Abstract
Living with a chronic illness such as multiple sclerosis (MS) has significant psychosocial ramifications. In particular, the patient's relationship with a spouse or significant other is often negatively affected. Programs are needed to address the psychosocial challenges of the illness and help improve outcomes for both the person with MS and his or her romantic support partner. Relationship Matters (RM) is a relationship enrichment program that integrates information and resources of the National Multiple Sclerosis Society with empirically based marriage education. The purpose of this study was to examine the effectiveness of the RM program in increasing relationship satisfaction and aspects of health-related quality of life in couples living with MS over a 3-month follow-up period. Couples were given 8 hours of programming via in-person workshops disseminated across the country or teleconferences. A control group consisting of members of MS couples who did not receive the intervention was used for comparison. The results indicate that RM significantly improved relationship satisfaction over time compared with no intervention (P < .05). Additional findings include significant improvements in mental health–related quality of life as well as reported improvements in communication, conflict resolution, and ability to handle MS-specific relationship issues. Overall, these findings show that RM results in improved couple functioning and additional psychological health benefits for individuals with MS and their romantic support partners.
Multiple sclerosis (MS) is one of the most prevalent chronic disabling neurologic diseases among adults, affecting an estimated 400,000 people in the United States and 2.1 million people worldwide.1 The disease affects not only the individual diagnosed, but also his or her family members, who often assume caregiving responsibilities. As the onset of MS is usually in early adulthood, interference with development and maintenance of intimate relationships is pervasive. Women diagnosed with a chronic illness such as MS face a 6-fold increase in the risk of divorce.2 A myriad of mental and physical factors are intertwined with health and relationship functioning in physically healthy couples; this interplay is even more complicated in the presence of a chronic illness such as MS. Relationship distress may lead to a poorer course of illness if not addressed adequately.3
The last decade has seen a surge of marriage and relationship education programming and research focused on helping to foster healthy and stable relationships.4 A healthy marriage has been linked to numerous physical and mental health benefits.5 Although the majority of interventions are conducted with non–chronically ill populations, marital quality is likely to be an important resource when dealing with the unique physical and psychological stressors associated with living with—or caring for a loved one with—a chronic illness. The current study examined the results of a relationship enrichment program tailored to couples living with MS in order to assess the potential impact of such programs on relationship functioning and health.
Impact of MS on Relationships
Approximately 30% of people with MS require supportive aid at home, with the majority of care being provided by informal support partners, typically the spouse.6,7 The unpredictable, chronic, disabling, and progressive nature of MS can result in a significant psychosocial burden on the person with MS and his or her family members. The potential effects of the disease on romantic relationships include disease-adjustment challenges, difficulties in relationship and sexual functioning, and relationship dissolution.2,8 Additional ramifications that have been reported by the spousal support partner include decreased marital satisfaction, decreased satisfaction with physical intimacy, and decreased levels of communication.9 For individuals who take on the support partner role, stress can result from multiple factors, including financial strain and the need to provide daily care such as assistance with bathing and other personal needs. The strain of providing care to a chronically ill spouse can by itself lead to decreased marital quality.10 Programs that focus on the needs of both the person with MS and his or her romantic support partner can address multiple dimensions of coping, including important relationship skills.
Relationship Intervention Programs
A recent meta-analysis described the benefits of involving family members in the treatment of adult chronic illness, including positive effects on health outcomes for both the patient and his or her family.11 Intervention studies involving people with MS and their romantic support partners have focused mainly on sexual functioning.12 As relationship distress and reduced marital satisfaction are commonly reported in MS populations, interventions that address a wider range of relationship topics (eg, disease-specific communication and conflict management) are needed. In particular, avoidance of discussing illness-related issues can worsen outcomes for both the person with MS and the support partner.13 The current program was formed in response to the need for improved relationship functioning among MS couples and the astonishing lack of interventions currently available for this population.
