Abstract
Multiple sclerosis (MS) burdens not only patients but also their informal or family caregivers. This study was conducted to identify characteristics of caregivers, caregiving, and MS patients receiving informal care that are associated with caregiving burden. Data were collected through a national survey of informal MS caregivers and analyzed using an ordered logistic regression model to identify factors associated with burden. Burden was found to be significantly greater among male caregivers than among female caregivers. Moreover, greater burden was associated with more frequent patient bladder dysfunction, more hours per week spent providing assistance, and greater restriction on the caregiver's ability to perform daily activities because of caregiving responsibilities. A strong association was found between the mental health status of the caregiver and burden. Health professionals should be sensitive to the impact of caregiving on the mental health of MS caregivers. The results of this study suggest that treating patient bladder dysfunction and facilitating respite care may reduce burden and improve the mental health of informal caregivers of people with MS. Future research should identify programs and services designed specifically to reduce burden experienced by male caregivers.
Multiple sclerosis (MS) is characterized by episodes of neurologic symptoms that are often followed by fixed neurologic deficits, increasing disability, and medical and physical decline over 30 to 40 years.1,2 The progress and severity of MS symptoms are unpredictable, however, varying widely among those affected.3–5 About 30% of people with MS require some form of supportive assistance at home, with 80% of such care provided by informal or unpaid caregivers, usually the patient's spouse.6–10 Informal caregivers provide a range of services to people with MS, including assistance with personal care, homemaking, mobility, and leisure activities.8,9,11,12 Assistance from informal caregivers enables people with MS to remain in their homes as their functional dependence and need for assistance with daily activities increase.13
Caregiver Burden and MS Care
One study found that more than 20% of informal caregivers assisting people with MS thought that this caregiving was burdensome either most (11%) or all (10%) of the time.10 Caregiver burden is a multidimensional reaction to a number of factors associated with providing daily assistance to the person with MS, including physical, psychological, emotional, and social stressors.14 A study of informal caregivers assisting people with MS in Spain found that emotional and vitality factors in the caregiver and disability level in the person with MS were major predictors of caregiving burden.15 Khan et al.16 found that caregiver burden was higher in those assisting people with more severe MS.
Another study concluded that psychiatric symptoms and cognitive impairment in the person with MS were significant contributors to caregiver distress.17 Forbes et al.18 found that MS disease impact and patient/caregiver health explained most of the variance in the burden of caregiving. Therapeutic strategies to reduce caregiver burden are needed to improve the health status and health-related quality of life (HRQOL) of informal caregivers as well as people with MS receiving their assistance.16,19 Early recognition of caregiving burden and identification of factors linked with this burden are important to determine appropriate interventions.14 Thus the objective of the present study was to identify factors associated with burden among caregivers assisting people with MS.
Methods
The data analyzed in this study were collected in a national survey of 530 people providing informal care to individuals with MS, with 430 caregivers providing all the data needed to implement our regression model. The sample of informal caregivers was developed by contacting people with MS who were participating in the North American Research Committee on Multiple Sclerosis (NARCOMS) Registry. The NARCOMS Registry was created in 1993 by the Consortium of Multiple Sclerosis Centers (CMSC); currently, more than 34,000 people with MS participate in routine data collection.20 It is estimated that up to 10% of Americans with MS are in the NARCOMS Registry.21 Registry participants are assured that their names will not be disclosed to anyone without the participant's written permission.
Our study focused on caregiving to more functionally impaired people with MS. Functional impairment is measured in the NARCOMS Registry using the Patient-Determined Disease Steps (PDDS) scale, a self-assessment of how well the person with MS walks, with scores ranging from 0 (normal) to 8 (bedridden).22 We included in our study only those Registry participants who needed a cane to walk 25 feet (score of 5), required bilateral support (score of 6), primarily used a wheelchair or scooter (score of 7), or were bedridden (score of 8).
Survey Process
We identified 4943 NARCOMS Registry participants with MS who met our impairment criteria to receive a recruitment letter requesting their assistance in identifying informal caregivers. The letter explained the purpose of the study, stating that we wanted to interview “the person who provides the majority of informal or unpaid care to you to help you cope with the effects of MS on your daily life.” The letter requested that the person with MS ask the person who provided the majority of their informal care to call a toll-free telephone number to complete a computer-assisted telephone interview administered by the Public Policy Research Institute (PPRI) at Texas A&M University. The caregiver survey received human subjects approval from the Office of Regulatory Compliance at Mississippi State University in June 2006 and by the Office of Research Compliance Institutional Review Board at Texas A&M University in July 2006. Mailing of recruitment letters began in September 2006, and the survey was halted in March 2007, when no caregivers called in for 2 weeks.
