Abstract
The objective of this study was to identify characteristics of informal caregivers, caregiving, and the people with multiple sclerosis (MS) receiving assistance that are associated with reduced caregiver employment. Data were collected during telephone interviews with 530 MS caregivers, including 215 employed caregivers, with these survey data analyzed using logistic regression. Poorer cognitive ability by the care recipient to make decisions about daily tasks and more caregiving hours per week predicted reduced caregiver employment. Better physical health domains of caregiver quality of life were associated with significantly lower odds of reduced employment. Health professionals treating informal caregivers, as well as those treating people with MS, need to be aware of respite, support, and intervention programs available to MS caregivers and refer them to these programs, which could reduce the negative impact of caregiving on employment.
About 30% of people with multiple sclerosis (MS) require assistance at home, with 80% of that support provided by informal (or family) caregivers.1 Support from informal caregivers enables people with MS to remain in their homes as their dependence becomes more permanent and their need for personal assistance increases.2 Informal caregivers provide a range of services to people with MS, including personal care and assistance with homemaking, mobility, transportation, and recreation.3 A review of the literature found no studies identifying characteristics associated with reduced employment among MS caregivers. The objective of this study was to identify characteristics of caregivers, caregiving, and people with MS receiving assistance that are associated with reduced caregiver employment.
Previous caregiver studies found that helping family members cope with the impact of aging or other chronic illnesses on daily life can have a negative impact on caregiver employment.4,5 A 2009 national survey of a sample of 1480 informal caregivers assisting people with a range of chronic conditions found that the proportion of caregivers reporting they were employed declined as the level of caregiving burden increased.5 Previous studies indicated that caregiving responsibilities frequently interfered with employment, forcing a reduction in hours worked, change in work schedules, refusal of promotions, or the need for a leave of absence.4–6 Characteristics of elderly care recipients linked to reduced caregiver employment are dependence in activities of daily living and instrumental activities of daily living, dementia, and behavioral problems.4,5
Methods
The sample for our survey of informal caregivers was recruited from the Registry of the North American Research Committee on Multiple Sclerosis (NARCOMS) project. The objective of our survey was to learn more about the experiences of informal caregivers assisting people with MS who had greater physical dependency. The NARCOMS Registry contains information for 35,000 people with MS at least 18 years of age who volunteered to participate in data collection and other research projects.7 Registry participants are assured confidentiality and that their names will not be disclosed to anyone without the participant's written permission.
Sample Selection
We developed a sample of 530 caregivers by contacting people with MS participating in the NARCOMS Registry who were more dependent, with dependence measured using the Patient-Determined Disease Steps (PDDS). The PDDS, a self-assessment of mobility, is scored from 0 (normal) to 8 (bedridden).8 The PDDS is a surrogate for the physician-administered Expanded Disability Status Scale (EDSS), recognized as the gold standard for measuring physical disability and neurologic impairment in people with MS.9 PDDS scores are strongly linked with the EDSS, indicating that the PDDS is a good measure of MS-related impairment.9 We contacted people with MS who needed a cane to walk 25 feet (PDDS = 5), required bilateral support (PDDS = 6), primarily used a wheelchair or scooter (PDDS = 7), or were bedridden (PDDS = 8). We identified 4943 Registry participants with MS to receive a recruitment letter. This letter stated that we wanted to interview “the person who provides the majority of informal or unpaid care to you to help you cope with the effects of MS on your daily life.” The letter requested that the person with MS ask their caregiver to call a toll-free number to complete the computer-assisted telephone interview.
Survey Process
The survey was administered by the Public Policy Research Institute at Texas A&M University. The study was approved by the Office of Regulatory Compliance at Mississippi State University in June 2006 and by the Office of Research Compliance at Texas A&M University in July 2006. About 1000 recruitment letters per week were mailed in September 2006, for a total initial mailing of 4071 letters. By December 2006, we completed interviews with 432 MS caregivers. Additional recruitment letters were mailed in January 2007 to 872 people with MS not included in the September 2006 mailings. When the survey ended in March 2007, we had completed 530 interviews with MS caregivers.
The study protocol ended the survey when no caregivers called to complete the interview for 2 weeks. NARCOMS has institutional review board approval to inform Registry participants about opportunities to participate in additional studies, with the decision to participate left to each individual without any pressure. NARCOMS typically does not send reminders to participate in a study to Registry participants receiving a recruitment letter. All respondents invited to participate in our study received only one recruitment letter. Calculation of a participation rate is difficult because we do not know how many people with MS receiving the recruitment letter had an informal caregiver. About 25% of people with MS have an informal caregiver,6 or an estimated 1235 of the 4943 people with MS receiving our recruitment letters. Assuming 1235 informal caregivers, 530 completed interviews yields a 43% caregiver participation rate.
