Abstract
Cognitive dysfunction is observed in about half of people with multiple sclerosis (MS), and MS health-care professionals face the challenge of screening, assessing, and treating patients for cognitive problems. Considering the inconsistent or limited empirical evidence to assist in this task, a multidisciplinary consensus conference of MS experts, sponsored by the Consortium of Multiple Sclerosis Centers (CMSC), was held on September 24, 2010, to address these issues. Key articles from the literature on these topics were distributed prior to the meeting, and CMSC member professionals were surveyed on clinical practices related to screening, assessment, and treatment for cognitive problems. The purpose of the meeting was threefold: 1) to achieve a multidisciplinary perspective on practices for screening, monitoring, evaluating, and treating MS patients for cognitive problems; 2) to propose consensus candidate measures for screening and/or monitoring for cognitive problems in MS that neurologists or nurses might administer on a regular basis; and 3) to propose consensus treatment approaches from a multidisciplinary perspective. This article summarizes the conclusions of the conference participants and provides preliminary suggestions for screening and brief assessment.
Multiple sclerosis (MS) is an immune-mediated demyelinating disease of unknown etiology in which there is a T cell–mediated attack on oligodendrocyte and myelin epitopes in the central nervous system (CNS). As a result, MS patients may have localized areas of demyelination in the CNS, as well as damage to or loss of proximal gray matter. The symptoms of MS run a wide gamut, depending on the location of the lesions. One category of symptoms affecting a large portion of the MS population is cognitive dysfunction, with estimated rates ranging from 43% to 70%.1,2 Cognitive dysfunction in MS spans the domains of visuospatial processing, information processing speed, working memory, executive functioning, verbal and visual learning, and episodic memory.
Symptoms of cognitive dysfunction can appear early, even before patients have reached the full criteria for MS.3 Even with mild cognitive impairment, patients can have significant functional disability.4 Cognitive dysfunction can interfere broadly with patients' lives, causing a decrease in quality of life,2 impairments in social functioning,5 and problems with employment.6 Thus, it is necessary to develop widely used screening tools, assessments, and interventions that have demonstrated reliability and validity. However, existing literature on the reliability and validity of screening tools and treatments is scarce or problematic, although the reliability and validity of more comprehensive assessment batteries has been well demonstrated.7 Although adequate assessment procedures exist, cognitive functioning is not routinely assessed.8 One obstacle mentioned in the literature to widespread cognitive assessment in MS patients is the cost and time involved in the testing.9 However, given the prevalence of cognitive impairment in MS and its consequences for patients and their families, its proper assessment and treatment is essential.
Because of the aforementioned limitations in screening, assessment, and treatment for cognitive dysfunction in MS, a multidisciplinary consensus conference of MS experts was planned by the Consortium of Multiple Sclerosis Centers (CMSC). The purpose of the meeting was threefold: 1) to achieve a multidisciplinary perspective on practices for screening, monitoring, evaluating, and treating MS patients for cognitive problems; 2) based on a review of the empirical literature, to propose consensus candidate measures for screening and/or monitoring for cognitive problems in MS that neurologists or nurses might administer on a regular basis; and 3) to propose consensus treatment approaches from a multidisciplinary perspective.
Methods
Selection of Consensus Conference Participants
Seventeen experts in MS from various disciplines were approached and agreed to participate in the conference: three neuropsychologists, one clinical psychologist, six neurologists, one neuropsychiatrist, one physiatrist, one nurse, two nurse practitioners, one occupational therapist, and one speech pathologist. Candidates were selected by the conference co-chairs, members of the CMSC Executive Committee, and the CMSC Executive Director. The selection criteria included the following: expertise in MS, representation of the major disciplines that provide care for MS patients, and knowledge about cognition and MS. Before the meeting, a thorough literature review was conducted by the conference chair with assistance from other committee members. Fifty key peer-reviewed articles related to cognition and MS, screening and assessment for cognitive problems in MS, and treatment of cognitive problems were identified and distributed to all committee members for review prior to the meeting.