One of the few studies that examined relationships beyond sexual intimacy among people with MS found that marital satisfaction can be improved through a counseling intervention consisting of multiple sessions, access to an MS medical team, and a specific treatment regimen and education.14 For the majority of MS couples, interventions as comprehensive as this are not available or practical. Therefore, the effectiveness of less-intensive interventions, such as short in-person workshops or telephone-based counseling, should be assessed. Advantages of a telephone-based intervention include accessibility for people with varying levels of disability and work status as well as convenience for individuals in more rural or remote areas where transportation to metropolitan areas would be difficult. Telephone-based interventions conducted with chronically ill individuals have been shown to result in improvements in physiological outcomes.15 Such studies provide support for the use of alternative delivery modes with a chronically ill population and provide impetus for further examination of how individuals with MS can benefit from more accessible and brief interventions.
Relationship Matters
Examination of relationship enrichment programs in people with MS is vital, particularly given the high risk of marital dissolution in this population. Therefore, through a 5-year Healthy Marriage Initiative grant, the National Multiple Sclerosis Society (NMSS) explored the effects of a relationship enrichment program designed for couples living with MS called Relationship Matters (RM). The aim was to determine whether participation in the RM program resulted in changes in relationship and health outcomes over a 3-month follow-up period compared with no intervention. Specific outcomes of interest were 1) marital/relationship satisfaction, 2) health-related quality of life (HRQOL), and 3) skills in communication and conflict management. The study also sought to determine whether mode of program delivery played a role in outcomes.
Methods
Participants
Relationship Matters program participants (n = 3002) were people with MS and their romantic support partners. Demographic data were collected for all participants (Table 1). Couples recruitment was conducted in each of the NMSS chapters. The RM sample reflected the gender difference in MS diagnosis, with 74% of the people with MS being female (Table 1). Of the RM participants, 83% (n = 2498) participated in a workshop format and 17% (n = 504) participated in a teleconference format. In year 3 of the 5-year demonstration grant, a relationship with the Multiple Sclerosis Society of Canada allowed collection of baseline and 3-month follow-up comparison data from 621 individuals who formed a control group. The Canada sample had larger overall numbers of women (78% of the total sample was female), as fewer support partners participated in the control group, leaving more people with MS in the Canadian sample (Table 1).
Table 1.
Baseline characteristics of RM and control group participants

Procedures
Participants were enrolled in the study through various methods, including the Society Information Resource Center, a website, brochures, targeted mailings, and newsletters. All participation was voluntary, participants provided written informed consent, and programs were free of charge. Additionally, all procedures were reviewed by the Healthy Marriage Grant Oversight Committee. The committee assisted with strategic implementation and oversight of the grant; members were recruited from the NMSS leadership, the mental health community, domestic violence professionals, and other community-based organizations serving people with disabilities. Participants could enroll based on their schedule and current need; randomization was not possible because of emergent need. Participants were offered the program in either the workshop or the teleconference format. Participants completed baseline surveys either in person (workshop group), online (teleconference group), or by mail (teleconference group).
The RM program integrated the information and resources of the NMSS with an empirically based marriage education program called the Prevention and Relationship Enhancement Program (PREP).16 The relationship curriculum was tailored to individuals living with MS. Specifically, the Society used tools created by PREP developers to build a program that was easy to understand, engaging, and relevant to couples living with a chronic illness such as MS. The curriculum taught participants effective communications skills, conflict resolution skills, and relationship maintenance techniques in the context of coping with a chronic illness. Concepts covered included intimacy, financial communication, anger management, and ways to “keep the fun alive.” The people with MS and romantic support partners received the same information and participated in sessions jointly, although each workshop included a 30-minute breakout session where the support partners could discuss concerns separately from the people with MS.
A “workshop-in-a-box” curriculum was created and used at locations throughout the Society's 50-state network. The majority of workshop facilitators were local and able to adjust the program to the local cultural norms of the particular region. All materials were translated into Spanish. Participants were invited to join either an in-person workshop in their local area or a teleconference series held over the phone, each consisting of 8 hours of programming. In-person workshops were held in either a 1-day or a 2-day (with overnight stay) format. The teleconference series took place over 4 or 6 weeks with either 1- or 2-hour calls held once a week during which the curriculum was delivered. Because the curriculum applied to intimate relationships in general, programs were advertised for couples and participants self-identified as “married,” “partnered,” or “dating.” Participants completed a survey immediately upon program completion and again at 3 months after program completion. Incentives to complete the program, such as $50 and an MS-specific book, were offered at 3 months after program completion.
Measures
Demographic Information
A demographic questionnaire gathered descriptive information about the participants: age, gender, geographic location, number of cohabiting children, relationship status, duration since disease diagnosis, type of MS, current symptoms related to MS, and comorbidities.