Caregiver Interview Questionnaire
The survey recorded caregiver assessments of MS disease and symptom characteristics, the impact MS had on the care recipient, the care needs of the person with MS, the caregiver's relationship to the person with MS, demographic information about the person with MS and the caregiver, and how assisting the person with MS affected the caregiver. The interview lasted about 35 minutes (median, 36.8 minutes).
Health Status and MS Symptoms
Interviewers asked caregivers to assess the current overall health of the person with MS, adapting a question from the 8-item Short Form Health Status Survey (SF-8).10 Survey questions on cognitive decision making and activities of daily living (ADLs) were adapted from the “Minimum Data Set (MDS) for Nursing Home Resident Assessment and Care Screening.”11 These MDS questions assessing ADLs and cognitive status have been included in a validated tool to measure physical dependence and cognitive function in people living in the community.12,13
The interviewer asked caregivers about the ability of the person with MS to make everyday decisions about daily tasks, such as scheduling activities and organizing and planning daily activities. Four possible responses for the decision-making ability of the person with MS were provided: 1) independent decision making, defined by the interviewer as “daily decisions are appropriate, consistent, reasonable, and organized”; 2) modified independence in decision making, defined as “daily decisions are typically appropriate and reasonable in familiar situations but [the person with MS] faces difficulty when faced with new tasks or situations”; 3) moderately impaired decision making, defined as “decisions are poor and [the person with MS] requires supervision in planning, organizing, and performing daily routines”; and 4) severely impaired decision making, defined as “decision making is severely impaired and [the person with MS] typically does not make decisions about day to day activities.”
ADL responses from the caregiver were used to develop an ADL Short Scale to measure the functional dependence of the person with MS.14 The ADL Short Scale includes four items: personal hygiene, toilet use, locomotion, and eating. Each ADL is scored on a scale of 0 to 4, with 0 indicating “independent (no assistance needed)” in the performance of the ADL, 1 indicating “supervision needed,” 2 indicating “limited assistance,” 3 indicating “extensive assistance,” and 4 indicating “complete assistance/total dependence.” The score on the ADL Short Scale for each person with MS can range from 0 to 16.
Caregiving
The interviewer asked caregivers to provide the average number of hours they spent each week assisting the person with MS to cope with the impact of MS on daily life. Interviewers asked the caregivers if paid caregivers or other unpaid caregivers also helped the person with MS cope with the impact of MS. Interviewers read a list of statements assessing a range of feelings that caregivers may have experienced when assisting the person with MS, including “caregiving is burdensome,” “caregiving is emotionally draining,” and “caregiving strained or threatened the caregiver/care recipient relationship.” These caregiver feelings were measured using a 5-point Likert item, with possible responses of none of the time, once in a while, some of the time, most of the time, and all of the time. The caregivers were asked if they needed or would have benefited from treatment from a mental health professional in the previous 12 months.
Health-Related Quality of Life
The interview included the SF-8, which is designed to provide a health-related quality of life (HRQOL) profile, to assess the HRQOL of the caregiver, not the person with MS. The SF-8 HRQOL profile consists of eight items and includes a Physical Component Summary and a Mental Component Summary, which are positively scored with higher scores indicating better health-related status.10,15 Previous studies documented the validity of the SF-8 in the United States,10 and the SF-8 meets standard evaluation criteria for content, construct, and criterion-related validity.15 We included the Mental Component Summary as a measure of the mental health status of the caregiver and the Physical Component Summary as a measure of caregiver physical health.
Statistical Methods
Of the 530 caregivers in our survey, 31.5% of caregivers were employed full time and 10.6% were employed part time at the time of the interview. Interviewers asked these 223 employed caregivers if providing assistance to the person with MS caused them to reduce the amount of time worked in the last 12 months, with 42% responding that they had reduced their employment. Because the study utilized a dichotomous dependent variable (a reduction in caregiver employment, coded as 0 = no; 1 = yes), we developed a logistic regression model. The initial regression model included 22 independent variables developed from survey response data. Of the 223 caregivers reporting employment, 215 caregivers provided data for all 22 independent variables and were included in the analyses. Table 1 presents these independent variables and describes how they were coded.
Table 1.