Calculation of a meaningful participation rate for the survey is difficult because we do not know how many people with MS receiving the recruitment letter had an informal caregiver. It is estimated that about 30% of people with MS require some form of home care assistance and that 80% of that assistance is provided by informal caregivers.6,7 Using those estimates, about 25% of people with MS receive home care assistance provided by an informal caregiver, or about 1235 of the 4943 people with MS who were sent recruitment letters. Given the study's focus on more functionally dependent people with MS, an estimate of 1235 informal caregivers may be low. Assuming 1235 informal caregivers, 530 completed interviews yields a participation rate of 43%.
Caregiver Interview Questionnaire
The caregiver survey was designed to record the caregiver's perceptions of the impact of MS on the person receiving their care, the care needs of the person with MS, informal care and services provided, and how assisting the person with MS affected the caregiver. The interview, which averaged about 30 minutes, asked about the caregiver's relationship with the person with MS; the patient's MS disease and symptom characteristics, cognitive decision making, and incontinence; and demographic information about the person with MS and the caregiver. The caregiver was asked to rate on a scale from 0 to 10 the extent to which MS symptoms affected the patient's independence in daily life, with 0 indicating no interference at all and 10 indicating the most severe interference.
The interviewer provided a list of statements designed to assess the caregiver's feelings and attitudes about assisting the person with MS, including “caregiving is burdensome.” Caregiver burden was measured using a 5-point Likert item, with possible responses of none of the time, once in a while, some of the time, most of the time, and all of the time. The caregiver was asked to report the average number of hours per week they spent helping the person with MS cope with the effects of their illness. The caregiver was also asked to rate on a scale from 0 to 10 the extent to which assisting the person with MS “affects your ability to perform activities in daily life that are important to you,” with 0 indicating no negative impact at all and 10 indicating the most severe impact. The caregiver was asked whether any paid caregiver was employed to help the patient perform activities necessary in day-to-day life.
The interview included the 8-item Short Form Health Status Survey (SF-8) to measure caregiver HRQOL.23,24 This instrument includes a Mental Component Summary (MCS). Higher scores on the SF-8 indicate better health status. Previous studies documented the validity of the SF-8 in the United States,24 and the instrument meets standard evaluation criteria for content, construct, and criterion-related validity.23 The MCS was included in our analysis as a measure of the mental health status of the caregiver.
