reported gardening, 34% reported weight training, 30% reported bicycling, and 20% reported calisthenics as self-selected forms of physical activity.
The frequency analysis also identified several modes of physical activity that were surprisingly infrequent in people with MS in the previous year. For example, swimming and water aerobics were reported as the most frequent self-selected mode of physical activity by only 2% and 3% of participants, respectively. In addition, swimming was reported as the second and third most frequent mode of self-selected physical activity by only 5% and 6% of participants, respectively. Yoga and tai chi were reported as the most frequent mode of self-selected physical activity by only 3% and 2% of the sample, respectively. Yoga was reported as the second or third most frequent mode of self-selected physical activity by only 7% of participants.
Demographic and Clinical Differences
This analysis examined differences in rates of the five most common types of physical activity reported by people with MS in the previous year based on sex, weight status, mobility disability, and disease duration. The frequency of the five most common types of physical activity did not differ significantly by sex (χ24= 4.70, P = .32, N = 214) but did differ by weight status (normal weight vs. overweight) (χ24 = 11.52, P = .02, N = 212). There were no significant differences in the rates of walking (59% vs. 66%) and weight training (7% vs. 8%) between normal and overweight groups, but there were significant differences between groups in the rates of bicycling (14% vs. 7%), calisthenics (13% vs. 4%), and gardening (6% vs. 14%).
The frequency of the five most common types of physical activity did differ by mobility disability status (χ24 = 9.94, P = .04, N = 212) and by disease duration (χ24 = 12.01, P = .02, N = 214). Between those without and with mobility disability, there were differences in the rates of walking (70% vs. 50%), calisthenics (5% vs. 14%), bicycling (9% vs. 13%), and weight training (6% vs. 11%), but not gardening (10% vs. 11%). Similarly, there were differences between those with shorter versus longer disease duration in the rates of walking (68% vs. 52%), calisthenics (7% vs. 14%), bicycling (7% vs. 19%), weight training (7% vs. 11%), and gardening (12% vs. 6%).
Discussion
Little information is available on the frequency of types of physical activity self-selected by people with MS,1 but such information has practical value in the promotion of physical activity in this population. In this study, walking was identified as a frequent type of physical activity self-selected by nearly 80% of the sample; it was followed in overall frequency by gardening (44%), weight training (34%), bicycling (30%), and calisthenics (20%). Not only was walking the most common type of physical activity self-selected by 50% of the sample, but this result was consistent across gender, weight status, mobility disability, and disease duration. Those who self-selected walking as their primary mode of physical activity were not meeting public health guidelines for the frequency and duration of moderate physical activity (5 or more days per week, 30 minutes per session) among adults in the United States.11 The other types of self-selected physical activity were ranked the most common by less than 10% of the sample. The results clearly identify walking as the primary type of physical activity self-selected by this sample of ambulatory individuals with RRMS. This observation is consistent with a recent study in which walking was reported as the most frequent type of physical activity by nearly 56% of older adults with a neurodegenerative disease.12
The possible implications of this finding are numerous. Walking is a relatively simple form of physical activity that can be performed by ambulatory individuals with MS almost anywhere. It does not require specialized equipment, access to a gym, or assistance from an exercise specialist, and it can be performed with minimal expense and experience. In addition, walking can be self-monitored by an individual or externally monitored by a clinician using a simple, inexpensive pedometer such as the Yamax SW-200 (Yamax, Tokyo, Japan) that has been effectively evaluated in people with MS.1 This suggests that clinicians could easily develop a walking program for their ambulatory patients with MS that is self-administered and monitored by pedometry. To that end, future researchers should develop and test the efficacy of interventions for increasing walking as a form of physical activity in people with MS, and secondarily examine the resulting impact on symptoms, function, disability, and quality of life. Given that people with MS are substantially less physically active than the general population of adults without a chronic condition,1 attempting to increase the rate of this vital health behavior in the MS population is clearly a worthwhile pursuit.