Independent variables used in analyses of reduced employment among MS caregivers
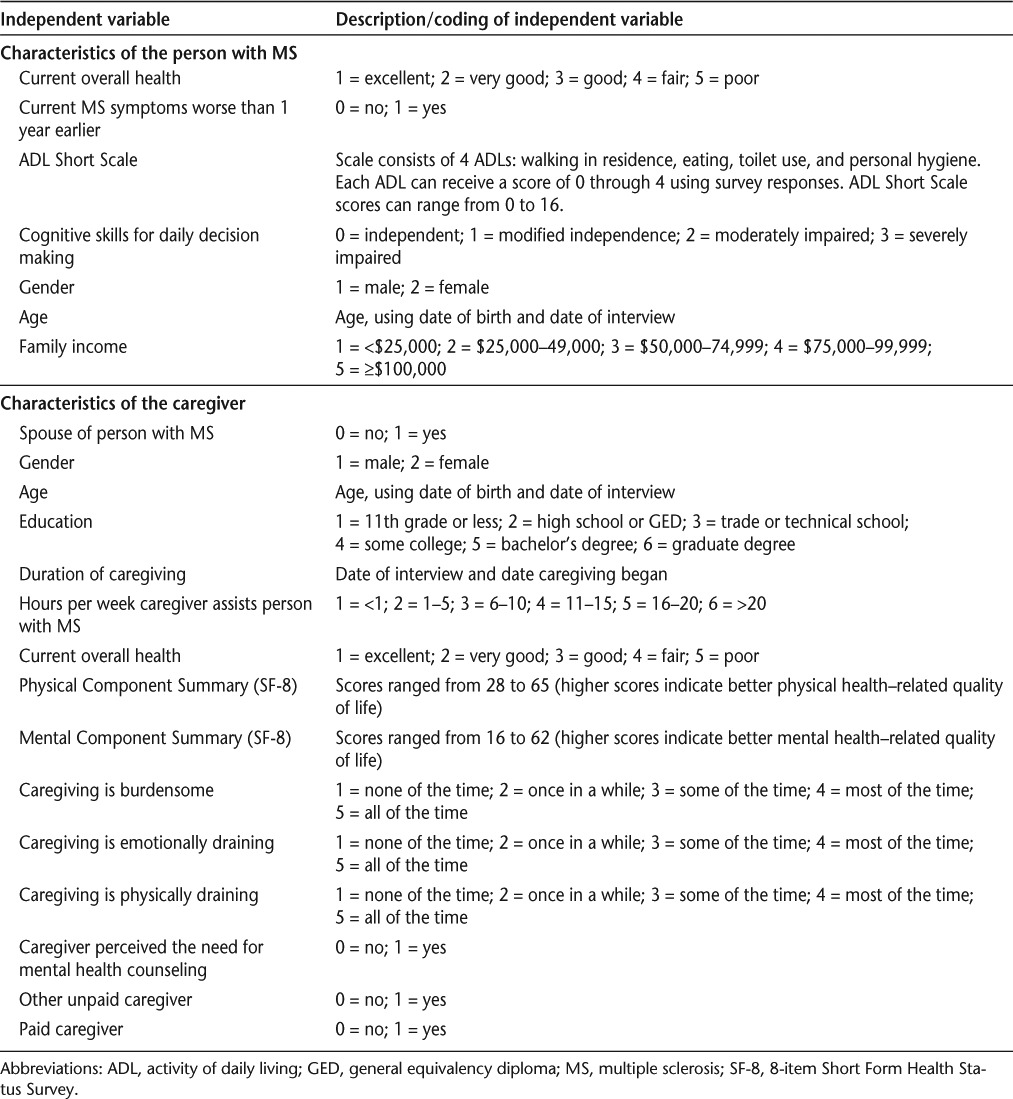
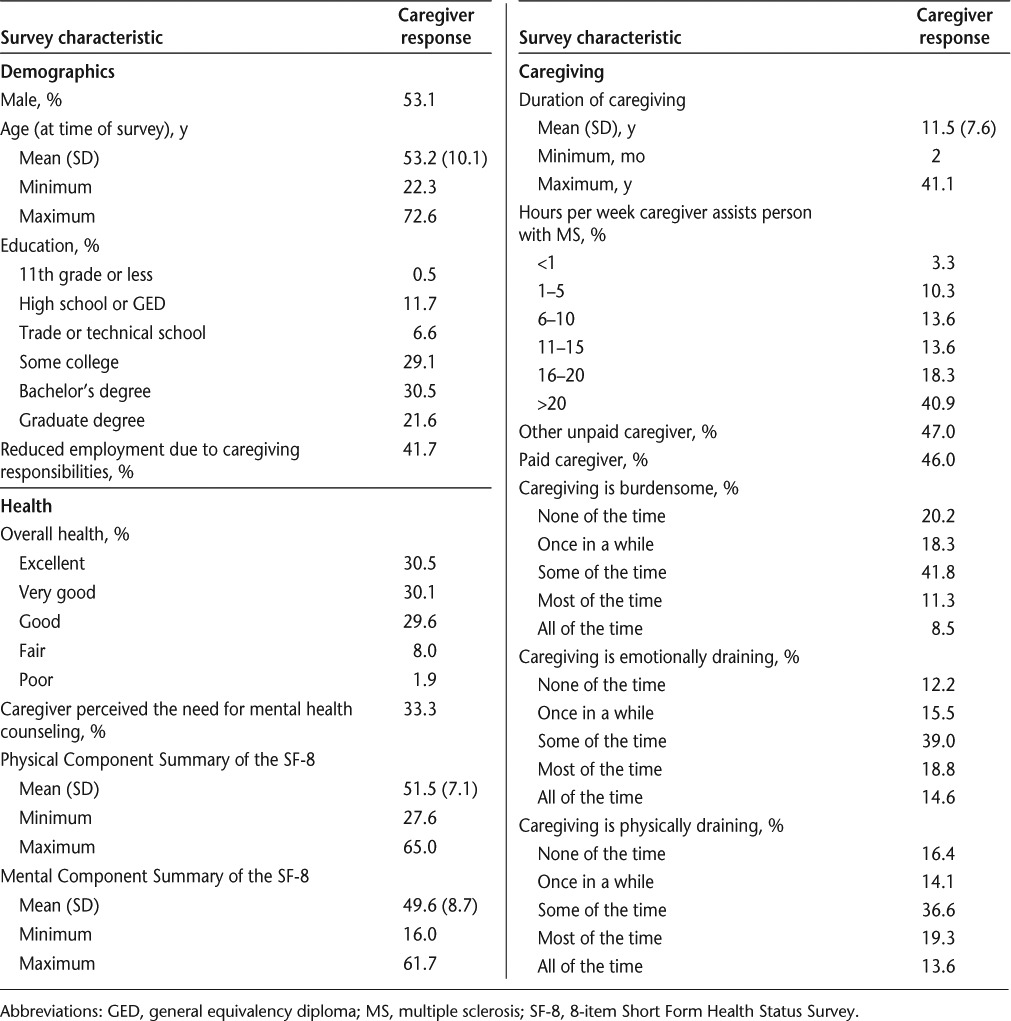
Table 2 presents key characteristics of the people with MS receiving assistance and Table 3 presents key characteristics of the employed caregivers included in our regression analyses. Our regression model included a range of independent variables we theorized might be associated with a reduction in caregiver employment. For example, we wanted to learn whether characteristics of the person with MS (such as level of dependence measured by the ADL Short Scale or cognitive