Ordered Logistic Regression Model
An ordered logistic regression model using survey data was developed to analyze the contributions of characteristics of the person with MS and the caregiver to caregiver burden. The analyses included 430 caregivers in the regression model (caregivers who provided all data in their survey responses needed to implement the model). The dependent variable, measured with ordinal data, was the caregiver's assessment of the burden of providing assistance to the person with MS. Caregiver burden was measured using a 5-point Likert item, with possible responses of none of the time, once in a while, some of the time, most of the time, and all of the time.
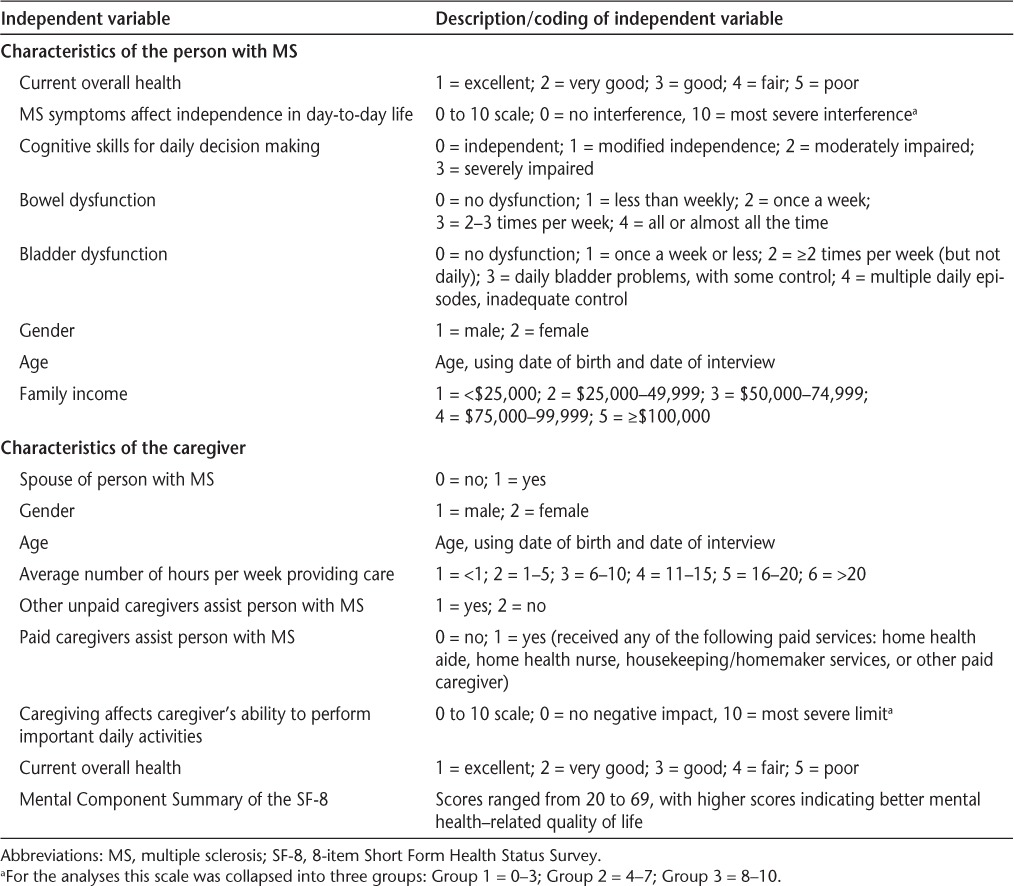
The model included 17 independent variables theorized to have predictive power in caregiver burden. These independent variables along with descriptions of how they were coded are presented in Table 1. The independent variables are other survey responses from the informal caregivers, including MS symptoms, demographic and overall health assessments of the person with MS and the caregiver, time spent providing informal care, the impact of providing assistance on the caregiver's day-to-day life, and the caregiver's SF-8 MCS. The model identified eight characteristics of the caregiver, caregiving, and the person with MS being assisted that were significantly associated with caregiver burden.
Table 1.
Independent variables used in analyses of burden among informal caregivers assisting people with MS
Results
Descriptive Characteristics
People with MS
Table 2 provides descriptive statistics for the people with MS included in our analyses. A large majority of people with MS in our study were female (64%). Their average age was 58.3 years, and most had 2006 family incomes below $50,000 per year (70%). Symptoms of MS interfered with independence in day-to-day life for most people with MS in our study, with nearly 95% experiencing at least moderate interference (a response of 4 or higher on the scale of 0 to 10). Large majorities of people with MS in our study had bowel and bladder dysfunction.
Table 2.
Characteristics of the person with MS

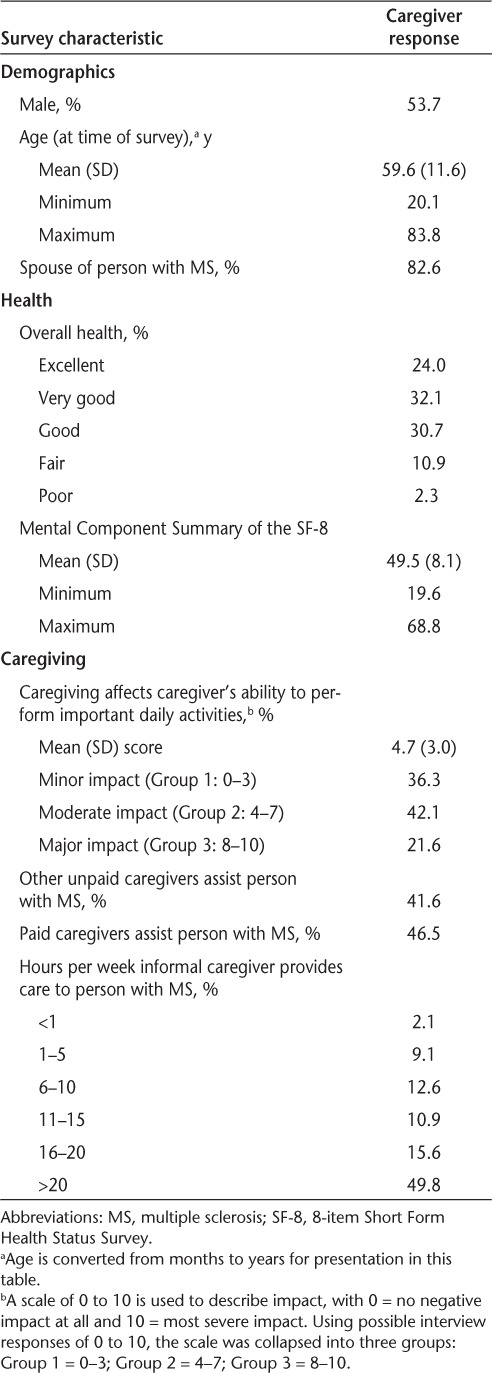
Caregivers
As shown in Table 3, 54% of informal caregivers in our study were male, the average age of the caregivers was 59.6 years, and about 83% were the spouse of the person with MS. Nonspousal caregivers included a child, parent, or neighbor/friend of the person with MS. About half of the caregivers said they provided more than 20 hours of assistance each week to the person with MS, while only about 11% said they provided 5 or fewer hours of informal care per week. About 64% of the caregivers replied that assisting the person with MS had at least a moderate impact on their ability to perform daily activities that were important to the caregiver (a response of 4 or higher on the scale of 0 to 10).
