Abstract
This study explored changes in quality of life (QOL) and psychosocial variables in a large cohort of people with multiple sclerosis (MS). A total of 1287 Australians with MS were administered self-report questionnaires at baseline and 24 months later to examine the impact of disease severity and duration, perceived stress, self-efficacy, depression, and social support on QOL and self-care. Over the 2-year survey period, MS remained stable for 70% of respondents. Disease severity correlated with social support at baseline but not at 24 months, when the only significant correlation with disease severity was that of the World Health Organization Quality of Life–100 instrument (WHOQOL-100) domain of Level of Independence. Although QOL improved across the WHOQOL-100 domains Physical, Psychological, Level of Independence, Social Relationships, and Environment, decreases were found in the WHOQOL-100 facet overall QOL and well-being as well as self-efficacy over the same time period. Hierarchical multiple regression was used to assess the utility of four control measures. MS disease severity and MS disease duration were entered at Step 1, explaining 16.1% of the variance in QOL. After entry of perceived stress, self-efficacy, social support, and the Depression, Anxiety and Stress Scale–21 (DASS-21) at Step 2, the total variance explained by the model as a whole was 55.8% (F6,1028 = 216.495, P < .001). Thus, even in the presence of stable disease and improvement in some WHOQOL-100 domains, overall QOL and self-efficacy had decreased at 2 years after the collection of baseline data. Loss of self-efficacy, increased stress, and depression are key factors in reduced QOL in people with MS.
An estimated 21,200 Australians have multiple sclerosis (MS),1 an inflammatory, often degenerative disease of the central nervous system with an uncertain trajectory that is commonly diagnosed in young adults.2 Residual disability is likely to result from loss of axons within the demyelinated areas of the brain and spinal cord. There is some evidence that disease-modifying drugs may delay disability in the long term.2 Reduced quality of life (QOL) in people with MS has been associated with increasing neurologic disability and psychological distress.3
Most previous research on QOL in MS has focused on the health-related components, such as physical health and symptoms, psychosocial factors, and psychiatric conditions.4 One limitation of using a health-related indicator of QOL is that it does not address other key factors such as social roles, environment, spirituality, and interpersonal relationships. The present study adopted the World Health Organization definition of QOL as “an individual's perception of his/her position in life in the context of the culture and value systems in which he/she lives, and in relation to his/her goals, expectations, standards and concerns. It is a broad-ranging concept, incorporating in a complex way the person's physical health, psychological state, level of independence, social relationships, and their relationship to salient features of their environment.”5(p6)
Quality of life has been measured using a range of instruments, including disease-specific (MSQOL), health-focused (health-related QOL; HRQOL),4 single-item,6 and generic instruments such as the 36-item Short Form Health Status Survey (SF-36).7 The present research measured QOL in people with MS using the World Health Organization Quality of Life–100 instrument (WHOQOL-100),5 as it reflects a broad definition of QOL and overcomes the limited context of purely health-related QOL measures. The 100 items in this self-administered questionnaire are rated on a 5-point scale and make up 24 “facets” each made up of four items and one additional cluster of four items addressing overall QOL and general health. These facets build six independent domains—Physical, Psychological, Level of Independence, Social Relationships, Environment, and Spiritual—and the additional cluster (four items) addressing overall QOL and general health. As an example, the domain addressing psychological health includes five facets, each with four questions, addressing 1) positive affect; 2) thinking, learning, memory, and concentration; 3) self-esteem; 4) body image and appearance; and 5) negative feelings.5 The WHOQOL-100 has been adopted by the Multiple Sclerosis International Federation (MSIF) as the “gold standard” measure for assessing QOL in people with MS.8
In a previous publication, we presented cross-sectional baseline data showing that deterioration in QOL and perceived stress as well as self-efficacy, mood, and social support occurs early in the disease trajectory. Interventions aimed at helping people with MS to improve these psychosocial factors during the years following diagnosis are essential in order to optimize their QOL.9 A longitudinal study was undertaken to determine whether these findings changed over a longer time period by repeating the survey at 12 months and 24 months later, with some modifications.