Revised Dyadic Adjustment Scale
The Revised Dyadic Adjustment Scale (RDAS)17 is a briefer 14-item version of the original 32-item Dyadic Adjustment Scale. The RDAS contains multiple items measuring the domains of consensus, satisfaction, and cohesion. Total RDAS scores may range from 0 to 69, with higher scores indicating less marital distress (better adjustment). A score of 48 has been determined to represent nondistress, with a score of 47 or below indicating distress.18 The RDAS scores were examined for each individual. This tool has been found to be a valid measure of relationship quality17 and has been previously used with MS samples (current Cronbach α = 0.88).19
Health-Related Quality of Life
The 12-item Short Form Health Status Survey (SF-12) is a multipurpose questionnaire with 12 items,20 all selected from the 36-item Short Form Health Status Survey (SF-36). The SF-12 focuses on general health and encompasses eight domains: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, mental health, and role-emotional. Ware et al.20 derived two summary measures from the item scores: the Physical Component Summary (PCS) and the Mental Component Summary (MCS). The PCS and MCS scores range from 1 to 100, with higher scores indicating better functioning. Both are norm-based measures, with a mean of 50 and a standard deviation of 10 in the general US population. Scores above 50 suggest better physical or mental health and scores below 50 suggest worse physical or mental health than that of the general population. The PCS and MCS scores have test-retest reliability of 0.89 and 0.76, respectively,20 and have been used in previous MS samples (current Cronbach α = 0.9).21
Program Outcome Measures
The program outcome measures were developed specifically for the RM program and consist of Likert and open-ended items regarding specific skills learned, instructor assessment, and overall quality of the program. Participants answered these questions immediately upon program completion and again 3 months after program completion. At the 3-month assessment, behavior change was assessed with questions focused on skills learned in the RM program.
Results
Preliminary Analysis
Because of the wide dissemination of the RM program through multiple NMSS chapters, the chronically diseased population, and the nature of the demonstration grant, a large amount of attrition and data incongruence occurred. The baseline RM sample consisted of 3002 participants, which dwindled to 2223 respondents to the surveys immediately after program completion and approximately 400 respondents providing 3-month follow-up outcome data. Of the 3002 individuals who participated in RM, 162 people who began the teleconference series and 34 people who began a workshop did not complete the required 8 hours of programming. Most of the postprogram attrition (583 individuals) was due to missing data. Because it is important to know whether those who left the study differed significantly from those who remained throughout the study, statistical analyses (χ2 tests or analyses of variance [ANOVAs]) were conducted to determine whether significant differences in demographic variables existed between these two groups. Results of these analyses showed that gender, type of MS, and parental status significantly predicted 3-month follow-up completion (women, those with a relapsing-remitting MS [RRMS] diagnosis, and those with children were more likely to drop out; P < .05). These variables were subsequently examined in outcome analyses. Additional analyses investigated whether scores for the outcome variables at baseline (RDAS and SF-12) differed between individuals who stayed and those who dropped out, with no significant differences found (P > .05). Thus, there were no baseline differences in variables such as reported symptoms and comorbidities between the two groups.
Program Outcome Measures
Immediately after program completion, workshop and teleconference surveys showed favorable results, with participants reporting improvements in communication (93%), willingness to try skills learned (99%), better preparedness for addressing issues with the relationship partner (96%), and acquisition of tools to address MS-specific issues with the partner (94%). The proportion of respondents reporting that they planned to incorporate at least one thing learned over the next 3 months was 99%. At 3 months after program completion, positive responses attributed to RM programming (“agree” or “strongly agree”) included reporting of direct use of skills learned (84%), reduced relationship conflict (80%), and improved ability to discuss MS challenges with their partner (81%).
Main Outcomes
Descriptive statistics for the intervention and control groups for the primary outcomes (RDAS and SF-12 scores) at baseline and at 3 months after program completion are shown in Table 2. The number of MS symptoms reported at baseline did not differ significantly between the intervention and control groups (P > .05). The number of comorbidities at baseline differed significantly between the intervention and control groups (P < .05), with the control group reporting fewer diagnosed comorbidities at baseline. In subsequent between-group analyses, baseline comorbidities were controlled for.