Table 3.
Characteristics of the caregiver
Ordered Logistic Regression
As Table 4 demonstrates, we identified three characteristics of the person with MS receiving informal care that were significantly associated with caregiver burden. First was worse overall health. A one-unit deterioration in reported overall health of the person with MS (eg, good health vs. fair health) increased the odds of the caregiver reporting higher levels of burden by 20.1%. A second characteristic was increased frequency of bladder dysfunction. Higher frequency of bladder dysfunction (eg, ≥ 2 times per week but not daily incontinence vs. daily bladder problems with some control) increased the odds of greater caregiver burden by 15.6%. Finally, gender of the person with MS was significantly associated with burden, with female gender reducing the odds of greater caregiver burden by 45.3%.
Table 4.
Factors associated with caregiver burden
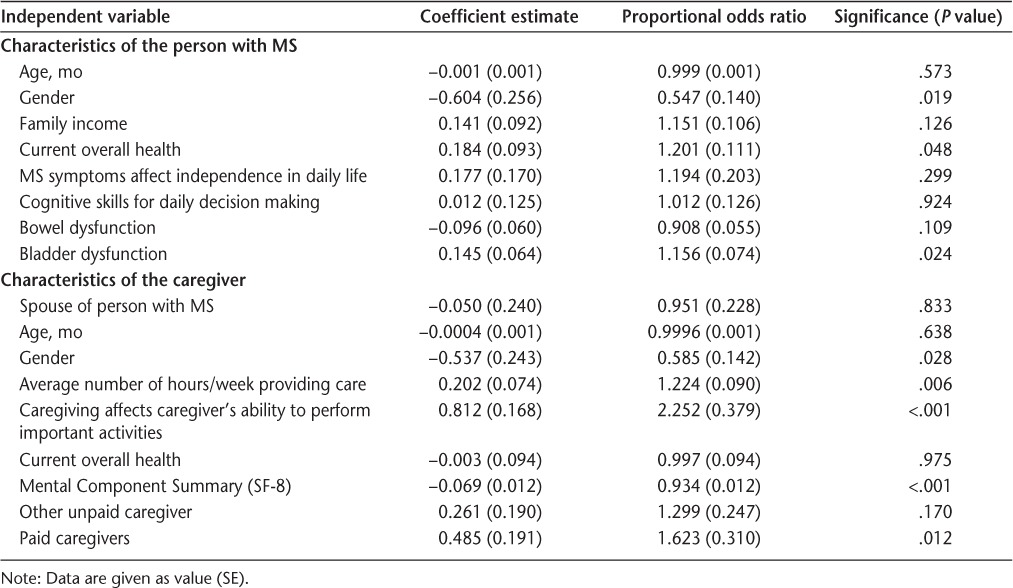
We identified five characteristics of the caregiver or caregiving that were significantly associated with burden. First was the gender of the caregiver: female caregivers had 41.5% lower odds of reporting greater burden. The average number of hours per week spent assisting the person with MS was also significantly linked to burden, with increased hours associated with greater burden. A one-unit increase in reported number of hours per week providing care (eg, an increase from 6–10 hours per week to 11–15 hours per week) increased the odds of the caregiver reporting higher levels of burden by 22.4%. Similarly, the more the caregiver perceived that assisting the person with MS limited their ability to perform important activities in their daily lives, the greater the level of burden reported. A one-unit increase in reported impact of caregiving on the ability of the caregiver to perform important daily activities (eg, moderate impact [Group 2] vs. major impact [Group 3]) increased the odds of the caregiver reporting higher levels of burden by 125%.