ability to make decisions about daily tasks) and MS-related symptoms (for example, whether MS symptoms were worse than 1 year earlier) were associated with caregiver employment. We also wanted to learn whether any demographic characteristics of the caregiver or care recipient, aspects of caregiving (such as the amount of time spent assisting the person with MS), or feelings about caregiving (for example, whether caregiving was emotionally draining) were associated with any reduction in employment.
Table 2.
Characteristics of the people with MS receiving assistance (N = 215)
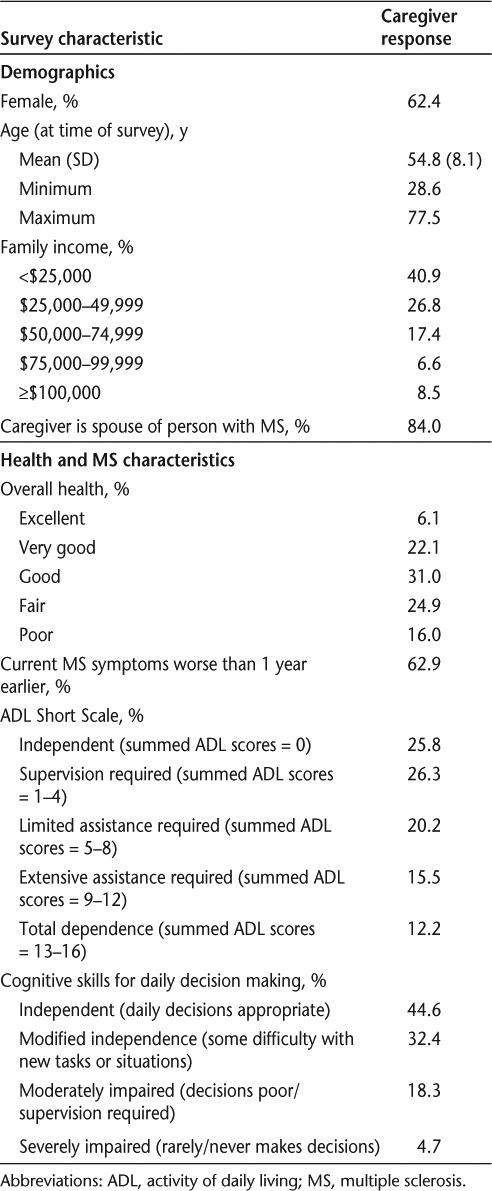
Table 3.