Table 2.
Mean (SD) RDAS and SF-12 MCS scores at baseline and 3 months for the RM (workshop and teleconference) and control group participants
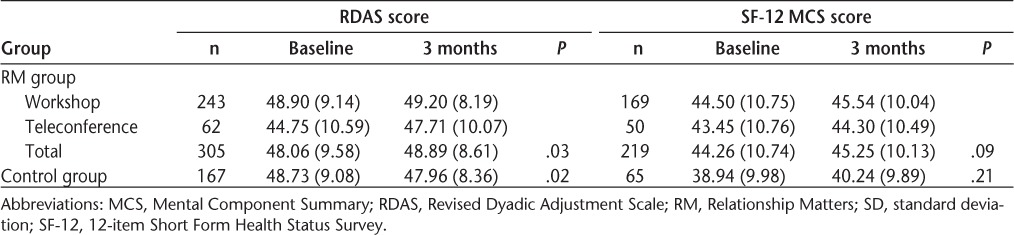
Relationship Quality
A 2 × 2 repeated-measures analysis of covariance (ANCOVA) controlling for baseline reported comorbidities with group (intervention [RM] or control) as the between-subjects factor and the two time points (baseline and 3 months) as the within-subjects factor revealed a significant interaction: F1,469 = 5.89, P < .05, η2 = 0.01. As shown in Figure 1, RM participants experienced an increase in relationship satisfaction over time (from a mean [SD] of 48.06 [9.58] to 48.89 [8.61]; F1,304 = 5.51, P < .05, η2 = 0.02), while control group participants experienced a decrease in such satisfaction (from a mean [SD] of 48.73 [9.08] to 47.96 [8.36]; F1,166 = 3.10, P < .10, η2 = 0.02).
Figure 1.
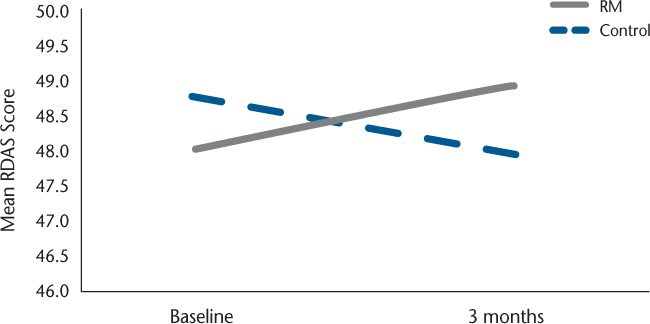
Mean Revised Dyadic Adjustment Scale (RDAS) scores for the Relationship Matters (RM) intervention group and the control group at baseline and at 3 months after program completion
Influence of Demographic Factors
In subsequent ANCOVAs with the RM sample, a second between-subjects factor was added to include status of participant (person with MS or support partner), gender, type of MS, parental status, and duration since disease diagnosis. Neither main effects nor interactions for these additional variables were significant (P > .05), showing that the program was effective for a wide variety of individuals.
Program Delivery Mode
An additional analysis was conducted with the RM sample to examine differences in RDAS scores for the two delivery modes. Specifically, a 2 × 2 repeated-measures ANCOVA controlling for baseline differences in RDAS scores with mode (workshop and teleconference) as the between-subjects factor and the two time points (baseline and 3 months) as the within-subjects factor revealed a significant interaction: F1,302 = 3.49, P < .10, η2 = 0.01. A sharper increase was seen in RDAS scores from baseline (mean [SD], 44.75 [10.59]) to 3 months (mean [SD], 47.71 [10.07]; F1,61 = 14.86, P < .05, η2 = 0.20) for the RM teleconference participants (Table 2). Importantly, teleconference participants' beginning RDAS score was significantly lower (P < .05) and well below the cutoff (48) for distressed relationships. Additional variables that significantly differed at baseline such as age (teleconference group was younger), relationship duration (teleconference group had been in the relationship for a shorter amount of time), and duration since disease diagnosis (teleconference group had a shorter duration) were also examined in separate ANCOVAs, and no significant interactions with these variables was found (P > .05).