We found a significant association between the MCS of the SF-8 and burden, with higher scores for this mental health measure linked to lower levels of burden. A 1-point increase in the MCS reduced the odds of the caregiver reporting greater levels of burden by 6.6%. The use of a paid caregiver to help the person with MS perform activities of daily living increased the odds of informal caregivers reporting greater levels of burden by 62.3%.
Discussion
We identified a number of characteristics of the caregiver, caregiving, and the person with MS receiving care that were significantly associated with caregiver burden. Consistent with the findings of Forbes et al.,18 we found that worse overall health among people with MS was significantly associated with increased caregiver burden. However, in contrast to the findings of Forbes et al., we found that caregiver burden was significantly greater among men than among women. Future research is needed to identify programs and services specifically designed to reduce the burden experienced by male caregivers assisting people with MS. We also found that caregivers of either gender assisting males with MS experienced significantly greater burden. Informal caregivers reporting that a paid caregiver also assisted the person with MS had higher odds of reporting greater burden. The presence of a paid caregiver may be due to greater disability in the person with MS or a flare-up of MS symptoms leading to greater caregiver burden. Our findings indicate that treating bladder dysfunction among MS patients, providing access to respite care, and improving the mental health of caregivers would help reduce caregiver burden.
Bladder Dysfunction
Bladder dysfunction is among the most distressing and socially disabling problems associated with MS, affecting the quality of daily life and leading to social isolation.25–27 Consistent with our findings, Bosma et al.28 concluded that bladder dysfunction may increase the burden experienced by the partner or caregiver of the person with MS. However, bladder dysfunction can be prevented or symptomatically treated through various strategies, including pharmacologic therapies and behavioral approaches.25–31 Del Popolo et al.29 concluded that behavioral rehabilitation and conservative treatments for bladder dysfunction are sufficient for most MS patients, with innovations in neurourology improving urologic function and QOL for patients not responding to firstline treatments. Options for bladder management in MS care have improved, and more patients are receiving effective treatment, with bladder problems often treated at the same clinic providing neurologic care.31 Our findings indicate that reducing bladder dysfunction in people with MS could result in decreased caregiver burden.
Respite Care
We found that burden was significantly associated with the number of hours per week the caregiver provided assistance, as well as with restrictions on the caregiver's ability to perform important daily activities due to caregiving responsibilities. Previous studies found that caregivers experienced high levels of stress and substantial burden, with risk of “burnout” a possibility for those without support.32,33 Respite services provide caregivers with temporary relief and the opportunity to pursue important activities, which may reduce their perceived burden.34,35 Respite services include adult day care, inhome respite, institutional respite, and host respite (in which the care recipient stays in the home of the service provider for short periods).32
A previous study found that only small proportions of informal caregivers assisting people with MS reported the use of respite services, such as at-home respite care (5.3% of caregivers), adult day care (3.6%), or inpatient respite care (1.5%).12 That study also found that many informal caregivers not using respite care thought these services were needed, such as at-home respite care (29% of caregivers), inpatient respite care (16%), or adult day care (15%). A study of Dutch informal caregivers found that more than one-third needed but did not ask for respite care,33 indicating a need to educate caregivers about the availability and benefits of respite care.
Mental Health
This study identified a strong and significant relationship between caregiver burden and mental health dimensions of the caregiver's HRQOL. A previous study of informal caregivers assisting people with MS found that about one in four caregivers reported the need for treatment from a mental health professional in the previous 12 months, but only one-third of caregivers reporting the need for counseling sought this care.10 Providing informal care to a person with MS can have a negative impact on the caregiver's psychological wellbeing. 13,16,17,36 Pozzilli et al.19 observed that depression in caregivers was linked to the physical, emotional, and health status of the people with MS receiving assistance, concluding that informal caregivers would benefit from access to independent and targeted therapies. A study of informal caregivers assisting people with Alzheimer's disease found that higher burden led to greater feelings of depression among caregivers.37
Interventions and therapeutic strategies to reduce caregiver burden are needed to improve the health status and HRQOL of caregivers and people with MS receiving their assistance.16,19 Early recognition of caregiver burden and identification of factors linked with this burden are important to determine appropriate interventions. 14 Health professionals should be sensitive to the impact of caregiving on the mental health dimensions of HRQOL experienced by caregivers. As advocated by Patti et al.,38 informal caregivers assisting people with MS should be referred to supportive programs that may benefit them.