Preliminary Survey of CMSC Professionals and Data from NARCOMS Registry Patients
To provide additional information to the consensus committee members, two sources of data on the topic of cognition and MS were used. First, a survey of CMSC member health-care providers was developed by the conference co-chairs and e-mailed to each CMSC member center. A total of 252 health-care providers were e-mailed a questionnaire in which they were asked about their practice patterns regarding screening, assessment, and treatment for cognitive dysfunction in MS. A total of 207 members completed and returned the survey, for a response rate of 82%. Demographic information was collected regarding the type of practice respondents had, the percentage of MS patients in their practice, and their MS patients' access to neuropsychologists. In addition, respondents were asked about their assessment procedures and the treatments they prescribe for MS patients with cognitive dysfunction.
In addition to the survey of CMSC health-care providers, archived data on patients' perceptions on cognition as indicated in the fall 2004 survey of the North American Research Committee on Multiple Sclerosis (NARCOMS) were retrieved.
Results of Preliminary Surveys
Demographics of Health-Care Providers
Of the 207 respondents to the survey of health-care providers, 28% (n = 58) were registered nurses or another type of nurse other than a nurse practitioner, 23% (n = 47) were neurologists, 12% (n = 25) were nurse practitioners, 6% (n = 13) were neuropsychologists, 6% (n = 12) were physical therapists, 5% (n = 11) were occupational therapists, 2% (n = 4) were psychologists, and less than 1% (n = 1) were speech therapists. Thirteen percent (n = 26) responded as “other,” and 5% (n = 10) did not provide a discipline.
Regarding respondents' practices, 50% (n = 103) saw mostly MS patients, while 24% (n = 50) reported that about half of their patients had MS, 20% (n = 42) reported that less than half had MS, and 6% (n = 12) said that less than 25% had MS. Seventy percent (n = 144) of the practices are hospital-based, 21% (n = 43) are community-based, 5% (n = 11) of respondents did not provide a response, and 4% (n = 9) listed their practice as “other.” Most of the practices, 70% (n = 144), participate in MS clinical trials. Twenty-one percent (n = 43) of the practices do not participate, 5% (n = 11) of the respondents did not provide an answer, and 4% (n = 9) responded that they did not know.
The vast majority of respondents at 82% (n = 169) have access to neuropsychologists knowledgeable about MS at their practice, while 12% (n = 24) do not and 7% (n = 14) did not provide a response.
CMSC Health-Care Professionals' Perspectives on Screening and Assessment for Cognitive Dysfunction in MS
Approximately 49% of respondents (n = 133) reported having no formal procedure for screening patients for cognitive impairment but said that they were very attuned to symptoms and signs of cognitive impairment and routinely assess and query patients about it. For 21% (n = 58) of respondents, cognitive performance tests such as the Paced Auditory Serial Addition Test (PASAT) and/or Symbol Digit Modalities Test (SDMT) were used as screening instruments at their practice sites. Self-report instruments, including the Multiple Sclerosis Neuropsychological Screening Questionnaire (MSNQ), are used by 12% (n = 32) of respondents for screening. For 8% (n = 23) of respondents, cognitive performance tests administered by a computer are used to screen for cognitive problems in MS patients. Seven percent (n = 19) of respondents use informant-report instruments such as the MSNQ. For 3% (n = 9) of respondents, there is no formal procedure and little specific attention to cognitive problems by clinicians.
Respondents were asked about the frequency of cognitive impairments among MS patients in their practices. Although 62% (n = 129) responded that they could estimate the frequency of cognitive problems, more (n = 152) completed the estimate questions. About 21% (n = 43) responded that they did not know the frequency and could not estimate it, and 17% (n = 35) gave no answer. Of those who could provide an estimate, 69 respondents indicated that between 40% and 60% of their patients had cognitive problems, 33 respondents indicated between 61% and 80%, 33 respondents indicated between 21% and 40%, 8 respondents indicated between 81% and 90%, 6 respondents indicated between 11% and 20%, and 3 respondents indicated between 1% and 10%.