Characteristics of MS caregivers (N = 215)
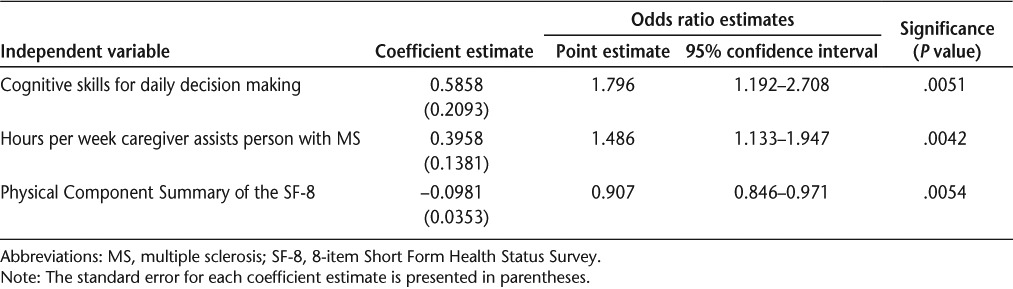
We utilized the stepwise selection procedure to reduce the number of independent variables in the initial regression model, eliminating the least significant variables. Stepwise selection has the advantage of producing a small, readily interpretable model, containing the most important predictor variables.16 Stepwise selection methods are among the most widely used in medical applications.17 The stepwise selection method excluded 19 independent variables from our initial regression model. Table 4 presents the three characteristics of the caregivers, caregiving, and the person with MS receiving assistance that were significantly associated with caregiver employment at the level of α = .05.
Table 4.
Factors associated with reduced employment among MS caregivers
Results
Poorer cognitive skills to make decisions about daily tasks exhibited by the care recipient were significantly linked to reduced caregiver employment, with a one-category decline in these cognitive skills (for example, from modified independence to moderately impaired) increasing the odds of reduced caregiver employment by 79.6%. The number of hours per week assisting the person with MS cope with the impact of the disease on daily life also was significantly associated with caregiver employment, with more hours of caregiving linked to greater odds of reduced employment. A one-unit increase in the reported number of hours per week assisting the person with MS (for example, an increase in the number of hours from “6 to 10 hours per week” to “11 to 15 hours per week”) increased the odds of the caregiver reporting reduced employment by 48.6%. In contrast, a one-unit increase in the caregiver's Physical Component Summary of the SF-8 (better physical health) decreased the odds of reduced caregiver employment by 9.3%. A five-unit increase in the physical health domain for the caregiver decreased the odds of the caregiver reporting reduced employment by 38.8%.
Discussion
Helping family members cope with chronic illness or the effects of aging on daily life can have a negative impact on caregiver employment, forcing a reduction in hours worked, change in work schedules, refusal of promotions, or the need for a leave of absence.4–6 However, a review of the literature found no studies identifying characteristics associated with reduced employment among informal caregivers assisting people with MS. The objective of our study was to identify characteristics of informal caregivers, caregiving, and people with MS receiving assistance associated with reduced caregiver employment.
Cognitive Skills
The care recipient's cognitive ability to make decisions about daily tasks was significantly linked to caregiver employment, with cognitive dysfunction predicting reduced caregiver employment. Cognitive impairment affects up to 65% of people with MS and can occur in early stages of the disease,18,19 even among those without physical disability.20 Cognitive impairment among people with MS can disrupt social relationships and family life, with more frequent divorce compared to MS patients without cognitive disability but with similar levels of physical disability.21 Cognitive dysfunction interferes with the ability of the person with MS to perform day-to-day life activities, work, drive, and travel independently, resulting in a loss of mobility and independence.21,22 Cognitively impaired people with MS are more likely to need assistance with personal care, managing the household, and the performance of ADLs than healthy controls.21
Given the association between cognitive dysfunction exhibited by the care recipient and caregiver employment, reducing cognitive difficulties in people with MS could help offset the negative impact of this MS-related condition on caregiver employment. Available approaches to treat MS-related cognitive dysfunction include pharmacologic and behavioral methods.23,24 An earlier study found beneficial effects with pharmacologic treatment of cognitive impairment in MS.25 Another study indicates that cognitive rehabilitation programs and enhancement strategies may be beneficial in combating cognitive decline in people with MS.26 Assistive technologies, cognitive aids, personal digital assistants, and exercise training may help improve daily function and manage cognitive impairment in people with MS.20,27
Interventions to support informal caregivers assisting people with dementia or stroke could be adapted for caregivers assisting people with MS who have cognitive difficulties. For example, the program “Resources for Enhancing Alzheimer's Caregiver Health (REACH)” is a behavioral intervention for dementia caregivers that includes education, support, and skills training.28 Caregivers participating in the REACH intervention reported significant reductions of burden, depression, and caregiving frustrations, as well as increased social support.28 The Transition Assistance Program (TAP), developed for stroke caregivers, has three components: skill development, education, and supportive problem solving.29 Participation in TAP was associated with decreased caregiver strain and depression, with high rates of caregiver satisfaction with the intervention.