Study Limitations
The survey sample of informal caregivers in this study was developed by contacting people with MS who participated in the NARCOMS Registry. Such participation is voluntary; thus the Registry membership is not a random sample of people with MS, resulting in possible selection bias. However, the Registry population is large, accounting for an estimated 10% of the MS population in the United States.22 In addition, Registry participants have age at onset of MS symptoms and demographic characteristics comparable to those of people with MS in the National Health Interview Survey and the Slifka Study (a representative national sample of people with MS).22,39,40 Another possible limitation of our study is its reliance on caregivers' perceptions of the dependency and care needs of the people with MS, as well as the care provided. A previous study found that caregivers reported providing more frequent care and for a longer duration than people with MS reported receiving.8
Conclusion
The results of this study indicate that treating bladder dysfunction of MS patients and providing access to respite care could reduce the burden of informal caregivers, improving their mental health. Future research is needed to identify programs and services specifically designed to reduce the burden experienced by male caregivers. Given the strong association of burden and the MCS of the SF-8, our findings highlight the importance of addressing the mental health needs of informal caregivers assisting people with MS.
PracticePoints.
Caregiver burden in MS is significantly associated with the number of hours per week spent providing assistance, the extent to which caregiving responsibilities restrict the caregiver's ability to perform important daily activities, and the frequency of bladder dysfunction in the person receiving assistance.
Caregiver burden is also strongly and significantly related to mental health dimensions of the caregiver's health-related quality of life.
Improved control of bladder dysfunction among MS patients may help reduce caregiver burden.
Our findings highlight the importance of addressing the mental health needs of informal caregivers assisting people with MS.
Acknowledgments
The authors thank Dr. Nicholas LaRocca, Director of the Health Care Delivery and Policy Research Program of the National Multiple Sclerosis Society (NMSS), for his assistance with this research. The Lone Star Chapter of the NMSS recruited volunteers to pretest the caregiver survey questionnaire. The Central New England Chapter and the Ozark Branch of the Mid America Chapter of the NMSS recruited volunteers to participate in focus groups for this study. In addition, the authors are grateful to the people with MS who identified their caregivers and the caregivers who participated in the focus groups, the pretest of the survey questionnaire, and the telephone interviews. Without their cooperation and input, this study could not have been completed.
Footnotes
Funding/Support: This research was supported by a contract from the Health Care Delivery and Policy Research Program of the NMSS (HC 0043).
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Lublin F, Reingold S. Defining the clinical course of multiple sclerosis: results of an international survey. Neurology. 1996;46:907–911. doi: 10.1212/wnl.46.4.907. [DOI] [PubMed] [Google Scholar]
- 2.Rudick R, Cohen J, Weinstock-Guttman B, Kinkel R, Ransohoff R. Drug therapy: management of multiple sclerosis. N Engl J Med. 1997;337:1604–1611. doi: 10.1056/NEJM199711273372207. [DOI] [PubMed] [Google Scholar]
- 3.National Multiple Sclerosis Society. What is multiple sclerosis? http://www.nationalmssociety.org/about-multiple-sclerosis/what-we-know-about-ms/what-is-ms/index.aspx. Published 2008. Accessed September 5, 2010.
- 4.Somerset M, Sharp D, Campbell R. Multiple sclerosis and quality of life: a qualitative investigation. J Health Serv Res Policy. 2002;7:151–159. doi: 10.1258/135581902760082454. [DOI] [PubMed] [Google Scholar]
- 5.Thompson AJ, Hobart JC. Multiple sclerosis: assessment of disability and disability status. J Neurol. 1998;245:189–196. doi: 10.1007/s004150050204. [DOI] [PubMed] [Google Scholar]
- 6.Minden SL, Frankel D, Hadden LS, Srinath KP, Perloff JN. Disability in elderly people with multiple sclerosis: an analysis of baseline data from the Sonya Slifka Longitudinal Multiple Sclerosis Study. NeuroRehabilitation. 2004;19:55–67. [PubMed] [Google Scholar]
- 7.National Multiple Sclerosis Society. Sonya Slifka Longitudinal Study renewed. NMSS Research Highlights. Winter-Spring. 2007. http://www.nationalmssociety.org/download.aspx?id=77. Accessed September 5, 2010.