Methods
The research project was established using the theoretical framework from Braden's10 Model of Self Help, which suggests that outcome factors such as QOL and potential for self-management result from the interaction between relevant antecedent factors and mediating factors. Disease severity and disease duration were identified as antecedent variables; the mediating variables included perceived stress, self-efficacy, mood, and social support; and the outcome factors were QOL and self-management.
Sample
The study sample was recruited from the Australian Multiple Sclerosis Longitudinal Study (AMSLS), described elsewhere.9 Briefly, the AMSLS maintains a large national sample of volunteer Australians with MS, recruited with the assistance of MS societies in all states and territories. More than 96% of participants have definite MS using the international criteria of McDonald et al.,11 according to their neurologist or treating physician. Privacy is protected by use of unique identification numbers stored in a relational database. Ongoing recruitment to the AMSLS and voluntary participation in all surveys meant that there were more participants in the QOL study over time.
Of the baseline sample (N = 1790) and the 24-month sample (N = 2086), 1287 people with MS completed the WHOQOL-100 in both rounds of data collection. Our previous publication9 gave cross-sectional results from baseline; the present report focuses on the changes in QOL across the 2 years from 2006 to 2008 (from baseline to 24 months) of data collection from the 1287 people who completed the longitudinal study. Because MS is often a slowly progressive disease, this 2-year time frame allows sufficient time to have passed for MS-associated changes to occur.
The project received ethical approval from the ACT Health Human Research Ethics Committee and Griffith University Human Research Ethics Committee (both National Health & Medical Research Council [NHMRC]–constituted, independent ethics committees).
Data-Collection Measures
Participants completed a composite questionnaire made up of a self-reported Disease Steps Scale9(p135); a self-reported disease severity scale ranging from minimal impairment to bedridden because of MS; the Perceived Stress Scale12 (a 5-item instrument requiring individuals to rate how disruptive, upsetting, difficult, severe, and stressful they have found the impact of MS); the Multiple Sclerosis Self-Efficacy Scale13 (a 14-item self-efficacy measure with responses given on a 5-point Likert scale from “strongly disagree” to “strongly agree,” with higher scores indicating a more positive appraisal of self-efficacy); a 5-item depression scale based on the Geriatric Depression Scale (GDS)14; the Social Support Scale9 (a 13-item scale that measures day-to-day activities including mobility, personal care, meal preparation, and usual activities on a 4-point Likert scale from “never” to “all the time”); the WHOQOL-1005 (a comprehensive measure of QOL designed by the World Health Organization that addresses QOL in six domains—Physical, Psychological, Level of Independence, Social Relationships, Environment, and Spirituality—using a 5-point Likert scale from “an extreme amount” to “not at all,” with higher scores indicating a more positive appraisal of QOL; and the Therapeutic Self-Care Scale15 (a 12-item instrument used to determine how individuals manage their health, including family assistance and resources needed in the home, on a 5-point Likert scale from “not at all” to “very much so”). The questionnaires used for data collection are presented in greater detail in the article addressing the baseline round of data collection in this longitudinal study.9
In order to gain additional insights into depressive symptoms in this sample, the Depression, Anxiety and Stress Scale–21 (DASS-21) was added to the study for data collection at 12 months and 24 months. The DASS-21 is a self-report scale designed to measure the severity of the core symptoms of depression, anxiety, and stress.16 The depression component of the scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia. The anxiety component assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress component is sensitive to levels of chronic nonspecific arousal. It assesses difficulty relaxing, nervous arousal, and being easily upset/agitated, irritable/overreactive, and impatient. Subjects are asked to use 4-point severity/frequency scales to rate the extent to which they have experienced each state over the past week. Scores for depression, anxiety, and stress are calculated by summing the scores for the relevant items.
Analysis
Once the exploratory data analysis was completed, correlations were identified using a bivariate Pearson correlational analysis with two-tailed test. The number of respondents to the survey was large; hence there was a tendency for even relatively low correlation coefficients to become statistically significant. Thus, in order to reduce the risk of overstating the findings, only correlation coefficients greater than 0.6 or less than −0.6 have been reported, and all reported correlations were significant at the .01 level unless otherwise stated. The analysis was guided by the Braden theoretical framework referred to previously.
After demographic data were analyzed, the role of antecedent and mediating variables in QOL were examined. The interrelationships between QOL domains were also explored. Based on the correlations, hierarchical regression analysis was performed to identify key variables that may influence QOL.