When the respondents were asked about referring patients they suspect of having cognitive impairments for formal assessment, such as neuropsychological or speech/language evaluations, 62% (n = 129) responded that they could provide a clear estimate of how many patients they refer (although more [n = 138] answered some of the subsequent questions), 21% (n = 43) responded that they could not, and 17% (n = 35) gave no answer. Of those practitioners who provided estimates, 36 said that between 21% and 40% of the patients were referred for further testing, 35 said between 1% and 10%, 26 said between 41% and 60%, 17 said between 61% and 80%, 15 said between 11% and 20%, 5 said between 91% and 100%, and 4 said between 81% and 90%.
When suspecting that an MS patient has cognitive impairment, 43% (n = 90) responded that they would refer the patient to an in-house neuropsychologist or psychologist, and 16% (n = 33) responded that they would refer the patient to an outside neuropsychologist or psychologist. Sixteen percent (n = 33) responded that they would refer the patient to another professional, such as a psychiatrist, an occupational therapist, or a speech therapist. Twelve percent (n = 24) responded that they would address the cognitive impairment with in-house medical, nursing, or other medical staff, and the remaining 13% (n = 27) did not provide an answer.
Health-care professionals who refer their patients for neuropsychological testing were asked about different aspects of working with a neuropsychologist and responded with the ratings of “excellent,” “good,” “fair,” and “poor.” When asked about the time it takes to get an appointment, 40% (n = 65) said the time it takes was good, 33% (n = 54) said it was fair, 14% (n = 23) said it was excellent, and 13% (n = 21) said it was poor. Regarding the time it takes to get a report, 49% (n = 80) said the time it takes was good, 23% (n = 38) said it was fair, 22% (n = 35) said it was excellent, and 6% (n = 10) said it was poor. Forty-five percent (n = 73) said the clarity and readability of the report were excellent, 44% (n = 72) said they were good, 10% (n = 16) said they were fair, and 1% (n = 1) said they were poor. Regarding the quality of the neuropsychologist's recommendations, 41% (n = 66) said they were good, 41% (n = 66) said they were excellent, 17% (n = 27) said they were fair, and 2% (n = 4) said they were poor. When asked about the neuropsychologist's certifications, 76% (n = 123) reported that the neuropsychologists they refer to are board certified, 22% (n = 36) responded that they did not know, and 4% (n = 6) reported that they are not board certified. Seventy-seven percent (n = 125) of the respondents said that the neuropsychologists they refer to have an expertise in MS, 17% (n = 28) responded that they did not know, and 7% (n = 11) responded that the neuropsychologists did not have expertise in MS.
One of the major limitations of the MS health-care provider survey was that all of those surveyed were members of the CMSC. Most were hospital-based practices that specialized in MS, and most respondents participated in MS clinical trials. The generalizability of these practice patterns to the general neurologic community, where most MS patients receive care, is unknown.
Patients' Perceptions of Cognitive Dysfunction in MS—NARCOMS Data
The information on the MS patients' perceptions of their cognitive status was taken from a NARCOMS survey conducted in the fall of 2004 (N = 9083). The NARCOMS responders were asked five questions about their cognitive abilities. Patients rated their organization, concentration, orientation, recent memory, and thinking on a scale of “never” to “almost always.” Table 1 shows patients' responses to the questions.
Table 1.