- 8.Aronson KJ, Cleghorn G, Goldenberg E. Assistance arrangements and use of services among persons with multiple sclerosis and their caregivers. Disabil Rehabil. 1996;18:354–361. doi: 10.3109/09638289609165894. [DOI] [PubMed] [Google Scholar]
- 9.Carton H, Loos R, Pacolet J, Versieck K, Vlietinck R. A quantitative study of unpaid caregiving in multiple sclerosis. Mult Scler. 2000;6:274–279. doi: 10.1177/135245850000600409. [DOI] [PubMed] [Google Scholar]
- 10.Buchanan RJ, Radin D, Chakravorty B, Tyry T. Informal care giving to more disabled people with multiple sclerosis. Disabil Rehabil. 2009;31:1244–1256. doi: 10.1080/09638280802532779. [DOI] [PubMed] [Google Scholar]
- 11.O'Hara L, DeSouza L, Ide L. The nature of care giving in a community sample of people with multiple sclerosis. Disabil Rehabil. 2004;26:1401–1410. doi: 10.1080/09638280400007802. [DOI] [PubMed] [Google Scholar]
- 12.Buchanan RJ, Radin D, Chakravorty B, Tyry T. Perceptions of informal care givers: health and support services provided to people with multiple sclerosis. Disabil Rehabil. 2010;32:500–510. doi: 10.3109/09638280903171485. [DOI] [PubMed] [Google Scholar]
- 13.McKeown LP, Porter-Armstrong AP, Baxter GD. The needs and experiences of caregivers of individuals with multiple sclerosis: a systematic review. Clin Rehabil. 2003;17:234–248. doi: 10.1191/0269215503cr618oa. [DOI] [PubMed] [Google Scholar]
- 14.Buhse M. Assessment of caregiver burden in families of persons with multiple sclerosis. J Neurosci Nurs. 2008;40:25–31. doi: 10.1097/01376517-200802000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Rivera-Navarro J, Benito-Leon J, Oreja-Guevara C, et al. Burden and health-related quality of life of Spanish caregivers of persons with multiple sclerosis. Mult Scler. 2009;15:1347–1355. doi: 10.1177/1352458509345917. [DOI] [PubMed] [Google Scholar]
- 16.Khan F, Pallant J, Brand C. Caregiver strain and factors associated with caregiver self-efficacy and quality of life in a community cohort with multiple sclerosis. Disabil Rehabil. 2007;29:1241–1250. doi: 10.1080/01443610600964141. [DOI] [PubMed] [Google Scholar]
- 17.Figved N, Myhr KM, Larsen JP, Aarsland D. Caregiver burden in multiple sclerosis: the impact of neuropsychiatric symptoms. J Neurol Neurosurg Psychiatry. 2007;78:1097–1102. doi: 10.1136/jnnp.2006.104216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forbes A, While A, Mathes L. Informal carer activities, carer burden and health status in multiple sclerosis. Clin Rehabil. 2007;21:563–575. doi: 10.1177/0269215507075035. [DOI] [PubMed] [Google Scholar]
- 19.Pozzilli C, Palmisano L, Mainero C, et al. Relationship between emotional distress in caregivers and health status in persons with multiple sclerosis. Mult Scler. 2004;10:442–446. doi: 10.1191/1352458504ms1046oa. [DOI] [PubMed] [Google Scholar]
- 20.North American Research Committee on Multiple Sclerosis (NAR-COMS) Project. Information: About NARCOMS. http://narcoms.org/about. Accessed September 5, 2010.