Results
Demographics
Survey respondents came from all states and territories of Australia, including urban and rural areas. There were three data-collection times, but only the analyses of baseline and 24 months are reported in this article, in order to establish changes in QOL over the greatest time span of data collection. Of the 1287 people with MS who completed both baseline and 24-month rounds of data collection, 265 (20.6%) were male and 1014 (78.8%) female. The age of participants ranged from 21 to 88 years (mean, 55 years; SD, 11.38 years). The duration of disease ranged from 3 to 61 years (mean, 13 years; SD, 8.3 years).
Antecedent Variables
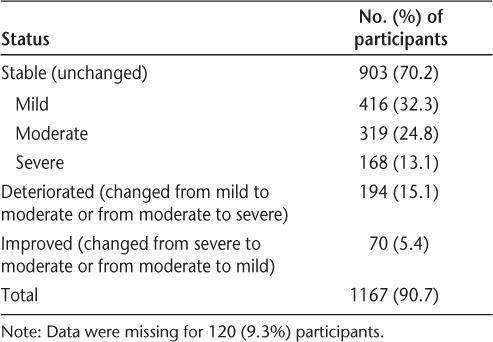
The antecedent variables were disease duration and disease severity. Disease duration did not correlate with any mediating or outcome variables at either baseline or 24 months. Of the people with MS who completed both baseline and 24-month data collection, 903 (70.2%) reported no change in disease severity during the 2-year period from 2006 to 2008. A further 194 (15.1%) reported that their MS had worsened, and 70 (5.4%) reported that their disease had improved (Table 1).
Table 1.
Changes in disease severity over the 2-year study period (N = 1287)
The baseline results indicated that the antecedent factor disease severity correlated with only one variable, social support (r = 0.603). The 24-month results indicated that disease severity was negatively correlated with the WHOQOL-100 domain Independence (−0.621) and no longer positively correlated with social support.
Mediating Variables
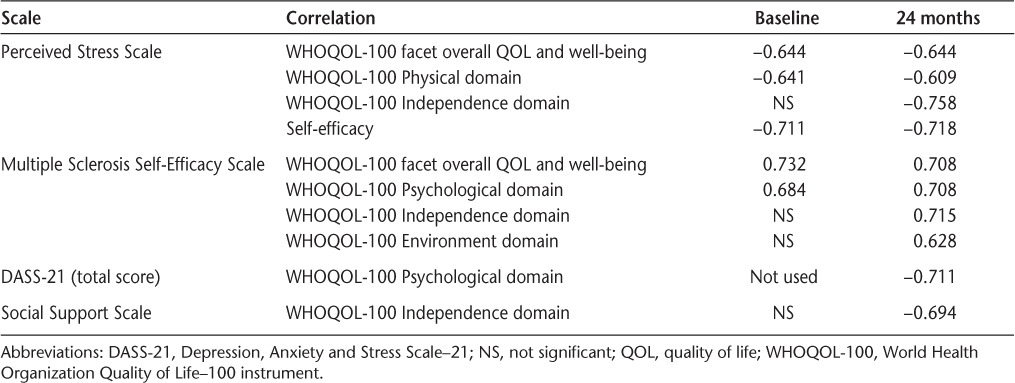
The mediating variables were perceived stress, self-efficacy, mood, and social support. Participants were asked to report their perceptions of the stress MS had caused in recent weeks. Baseline and 24-month results indicated that perceived stress was negatively correlated with the WHOQOL-100 facet overall QOL and well-being (−0.644 and −0.644, respectively), the WHOQOL-100 Physical domain (−0.641 and −0.609), and self-efficacy (−0.711 and −0.718). At 24 months, perceived stress was also negatively correlated with the WHOQOL-100 Independence domain (−0.758).
Participants reported self-efficacy using the Multiple Sclerosis Self-Efficacy Scale. At baseline and 24 months, self-efficacy was positively correlated with the WHOQOL-100 Psychological domain (0.684 and 0.708) and the WHOQOL-100 facet overall QOL and well-being (0.732 and 0.708) and negatively correlated with perceived stress (−0.711 and −0.718). Additional correlations were identified at 24 months; self-efficacy was positively correlated with the WHOQOL-100 Independence domain (0.715) and the WHOQOL-100 Environment domain (0.628) and negatively correlated with the DASS-21depression component (−0.759).