Health-Related Quality of Life
Because of the addition of the SF-12 scale later in the grant period and the lower number of control group responses, the effects were examined separately for each group (intervention [RM] and control group). Mental health–related quality of life (MCS) was examined first. A repeated-measures ANCOVA with the two time points (baseline and 3 months) as the within-subjects factor, and controlling for baseline reported depression, was conducted for RM participants for the MCS. The results indicated a significant main effect (F1,217 = 2.97, P < .10, η2 = 0.01), with mean score improvements for RM participants (from a mean [SD] of 44.26 [10.74] to 45.25 [10.13]). No significant change in MCS was found for the control group (P > .05; Table 2). Also, no significant changes were seen in the PCS (P > .05) for either the RM or the control group.
Additional variables including status of participant (person with MS or support partner), gender, type of MS, duration since disease diagnosis, parental status, and program delivery mode were examined, although no significant interactions or main effects were found (P > .05).
Discussion
The current evaluation of a relationship enrichment program, RM, disseminated nationwide via the NMSS yielded encouraging findings overall. Specifically, both the person with MS and his or her romantic support partner reported the acquisition and use of relationship skills over the course of 3 months (communication and disease-specific conflict management). Furthermore, the main outcome of relationship satisfaction was found to significantly improve in the RM group compared with a control group. Additionally, the RM participants showed a significant increase in mental health–related quality of life at 3 months after program completion.
The improvement in relationship satisfaction in this population, although small, is noteworthy, as couples living with a chronic illness commonly report lower relationship satisfaction than do normative samples.9 Therefore, improvement in relationship functioning demonstrates the effectiveness of RM programming in preventing a possible decline. Further evidence that RM is causing this effect is the decline in relationship satisfaction found for the comparison group. Depression, fatigue, and cognitive dysfunction are correlated to dyadic adjustment (RDAS scores), suggesting that improvement in this measure may reduce multiple MS symptoms.19 Social support is critical for managing a chronic disease such as MS,22 and as the majority of this support comes from a romantic partner, the maintenance of that relationship can play an important role in disease management. Unique to this intervention was the active inclusion of the romantic support partner. As family members can have a powerful influence on the physical progression of chronic diseases and a patient's self-care behaviors, including family in disease-specific interventions is crucial.
This study also aimed to examine the potential impact of the relationship enrichment program on participant HRQOL. Scores were not comparable with those of the control group, but significant improvements were found in the MCS scores of the RM participants. Also, no significant change was found over the 3-month period for control group participants. Health-related quality of life has been of increasing interest to researchers assessing interventions for those with MS, as it can provide insight into ways to improve MS care.23 Recent examinations of HRQOL in people with MS found significantly lower scores on both the PCS and MCS compared with the general population and populations with other chronic diseases.21,24 Suggested ways to improve HRQOL in people with MS have ranged from reducing barriers to MS care to supporting employment in order to reduce financial strain21; we would add to that list improvement of relationship satisfaction via psychosocial interventions.
An additional goal of the study was to examine the effects of program delivery mode on outcomes of interest. Teleconference participants had a significantly higher effect size at η2 = 0.20; this is considered to be a medium effect size25 and defines the increase from baseline to 3 months after program completion as clinically meaningful. In addition to the convenience of a telephone intervention, a benefit may be the ability to cater to unique symptoms and have more intimate group conversations over the course of multiple sessions. The teleconference group's greater improvement in relationship satisfaction may be due to the ability to practice concepts and the more recent nature of this group's diagnosis. The current findings as well as those of previous studies15 give support to the use of alternative delivery modes for providing programs to a chronically ill population and provide impetus for further examination of how people with MS can benefit from telephone-based interventions.
Given that MS typically has its onset in young adulthood, often affecting newly formed families, including both the person with MS and the romantic support partner in psychosocial interventions is essential. Relationship Matters is a unique program that gives attention to both individuals involved in the relationship. Thus, the benefits of RM extend beyond the person with MS to the support partner. It has been established that informal MS caregivers can experience impairments in mental health as a result of caregiving burden.26 Interventions such as RM can result in improved mental health and relationship satisfaction of the romantic support partner. Similar improvement in the person with MS can create a healthier environment that facilitates management of a chronic disease.