Caregiving
We found that longer hours providing assistance were associated with reduced caregiver employment. Community health services, neurorehabilitation teams, and social services can provide valuable support to people with MS, enabling them to live as independently as possible. 30 In addition, respite services can provide caregivers with temporary relief and the opportunity to pursue important activities.31 Respite services include adult day care, in-home respite, and institutional respite.3 However, a previous study found that only small proportions of informal caregivers assisting people with MS used respite services and many caregivers not using respite care thought these services were needed, with low satisfaction with health insurance coverage of respite care reported.3
Caregiver Physical Health
The caregiver's physical health, as measured by the Physical Component Summary of the SF-8, was significantly linked to caregiver employment, with caregivers experiencing better physical dimensions of health less likely to report reduced employment. The physical, emotional, and financial challenges experienced while providing informal care can affect the caregiver's health and quality of life.32 Health professionals who treat informal caregivers, as well as health professionals treating people with MS, need to be sensitive to the impact that providing assistance has on the physical and mental health of caregivers.
Physicians can have a positive impact on the caregiving experience by recognizing the caregiver's physical, psychological, and emotional needs, as well as developing an integrated plan for medical care in collaboration with patients and their families.32 Patti et al.33 noted that health professionals need to be aware of support programs available to MS caregivers and refer caregivers to these programs. Future studies are needed to identify the types of assistance MS caregivers need at different points along the duration of caregiving. Do informal caregivers just beginning to assist people with MS have different needs and require different types of support and education than caregivers who have been providing assistance for longer periods of time?
Study Limitations
Our survey sample of informal caregivers was developed by contacting people with MS in the NARCOMS Registry. NARCOMS Registry participation is voluntary, and the Registry is not a random sample of people with MS, resulting in possible self-selection bias. However, the Registry membership is large, including about 10% of the American MS population.34 Registry participants have similar age at onset of MS symptoms and comparable demographic characteristics to people with MS in the National Health Interview Survey and the Slifka Study sample.34,35 A previous study found that caregivers and people with MS receiving assistance disagreed about the presence of cognitive symptoms in the person with MS in more than one-quarter of caregiver/care recipient pairs.36
Conclusion
Physicians can have a positive impact on the caregiving experience by recognizing the caregiver's physical, psychological, and emotional needs, as well as developing an integrated plan for medical care in collaboration with patients and their families.32 In addition, successful intervention programs developed for caregivers assisting people with dementia or stroke, such as REACH and TAP, could be adapted for caregivers assisting people with MS experiencing cognitive dysfunction. Health professionals treating caregivers or people with MS need to be aware of respite, support, and intervention programs available to MS caregivers and refer caregivers to these programs, which could reduce the negative impact of caregiving on employment.
PracticePoints.
In this study, poorer cognitive ability by the care recipient to make decisions about daily tasks predicted reduced caregiver employment.
Increased hours per week providing care also predicted reduced caregiver employment.
Interventions to support informal caregivers assisting people with dementia or stroke could be adapted for caregivers assisting people with MS who have cognitive difficulties.
Respite services can provide caregivers with temporary relief from assisting the person with MS and give them the opportunity to pursue important activities.
Acknowledgments
The Lone Star Chapter of the National Multiple Sclerosis Society (NMSS) recruited volunteers to pretest the caregiver survey questionnaire. The Central New England Chapter and the Ozark Branch of the Mid America Chapter of the NMSS recruited volunteers to participate in focus groups for this study. In addition, the authors are grateful to the people with MS who identified their caregivers and the caregivers who participated in the focus groups, the pretest of the survey questionnaire, and the telephone interviews. Without their cooperation and input, this study could not have been completed.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This research was supported by a contract from the Health Care Delivery and Policy Research Program of the National Multiple Sclerosis Society (HC 0043).