NARCOMS fall 2004 survey responses from patients with MS regarding cognitive problems (N = 9083)
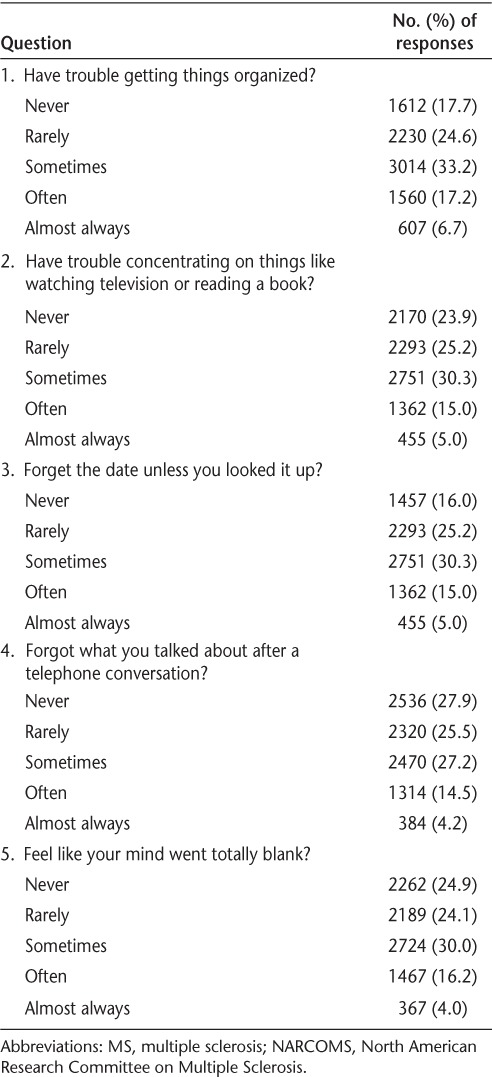
Overall, about 30% of patients responded that they experienced cognitive problems “sometimes,” about 15% experienced them “often,” and between 4% and 5% reported that they experienced them “almost always.” Sixteen to 28% never experienced the listed cognitive problems, and about 25% experienced them rarely.
Treatment of Cognitive Dysfunction in MS—Health-Care Professionals' Survey
If cognitive problems are detected, 58% of professionals (n = 121) said that they would prescribe medication, while 27% (n = 55) said they would not and 15% (n = 31) did not respond. Of the respondents who said they would prescribe medication, 83% (n = 101) responded that they would give a cholinesterase inhibitor, such as donepezil; 82% (n = 100) responded that they would give an antifatigue agent, such as modafinil; 56% (n = 68) responded that they would give a stimulant, such as methylphenidate; 52% (n = 63) responded that they would give a glutamate modifier, such as memantine; 52% (n = 63) responded that they would give a dopamine agonist antidepressant, such as bupropion; and 12% (n = 15) responded that they would give another medication that was not listed. For those who would (n = 121) or would not (n = 55) prescribe medication (total n = 176), 31% (n = 55) said they would recommend cognitive remediation, 20% (n = 35) said they would refer to another professional, and 7% (n = 12) said they would recommend another treatment that was not listed.
Consensus Conference Procedures
As mentioned, a thorough literature review helped identify 50 key empirical articles on screening, monitoring, assessment, and treatment for cognitive dysfunction, which were distributed to participants well ahead of the conference. The meeting was held on September 24, 2010, in Washington, DC. Keynote presentations were prepared on the above-mentioned topics by expert participants, and the results of the surveys were presented. Then, participants were divided into groups that independently identified recommendations/conclusions on the relevant topic (screening, monitoring, assessing, treating for cognitive impairments). An overall discussion followed each presentation, and consensus statements were summarized and presented to the entire group for final comment.
Results of the Consensus Conference: Conclusions of the Participants
The committee concluded that there is ample evidence in the peer-reviewed literature that neuropsychological testing detects cognitive impairments in MS in a highly reliable and valid fashion. Both the Rao Brief Repeatable Neuropsychological Battery (BRNB)10,11 and the Minimal Assessment of Cognitive Function in MS (MACFIMS)8 were cited as demonstrating excellent reliability and validity. The BRNB includes tests that assess verbal and visual learning and memory, processing speed/working memory, and verbal fluency. In addition to these domains, the MACFIMS assesses visual perception/spatial processing and executive function.
The experts concluded that much less is known about the reliability, validity, sensitivity, and specificity of brief measures for screening and monitoring purposes. The function of screening, and its utility related to monitoring and assessment, is illustrated in Figure 1. Given the varying domains of possible cognitive impairments in MS, there is insufficient current evidence to suggest that it is feasible to screen or monitor for all possible cognitive impairments in MS, especially since there is evidence of focal (nongeneralized) deficits. The committee concluded that candidate measures for limited screening or monitoring include the SDMT and MSNQ-informant version, although they both have limitations and, for the MSNQ, co-evaluating depression is important. Brief screens of memory frequently given during a neurologic examination such as the Mini-Mental State Exam or asking patients to remember three words or objects are inadequate in MS.