The program also resulted in improvements in communication, conflict resolution, ability to handle MS-specific relationship issues, and use of skills learned in the program at 3-month follow-up. These improvements represent both relationship and personal gains that can have cascading long-term effects. Although the current study found no improvements in the physical component of quality of life, a lack of decline in this variable can be meaningful in a population with a chronic disease. Studies of future interventions focusing on couples with MS should measure additional physiological outcomes in order to ascertain what effects such programs can have, if any, on disease progression.
Because this study was conducted across multiple NMSS chapter sites with various facilitators, certain limitations are inherent. The high attrition rate for the 3-month follow-up limits the generalizability of the results, as it is possible that only individuals in more stable relationships or those with higher-functioning MS responded to the 3-month data request. The higher dropout rate observed for certain groups of participants, such as women, further limits generalizability. However, mean differences were not found for RDAS scores, baseline reported symptoms, or comorbidities. An additional measure of current disease state at baseline such as the Patient-Determined Disease Steps Scale would have provided a more accurate picture of these differences. In order to be inclusive and reduce negative reaction in those newly diagnosed, this program did not formally assess disease severity. The researchers attempted to increase the 3-month response through multiple brainstorming meetings leading to increased incentives and additional phone calls, e-mails, and letters to nonresponders. In addition, the HRQOL outcome was added significantly later in the grant period, resulting in fewer 3-month follow-up responses and the inability to use the control group for direct comparison. A mean improvement was found, and it is recommended that future studies include this measure to better understand impact. The exploration of differences in delivery mode (in-person vs. teleconference) is somewhat limited, as the teleconference group was smaller and these participants had significantly lower baseline RDAS scores; thus results should be interpreted with caution. Finally, it is recommended that future research on relationship enrichment programs measure mechanisms of change in relationship satisfaction, such as MS-specific coping and communication skills.
Conclusion
Relationship Matters is an innovative program that successfully addresses how MS affects a couple beyond the physical. The findings of this study may be useful to those attempting to improve the relationship satisfaction and quality of life of people living with MS or other chronic illnesses. Interestingly, a stronger relationship effect was seen in the teleconference group; this may be due to the ability to practice techniques, a personal connection with the facilitator, or the convenience of participating in one's own environment. Future intervention studies should continue to include support partners in program design and explore alternative delivery modes. Overall, these findings demonstrate the ability of the RM program to help couples living with chronic diseases improve their relationship satisfaction and mental health–related quality of life. These findings are encouraging for the future development and use of similar programs.
PracticePoints.
MS has been shown to negatively affect relationship functioning; however, few empirically based relationship enrichment programs exist that target this population.
Including the romantic support partner in psychosocial programs for people with MS can have a positive impact on both members of the couple as well as the disease-management process.
Practitioners developing interventions for people with MS should explore alternative modes of program delivery, such as teleconferencing.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: Funding for this project was provided by the United States Department of Health and Human Services, Administration for Children and Families (grant 90FE0090). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the Department of Health and Human Services, Administration for Children and Families.
References
- 1.National Multiple Sclerosis Society. Multiple Sclerosis Information Sourcebook. New York, NY: Information Resource Center and Library of the National Multiple Sclerosis Society; 2006. [Google Scholar]