Mood was assessed at baseline using five questions addressing symptoms associated with depression. The DASS-21 was added at 12 and 24 months to gain additional insights. The DASS-21 (total score) results at 24 months were negatively correlated with the WHOQOL-100 Psychological domain (−0.711).
Social support was measured using the 13-item scale addressing the level of support required to perform day-to-day activities. At baseline, social support was positively correlated with disease severity, but this correlation was no longer significant at 24 months. Social support was negatively correlated with the WHOQOL-100 Independence domain (−0.694) at 24 months (Table 2).
Table 2.
Mediating factor correlations at baseline and 24 months
Outcome Factors
Quality of life and self-management were proposed as the two outcome factors prior to the start of the study. At both baseline and 24 months, self-management did not correlate with any other variable being addressed.
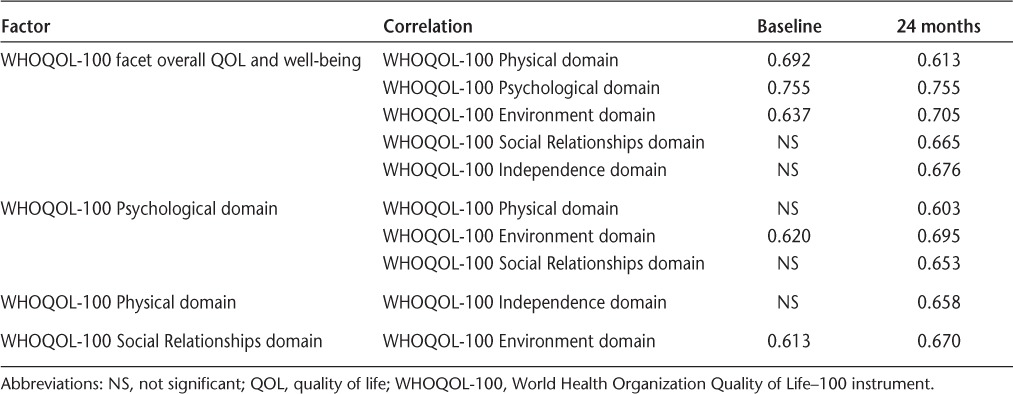
Quality of life was measured using the WHOQOL-100. There were no correlations with antecedent variables at baseline or 24 months. The correlations between the WHOQOL-100 and the mediating variables were discussed above. The WHOQOL-100 addresses a range of domains that were found to correlate positively with each other at baseline and 24 months. The WHOQOL-100 facet overall QOL and well-being (an independent variable and not a sum of other domains) correlated positively with a number of QOL domains at both baseline and 24 months. It correlated positively with the WHOQOL-100 Physical domain (0.692 and 0.613), the WHOQOL-100 Psychological domain (0.755 and 0.755), and the WHOQOL-100 Environment domain (0.637 and 0.705). The WHOQOL-100 Psychological domain correlated positively with the WHOQOL-100 Environment domain (0.620 and 0.695). In addition, the WHOQOL-100 facet overall QOL and well-being correlated positively with the WHOQOL-100 Social Relationships domain (0.665) at 24 months.
The WHOQOL-100 Social Relationships domain correlated positively with the WHOQOL-100 Environment domain at both baseline and 24 months (0.613 and 0.670). In addition, the WHOQOL-100 Psychological domain correlated positively with the WHOQOL-100 Physical domain (0.603) and Social Relationships domain (0.653) at 24 months (Table 3).
Table 3.
Outcome factor correlations at baseline and 24 months
A paired-samples t test was conducted to evaluate the changes over time in the participants' scores across the WHOQOL-100 domains, self-efficacy, and perceived stress. There was a statistically significant increase in means between baseline and 24 months for the WHOQOL-100 Physical domain, WHOQOL-100 Psychological domain, WHOQOL-100 Independence domain, WHOQOL-100 Social Relationships domain, and WHOQOL-100 Environment domain scores. The results indicate improved QOL across these domains over the 2-year study period. There was a statistically significant decrease in means between baseline and 24 months for the WHOQOL-100 overall QOL and well-being and self-efficacy scores. The results indicate reduced overall QOL and self-efficacy over the 2-year study period (Appendix 1).