References
- 1.National Multiple Sclerosis Society. Research highlights; Winter/Spring 2007. Sonya Slifka Longitudinal Study Renewed. http://www.nationalmssociety.org/download.aspx?id=77. Accessed October 12, 2012.
- 2.McKeown LP, Porter-Armstrong AP, Baxter GD. Caregivers of people with multiple sclerosis: experiences of support. Mult Scler. 2004;10:219–230. doi: 10.1191/1352458504ms1008oa. [DOI] [PubMed] [Google Scholar]
- 3.Buchanan RJ, Radin D, Chakravorty B et al. Perceptions of informal care givers: health and support services provided to people with multiple sclerosis. Disabil Rehabil. 2010;32:500–510. doi: 10.3109/09638280903171485. [DOI] [PubMed] [Google Scholar]
- 4.Covinsky KE, Eng C, Lui L et al. Reduced employment in caregivers of frail elders: impact of ethnicity, patient clinical characteristics, and caregiver characteristics. J Gerontol A Med Sci. 2001;56:M707–M713. doi: 10.1093/gerona/56.11.m707. [DOI] [PubMed] [Google Scholar]
- 5.National Alliance for Caregiving. Caregiving in the U.S. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf. Accessed October 12, 2012.
- 6.Buchanan RJ, Radin D, Chakravorty B et al. Informal care giving to more disabled people with multiple sclerosis. Disabil Rehabil. 2009;31:1244–1256. doi: 10.1080/09638280802532779. [DOI] [PubMed] [Google Scholar]
- 7.North American Research Committee on Multiple Sclerosis (NARCOMS) Project. Welcome to the NARCOMS Registry. http://narcoms.org/. Accessed October 12, 2012.
- 8.Marrie RA, Cutter G, Tyry T et al. Does multiple sclerosis-associated disability differ between races? Neurology. 2006;66:1235–1240. doi: 10.1212/01.wnl.0000208505.81912.82. [DOI] [PubMed] [Google Scholar]
- 9.Orme M, Kerrigan J, Tyas D et al. The effect of disease, functional status, and relapses on the utility of people with multiple sclerosis in the UK. Value Health. 2007;10:54–60. doi: 10.1111/j.1524-4733.2006.00144.x. [DOI] [PubMed] [Google Scholar]
- 10.Ware JE, Kosinkski M, Dewey JE How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8TM Health Survey. Lincoln, RI: QualityMetric Inc; 2001. [Google Scholar]
- 11.US Department of Health and Human Services. Minimum Data Set (MDS)–Version 2.0–for Nursing Home Resident Assessment and Care Screening. Basic Assessment Tracking Form. http://www.cms.hhs.gov/NursingHomeQualityInits/Downloads/MDS20MDSAllForms.pdf. Accessed October 12, 2012.
- 12.Landi F, Tua E, Onder G et al. Minimum Data Set for home care: a valid instrument to assess frail older people living in the community. Med Care. 2000;38:1184–1190. doi: 10.1097/00005650-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Landi F, Capoluongo E, Russo A et al. Free insulin-like growth factor-I and cognitive function in older persons living in the community. Growth Horm IGF Res. 2007;17:58–66. doi: 10.1016/j.ghir.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Med Sci. 1999;54:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 15.Turner-Bowker DM, Bayliss MS, Ware JE et al. Usefulness of the SF-8TM Health Survey for comparing the impact of migraine and other conditions. Qual Life Res. 2003;12:1003–1012. doi: 10.1023/a:1026179517081. [DOI] [PubMed] [Google Scholar]
- 16.Steyerberg EW, Harrell FE. Statistical models for prognostication. In: Max MB, Lynn J, editors. Symptom Research: Methods and Opportunities. Bethesda, MD: National Institutes of Health; Interactive textbook available online at: http://painconsortium.nih.gov/symptomresearch/chapter_8/index.htm. Accessed October 12, 2012. [Google Scholar]
- 17.Steyerberg EW, Eijkemans MJC, Harrell FE, Habbema DF. Prognostic modeling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Stat Med. 2000;19:1059–1079. doi: 10.1002/(sici)1097-0258(20000430)19:8<1059::aid-sim412>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 18.Patti F. Cognitive impairment in multiple sclerosis. Mult Scler. 2009;15:2–8. doi: 10.1177/1352458508096684. [DOI] [PubMed] [Google Scholar]