- 21.Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Volmer T. Comorbidity, socioeconomic status and multiple sclerosis. Mult Scler. 2008;14:1091–1098. doi: 10.1177/1352458508092263. [DOI] [PubMed] [Google Scholar]
- 22.Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Volmer T. Comorbidity delays diagnosis and increases disability at diagnosis in MS. Neurology. 2009;72:117–124. doi: 10.1212/01.wnl.0000333252.78173.5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turner-Bowker DM, Bayliss MS, Ware JE, Kosinski M. Usefulness of the SF-8 Health Survey for comparing the impact of migraine and other conditions. Qual Life Res. 2003;12:1003–1012. doi: 10.1023/a:1026179517081. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Kosinski M, Dewey JE, Gandek B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8TM Health Survey. Lincoln, RI: QualityMetric Inc; 2001. [Google Scholar]
- 25.DasGupta R, Fowler CJ. Bladder, bowel, and sexual dysfunction in multiple sclerosis: management strategies. Drugs. 2003;63:153–166. doi: 10.2165/00003495-200363020-00003. [DOI] [PubMed] [Google Scholar]
- 26.Nortvedt MW, Riise T, Frugard J, et al. Prevalence of bladder, bowel, and sexual problems among multiple sclerosis patients two to five years after diagnosis. Mult Scler. 2007;13:106–112. doi: 10.1177/1352458506071210. [DOI] [PubMed] [Google Scholar]
- 27.De Ridder D, Ost D, Van der Aa F, et al. Conservative bladder management in advanced multiple sclerosis. Mult Scler. 2005;11:694–699. doi: 10.1191/1352458505ms1237oa. [DOI] [PubMed] [Google Scholar]
- 28.Bosma R, Wynia K, Havlikova E, De Keyser J, Middel B. Efficacy of desmopressin in patients with multiple sclerosis suffering from bladder dysfunction: a meta-analysis. Acta Neurol Scand. 2005;112:1–5. doi: 10.1111/j.1600-0404.2005.00431.x. [DOI] [PubMed] [Google Scholar]
- 29.Del Popolo G, Panariello G, Del Corso F, De Scisciolo G, Lombardi G. Diagnosis and therapy for neurogenic bladder dysfunctions in multiple sclerosis patients. Neurol Sci. 2008;29:S352–S355. doi: 10.1007/s10072-008-1042-y. [DOI] [PubMed] [Google Scholar]
- 30.Haslam C. Management options for bladder dysfunction in patients with multiple sclerosis. Nurs Times. 2009;105:24–27. [PubMed] [Google Scholar]
- 31.Kalsi V, Fowler CJ. Therapy insight: bladder dysfunction associated with multiple sclerosis. Nat Clin Pract Urol. 2005;2:492–501. doi: 10.1038/ncpuro0323. [DOI] [PubMed] [Google Scholar]
- 32.Mason A, Weatherly H, Spilsbury K, et al. The effectiveness and cost-effectiveness of respite for caregivers of frail older people. J Am Geriatr Soc. 2007;55:290–297. doi: 10.1111/j.1532-5415.2006.01037.x. [DOI] [PubMed] [Google Scholar]
- 33.van Exel J, de Graaf G, Brouwer W. Give me a break! Informal care-giver attitudes towards respite care. Health Policy. 2008;88:73–87. doi: 10.1016/j.healthpol.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 34.Whitlach CJ, Feinberg LF. Family and friends as respite providers. J Aging Soc Policy. 2006;18:127–139. doi: 10.1300/J031v18n03_09. [DOI] [PubMed] [Google Scholar]
- 35.Dal Santo TS, Scharlach AE, Nielsen J, Fox PJ. A stress process model of family caregiver service utilization: factors associated with respite and counseling service use. J Gerontolog Soc Work. 2007;49:29–49. doi: 10.1300/J083v49n04_03. [DOI] [PubMed] [Google Scholar]
- 36.Knight RG, Devereux RC, Godfrey HP. Psychosocial consequences of caring for a spouse with multiple sclerosis. J Clin Exp Neuropsychol. 1997;19:7–19. doi: 10.1080/01688639708403832. [DOI] [PubMed] [Google Scholar]
- 37.Clyburn LD, Stones MJ, Hadjistravropoulos T, Tuokko H. Predicting caregiver burden and depression in Alzheimer's disease. J Gerontol: Soc Sci. 2000;55B:S2–S13. doi: 10.1093/geronb/55.1.s2. [DOI] [PubMed] [Google Scholar]
- 38.Patti F, Amato MP, Battaglia MA, et al. Caregiver quality of life in multiple sclerosis: a multicentre Italian study. Mult Scler. 2007;13:412–419. doi: 10.1177/1352458506070707. [DOI] [PubMed] [Google Scholar]
- 39.Marrie RA, Hadjimichael O, Vollmer T. Predictors of alternative medicine use by multiple sclerosis patients. Mult Scler. 2003;9:461–466. doi: 10.1191/1352458503ms953oa. [DOI] [PubMed] [Google Scholar]
- 40.Minden SL, Frankel D, Hadden L, et al. The Sonya Slifka Longitudinal Multiple Sclerosis Study: methods and sample characteristics. Mult Scler. 2006;12:24–38. doi: 10.1191/135248506ms1262oa. [DOI] [PubMed] [Google Scholar]