Our research has additional implications for clinicians and practitioners who are interested in the promotion of physical activity in people with MS. Other activities that can be encouraged in this population beyond walking include gardening, weight training, bicycling, and calisthenics. No evidence currently exists on the consequences of gardening as a type of physical activity in MS, but the rate of gardening in the current sample of people with MS is roughly consistent with that reported in a sample of older adults with a degenerative neurologic disease (44% and 33%, respectively).12 Individuals with mobility disability and longer disease duration had higher rates of bicycling, weight training, and calisthenics compared with those without mobility disability and shorter disease duration. This may be related to evidence that weight training has been associated with desirable effects on muscle strength and function as well as walking capacity in people with MS.13 In addition, bicycling has been associated with reductions in lower-leg spasticity in people with MS.14 Gardening, weight training, bicycling, and calisthenics could be easily integrated along with walking into a recommendation for becoming more physically active. This recommendation would provide a great amount of flexibility for initiating and maintaining a physical activity routine among those with MS.
The frequency of walking behavior in MS may have implications for the measurement of physical activity in this population. Motion sensors such as pedometers and accelerometers are typically worn around a person's center of mass to measure displacement of the “whole body” in order to quantify physical activity, particularly walking. Because walking is a common type of activity among ambulatory adults with MS, pedometry and accelerometry—which measure both the frequency and rate of walking—are good choices for quantifying physical activity in this population. This technology can also capture physical activity associated with gardening, another common form of physical activity among those with MS, but is less applicable to weight training, bicycling, and calisthenics. Collectively, motion sensors are a good choice for measuring physical activity in MS because of their ability to measure walking either directly or indirectly. This recommendation is consistent with previous research suggesting that pedometers are easy-to-use and cost-effective tools for measuring physical activity in sedentary populations.15 The other forms of physical activity, including bicycling, weight training, and calisthenics, can be captured through the use of supplemental questionnaires.
Interestingly, water-based physical activities such as swimming and water aerobics, along with alternative forms of physical activity such as yoga and tai chi, were not commonly reported in this sample of individuals with RRMS. The infrequent performance of yoga in people with MS was consistent with the previous and current rates of yoga practice (7% and 5%, respectively) found in a large descriptive study of complementary and alternative medicines in MS.16 The infrequency of swimming is consistent with the rate of about 8% reported in a sample of older adults with a degenerative neurologic disease.12 This is surprising, as swimming and yoga are frequently suggested as forms of physical activity for individuals with MS. Swimming, for example, is a non-weightbearing activity that can increase aerobic capacity while avoiding possible complications of overheating in thermosensitive people with MS. Yoga, as another example, is a mind-body approach that emphasizes meditation, breathing, and postures and has been reported to be very beneficial for people with MS.16 Future research might examine reasons why swimming and yoga are significantly less common than other physical activities in people with MS. Such reasons may include the inconvenience of accessing a pool and/or the cost of attending yoga classes. If the cost of yoga classes is a burden, this might support the development and evaluation of a yoga intervention that is delivered through DVD or the Internet. Such an effort may be worthwhile given the significant possible benefits of yoga in MS.17
This study has several limitations that warrant discussion. The sample volunteered for a study on symptoms and physical activity in RRMS; this may reflect an increased interest and rate of participation in physical activity that positively biased our results. By extension, the sample may not be representative of people with MS, thereby limiting the generalizability of the results more broadly. Also, the sample included only ambulatory individuals with RRMS, and the results would clearly be different in a less ambulatory or even wheelchair-bound sample of people with MS. The fact that the sample included only people with RRMS limits the generalizability of our results to those with other types of MS. Moreover, the MAQ included a list of only 40 activities; this may have limited the response options by failing to capture other forms of physical activity commonly self-selected by people with MS. Finally, the MAQ has not been validated in people with MS, and this was not accomplished in the present study.
Overall, the present study provides valuable information on the most common types of physical activity self-selected by people with MS. This information may assist clinicians and practitioners in the development of physical activity programs and recommendations for individuals with MS. It also supports existing methods of quantifying physical activity in MS and sets the stage for subsequent programs that focus on promoting walking and examining its possible consequences in people with MS. Physical activity is associated with numerous benefits, but people with MS are still largely inactive and sedentary. The results of this study may ultimately facilitate the promotion of increased physical activity among people with MS.
