Mobility limitations, which affect the majority of individuals living with multiple sclerosis (MS), are frequently addressed by clinicians and researchers, as they are at the heart of patients' (and families') concerns at the time of diagnosis and throughout the course of the disease. Ambulation, one of the key components of mobility, is routinely assessed through patient report, direct observation, and standardized tests and scales to monitor the progression of MS and the efficacy of disease-modifying therapies. Mobility-related issues can be a major source of frustration for patients, families, and health-care providers given the progressive nature of the disease, its heterogeneity, and its unpredictability. However, the recent growth in the body of evidence for the assessment and management of mobility restrictions, and in the spectrum of interventions available, brings renewed energy and hope.
One of the main features of mobility limitations, besides their high prevalence, is their complexity, as illustrated in Figure 1. A key underlying factor in the complexity of mobility limitations is the neurologic impairments (eg, loss of motor control, spasticity, sensory loss, imbalance) resulting from disease activity. We are just starting to understand how multiple impairments compound one another to create a synergistic rather than an additive disabling effect. For example, studies have demonstrated how cognitive challenges during walking can worsen motor-induced gait deviations by limiting compensation strategies. In turn, decreased mobility can affect MS-related impairments and symptoms (eg, increased fatigue due to decreased activity, decreased range of motion due to reduced voluntary limb motion), and may even affect the disease process (eg, frequent urinary-tract infections may lead to increased frequency of MS exacerbations). Comorbidities also affect mobility, whether they are indirectly related to MS (eg, musculoskeletal problems due to abnormal gait pattern, decreased respiratory function due to respiratory muscle weakness and deconditioning) or are independent of MS (eg, cardiovascular conditions). In turn, decreased mobility can increase the risk of comorbidities (eg, obesity, osteoporosis).
Figure 1.
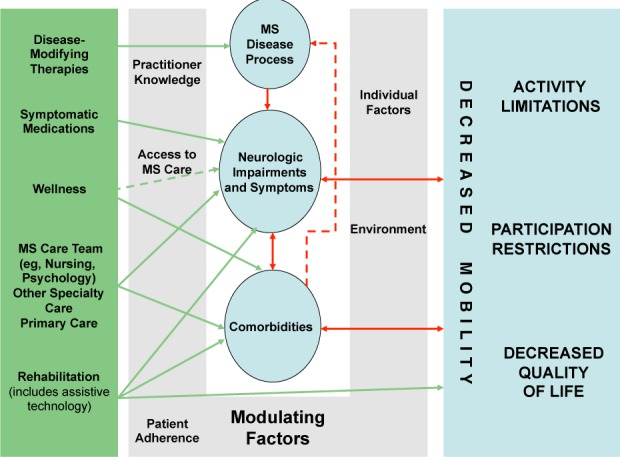
Complexity of mobility limitations
Assessing mobility, and the effect of interventions on mobility, is more complex than it seems. Walking, the activity most often assessed, has been monitored through the clinician's observation of walking a specific distance, calculating walking speed, and documenting the need for assistive devices. Detailed gait analysis usually requires too much time and equipment to be used in clinical care, and performance on tests administered at a given point in time in the clinic do not fully reflect a patient's success in safe and efficient ambulation in his or her own environment over the course of a day or week. The clinical trials of dalfampridine have reignited a debate regarding the use of walking speed as a proxy for ambulation, and what represents a clinically significant change in walking speed. Walking speed is increasingly valued as a predictor of overall function and health outcomes in other fields, particularly in the elderly and in stroke survivors. This has yet to be demonstrated in MS. At this time, it seems that a combination of simple walking tests and validated questionnaires (in addition to a complete history and examination) is the most efficient way of monitoring mobility in a clinical setting. Beyond walking, the assessment of transfers, wheelchair mobility, driving, and the impact of trunk control and upper-extremity function is traditionally handled by rehabilitation professionals, to whom patients do not always have easy and consistent access.