Hierarchical multiple regression was used to assess the ability of three control measures (perceived stress, self-efficacy, and social support) to predict levels of QOL (WHOQOL-100 overall QOL and well-being) at baseline, after controlling for the influence of MS disease severity and MS disease duration. Preliminary analysis was conducted to ensure no violation of the assumptions of normality, linearity, multicollinearity, and homoscedasticity. MS disease severity and MS disease duration were entered at Step 1, explaining 12.1% of the variance in QOL. After entry of perceived stress, self-efficacy, and social support at Step 2, the total variance explained by the model as a whole was 57.2% (F5,939 = 250.688, P < .001). The three control measures explained an additional 45.1% of the variance in QOL after controlling for MS disease severity and MS disease duration (change in R2 = 0.45, change in F3,939 = 329.264, P < .001). In the final model, only perceived stress and self-efficacy were statistically significant, with self-efficacy having an unstandardized (B) coefficient (0.175, SE 0.020) and perceived stress an unstandardized (B) coefficient (−0.113, SE 0.013).
Hierarchical multiple regression was used to assess the ability of four control measures (perceived stress, self-efficacy, social support, and DASS-21) to predict levels of QOL (WHOQOL-100 overall QOL and well-being) at 24 months, after controlling for the influence of MS disease severity and MS disease duration. Preliminary analysis was conducted to ensure no violation of the assumptions of normality, linearity, multicollinearity, and homoscedasticity. MS disease severity and MS disease duration were entered at Step 1, explaining 16.1% of the variance in QOL. After entry of perceived stress, self-efficacy, social support, and DASS-21 at Step 2, the total variance explained by the model as a whole was 55.8% (F6,1028 = 216.495, P < .001). The four control measures explained an additional 39.8% of the variance in QOL after controlling for MS disease severity and MS disease duration (change in R2 = 0.40, change in F4,1028 = 231.801, P < .001). In the final model, perceived stress, self-efficacy, and DASS-21were statistically significant, with self-efficacy having an unstandardized (B) coefficient (0.131, SE 0.010), perceived stress an unstandardized (B) coefficient (−0.120, SE 0.021), and the DASS-21 an unstandardized (B) coefficient (−0.126, SE 0.004).
Discussion
The preliminary analysis of disease severity in this large sample of people with MS indicated that for approximately 70% of people, their MS had been stable for 24 months, with a further 15% reporting that their MS had deteriorated and 5% reporting that their MS had improved during that time. The natural history of MS is uncertain for any given individual. There is some evidence that the number of exacerbations in relapsing-remitting MS early in the disease is associated with a worse prognosis.17 Previous work on the natural history of MS has established that median times to reach irreversible limitation in ambulation (Disability Status Scale [DSS] 4) and the wheelchair-bound stage (DSS 7) among people with MS not on disease-modifying drugs are approximately 8 and 30 years, respectively.2 Possible explanations for the reports of MS improving over the 24 months include normal fluctuations in the disease, including post-exacerbation resolution; and better coping strategies that increase self-efficacy, perhaps including hope, which has been associated with increased success in coping with MS.18
The impact of self-efficacy, depression, and stress in people with MS is receiving increasing research focus. The results of the present research confirm those of other studies addressing the effect of self-efficacy on adjustment to MS. Self-efficacy (“the individual's belief that they have the ability to overcome challenges presented to them”)13 is linked to self-care and improved ability to adjust to MS.19,20 It was found that, when combined with outcome expectations and disease severity, self-efficacy predicted 51% of the variance in adjustment to MS.20 There are significant differences in self-efficacy between those with relapsing-remitting MS and those with progressive forms of the disease.21 In the current study, perceived stress, self-efficacy, social support, and depression predicted 55.8% of variance in QOL when disease duration and disease severity were controlled for. Self-efficacy made the largest unique contribution to the model (beta = .416). It has been suggested that self-efficacy and social support may play a positive role in countering the effects of existing disability to increase QOL,22 and people with MS could benefit from strategies that enhance self-efficacy.21