Figure 1.
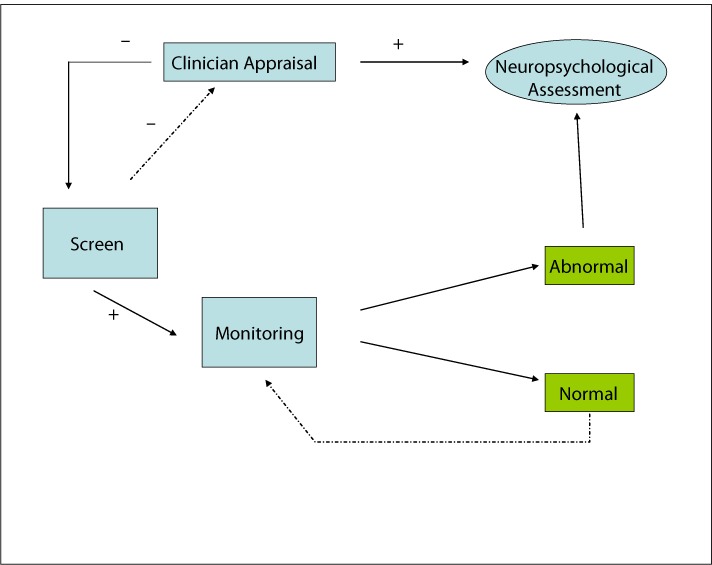
Utility of screening and its relation to clinician appraisal, monitoring, and neuropsychological assessment
Some MS neurologists are routinely utilizing computerized cognitive tests to monitor patients over time, although more work on the reliability, validity, sensitivity, and specificity of computerized testing needs to be done.
Routine monitoring of cognitive function was viewed by the committee as important, similar to routine monitoring of neurologic status. However, significant problems were cited regarding routine monitoring of patients with candidate tests, such as the SDMT. Although the SDMT is considered by the committee to be the best candidate measure at present because of its sensitivity, more research is necessary to determine what incremental changes are required on the SDMT or other tests to enable them to be used regularly to monitor cognition in patients.
Measures of verbal learning and memory that are reliable and valid in MS are too time-consuming to be used for screening during a regular neurologic examination, and shorter tests must be developed. Preliminary evidence suggests that the California Verbal Learning Test–II (CVLT-II) can be shortened to two administrations of the 16-item word list, which seems to capture most of the variance (96%) in total learning.12
Regarding treatment for cognitive dysfunction, there is little or no empirical evidence that pharmacologic approaches can manage or improve symptoms. Initially there were encouraging data showing that l-amphetamine13 and donepezil14 can be effective for improving processing speed and memory defects, respectively.15,16 Unfortunately, these studies were not replicated in subsequent research. Despite the lack of evidence, 58% of MS health-care providers in the survey indicated that they prescribe a variety of medications to improve cognitive symptoms in MS.
The committee members agreed that there is some preliminary evidence that secondary outcomes or sub-studies from clinical trials of disease-modifying therapies (DMTs) indicate that DMTs may slow cognitive deterioration, although the findings are inconsistent, the studies generally underpowered, and the designs not optimal to detect cognitive changes.
A number of experimental studies suggest that cognitive improvement via rehabilitation is feasible. For example, several studies have shown that employing self-generated learning techniques, where patients generate the right answer, as opposed to being told what to remember, can significantly improve recall of everyday functional activity such as remembering names and appointments, and tasks such as financial management and meal preparation.17,18 Another technique called “spaced learning,” in which opportunities to learn new information are spread across time rather than repeated consecutively, has also resulted in significant improvement in everyday functional performance. Utilizing both self-generation and spaced learning simultaneously resulted in almost 50% greater recall than either technique alone.18 Another technique called the “testing effect” (also called retrieval practice) can significantly improve learning and memory.19 In this study, simply testing subjects on material previously learned resulted in their recalling about twice as much information as being given an additional opportunity to learn the material.