Addressing mobility limitations is indeed a complex task. Comprehensive MS care offers a variety of interventions designed to reduce or circumvent mobility limitations. Disease-modifying therapies, even though they often do not produce an immediate improvement in neurologic status, are essential in attempting to slow down the development of neurologic disability over time. Symptomatic therapies aim at providing more immediate relief of symptoms and impairments. For example, treating pain or spasticity may improve the capacity for ambulation or transfers; treating urinary urgency may allow people with MS to venture out of their house more often without fearing an episode of incontinence. Unfortunately, there is only limited evidence demonstrating the impact of most symptomatic therapies on mobility. Last year, the US Food and Drug Administration approved dalfampridine (extended-release 4-aminopyridine) to improve walking in patients with MS, based on the results of two large phase 3 placebo-controlled clinical trials. To our knowledge, this is the first time that a symptomatic medication for MS has been approved based on its effect on function. The importance of lifestyle changes, often labeled “wellness,” should not be underestimated. The wellness approach can empower patients and their families in their fight against this lifelong disease, may decrease the need for medications (eg, relaxation and sleep hygiene for fatigue), and can help augment and prolong the effect of skilled interventions such as rehabilitation. A variety of other interventions, involving the entire MS-care team, primary care, and non-neurologic specialty care, are essential in addressing comorbidities and complex symptom-management issues.
Rehabilitation can assist in managing the complexity of mobility limitations by direct interventions, establishing home exercise programs, and promoting independence in home and community mobility. In addition, comprehensive assessment by rehabilitation therapists knowledgeable about MS medical and rehabilitation care can open the door for new interventions based on underlying impairments or comorbidities that affect activity and participation. Assistive devices are frequently proposed and prescribed as patients have increasing difficulty in safe and independent ambulation. They are not always well accepted, in part because of their imperfections, but also often because they stigmatize disability in the general public, and may give patients the impression that they are “giving in to the disease.” Education and proper training in their use are key in helping patients and families to realize that these devices represent a way to fight the consequences of MS on activities and participation. Technological advances have led to the development of a new generation of “active devices,” such as functional electrical stimulation devices for footdrop, or robotic devices for gait training, which have a more positive image but need to be more extensively tested to understand how to use them optimally.
There are many personal, social, and environmental factors that influence the effect of MS and comorbidities on mobility, and the results of interventions. These factors may be intrinsic to the patient, such as personality, ability to adjust to the consequences of MS, spiritual background, premorbid activity level, and exercise routine. Or they may be external, such as the broad concept of environment, including geographic environment (eg, proximity to specialized MS care), physical environment (eg, stairs in the home, small bathroom that cannot accommodate a walker or a wheelchair), human environment (eg, presence of a spouse or family member to help at home), social and economic environment (education level, occupation, income, health-care insurance), and cultural environment (eg, cultural differences in handling disability and interacting with the health-care system). Access to care, practitioner knowledge, and patient adherence to treatment (medications, rehabilitation) are examples of factors that can affect the design and implementation of a plan of care. People living with MS often exhibit difficulty tolerating medications, rehabilitation interventions, and physical activity in general.
The accumulation of obstacles described above has led at times to a fatalistic view among patients and health-care professionals. It is true that it is important to define realistic expectations in both the short and the long term. However, never in the history of MS management has there been such a profusion of advances: a better understanding of the factors undermining mobility (including less frequently cited factors such as respiratory impairment), an increasing array of well-validated and user-friendly assessment tools, a growing body of evidence on the effects of medication on mobility, and the advent of a new generation of assistive devices. We thank the authors contributing to this theme issue of the International Journal of MS Care and look forward to working with them and all of our colleagues to continue to promote the recovery of function and community participation in those living with MS.
IN MEMORY OF HILLEL PANITCH, MD 1940–2010
Hillel Panitch, MD, a beloved husband, father, and physician, died on December 23, 2010, after a year-long battle with melanoma.
Dr. Panitch graduated from Wesleyan University and the New York University School of Medicine, and completed a residency in neurology at the University of California, San Francisco. He was appointed to professorships at the University of California and the University of Maryland School of Medicine and became internationally known for his pioneering work in the diagnosis and treatment of MS. In 2000, he moved to Vermont, where he founded and directed the Multiple Sclerosis Center at the University of Vermont. Dr. Panitch is survived by his companion and wife of 45 years, Adine Katzen Panitch; daughters Judy and Sharon, four grandchildren, and siblings Yetta, Deborah, and William Panitch. A memorial service was held in February.
Dr. Panitch was a historic figure in MS care and research, a quiet hero who contributed a great deal to the lives of all those affected by the disease. His family, friends, and colleagues will miss him terribly.