Depression is common in people with MS,23,24 and it adversely affects QOL and activity while being a “significant source of misery, independent from MS symptoms.”25(p215) Self-efficacy, helplessness, and cognitive distortions have been found to predict depression in people with MS.19 Depression adversely affects the patient's capacity to self-manage. It has been established that “Those who have depressive symptoms (including subclinical depression) were much less likely to gain in activation and to improve in their self-management behaviors. It appears that as long as depressive symptoms persist, activation is unlikely to occur.”26(p1461) Activation is a developmental process in which people move from a state of very little understanding of their condition and taking little or no active role in their own health-care management to a state of understanding the disease and taking an active role in their own care.27 Activation and self-efficacy and taking an active role in self-management are all linked. Therefore, factors that inhibit activation and self-efficacy are likely to adversely affect self-management strategies. The results of the present research confirm the adverse impact of depression. Depression made a unique contribution to the model (beta = −.196). It has been suggested previously that people with MS are not being adequately screened, diagnosed, or referred for treatment for depression,28 even though depression in this population is responsive to treatment.29
Stress was the third factor that made a significant unique contribution to the model predicting QOL (beta = −.202). The uncertainty associated with the diagnosis of MS and its trajectory place people with MS at higher risk for negative outcomes. Illness uncertainty explained a significant portion of the variance in mood state in research addressing illness uncertainty, stress, coping, and emotional well-being in people with MS.30 The present research confirms the adverse impact of stress and the interdependence between self-efficacy, depression, and stress and QOL in people with MS.
Strengths and Limitations
This research provides important insights into factors that affect the QOL of people with MS over time. Strengths of the study include a large sample size and repeated QOL measures in the same cohort. A limitation was the use of a single generic measure of QOL, the WHOQOL-100, which is less sensitive to change in QOL in MS than are some disease-specific measures of QOL. Nevertheless, the generic measure did allow comparison with the general population. The DASS-21 was added at 12 and 24 months to gain additional insights into the role of depression in QOL. Because this article focuses on changes between baseline and 24 months, only the 24-month DASS-21 results are reported here.
Implications for Practice
The QOL of people with MS is affected by their levels of self-efficacy, depression, and stress. Optimizing QOL in people with MS requires accurate diagnoses of depression and stress as well as appropriate treatment for them. Increased self-efficacy is likely to result in improved self-management. However, the presence of depression is likely to hinder MS patients' ability to take an active role in self-management. For health-care providers aiming to maximize self-management, the first step must be to ensure that the patient is assessed for mood disorders and that appropriate therapy is provided. People make self-management decisions that reflect their sociocultural characteristics, psychological interpretations, spiritual beliefs, and personal priorities31; therefore, a holistic, patient-centered approach to care is required.
PracticePoints.
The quality of life of people with MS is affected by their levels of self-efficacy, depression, and stress.
Accurate diagnoses of depression and stress followed by appropriate treatment are required to address these conditions.
Depression may prevent the person with MS from taking an active role in self-management.
Acknowledgments
We would like to thank the volunteers at MS Australia, ACT Branch, for survey collation and mailing assistance. We gratefully acknowledge the essential contribution made by the survey respondents from the Australian Multiple Sclerosis Longitudinal Study (AMSLS).
Appendix 1. Paired-samples t test
Statistically significant increases in means over time
WHOQOL-100 Physical domain scores from baseline (mean, 12.13; SD, 1.6) to 24 months (mean, 12.62; SD, 3.04), t1202 = −7.623, P < .0005 (two-tailed). The mean increase in WHOQOL-100 Physical domain scores was 0.4, with a 95% confidence interval (CI) of −0.619 to −0.365.
WHOQOL-100 Psychological domain scores from baseline (mean, 13.39; SD, 2.13) to 24 months (mean, 13.94; SD, 2.54), t1156 = −11.384, P < .0005 (two-tailed). The mean increase in WHOQOL-100 Psychological domain scores was 0.55, with a 95% CI of −0.642 to −0.454.
WHOQOL-100 Independence domain scores from baseline (mean, 12.7; SD, 1.9) to 24 months (mean, 13.15; SD, 3.6), t1166 = −5.906, P < .0005 (two-tailed). The mean increase in WHOQOL-100 Independence domain scores was 0.45, with a 95% CI of −0.602 to −0.302.