However, results of these experimental studies need to be translated into clinical trials and tested. Chiaravalloti et al.20 used a double-blind, placebo-controlled, randomized clinical trial to show that training in the use of context and imagery to improve the strength of encoding results in significantly improved recall on cognitive testing as well as self-report of everyday activities.20
PracticePoints.
Many MS patients who have cognitive deficits are not screened or assessed for these problems.
The Symbol Digit Modalities Test is probably the best candidate measure for regular screening of MS patients for potential cognitive problems, but it is limited in scope and does not assess many cognitive problems that MS patients may manifest, such as those related to episodic memory.
Although the literature on the treatment of cognitive problems is sparse, some promise is being shown by experimental studies on cognitive rehabilitation, especially those that focus on enhancing memory.
Acknowledgments
We are grateful to Tuula Tyry for providing the archived NARCOMS data.
Footnotes
Consensus Conference Participants: Frederick W. Foley, PhD (Chair), Ralph H. Benedict, PhD (Co-chair), Patricia Bednarik, MS, Christopher Bever, MD, Julie Bobholtz, PhD, John DeLuca, PhD, Anthony Feinstein, MD, PhD, Mark Freedman, MD, Mark Gudesblatt, MD, Colleen Harris, MN, NP, Steve Kamin, MD, George Kraft, MD, Marie Namey, MSN, Anthony Reder, MD, Amy Perrin Ross, APN, MSN, Christine Smith, OTR/L, MSCS, Lael Stone, MD.
Financial Disclosures: Dr. Foley has served on speakers' bureaus for Bayer, Biogen, and Teva Neuroscience; has served on advisory boards or as a consultant for Bayer and Biogen; and has received an independent investigator grant from Bayer. Dr. Benedict has served on speakers' bureaus for Bayer and Serono; has served on advisory boards for Bayer, Biogen, and Novartis; and has received research grants from Acorda, Biogen, and Shire Pharmaceutical. Dr. DeLuca has served on advisory boards for Biogen and Memen Pharmaceutical and has received research grants from Biogen and Memen Pharmaceutical. Ms. Gromisch has no potential conflicts of interest to disclose.
Funding/Support: This conference was supported through Foundation of the Consortium of Multiple Sclerosis Centers grants from Bayer HealthCare Pharmaceuticals, Teva Neuroscience, and Genentech. Dr. DeLuca received grant funding from the National Multiple Sclerosis Society (MB003, RG3935a2/2) and the National Institute on Disability and Rehabilitation Research (H133a070037).
References
- 1.Peyser JM, Rao SM, LaRocca NG, Kaplan E. Guidelines for neuropsychological research in multiple sclerosis. Arch Neurol. 1990;47:94–97. doi: 10.1001/archneur.1990.00530010120030. [DOI] [PubMed] [Google Scholar]
- 2.Rao SM, Leo GJ, Bernadin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and predictions. Neurology. 1991;41:685–691. doi: 10.1212/wnl.41.5.685. [DOI] [PubMed] [Google Scholar]
- 3.Glanz BL, Holland CM, Gauthler SA et al. Cognitive dysfunction in patients with clinically isolated syndromes or newly diagnosed multiple sclerosis. Mult Scler. 2007;13:1004–1010. doi: 10.1177/1352458507077943. [DOI] [PubMed] [Google Scholar]
- 4.Rogers JM, Panegyres PK. Cognitive impairment in multiple sclerosis: evidence-based analysis and recommendations. J Clin Neurosci. 2007;14:919–927. doi: 10.1016/j.jocn.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Rao SM, Leo GJ, Ellington L, Nauertz T, Bernadin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology. 1991;41:692–696. doi: 10.1212/wnl.41.5.692. [DOI] [PubMed] [Google Scholar]