- 2.Glantz MJ, Chamberlain MC, Liu Q. Gender disparity in the rate of partner abandonment in patients with serious medical illness. Cancer. 2009;115:5237–5242. doi: 10.1002/cncr.24577. et al. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz L, Kraft GH. The role of spouse responses to disability and family environment in multiple sclerosis. Am J Phys Med Rehabil. 1999;78:525–532. doi: 10.1097/00002060-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Halford K, Markman H, Stanley S. Strengthening couples' relationships with education: social policy and public health perspectives. J Fam Psychol. 2008;22:497–505. doi: 10.1037/a0012789. [DOI] [PubMed] [Google Scholar]
- 5.Robles TF, Kiecolt-Glaser JK. The physiology of marriage: pathways to health. Physiol Behav. 2003;79:409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- 6.Minden SL, Frankel D, Hadden LS, Srinath KP, Perloff JN. Disability in elderly people with multiple sclerosis: an analysis of baseline data from the Sonya Slifka Longitudinal Multiple Sclerosis Study. NeuroRehabilitation. 2004;19:55–67. [PubMed] [Google Scholar]
- 7.Buchanan RJ, Radin D, Chakravorty B, Tyry T. Informal care giving to more disabled people with multiple sclerosis. Disabil Rehabil. 2009;31:1244–1256. doi: 10.1080/09638280802532779. [DOI] [PubMed] [Google Scholar]
- 8.Dennison L, Moss-Morris R, Chalder T. A review of psychological correlates of adjustment in patients with multiple sclerosis. Clin Psychol Rev. 2009;29:141–153. doi: 10.1016/j.cpr.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Perrone K, Gordon PA, Tschopp MK. Caregiver marital satisfaction when a spouse has multiple sclerosis. J Appl Rehabil Counseling. 2006;37:26–32. [Google Scholar]
- 10.O'Connor EJ, McCabe M, Firth L. The impact of neurological illness on marital relationships. J Sex Marital Ther. 2008;34:115–132. doi: 10.1080/00926230701636189. [DOI] [PubMed] [Google Scholar]
- 11.Hartmann M, Bazner E, Wild B, Eisler I, Herzog W. Effects of interventions involving the family in the treatment of adult patients with chronic physical diseases: a meta-analysis. Psychother Psychosom. 2010;79:136–148. doi: 10.1159/000286958. [DOI] [PubMed] [Google Scholar]
- 12.Wright DE, Stepleman LM, Davis KN, Hughes MD. Development of a group educational intervention for sexual functioning and intimacy concerns in patients with multiple sclerosis. Int J MS Care. 2009;11:107–113. [Google Scholar]
- 13.Manne SL, Ostroff JS, Norton TR, Fox K, Goldstein L, Grana G. Cancer-related relationship communication in couples coping with early stage breast cancer. Psycho-Oncology. 2006;15:234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- 14.Foley FW, LaRocca NG, Sanders AS, Zemon V. Rehabilitation of intimacy and sexual dysfunction in couples with multiple sclerosis. Mult Scler. 2001;7:417–421. doi: 10.1177/135245850100700612. [DOI] [PubMed] [Google Scholar]
- 15.Trief P, Sandberg JG, Ploutz-Snyder R. Promoting couples collaboration in type 2 diabetes: the diabetes support project pilot data. Fam Syst Health. 2011;29:253–261. doi: 10.1037/a0024564. et al. [DOI] [PubMed] [Google Scholar]
- 16.Renick MJ, Blumberg S, Markman HJ. The Prevention and Relationship Enhancement Program (PREP): an empirically based preventive intervention program for couples. Fam Relations. 1992;41:141–147. [Google Scholar]
- 17.Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and non-distressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21:289–308. [Google Scholar]
- 18.Crane DR, Middleton KC, Bean RA. Establishing criterion scores for the Kansas marital satisfaction scale and the revised dyadic adjustment scale. Am J Fam Ther. 2000;28:53–60. [Google Scholar]
- 19.King KE, Arnett PA. Predictors of dyadic adjustment in multiple sclerosis. Mult Scler. 2005;11:700–707. doi: 10.1191/1352458505ms1212oa. [DOI] [PubMed] [Google Scholar]
- 20.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. Lincoln, RI: QualityMetric Inc; 1998. [Google Scholar]
- 21.Wu N, Minden SL, Hoaglin DC, Hadden L, Frankel D. Quality of life in people with multiple sclerosis: data from the Sonya Slifka Longitudinal Multiple Sclerosis Study. J Health Hum Serv Admin. 2007;30:233–267. [PubMed] [Google Scholar]
- 22.Campbell TL. The effectiveness of family interventions for physical disorders. J Marital Fam Ther. 2003;29:263–281. doi: 10.1111/j.1752-0606.2003.tb01204.x. [DOI] [PubMed] [Google Scholar]
- 23.Kargiotis O, Paschali A, Messinis L, Papathanasopoulos P. Quality of life in multiple sclerosis: effects of current treatment options. Int Rev Psychiatry. 2010;22:67–82. doi: 10.3109/09540261003589521. [DOI] [PubMed] [Google Scholar]
- 24.Buchanan RJ, Huang C, Kaufman M. Health-related quality of life among young adults with multiple sclerosis. Int J MS Care. 2011;12:190–199. [Google Scholar]
- 25.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 26.Buchanan RJ, Radin D, Huang C. Caregiver burden among informal caregivers assisting people with multiple sclerosis. Int J MS Care. 2011;13:76–83. doi: 10.7224/1537-2073-13.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]