WHOQOL-100 Social Relationships domain scores from baseline (mean, 13.01; SD, 2.2) to 24 months (mean, 14.00; SD, 3), t1151 = −15.911, P < .0005 (two-tailed). The mean increase in WHOQOL-100 Social Relationships domain scores was 0.99, with a 95% CI of −1.109 to −0.865.
WHOQOL-100 Environment domain scores from baseline (mean, 13.68; SD, 1.49) to 24 months (mean, 15.17; SD, 2.17), t1138 = −32.659, P < .0005 (two-tailed). The mean increase in WHOQOL-100 Environment domain scores was 1.49, with a 95% CI of −1.573 to −1.395.
Statistically significant decreases in means over time
WHOQOL-100 overall QOL and well-being facet scores from baseline (mean, 14.02; SD, 3.46) to 24 months (mean, 13.83; SD, 3.58), t1286 = 2.515, P < .0005 (two-tailed). The mean decrease in WHOQOL-100 overall QOL and well-being facet scores was 0.19, with a 95% CI of 0.041 to 0.335.
Self-efficacy scores from baseline (mean, 52.20; SD, 11.44) to 24 months (mean, 51.46; SD, 11.9), t1238 = 3.374, P < .0005 (two-tailed). The mean decrease in total self-efficacy scores was 0.74, with a 95% CI of 0.310 to 1.171.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This study was funded by a grant from Griffith University and in part by MS Research Australia through corporate donations, including from Perpetual Trustees Philanthropic Division, Deloitte Australia, Bayer-Schering, Biogen Idec, Merck-Serono, and Sanofi-Aventis.
References
- 1.Covance Palmer A. Economic Impact of Multiple Sclerosis 2010. Prepared for MS Research Australia by Covance Pty Ltd, North Ryde, NSW, and Prof. Andrew Palmer, Menzies Research Institute Tasmania, TAS, Australia, 2011. http://www.msra.org.au/files/msra/docs/Economic%20Impact%20of%20MS%20in%202010%20Full%20Report.pdf. Accessed October 2011.
- 2.Trojano M, Paolicelli D, Tortorella C et al. Natural history of multiple sclerosis: have available therapies impacted long-term prognosis? Neurol Clin. 2011;29:309–321. doi: 10.1016/j.ncl.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Kern S, Schrempf W, Schneider H et al. Neurological disability, psychological distress, and health-related quality of life in MS patients within the first three years after diagnosis. Mult Scler. 2009;15:752–758. doi: 10.1177/1352458509103300. [DOI] [PubMed] [Google Scholar]
- 4.Buchanan RJ, Huang C, Kaufman M. Health-related quality of life among young adults with multiple sclerosis. Int J MS Care. 2010;12:190–199. [Google Scholar]
- 5.Murphy B, Herrman H, Hawthorne G, Pinzone T, Evert H. Australian WHOQOL Instruments: User's Manual and Interpretation Guide. Melbourne, Australia: Australian WHOQOL Field Study Centre; 2000. http://www.psychiatry.unimelb.edu.au/centres-units/cpro/whoqol/instruments/manual.pdf. [Google Scholar]
- 6.Cosio D, Jin L, Siddique J, Mohr PH, Mohr DC. The effect of telephone-administered cognitive-behavioral therapy on quality of life among patients with multiple sclerosis. Ann Behav Med. 2011;41:227–234. doi: 10.1007/s12160-010-9236-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dalgas U, Stenager E, Jakobsen J et al. Fatigue, mood and quality of life improve in MS patients after progressive resistance training. Mult Scler. 2010;16:480–490. doi: 10.1177/1352458509360040. [DOI] [PubMed] [Google Scholar]
- 8.Trisolini M, Wiener J, Miller DM. Principles to Promote the Quality of Life of People with Multiple Sclerosis. London: Multiple Sclerosis International Federation; 2005. [Google Scholar]
- 9.Wollin J, Fulcher G, McDonald E et al. Psychosocial factors that influence quality of life and potential for self-management in multiple sclerosis. Int J MS Care. 2010;12:133–141. [Google Scholar]
- 10.Braden CJ. Learned self-help response to chronic illness. Sch Inq Nurs Pract. 1990;4:23–41. [PubMed] [Google Scholar]