- 6.Beatty WW, Blanco CR, Wilbanks SL, Paul RH. Demographic, clinical, and cognitive characteristics of multiple sclerosis patients who continue to work. J Neurol Rehabil. 1995;9:167–173. [Google Scholar]
- 7.Benedict RHB. Effects of using same vs. alternate form memory tests in short-interval, repeated assessment in multiple sclerosis. J Int Neuropsychol Soc. 2005;11:727–736. doi: 10.1017/S1355617705050782. [DOI] [PubMed] [Google Scholar]
- 8.Benedict RHB, Fischer JS, Archibald CJ et al. Minimal neuropsychological assessment of MS patients: a consensus approach. Clin Neuropsychol. 2002;16:381–391. doi: 10.1076/clin.16.3.381.13859. [DOI] [PubMed] [Google Scholar]
- 9.Chiaravalloti ND, DeLuca J. Cognition and multiple sclerosis: assessment and treatment. In: Frank RG, Rosenthal M, Caplan B, editors. Handbook of Rehabilitation Psychology. Washington, DC: American Psychological Association; 2010. pp. 133–144. [Google Scholar]
- 10.Rao SM. Neuropsychological Screening Battery for Multiple Sclerosis. New York, NY: National Multiple Sclerosis Society; 1991. [Google Scholar]
- 11.Rao SM. A Manual for the Brief, Repeatable Battery of Neuropsychological Tests in Multiple Sclerosis. New York, NY: National Multiple Sclerosis Society; 1991. [Google Scholar]
- 12.Gromisch ES, Zemon V, Picone M, Kim S, Foley F. Using a highly abbreviated CVLT-II to detect verbal memory deficits: an ROC analysis of the MS population. Poster presented at: New York Academy of Sciences; June 2011; New York, NY.
- 13.Benedict RH, Munschauer F, Zarevics P et al. Effects of l-amphetamine sulfate on cognitive function in multiple sclerosis patients. J Neurol. 2008;255:848–852. doi: 10.1007/s00415-008-0760-7. [DOI] [PubMed] [Google Scholar]
- 14.Krupp LB, Christodoulou C, Melville P, Scherl WF, MacAllister WS, Elkins LE. Donepezil improves memory in multiple sclerosis in a randomized clinical trial. Neurology. 2004;63:1579–1585. doi: 10.1212/01.wnl.0000142989.09633.5a. [DOI] [PubMed] [Google Scholar]
- 15.Morrow SA, Kaushik T, Zarevics P et al. The effects of L-amphetamine sulfate on cognition in MS patients: results of a randomized controlled trial. J Neurol. 2009;256:1095–1102. doi: 10.1007/s00415-009-5074-x. [DOI] [PubMed] [Google Scholar]
- 16.Krupp LB, Christodoulou C, Melville P et al. Multicenter randomized clinical trial of donepezil for memory impairment in multiple sclerosis. Neurology. 2011;76:1500–1507. doi: 10.1212/WNL.0b013e318218107a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goverover Y, Chiaravalloti ND, DeLuca J. Self-generation to improve learning and memory of functional activities in multiple sclerosis: meal preparation and managing finances. Arch Phys Med Rehabil. 2008;89:1514–1521. doi: 10.1016/j.apmr.2007.11.059. [DOI] [PubMed] [Google Scholar]
- 18.Goverover Y, Basso MR, Wood H, Chiaravalloti N, DeLuca J. Examining the benefits of combining two learning strategies on recall of functional information in persons with multiple sclerosis. Mult Scler. 2011;17:1488–1497. doi: 10.1177/1352458511406310. [DOI] [PubMed] [Google Scholar]
- 19.Sumowski JF, Chiaravalloti N, DeLuca J. Retrieval practice improves memory in multiple sclerosis: clinical application of the testing effect. Neuropsychology. 2010b;24:267–272. doi: 10.1037/a0017533. [DOI] [PubMed] [Google Scholar]
- 20.Chiaravalloti ND, DeLuca J, Moore NB, Ricker JH. Treating learning impairments improves memory performance in multiple sclerosis: a randomized clinical trial. Mult Scler. 2005;11:58–68. doi: 10.1191/1352458505ms1118oa. [DOI] [PubMed] [Google Scholar]