PracticePoints.
Although physical activity is associated with numerous benefits, people with MS are still generally inactive and sedentary.
Walking is the most common type of physical activity self-selected by people with MS.
The findings of this study may assist clinicians and practitioners in the development of physical activity programs and recommendations for people with MS.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This work was supported, in part, by a grant from the National Multiple Sclerosis Society (RG 3926A2/1).
References
- 1.Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler. 2005;11:459–463. doi: 10.1191/1352458505ms1188oa. [DOI] [PubMed] [Google Scholar]
- 2.Garrett M, Coote S. Multiple sclerosis and exercise in people with minimal gait impairment—a review. Phys Ther Rev. 2009;14:169–180. [Google Scholar]
- 3.Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;25:CD003980. doi: 10.1002/14651858.CD003980.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Motl RW, McAuley E, Wynn D, Suh Y, Weikert M, Dlugonski D. Symptoms and physical activity among adults with relapsing-remitting multiple sclerosis. J Nerv Ment Dis. 2010;198:213–219. doi: 10.1097/NMD.0b013e3181d14131. [DOI] [PubMed] [Google Scholar]
- 5.Weikert M, Motl RW, Suh Y, McAuley E, Wynn D. Accelerometry in persons with multiple sclerosis: measurement of physical activity or walking mobility? J Neurol Sci. 2010;290:6–11. doi: 10.1016/j.jns.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 6.Hadjimichael O, Kerns RD, Rizzo MA, Cutter G, Vollmer T. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007;127:35–41. doi: 10.1016/j.pain.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(suppl 6):S1–205. [PubMed] [Google Scholar]
- 8.Vuillemin A, Boini S, Bertrais S, et al. Leisure time physical activity and health-related quality of life. Prev Med. 2005;41:562–569. doi: 10.1016/j.ypmed.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Kriska AM, Knowler WC, LaPorte RE, et al. Development of questionnaire to examine the relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990;13:401–411. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 10.Schulz LO, Harper IT, Smith CJ, Kriska AM, Ravussin E. Energy intake and physical activity in Pima Indians: comparison with energy expenditure measured by doubly-labeled water. Obes Res. 1994;2:541–548. doi: 10.1002/j.1550-8528.1994.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 11.United States Department of Health and Human Services. Healthy People 2010 Objectives. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 12.Ashe MC, Miller WC, Eng JJ, Noreau L. Older adults, chronic disease, and leisure-time physical activity. Gerontology. 2009;55:764–772. doi: 10.1159/000141518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dalgas U, Stenager E, Jakobsen J, et al. Resistance training improves muscle strength and functional capacity in multiple sclerosis. Neurology. 2009;73:1478–84. doi: 10.1212/WNL.0b013e3181bf98b4. [DOI] [PubMed] [Google Scholar]
- 14.Motl RW, Snook EM, Hinkle ML, McAuley E. Effect of acute leg cycling on the soleus H-reflex and modified Ashworth scale scores in individuals with multiple sclerosis. Neurosci Lett. 2006;406:289–292. doi: 10.1016/j.neulet.2006.07.061. [DOI] [PubMed] [Google Scholar]
- 15.Tudor-Locke CE, Myers AM. Challenges and opportunities for measuring physical activity in sedentary adults. Sports Med. 2001;31:91–100. doi: 10.2165/00007256-200131020-00002. [DOI] [PubMed] [Google Scholar]
- 16.Schwarz S, Knorr C, Geiger H, Flachenecker P. Complementary and alternative medicine for multiple sclerosis. Mult Scler. 2008;14:1113–1119. doi: 10.1177/1352458508092808. [DOI] [PubMed] [Google Scholar]
- 17.Oken BS, Kishiyama S, Zaidel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058–2064. doi: 10.1212/01.wnl.0000129534.88602.5c. [DOI] [PubMed] [Google Scholar]