- 11.Polman CH, Reingold SC, Edan G et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria.”. Ann Neurol. 2005;58:840–846. doi: 10.1002/ana.20703. [DOI] [PubMed] [Google Scholar]
- 12.Terry DJ. Stress, coping and adaptation to new parenthood. J Soc Pers Relat. 1991;8:527–547. [Google Scholar]
- 13.Rigby SA, Domenech C, Thornton EW, Tedman S, Young CA. Development and validation of a self-efficacy measure for people with multiple sclerosis: the Multiple Sclerosis Self-Efficacy Scale. Mult Scler. 2003;9:73–81. doi: 10.1191/1352458503ms870oa. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh JI, Yesavage J. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol: J Aging Mental Health. 1986;5:165–173. [Google Scholar]
- 15.Doran DI, Sidani S, Keatings M, Doidge D. An empirical test of the nursing role effectiveness model. J Adv Nurs. 2002;38:29–39. doi: 10.1046/j.1365-2648.2002.02143.x. [DOI] [PubMed] [Google Scholar]
- 16.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney, Australia: Psychology Foundation; 1995. [Google Scholar]
- 17.Mowry EM. Natural history of multiple sclerosis: early prognostic factors. Neurol Clin. 2011;29:279–292. doi: 10.1016/j.ncl.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 18.Pinson DMK, Ottens AJ, Fisher TA. Women coping successfully with multiple sclerosis and the precursors of change. Qual Health Res. 2009;19:181–193. doi: 10.1177/1049732308329465. [DOI] [PubMed] [Google Scholar]
- 19.Shnek ZM, Foley FW, LaRocca NG, Smith CR, Halper J. Psychological predictors of depression in multiple sclerosis. Neurorehabil Neural Repair. 1995;9:15–23. [Google Scholar]
- 20.Wassem R. Self-efficacy as a predictor of adjustment to multiple sclerosis. J Neurosci Nurs. 1992;24:224–229. doi: 10.1097/01376517-199208000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Fraser C, Polito S. A comparative study of self-efficacy in men and women with multiple sclerosis. J Neurosci Nurs. 2007;39:102–106. doi: 10.1097/01376517-200704000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Stuifbergen AK, Seraphine A, Roberts G. An exploratory model of health promotion and quality of life in chronic disabling conditions. Nurs Res. 2000;49:122–129. doi: 10.1097/00006199-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Sadovnick AD, Remick RA, Allen J et al. Depression and multiple sclerosis. Neurology. 1996;46:628–632. doi: 10.1212/wnl.46.3.628. [DOI] [PubMed] [Google Scholar]
- 24.Simmons RD. Life issues in multiple sclerosis. Nat Rev Neurol. 2010;6:603–610. doi: 10.1038/nrneurol.2010.143. [DOI] [PubMed] [Google Scholar]
- 25.Mohr DC, Hart SL, Julian L, Tasch ES. Screening for depression among patients with multiple sclerosis: two questions may be enough. Mult Scler. 2007;13:215–219. doi: 10.1177/1352458506070926. [DOI] [PubMed] [Google Scholar]
- 26.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42:1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohr DC, Hart SL, Fonareva I, Tasch ES. Treatment of depression for patients with multiple sclerosis in neurology clinics. Mult Scler. 2006;12:204–208. doi: 10.1191/135248506ms1265oa. [DOI] [PubMed] [Google Scholar]
- 29.Mohr DC, Boudewyn AC, Goodkin DE, Bostrom A, Epstein L. Comparative outcomes for individual cognitive-behavior therapy, supportive-expressive group psychotherapy, and sertraline for the treatment of depression in multiple sclerosis. J Consult Clin Psychol. 2001;69:942–949. [PubMed] [Google Scholar]
- 30.Wineman NM, Schwetz KM, Goodkin DE, Rudick RA. Relationships among illness uncertainty, stress, coping, and emotional well-being at entry into a clinical drug trial. Appl Nurs Res. 1996;9:53–60. doi: 10.1016/s0897-1897(96)80413-7. [DOI] [PubMed] [Google Scholar]
- 31.Kralik D. Poodle skirts, lava lamps and hot pants . . . is chronic condition self-management another fad? J Adv Nurs. 2008;62:74–83. doi: 10.1111/j.1365-2648.2008.04595.x. [DOI] [PubMed] [Google Scholar]