- 19.Reuter F, Zaaraoui W, Crepsy L et al. Frequency of cognitive impairment dramatically increases during the first 5 years of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2011;82:1157–1159. doi: 10.1136/jnnp.2010.213744. [DOI] [PubMed] [Google Scholar]
- 20.Motl RW, Sandroff BM, Benedict RHB. Cognitive dysfunction and multiple sclerosis: developing a rationale for considering the efficacy of exercise training. Mult Scler J. 2011;17:1034–1040. doi: 10.1177/1352458511409612. [DOI] [PubMed] [Google Scholar]
- 21.Pierson SH, Griffith N. Treatment of cognitive impairment in multiple sclerosis. Behav Neurol. 2006;17:53–67. doi: 10.1155/2006/545860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalmar JH, Gaudino EA, Moore NB, Halper J, DeLuca J. The relationship between cognitive deficits and everyday functional activities in multiple sclerosis. Neuropsychology. 2008;22:442–449. doi: 10.1037/0894-4105.22.4.442. [DOI] [PubMed] [Google Scholar]
- 23.Julian LJ. Cognitive functioning in multiple sclerosis. Neurol Clin. 2011;29:507–525. doi: 10.1016/j.ncl.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Christodoulou C, MacAllister WS, McLinskey NA, Krupp LB. Treatment of cognitive impairment in multiple sclerosis. CNS Drugs. 2008;22:87–97. doi: 10.2165/00023210-200822020-00001. [DOI] [PubMed] [Google Scholar]
- 25.Lyros E, Messinis L, Papageorgiou SG, Papathanasopoulos P. Cognitive dysfunction in multiple sclerosis: the effect of pharmacological interventions. Int Rev Psychiatry. 2010;22:35–42. doi: 10.3109/09540261003589455. [DOI] [PubMed] [Google Scholar]
- 26.Benedict RHB, Zivadinov R. Risk factors for and management of cognitive dysfunction in multiple sclerosis. Nature Rev/Neurology. 2011;7:332–342. doi: 10.1038/nrneurol.2011.61. [DOI] [PubMed] [Google Scholar]
- 27.Johnson KL, Bamer AM, Yorkston KM, Amtmann D. Use of cognitive aids and other assistive technology by individuals with multiple sclerosis. Disabil Rehabil Assist Technol. 2009;4:1–8. doi: 10.1080/17483100802239648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nichols LO, Martindale-Adams J, Burns R, Graney MJ, Zuber J. Translation of a dementia caregiver support program in a health care system–REACH VA. Arch Intern Med. 2011;171:353–359. doi: 10.1001/archinternmed.2010.548. [DOI] [PubMed] [Google Scholar]
- 29.Perrin PB, Johnston A, Vogel B et al. A culturally sensitive Transition Assistance Program for stroke caregivers: examining caregiver mental health and stroke rehabilitation. J Rehabil Res Dev. 2010;47:605–616. doi: 10.1682/jrrd.2009.10.0170. [DOI] [PubMed] [Google Scholar]
- 30.Barnes F. Care of people with multiple sclerosis in the community setting. Br J Commun Nurs. 2007;12:552, 554–557. doi: 10.12968/bjcn.2007.12.12.27741. [DOI] [PubMed] [Google Scholar]
- 31.Dal Santo TS, Scharlach AE, Nielsen J, Fox PJ. A stress process model of family caregiver service utilization: factors associated with respite and counseling service use. J Gerontolog Soc Work. 2007;49:29–49. doi: 10.1300/J083v49n04_03. [DOI] [PubMed] [Google Scholar]
- 32.Mitnick S, Leffler C, Hood VL. Family caregivers, patients, and physicians: ethical guidance to optimize relationships. J Gen Intern Med. 2010;25:255–260. doi: 10.1007/s11606-009-1206-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patti F, Amato MP, Battaglia MA et al. Caregiver quality of life in multiple sclerosis: a multicentre Italian study. Mult Scler. 2007;13:412–419. doi: 10.1177/1352458506070707. [DOI] [PubMed] [Google Scholar]
- 34.Marrie RA, Horwitz R, Cutter G et al. Comorbidity, socioeconomic status and multiple sclerosis. Mult Scler. 2008;14:1091–1098. doi: 10.1177/1352458508092263. [DOI] [PubMed] [Google Scholar]
- 35.Minden SL, Frankel D, Hadden L et al. The Sonya Slifka Longitudinal Multiple Sclerosis Study: methods and sample characteristics. Mult Scler. 2006;12:24–38. doi: 10.1191/135248506ms1262oa. [DOI] [PubMed] [Google Scholar]
- 36.Finlayson M, Shevil E, Cho CC. Perceptions of cognitive symptoms among people aging with multiple sclerosis and their caregivers. Am J Occup Ther. 2009;63:151–159. doi: 10.5014/ajot.63.2.151. [DOI] [PubMed] [Google Scholar]


